Abstract
Introduction
Chimeric antigen receptor (CAR) T cell therapy is a promising treatment for pediatric patients with relapsed or refractory B cell acute lymphoblastic leukemia (R/R B ALL). Cytokine release syndrome (CRS) is a common toxicity characterized by fever and hemodynamic instability due to pro-inflammatory cytokines. Patients receiving CAR-T cell therapy are also at high risk of infection. Because both infection and CRS present with fever and signs of inflammation, they can be difficult to distinguish.
Karius Inc has developed and validated a novel method for detecting and quantifying microbial cell free DNA (mcfDNA) in plasma for over 1000 species. McfDNA of organisms observed above background at statistically significant levels are reported in molecules per microliter (MPM). This retrospective cohort study sought to describe bacterial Karius Test®(KT) results, concordance with blood culture results, and association with signs of CRS in pediatric patients in the first 2 months after CAR-T cell infusion for R/R B ALL.
Methods
We identified 27 patients who had received CAR-T cell therapy at Lucile Packard Children's Hospital between November 2017 and March 2021 with banked plasma samples available for KT. Patients received CARs targeting CD19, CD22, or CD19-CD22 bispecific. We performed KT prior to CAR-T infusion, week 1, week 2, week 3 and week 4 or later. KT results were classified as likely pathogenic if MPM was >300 or if the same organism was detected on 2 consecutive tests.
Results
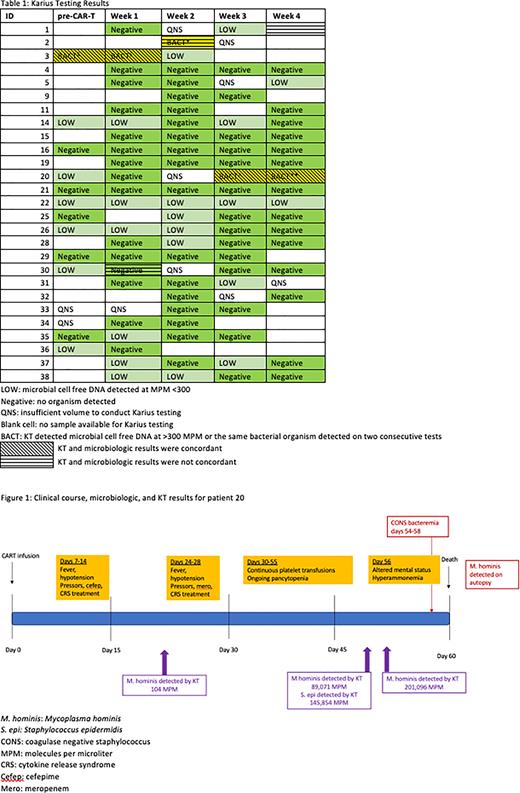
KT results are summarized in Table 1. Five patients had a least 1 positive blood culture in the 2 months post CAR-T infusion. Two of these patients had concurrent KT results that detected the same organism. Patient 3 experienced coagulase negativeStaphylococcus (CONS) bacteremia on days 0-2 post CAR-T. He was febrile a few hours after CAR-T infusion with no signs of CRS. KT was positive for Staphylococcus epidermidis on day -6 and day +3 after CAR-T infusion at MPM of 104,913 and 17,957, respectively.
Patient 20 had grade 3 CRS by day 9 which improved after tocilizumab and steroids. She had recurrence of fevers at Day 24 and was treated with broad spectrum antimicrobials as well as immunosuppressive therapy for CRS. Blood cultures were persistently positive for CONS. She developed severe hyperammonemia at Day 56 with no evidence of hepatic dysfunction and subsequently progressed to cerebral edema and died on day 60 post CAR-T. Mycoplasma hominis was detected by bacterial sequencing on autopsy. KT detected M. hominis at a very low level (MPM 104) on day 21 post CAR-T. Subsequent measurements found increasing MPM for M. hominis at 89,071 on day 52 and then 201,096 on day 57 (Figure 1). Case reports have described M. hominis as a cause of severe hyperammonemia in immunocompromised patients.
The 3 remaining patients (Patients 1, 2, and 30) did not have positive KT results for various reasons. Patient 1 experienced Enterococcus faecium bacteremia on day 23 but did not have a banked sample available for KT. This was in the setting of fevers and hypotension after progression of leukemia post CAR-T. Patient 2 had Streptococcus mitis bacteremia on day 11 post CAR-T and was started on cefepime. His KT was positive for Escherichia coli (but not s. mitis) at 11,559 MPM on day 14. He did not have blood cultures drawn that day so it is unclear if this KT result would have been detected on blood culture. Patient 30 had one blood culture positive for CONS. She was briefly treated with cefepime which was discontinued when subsequent cultures were negative. The CONS was thought to be a contaminant. KT was negative. Patients 2 and 30 had blood cultures sent in the setting of persistent fevers with rising inflammatory markers and Grade 1 CRS.
Analysis across the cohort suggests KT positivity may correlate with periods of increased inflammation after CAR-T infusion. The relationship between KT positivity, inflammatory laboratory values, elevated temperature, and CRS score will be presented.
Conclusions
KT results may be helpful in identifying organisms in febrile patients following CAR-T when other diagnostic measures are unrevealing. This is especially true for fastidious organisms that may not grow in blood culture. Increased KT positivity during times of inflammation after CAR-T may reflect low level translocation rather than environmental contaminants. More work is needed to determine how best to use KT clinically in this patient population.
Disclosures
Berman:Precision Health Solutions: Consultancy; Karius Inc: Current Employment. Duttagupta:Nucleix: Current Employment; Karius Inc: Ended employment in the past 24 months.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal