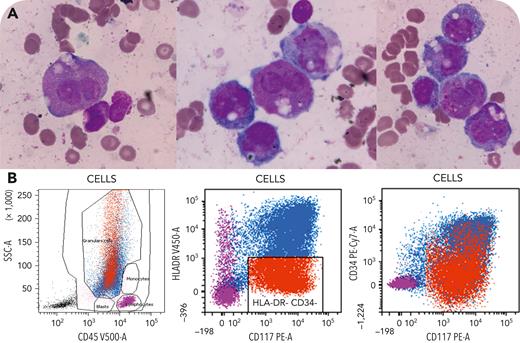
A 69-year-old woman was admitted for pancytopenia. Complete blood count showed the following: a leukocyte count of 1.3 × 109/L (reference values: 4-10 × 109/L); hemoglobin level of 46 g/L (reference values: 120-160 g/L); platelet count of 26 × 109/L (reference values: 150-350 × 109/L); and normal coagulation parameters. Bone marrow aspirate showed the presence of blast cells (90%), with multiple granulations associated with irregular nuclei, suggesting acute promyelocytic leukemia (APL) (panel A; May-Grunwald-Giemsa stain, objective 100×, original magnification ×100), although no Auer rod was detected. Flow cytometry analysis showed a side scatter pattern typical of APL diagnosis (blasts in granulocytes). Moreover, blast cells expressed CD13, CD33, and CD117, and 55% of them were negative for CD34 and HLA-DR (panel B), in agreement with the World Health Organization definition of APL. Full cytogenetic analyses based on 24 metaphases revealed 46,XX. Fluorescence in situ hybridization analysis revealed no PML-RARA gene fusion. Next-generation sequencing (46-gene panel) identified mutations in BCOR and BCORL1 (variant allele fraction [VAF] 42%), NRAS and STAG2 (VAF 39% for both), and 2 TET2 variants (VAF 39% and 42%).
In this patient, the presence of atypical blast cells and flow cytometry features suggested APL, but without the classical PML-RARA gene fusion. Finally, the identification of BCOR/BCORL1 mutations, which have been reported only once in acute myeloid leukemia, confirmed another mechanism for hypergranular acute myeloid leukemia.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal