Patients with sickle cell disease (SCD) commonly experience episodes of disabling vaso-occlusive pain leading to emergency department (ED) visits or hospitalizations. SCD is also associated with significant neurocognitive risk due to overt stroke, silent cerebral infarcts, and chronic insufficiencies in oxygen and/or glucose delivery to the brain. Neurocognitive deficits are observed early in life and are often characterized by deficits in executive functioning skills (e.g., planning, organizing, attention). The patterns of progressive chronic medical complications and functional limitations associated with SCD place children at higher risk of experiencing depressive symptoms.
Research in patients with SCD has suggested that the experience of pain is associated with executive skills and depression in children with SCD. However, studies have yet to explore the bidirectional relationship between these constructs. It is important to understand the directionality and causal nature of this relationship using a longitudinal approach to optimize treatment approaches. The primary objective of this study was to investigate associations between pain-related ED visits or hospitalizations with future parent-reported executive functioning and depression; conversely we examined how executive difficulties and depression predicted subsequent pain-related visits.
All patients were enrolled in the St. Jude longitudinal cohort study, the Sickle Cell Clinical Research Intervention Program (SCCRIP; Hankins et al., Pediatric Blood & Cancer 2018). The number of ED visits or hospitalizations due to pain-related reasons in the year pre- and post-assessment were obtained retrospectively from chart review. This data was then cleaned, validated, and merged with other data sets. Parent ratings of executive skills were collected using the Behavior Rating Inventory of Executive Function (BRIEF) Global Executive Composite scale. Depressive symptoms were measured using the parent version of the Behavior Assessment System for Children 2 nd or 3 rd Edition (Depression scale). Multivariable generalized linear regression was used to examine associations between the number of pain-related hospitalizations with executive difficulties and depressive symptoms after adjusting for age, sex, sickle genotype, current hydroxyurea treatment, and geocoded social vulnerability. P-values <0.05 were considered significant.
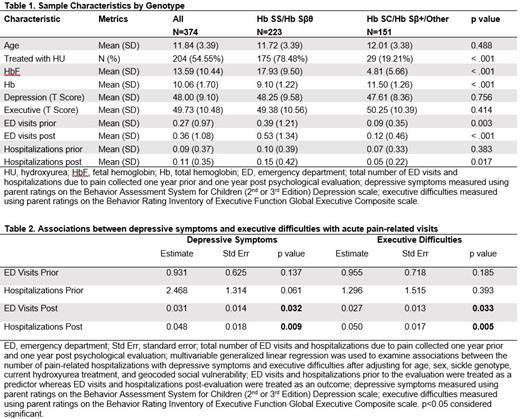
We included 374 patients with SCD (60% HbSS/HbSβ 0-thalassemia; see Table 1). The mean age of participants at the time of psychological evaluation was 11.84 years (SD=3.39; Range= 8-18). In the year prior to the assessment, patients experienced an average of 0.27 pain events requiring a visit to the ED (SD=0.97, Range=0-11). In the year post evaluation, there were an average of 0.36 events (SD=1.08, Range=0-9). Hospitalizations due to pain occurred an average of 0.09 times (SD=0.37, Range=0-3) in the year before the evaluation and 0.11 times (SD=0.35, Range=0-2) post-evaluation. The number of pain events leading to ED visits or hospitalization in the year prior to the evaluation were not associated with future depressive symptoms or executive difficulties. However, parent-rated executive difficulties and symptoms of depression were positively associated with future ED visits (p=0.033 and p=0.032) and hospitalizations (p=0.005 and p=0.009) in the year following the evaluation (Table 2).
Executive functioning difficulties and depressive symptoms predicted greater frequency of future ED visits and hospitalizations among children with SCD. Hospital visits due to acute SCD pain did not predict future executive difficulties or depressive symptoms. Behavioral and pharmacological treatments targeting depressive symptoms and executive difficulties should be tested to decrease the frequency of acute care visits due to pain in SCD.
Disclosures
Heitzer:Global Blood Therapeutics: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal