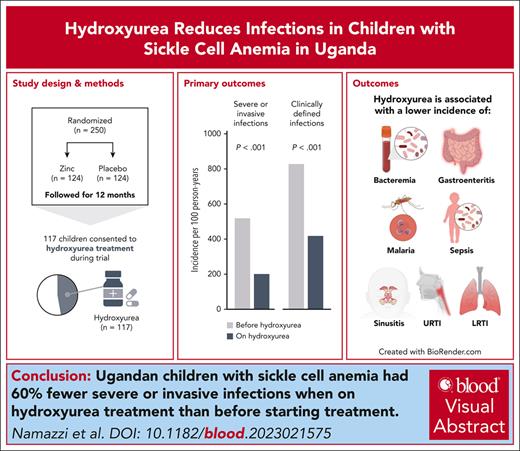
Visual Abstract
After starting hydroxyurea treatment, Ugandan children with sickle cell anemia had 60% fewer severe or invasive infections, including malaria, bacteremia, respiratory tract infections, and gastroenteritis, than before starting hydroxyurea treatment (incidence rate ratio, 0.40 [95% confidence interval, 0.29-0.54]; P < .001).
TO THE EDITOR:
Infections remain an important cause of morbidity and mortality for children with sickle cell anemia (SCA) in Africa,1 the continent with the highest burden.2 Infections often precede SCA-related complications (eg, vaso-occlusive crises [VOC],3 hemolytic anemia,4 acute chest syndrome5), and infections are also a major cause of hospitalization and death.6
Hydroxyurea is efficacious against SCA-related complications, reducing the incidence of VOC, hospitalization, and blood transfusion.7-9 Furthermore, hydroxyurea is safe and feasible in Africa,7,9 and is now licensed for SCA in Uganda. BABY HUG and NOHARM, 2 placebo-controlled randomized trials of hydroxyurea in children with SCA, reported fewer infections in the hydroxyurea arm, but with low rates and no statistically significant differences.7,10 REACH, a large multicountry prospective open label trial in African children with SCA, reported a significantly lower incidence of nonmalarial infections (32%) and malaria (50%) after initiating hydroxyurea.9,11 However, these studies did not focus primarily on infections, so rigorous diagnostic definitions and evaluations were not included. Consequently, no conclusive evidence exists on whether hydroxyurea reduces infections in children with SCA.
Zinc for infection prevention in sickle cell anemia (ZIPS, NCT03528434) was a randomized, placebo-controlled, double-blind trial evaluating daily oral zinc (10 mg/day for 12 months) to prevent infections in Ugandan children with SCA.12 ZIPS was conducted at the Nalufenya Sickle Cell Clinic, Jinja Regional Referral Hospital in Uganda. The study included rigorous definitions of severe or invasive infections and found that zinc at 10 mg/day did not reduce infections.13 During ZIPS, hydroxyurea was recommended for SCA and many parents agreed to start treatment. We now report the incidence of infections in ZIPS before and after initiating hydroxyurea.
The parents or legal guardians of all study participants provided written informed consent to participate in the study. Ethical approval was obtained from the Makerere University School of Medicine Research and Ethics Committee and the Indiana University Institutional Review Board. The Uganda National Drug Authority and the Uganda National Council of Science and Technology granted regulatory approval.
When ZIPS began enrollment in 2019, hydroxyurea was new to the study area and local sickle cell clinic. Based on the published NOHARM7 and REACH9 trial results, the study team recommended hydroxyurea for all study participants, and required hydroxyurea for children meeting the 2016 Ugandan Ministry of Health SCA treatment guidelines criteria unless parents refused the drug. Hydroxyurea treatment during the study was provided by the study free of charge. Because of the novelty of hydroxyurea as SCA treatment, plus concerns about side effects, its role as a cancer drug, and concerns about future drug costs after the study ended, most parents initially refused hydroxyurea treatment, but approximately half agreed to start hydroxyurea by the end of the trial.
Treatment used locally available hydroxyurea formulations and per national guidelines, was offered at 20 ± 2.5 mg/kg per day, with dose adjustments for weight or hematological toxicities. Children were monitored monthly for 3 months after treatment initiation, then quarterly to coincide with ZIPS study visits. Severe or invasive infections were defined based on World Health Organization criteria (supplemental Tables 1-2, available on the Blood website).13 Children were evaluated in the clinic for evidence of infection and SCA-related events using rigorous protocol-based definitions (supplemental Table 3).12 All children were on daily penicillin prophylaxis and monthly sulfadoxine-pyrimethamine malaria prophylaxis.
The incidence of infection and SCA-related events before and after hydroxyurea was evaluated using negative binomial regression or Poisson regression models as appropriate. Analyses were adjusted for the zinc treatment arm, and a P value of <.05 after Benjamini-Hochberg correction for multiple comparisons was considered significant.
Of 248 eligible children randomly assigned in the ZIPS trial, only 2 were taking hydroxyurea at enrollment, but 117 children initiated hydroxyurea during the study. Parental willingness to use hydroxyurea (60.7%) and frequent VOC (36.8%) were the most common treatment indications. The median age of children on hydroxyurea was 2.8 years (interquartile range, 2.0-3.7) and 51 (43.6%) were male. The average starting dose (mean ± SD) was 20.0 ± 0.1 mg/kg per day and the duration on hydroxyurea was 224 ± 85 person-days.
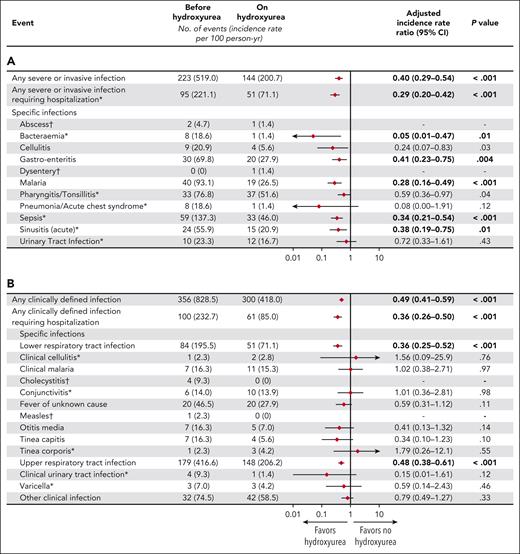
There was a large decrease in the incidence of severe or invasive infections after hydroxyurea treatment was started vs before starting hydroxyurea treatment: 519 vs 201 severe or invasive infections per 100 person-years, for an adjusted incidence rate ratio (IRR), 0.40 (95% confidence interval [CI], 0.29-0.54), P < .001 (Figure 1A). Severe or invasive infections requiring hospitalization declined even more sharply during hydroxyurea treatment (IRR, 0.29; 95% CI, 0.20-0.42; P < .001). Among predefined severe or invasive infections, the incidence of bacteremia, gastroenteritis, malaria, sepsis, and sinusitis all decreased significantly on hydroxyurea treatment. The incidence of malaria was reduced by 72% (IRR, 0.28; 95% CI, 0.16-0.49; P < .001).
Incidence of infections in children before hydroxyurea treatment compared to during hydroxyurea treatment. (A) Severe or invasive infections; (B) clinically defined infections. Negative binomial or ∗Poisson mixed effects regression analysis adjusted for zinc treatment arm. Person-years before hydroxyurea = 43.0; after hydroxyurea = 71.8. †Both models did not converge or had nonpositive definite G matrix. Incidence rates that differ significantly after adjustment by the Benjamini-Hochberg method are in bold type.
Incidence of infections in children before hydroxyurea treatment compared to during hydroxyurea treatment. (A) Severe or invasive infections; (B) clinically defined infections. Negative binomial or ∗Poisson mixed effects regression analysis adjusted for zinc treatment arm. Person-years before hydroxyurea = 43.0; after hydroxyurea = 71.8. †Both models did not converge or had nonpositive definite G matrix. Incidence rates that differ significantly after adjustment by the Benjamini-Hochberg method are in bold type.
Clinically defined infections were also reduced significantly during hydroxyurea treatment (IRR, 0.49; 95% CI, 0.41-0.59; P < .001; Figure 1B). This reduction was largely driven by decreased lower respiratory (IRR, 0.36; 95% CI, 0.25-0.50; P < .001) and upper respiratory tract infections (IRR, 0.48; 95% CI, 0.38-0.61; P < .001), respectively. Clinically defined infections requiring hospitalization decreased even more substantially (IRR, 0.36; 95% CI, 0.26-0.50; P < .001). Analysis comparing infection incidence in the 117 children started on hydroxyurea to 117 study children not started on hydroxyurea, matched by month of enrollment to account for potential variations in infection incidence by season or year, and adjusted for age and zinc treatment arm, showed that children in the hydroxyurea group had significantly higher incidence of infection than children in the no hydroxyurea before starting hydroxyurea, which decreased to the levels of the no hydroxyurea group after hydroxyurea initiation (supplemental Tables 4-5). Thus, relative risk of infection in the period after hydroxyurea initiation was significantly lower in the hydroxyurea than no hydroxyurea group when compared with the prior period in which both groups were not on hydroxyurea, (supplemental Table 6). These findings provide further evidence that hydroxyurea treatment was associated with reduced infection.
The incidence of SCA-related complications, including VOC, hospitalizations, and blood transfusions, decreased substantially on hydroxyurea (P ≤ .001, supplemental Figure 1). Six of the 9 deaths occurred in children on placebo and not taking hydroxyurea, and all 5 deaths for which a cause was known were due to infection (pneumonia [n = 4], malaria [n = 2], and/or sepsis [n = 2]). The only child on hydroxyurea who died had cellulitis and sepsis and was prescribed hydroxyurea only 4 days before death.
Our results document that hydroxyurea was associated with a 60% reduction of all severe or invasive infections (71% requiring hospitalization), and a 51% reduction of all clinically defined infections (64% requiring hospitalization). Multiple severe infections were significantly reduced on hydroxyurea, including malaria, bacteremia, sepsis, gastroenteritis, sinusitis, and lower respiratory infections. All deaths in the study with a known cause were due to infection. Study limitations include the lack of monitoring of hydroxyurea use by pill count or other method and potential confounding by indication.
The reduced incidence of malaria on hydroxyurea in our cohort was 72%, consistent with the recently published long-term REACH results with a 76% malaria reduction.14 The incidence of nonmalarial infections in our cohort (60% reduction) is even greater than REACH (38% reduction). Together, these study results strongly suggest that hydroxyurea treatment lowers malaria incidence and other infections in African children with SCA, thereby reducing an important source of morbidity and mortality.
Hydroxyurea is a particularly attractive agent for infection prevention as it combines qualities of once daily dosing, documented safety, lack of drug tolerance or resistance, and compelling efficacy against multiple SCA-related complications.14 Although its mechanisms of protection against infections are not fully defined, the documented effects against multiple pathogens suggest that hydroxyurea may reduce infection in part through improved immune function, potentially preserved splenic function, and may reduce disease severity through its anti-inflammatory effects. Direct antimicrobial activity by hydroxyurea could also play a role, given documented in vitro bacterial killing by hydroxyurea, notably Escherichia coli15,16 and potent in vitro hydroxyurea activity against multiple parasites, including Leishmania species,17,18Trypanosoma cruzi,17 and the apicomplexan parasites Toxoplasma gondii17,19 and Babesia microti.20 In murine models, hydroxyurea decreased parasitemia, prevented experimental cerebral malaria,21 and had direct activity against schizont stages of malaria.22 Together, these data suggest that hydroxyurea may have both immunomodulatory and antimicrobial effects that reduce the risk of infections.
The present study provides compelling evidence that hydroxyurea decreases not only SCA-related clinical complications but also a broad spectrum of infections, including malaria. These data support the wider use of hydroxyurea in malaria-endemic areas and suggest that hydroxyurea should be considered the standard of care for SCA across Africa.
Acknowledgments
The authors thank the study participants and their caregivers, the Jinja Regional Referral Hospital children's ward and sickle cell clinic, the study team at Global Health Uganda for conducting the study, and the data-coordinating center at Indiana University for data management and analysis and especially.
The Thrasher Research Fund (TRF14221) provided funding but did not participate in study design, analysis, report writing, or the decision to submit the study for publication.
Authorship
Contribution: R.N., R.O., A.T., R.E.W., and C.C.J. designed the study, supervised the study, and analyzed the results; R.N. wrote the first draft of the manuscript; D.D. and A.L.C. performed laboratory analyses, supervised laboratory processes, analyzed the results, and monitored the study; C.B., J.H.J., and M.J.G. supervised data management and quality control and analyzed the results; and all authors participated in the editing of the manuscript and approved the final version.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Chandy C. John, Department of Pediatrics, Ryan White Center for Pediatric Infectious Disease and Global Health, Indiana University School of Medicine, 705 Riley Hospital Dr, RI5900, Indianapolis, IN; email: chjohn@iu.edu.
References
Author notes
Original data are available upon reasonable request from Chandy C. John (chjohn@iu.edu) or Ruth Namazzi (namazzi101@gmail.com).
The online version of this article contains a data supplement.
There is a Blood Commentary on this article in this issue.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal