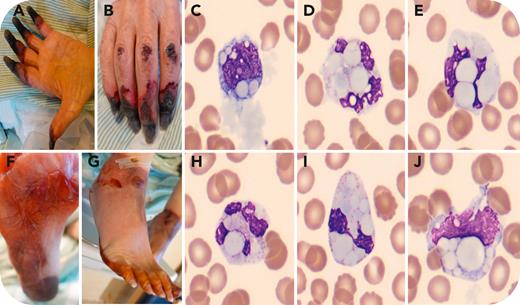
An 84-year-old man with chronic lymphocytic leukemia (CLL), recently transformed into Hodgkin lymphoma, presented with fatigue, diarrhea, pain, and progressive necrosis of the fingers (panels A-B) and toes (panels F-G) shortly after his first chemotherapy session. His complete blood count showed hemoglobin of 89 g/L, leukocytes 9.11 × 109/L, and platelets 103 × 109/L. Wright-Giemsa staining (panels C-E, H-J) revealed amorphous crystals within red blood cells and globular inclusions in neutrophils and monocytes (100× objective). Cryoglobulin testing was positive for heat-insoluble cryoglobulins. Serum protein electrophoresis showed monoclonal immunoglobulin IgG-κ (2 g/L) and monoclonal IgA (<1 g/L). Complement levels were low, and IgG4 was selectively increased. Hepatitis C and HIV tests were negative. The analyzer flagged immature granulocytes and platelet clumps, likely due to larger neutrophils phagocytosing precipitates (panels D-E, H-I) and platelet aggregation from circulating precipitates.
Standard cryoglobulin testing, which heats the sample to 37°C, would not allow detection of heat-insoluble cryoglobulins, potentially causing false negatives and delays in treatment. These atypical cryoglobulins, which may dissolve at higher temperatures (eg, 56°C), can cause severe systemic damage, including renal failure and gangrene. The detection of cryoglobulin crystals in the blood smear was crucial for the diagnosis. This case highlights the need for improved diagnostic and therapeutic protocols for heat-insoluble cryoglobulinemia.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal