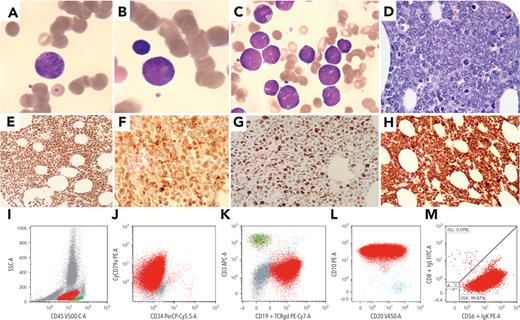
A 72-year-old man admitted with psoas hematoma. Laboratory results showed leukocytosis (15 × 109/L), anemia (75 g/L), thrombocytopenia (110 × 109/L), creatinine 130 μmol/L, and lactate dehydrogenase 3500 U/L. There was no evidence of lymphadenopathy or organomegaly. Peripheral blood showed 3% medium-sized mononuclear cells with scant cytoplasm, round nuclei with fine chromatin, and inconspicuous nucleoli (panels A-B; Wright-Giemsa stain, 100× lens objective). Bone marrow aspirate revealed 70% blastoid cells (panel C;100× lens objective). Bone marrow biopsy exhibited sheets of mononuclear cells with some chromatin margination (panel D; hematoxylin and eosin stain, 40× lens objective), which were positive for PAX5 (panel E); CD20 (partial), CD10, IRF4, and BCL2 (panel F); MYC (panel G); and Ki-67 (∼100%, panel H); and negative for CD34/TdT/cyclin D1. Flow cytometry (panels I-M) identified 65% of cells in the “blast” gate expressing CD19, CD20, CD79b, CD10, and kappa, but negative for CD34/TdT/CD5/BCL6. Cytogenetics showed a complex karyotype. Fluorescence in situ hybridization was positive for MYC and IGH/BCL2 rearrangements but negative for BCL6 rearrangement. A diagnosis was made of DLBCL/HGBL with MYC and BCL2 rearrangements.
Double-hit B-cell lymphoma, usually presenting in adults with lymphadenopathy, is very rare with isolated peripheral blood and bone marrow involvement. It is important to be aware of this unusual presentation and blastoid morphology to avoid the misdiagnosis of acute lymphoblastic leukemia, as these conditions differ in their treatment approach and prognosis. Appropriate ancillary testing is crucial to reach an accurate diagnosis.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal