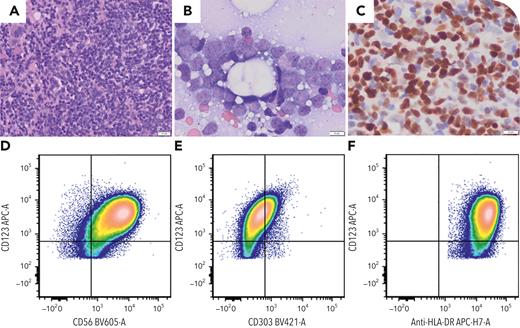
A 57-year-old woman presented with fatigue and progressive abdominal pain. Physical exam demonstrated splenomegaly. No skin lesions were present. A complete blood count showed a white blood cell count of 4.6 × 109/L, transfusion-dependent anemia (hemoglobin 7.2 g/dL), and a platelet count of 22 × 109/L. Splenic ultrasound revealed splenic infarct. Bone marrow biopsy demonstrated 88% abnormal immature cells (panel A; hematoxylin and eosin stain, original magnification × 400; panel B; Giemsa stain, original magnification ×1000), positive for CD123, HLA-DR, CD56, and downregulation of CD303 (panels D-F) with expression of CD4, TCL1, and TCF4 (panel C; TCF4 immunohistochemistry with hematoxylin counterstain, original magnification ×1000), and negative for other lineage-defining markers. Lumbar puncture with intrathecal cytarabine was performed demonstrating cerebrospinal fluid (CSF) involvement at baseline. A diagnosis was established of blastic plasmacytoid dendritic cell neoplasm (BPDCN) extensively replacing the bone marrow with concomitant baseline CSF involvement. Cytogenetics studies showed diploid karyotype and next-generation sequencing showed dominant clonal TET2 and SRSF2 and subclonal ASXL1, and NRAS (×2) mutations. The patient was treated with a frontline CD123-targeted regimen and scheduled for allogeneic stem cell transplantation.
In the setting of BPDCN being historically regarded as predominantly an older male disease with the vast majority presenting with cutaneous lesions, this case highlights an unusual clinical presentation of a female patient, younger than 60 years of age, and with extensive bone marrow and CSF involvement and, importantly, the absence of typical BPDCN skin lesions.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal