Abstract
A retrospective analysis of cytomegalovirus (CMV) genotype was conducted on 281 CMV isolates obtained from marrow transplant recipients. The genotyping was based on sequence variations in the gene encoding envelope glycoprotein B (gB) as detected by restriction analysis of polymerase chain reaction (PCR)-amplified gB DNA. Among all isolates studied, the distribution of gB types 1-4 was 48.4%, 16.4%, 24.6%, and 8.2%, respectively, with only 2.5% of all isolates containing more than one gB type. The association of gB types with acute graft-versus-host-disease (GVHD) and death related to myelosuppression was examined using appropriate multivariable regression models. Covariables in addition to gB type included underlying disease type, donor-recipient HLA matching, donor CMV serostatus, and age as a continuous variable. Death associated with myelosuppression occurred in 2.9% or 4 of 136 patients with gB1, 0% or 0 of 46 patients with gB2, 21.7% or 15 of 69 patients with gB3, and 17.4% or four of 23 patients with gB4. The significant association of CMV gB type with death due to myelosuppression was maintained in a multivariable analysis (P < .001). In addition, the data also suggested that gB types 3 and 4 may be associated with a reduced hazard of grades II to IV acute GVHD.
CYTOMEGALOVIRUS (CMV) infection has long been suspected of causing myelosuppression in a subset of marrow transplant recipients.1-6 This supposition is supported by in vitro studies, which have identified several different mechanisms by which CMV may interfere with hematopoiesis.7-13 These include direct infection of progenitor cells, stromal cells, or accessory cells, resulting in cell death, altered expression of cellular genes, or immune reactions against the CMV-infected cells or noninfected bystanders. Examples of all of these have been reported, but the basis for the diversity of effects is unknown. Given this diversity and the observation that only a subset of CMV-infected patients will experience myelosuppression, it is reasonable to speculate that some undefined variable particular to the virus may influence the outcome of infection.
Currently, comparative sequencing studies have begun to define the extent of interstrain variations in selected coding regions of the CMV genome. Analysis of the gene encoding envelope glycoprotein B (gB) showed that clinical isolates adopted one of four sequence configurations, allowing all isolates to be assigned a gB genotype of 1-4.14 The different gB genes display significant amino acid variations in their variable domains, including changes that affect glycosylation. However, it has not been determined how these differences may affect function, particularly given that the function of gB is not completely defined. Studies do suggest that gB may be the target for antibodies and may play a role in viral entry into cells.15-17 Therefore, genetic variation could affect pathogenicity and clinical outcome in immunocompromised patients. This contention is supported by previous reports that showed an increased frequency of gB1 among marrow transplant recipients with a favorable outcome following CMV infection, an increased frequency of gB2 among acquired immunodeficiency syndrome (AIDS) patients with CMV retinitis, and an association of gB type with CMV dissemination in human immunodeficiency virus (HIV)-infected patients.18-20
In the current report, a retrospective analysis was used to test the hypothesis that gB type will influence the manifestation of CMV infection in patients receiving marrow transplants. The endpoint of interest was death from infectious complications of neutropenia, which appeared to be significantly associated with the relatively rare gB genotypes 3 and 4.
MATERIALS AND METHODS
Patients.The study included 281 marrow transplant recipients with CMV infection, defined as positive culture from blood, urine, throat, or tissue. This number is composed of samples from 150 consecutive patients with positive virus cultures from any site, with or without CMV disease, who were typed to estimate the gB frequency distribution among all infected patients. The remaining 131 patients were typed as part of a separate study designed to determine gB frequency distribution among patients with different forms of CMV disease. This study includes cohorts representing consecutive patients with CMV pneumonia, gastrointestinal disease, or viremia only. Patients were not selected on the basis of neutrophil counts or cause of death. The majority of patients entered in the study were transplanted between January 1984 and December 1990, with only 20 of the 281 transplanted after 1990. Likewise, with few exceptions, the patients studied were not enrolled in early treatment protocols involving ganciclovir or foscarnet.
The endpoint of interest was death due to infectious complications associated with neutropenia (absolute neutrophil count [ANC] <500). All causes of death were determined by chart review blinded with respect to gB type.
Viral isolates.CMV isolates from transplant recipients were routinely frozen at −70°C after 0 to 3 passages in human foreskin fibroblasts. Sufficient DNA could be directly isolated from these stocks without further culture. The gB typing was performed on the first isolate obtained from each patient.
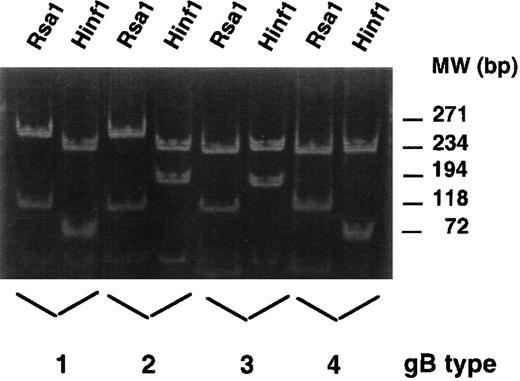
gB typing.In the first 200 patients, gB typing was performed as previously described.18 Briefly, DNA was extracted from viral isolates using a polymerase chain reaction (PCR)-compatible lysing buffer. Samples were digested with proteinase K at 55°C for 1 hour. PCR was conducted using primers gB1319 and gB1604, which amplify a region of high peptide variability in the gB gene corresponding to a portion of gp55. Depending on the genotype of the virus, these primers yielded amplimers of 293 to 296 bp. The amplimers were then digested with Hinf1 and Rsa1 in two separate reactions. The digested DNA was resolved into informative banding patterns on 8% polyacrylamide gels.
A more sensitive nested PCR method was developed and used for subsequent isolates. In this method, the first round of amplification uses oligonucleotides located in the region spanning nucleotides 1292 to 1676 of the gB gene. The numbering of base pairs is according to Genbank sequence M60931. PCR reaction mixtures contain 1.0 mmol/L Mg+, 50 μmol/L each deoxynucleotide triphosphate (dNTP), 1 U Taq polymerase, 20 mmol/L Tris-Cl (pH 8.4), 50 mmol/L KCl, and 0.5 μmol/L each primer. Amplification is performed with one cycle of 4 minutes at 94°C and 20 cycles of 30 seconds at 94°C, 1.5 minutes at 55°C, and 30 seconds at 72°C, one final extension cycle of 5 minutes at 72°C. PCR product from the first round of amplification is used as template in the second round of amplification with gB primers spanning the region 1292 to 1613. Amplification is performed using the same reaction components. After 4 minutes at 94°C, the DNA is amplified for 35 cycles (1 minute at 94°C, 1.5 minutes at 55°C, 2.0 minutes at 72°C) followed by a final cycle of 10 minutes at 72°C. The “uncut” product is then digested with Rsa1 or Hinf1 yielding the informative banding patterns shown in Fig 1.
Restriction digest patterns for gB types 1-4: Digestion with Rsa1 distinguishes types 1 and 2 from 3 and 4, whereas digestion with Hinf1 distinguishes 1 from 2 and 3 from 4. All lysates from four patients were amplified with primers gB1292 × gB1676. Aliquots of the first round of PCR were then amplified with primers gB1292 × gB1613. Products of the second round of amplification were digested with Rsa1 or Hinf1. Restriction digests were resolved on 10% polyacrylamide gels and stained with ethidium bromide. φχ176 HaeIII marker DNA was used to estimate molecular weight (lanes not shown). The DNA used for PCR template for gB types 1-3 were obtained from clinical isolates propagated on foreskin fibroblasts. The gB type 4 PCR product was directly amplified from cells harvested from a long-term marrow culture established from a patient with graft failure.
Restriction digest patterns for gB types 1-4: Digestion with Rsa1 distinguishes types 1 and 2 from 3 and 4, whereas digestion with Hinf1 distinguishes 1 from 2 and 3 from 4. All lysates from four patients were amplified with primers gB1292 × gB1676. Aliquots of the first round of PCR were then amplified with primers gB1292 × gB1613. Products of the second round of amplification were digested with Rsa1 or Hinf1. Restriction digests were resolved on 10% polyacrylamide gels and stained with ethidium bromide. φχ176 HaeIII marker DNA was used to estimate molecular weight (lanes not shown). The DNA used for PCR template for gB types 1-3 were obtained from clinical isolates propagated on foreskin fibroblasts. The gB type 4 PCR product was directly amplified from cells harvested from a long-term marrow culture established from a patient with graft failure.
Statistical analysis.The primary question of interest in this study addressed the association of gB type with the probability of death due to infectious complications of neutropenia. A χ2 test was used to compare the proportion of patients who experienced this complication across gB types. Further analysis was performed to allow for the possibility that other factors or complications might be associated with this outcome. This was done by fitting logistic regression models that used the occurrence of death due to the complications of neutropenia as the outcome variable. gB type was included as an explanatory variable in addition to other pre- and posttransplant factors known to impact on neutropenia. These included patient age, HLA matched versus mismatched versus unrelated donor status, disease risk (high v low), donor CMV serostatus, and occurrence of acute GVHD. Similarly, Cox regression was used to examine the association of gB type with the hazard of acute GVHD. All reported P values are two-sided and those associated with regression models are derived from the Wald test. No adjustments were made for multiple comparisons.
RESULTS
Genotyping of CMV isolates.PCR amplification and restriction digestion of the gB gene yielded informative banding patterns for all 281 isolates studied. The digest patterns that distinguish gB types 1-4 are shown in Fig 1. The data indicate that the distribution of gB types among all transplant recipients is 48.4%, 16.4%, 24.6%, and 8.2% for types 1-4, respectively, with only seven of 281 patient samples (2.5%) containing more than one gB type. This distribution in all patients does not differ significantly from that established in previous studies.14,18 21 However, results indicate only 4 of 136 patients with gB1, and none of the 46 patients with gB2 experienced death due to the complications of neutropenia. This was in contrast to 15 of 69 and 4 of 23 patients with types 3 and 4, respectively (Table 1).
Causes of Death Among Patients With CMV gB Types 1-4
| Cause of Death* . | gB1 (%) . | gB2 (%) . | gB3 (%) . | gB4 (%) . | Mix (%) . |
|---|---|---|---|---|---|
| CMV (n = 46) | 21 (15.4) | 11 (23.9) | 11 (15.9) | 2 (8.7) | 1 (14.3) |
| Relapse (n = 73) | 45 (33.1) | 10 (21.7) | 14 (20.3) | 3 (13.0) | 1 (14.3) |
| Other (n = 31) | 15 (11.0) | 7 (15.2) | 4 (5.8) | 4 (17.4) | 1 (14.3) |
| Unknown (n = 8) | 4 (2.9) | 2 (4.3) | 1 (1.4) | 1 (4.3) | 0 (0) |
| Myelosuppression (n = 24) | 4 (2.9) | 0 (0) | 15 (21.7) | 4 (17.4) | 1 (14.3) |
| Total dead | 89 | 30 | 45 | 14 | 4 |
| Total patients | 136 | 46 | 69 | 23 | 7 |
| Cause of Death* . | gB1 (%) . | gB2 (%) . | gB3 (%) . | gB4 (%) . | Mix (%) . |
|---|---|---|---|---|---|
| CMV (n = 46) | 21 (15.4) | 11 (23.9) | 11 (15.9) | 2 (8.7) | 1 (14.3) |
| Relapse (n = 73) | 45 (33.1) | 10 (21.7) | 14 (20.3) | 3 (13.0) | 1 (14.3) |
| Other (n = 31) | 15 (11.0) | 7 (15.2) | 4 (5.8) | 4 (17.4) | 1 (14.3) |
| Unknown (n = 8) | 4 (2.9) | 2 (4.3) | 1 (1.4) | 1 (4.3) | 0 (0) |
| Myelosuppression (n = 24) | 4 (2.9) | 0 (0) | 15 (21.7) | 4 (17.4) | 1 (14.3) |
| Total dead | 89 | 30 | 45 | 14 | 4 |
| Total patients | 136 | 46 | 69 | 23 | 7 |
Data represent the absolute number of patients and the percentages of patients dead of a specific cause among all patients with that gB type.
The causes of death were determined from archived research files. CMV deaths include deaths due to CMV pneumonia, disseminated CMV, as well as gastrointestinal CMV. Relapse was documented by histology and cytogenetics. Other causes included GVHD, veno-occlusive disease, and multiorgan failure. Deaths attributed to myelosuppression were caused by infectious complications of neutropenia (ANC < 500), none were associated with host-mediated graft rejection. Eight patients had incomplete files and were lost to follow-up.
The similar frequency of death due to myelosuppression in patients with gB types 1 and 2 compared with 3 and 4, together with a previous study, which also suggested functional similarities between CMV strains with gB3 and 4, provided the rationale for combining type 1 with 2, and 3 with 4 for the multivariable analysis. This also permitted the inclusion of two patients with a mix of types 3 and 4. In combination, there were 94 patients with strain type 3 and/or 4. Of these, 20 died of infectious complications of neutropenia, giving an incidence of 21.3%. In contrast, there were 182 patients with strain type 1 or 2, of which only 4 died of neutropenia-associated infections, giving an incidence of 2.2%. A simple comparison of these proportions leads to a difference that is highly significant (P < .001). Relevant characteristics of patients with gB1 and 2 compared with gB3 and 4 are shown in Table 2.
Patient Characteristics Sorted by gB Type
| . | Type 1 or 2 . | Type 3 or 4 . |
|---|---|---|
| . | (n = 183) . | (n = 92) . |
| . | No. of Patients . | No. of Patients . |
| Diagnosis at transplant | ||
| ALL/remission | 10 | 7 |
| ALL/relapse | 16 | 6 |
| AML/remission | 20 | 14 |
| AML/relapse | 32 | 17 |
| Breast cancer | 2 | 0 |
| CML-Chronic phase | 34 | 17 |
| CML-Accelerated phase | 10 | 6 |
| CML-Second chronic phase | 3 | 0 |
| CML-Blast phase | 4 | 2 |
| HD | 3 | 0 |
| NHL/remission | 4 | 1 |
| NHL/relapse | 13 | 5 |
| MDS | 7 | 3 |
| MM | 2 | 1 |
| Other | 23 | 13 |
| Acute GVHD | ||
| ? | 7 | 3 |
| 0-I | 64 | 38 |
| II-IV | 112 | 51 |
| CMV disease | 116 | 52 |
| Patient/donor CMV serostatus | ||
| +/+ | 81 | 44 |
| +/− | 58 | 30 |
| −/+ | 20 | 6 |
| −/− | 8 | 3 |
| ? | 16 | 9 |
| Donor type | ||
| Auto | 10 | 6 |
| Matched | 120 | 49 |
| Mismatched related | 32 | 21 |
| URD | 21 | 16 |
| Median age | 34 | 31 |
| Number dead | 120 | 59 |
| Median day of death | 140 | 145 |
| Median day 1st + CMV culture | 78 | 83 |
| . | Type 1 or 2 . | Type 3 or 4 . |
|---|---|---|
| . | (n = 183) . | (n = 92) . |
| . | No. of Patients . | No. of Patients . |
| Diagnosis at transplant | ||
| ALL/remission | 10 | 7 |
| ALL/relapse | 16 | 6 |
| AML/remission | 20 | 14 |
| AML/relapse | 32 | 17 |
| Breast cancer | 2 | 0 |
| CML-Chronic phase | 34 | 17 |
| CML-Accelerated phase | 10 | 6 |
| CML-Second chronic phase | 3 | 0 |
| CML-Blast phase | 4 | 2 |
| HD | 3 | 0 |
| NHL/remission | 4 | 1 |
| NHL/relapse | 13 | 5 |
| MDS | 7 | 3 |
| MM | 2 | 1 |
| Other | 23 | 13 |
| Acute GVHD | ||
| ? | 7 | 3 |
| 0-I | 64 | 38 |
| II-IV | 112 | 51 |
| CMV disease | 116 | 52 |
| Patient/donor CMV serostatus | ||
| +/+ | 81 | 44 |
| +/− | 58 | 30 |
| −/+ | 20 | 6 |
| −/− | 8 | 3 |
| ? | 16 | 9 |
| Donor type | ||
| Auto | 10 | 6 |
| Matched | 120 | 49 |
| Mismatched related | 32 | 21 |
| URD | 21 | 16 |
| Median age | 34 | 31 |
| Number dead | 120 | 59 |
| Median day of death | 140 | 145 |
| Median day 1st + CMV culture | 78 | 83 |
Abbreviations: ALL, acute lymphocytic leukemia; CML, chronic myelocytic leukemia; HD, Hodgkin's disease; NHL, non-Hodgkin's lymphoma; MDS, myelodysplastic syndrome; MM, multiple myeloma; GVHD, graft-versus-host disease; URD, unrelated donor.
Strain type 3 or 4 versus 1 or 2 was included as a covariable in various logistic regression models in addition to acute GVHD (present v absent for both grades 0 to I and grades II to IV), donor status (unrelated donor v mismatched v matched), underlying disease risk (high v low), and age at transplant as a continuous variable. Table 3 summarizes this analysis and shows that the qualitative conclusion with respect to the highly significant positive association of strain types 3 and 4 with fatal infectious complications of neutropenia remains unchanged even after the other variables were included in the regression models. Because of the relatively low number of events, only variables that were statistically significant or suggestive of being associated with the probability of death due to infectious complications of neutropenia were included in the final multivariable model shown in Table 3.
Logistic Regression Analyses of Death Associated With Myelosuppression
| Covariable . | P Value . | Odds Ratio . | 95% CI . |
|---|---|---|---|
| Strain type | |||
| 1 or 2 | — | 1.0 | — |
| 3 or 4 | <.001 | 12.26 | (4.05, 37.11) |
| Strain type | |||
| 1 or 2 | — | 1.0 | — |
| 3 or 4 | <.001 | 13.25 | (4.33, 40.53) |
| Age at TX | .086 | 1.03 | (0.996, 1.065) |
| Strain type | |||
| 1 or 2 | — | 1.0 | — |
| 3 or 4 | <.001 | 19.16 | (5.34, 68.75) |
| Acute GVHD | |||
| Grades 0-1 | — | 1.0 | — |
| Grades II-IV | .021 | 4.03 | (1.24, 13.08) |
| Age at TX | .058 | 1.04 | (0.999, 1.077) |
| Covariable . | P Value . | Odds Ratio . | 95% CI . |
|---|---|---|---|
| Strain type | |||
| 1 or 2 | — | 1.0 | — |
| 3 or 4 | <.001 | 12.26 | (4.05, 37.11) |
| Strain type | |||
| 1 or 2 | — | 1.0 | — |
| 3 or 4 | <.001 | 13.25 | (4.33, 40.53) |
| Age at TX | .086 | 1.03 | (0.996, 1.065) |
| Strain type | |||
| 1 or 2 | — | 1.0 | — |
| 3 or 4 | <.001 | 19.16 | (5.34, 68.75) |
| Acute GVHD | |||
| Grades 0-1 | — | 1.0 | — |
| Grades II-IV | .021 | 4.03 | (1.24, 13.08) |
| Age at TX | .058 | 1.04 | (0.999, 1.077) |
Abbreviation: TX, transplantation.
The association between CMV gB type and GVHD was tested directly in a Cox regression analysis with acute GVHD grades II to IV as the endpoint and each of the covariables listed above as explanatory variables in addition to gB type. Table 4 summarizes this analysis and indicates that relative to strain type 1, there is a suggestion of a reduced hazard of acute GVHD grades II to IV in patients with CMV gB types 3 and 4 relative to patients with CMV gB type 1, even after adjusting for selected patient characteristics.
Proportional Hazards Regression Analysis of Grades II-IV GVHD
| Covariable . | P Value . | Relative Risk . | 95% CI . |
|---|---|---|---|
| Strain type | |||
| 1 | — | 1.00 | — |
| 2 | .19 | 0.74 | 0.47, 1.16 |
| 3 | .05 | 0.68 | 0.46, 1.00 |
| 4 | .05 | 0.50 | 0.25, 1.00 |
| Disease type | |||
| Not high risk | — | 1.00 | — |
| High risk | .20 | 0.81 | 0.59, 1.12 |
| Donor type | |||
| Matched | — | 1.00 | — |
| Mismatched/URD | <.001 | 2.92 | 2.08, 4.09 |
| Donor CMV serostatus | |||
| Negative | — | 1.00 | — |
| Positive | .41 | 1.15 | 0.83, 1.59 |
| Age at transplant | |||
| Continuous variable | .82 | 1.00 | 0.99, 1.01 |
| Covariable . | P Value . | Relative Risk . | 95% CI . |
|---|---|---|---|
| Strain type | |||
| 1 | — | 1.00 | — |
| 2 | .19 | 0.74 | 0.47, 1.16 |
| 3 | .05 | 0.68 | 0.46, 1.00 |
| 4 | .05 | 0.50 | 0.25, 1.00 |
| Disease type | |||
| Not high risk | — | 1.00 | — |
| High risk | .20 | 0.81 | 0.59, 1.12 |
| Donor type | |||
| Matched | — | 1.00 | — |
| Mismatched/URD | <.001 | 2.92 | 2.08, 4.09 |
| Donor CMV serostatus | |||
| Negative | — | 1.00 | — |
| Positive | .41 | 1.15 | 0.83, 1.59 |
| Age at transplant | |||
| Continuous variable | .82 | 1.00 | 0.99, 1.01 |
DISCUSSION
Several reports indicate that between 10% and 24% of transplant recipients will either fail to engraft or, after achieving a graft, experience poor marrow function.22-25 Given our limited understanding of what events must occur for rapid and sustained engraftment, our ability to treat patients experiencing poor engraftment has been empirical. In some cases, patients have been treated with second transplants.26-29 In other cases, patients have been treated with recombinant growth factors.30 31 These protocols have met with limited success, which may not be surprising, as it is unclear whether paucity of donor stem cells or the absence of a particular growth factor is really the underlying mechanism of failure.
Studies of individual patients with graft failure have indicated that a proportion can be attributed to classic rejection mechanisms involving host lymphocytes reactive against donor cells.24,32 In contrast, the processes responsible for nonrejection failures or poor marrow function are not well-defined. In a number of clinical studies, myelosuppression has been observed in association with specific underlying diseases like aplastic anemia or myelodysplasia, as well as regimen-related toxicities, GVHD, and virus infection.1 33-36 The means by which these variables influence marrow function and why only a proportion of patients affected with these complications experience myelosuppression are largely unknown.
In this report, we have determined that death due to myelosuppression in CMV-infected marrow transplant recipients is associated with particular CMV genotypes. Whether CMV and myelosuppression are causally related is not addressed in this study. Hypothetically, if they were related, the association with specific CMV genotypes would help explain why only a subset of CMV-infected patients actually experience this complication. Data reported to date suggest that CMV strains distinguished by variations in the gene encoding envelope glycoprotein B (gB) may differ in tropism and pathogenicity. In keeping with this, our earlier report indicated that patients who survived CMV infection more commonly shed virus of gB type 1 than those who died of CMV infection.18 Additional support for a role of gB in viral tropism comes from recent studies of HIV-infected patients, which showed a predominance of CMV gB type 2 in patients with retinitis, a predominance of gB type 4 in semen,19 and an association of gB types with viral dissemination.20
In our current report, 21.3% of patients with gB types 3 and 4 died of infection associated with neutropenia compared with only 2.2% of patients with types 1 and 2. One could interpret this to mean either that gB types 3 and 4 are more likely to infect marrow, that once infected, marrow function is more adversely affected by these types of virus, or that types 3 and 4 are capable of escaping immune recognition in the marrow and therefore persist to cause more damage. The last hypothesis might also help explain the negative association of gB types 3 and 4 with acute GVHD that was also suggested by these data. One could speculate that CMV, in triggering an immune response, initiates or exacerbates GVHD. In this case, if CMV types 3 and 4 somehow escape immune recognition, they would not only persist to cause more damage, but they would also trigger less GVHD.
The possibility that gB variations may influence pathogenicity is very dependent on the function of gB. In herpes simplex virus, gB has been shown to be involved in cell entry.16 Therefore, one can speculate that alterations in gB could affect tropism. Alternatively, given that gB is abundantly expressed on the surface of virions and infected cells, gB variations could affect the ability of the host to clear virus.17 Finally, it is possible that gB is a surrogate marker for another gene, which is in linkage disequilibrium with gB. In fact, in our previous report, 73% of gB type 3 and 92% of type 4 were associated with gH type 1, whereas only 26% of gB type 1 and 54% of type 2 were associated with gH type 1.18 The preferential linkage of gB3 and 4 with gH1 was significant with P = .019 and P = .0002, respectively. Given that the predicted amino acid sequences of gB types 3 and 4 are very dissimilar, it may be reasonable to speculate that they do not have comparable function and that their association in the current analysis may be attributed to the strong linkage disequilibrium between gB3 and 4 and some other gene, perhaps gH. In this case, gB type may serve only as a surrogate marker for functionally distinct CMV strains.
In vitro studies designed to determine the effect of gB type on viral tropism or pathogenicity have been difficult to interpret. Although different isolates have been shown to infect different components of a long-term marrow culture, virtually all isolates showed some deleterious effect on myelopoiesis.7,11 12 The relevance of these observations becomes questionable because only a small subset of patients from whom these isolates were obtained actually experienced marrow failure and most isolates were obtained from sites other than marrow. One could argue that the in vitro propagation of virus in fibroblasts, which is necessary to generate sufficient virus for experimentation, altered the tropism of the virus and therefore its in vitro effect. In addition, the long-term marrow culture system is artificial and not subject to immune surveillance. Therefore, results obtained in long-term marrow cultures deliberately infected with propagated virus may not reflect the natural tropism or pathogenicity of the virus in vivo.
The outcome of the retrospective study presented in this report may be influenced by the way patients were selected. This concern notwithstanding, the strength of the association observed makes it reasonable to hypothesize that particular CMV genotypes may be responsible for myelosuppression. Testing this hypothesis in vivo will require detection and phenotyping of virus directly from marrow. Ideally this would involve a prospective study to determine the frequency and gB genotypes of CMV detected in the marrow of a patient population and subsequent analysis of these determinations with clinical outcome. This would allow a more formal test of the association suggested in this report and would minimize the chance of selection bias. Such a study is currently under way.
ACKNOWLEDGMENT
The authors thank medical students, Paul Cunningham and Peter Zia, for their help in CMV genotyping, Carol Bevan and Laura Bolles for their technical assistance, and Harriet Childs for preparing the manuscript.
Supported in part by Grants No. CA18029, CA18221, HL36444, DK34431, and DK51417 from the National Institutes of Health, Department of Health and Human Services (DHHS), Bethesda, MD.
Address reprint requests to Beverly Torok-Storb, PhD, Fred Hutchinson Cancer Research Center, 1124 Columbia St, M318, Seattle, WA 98104-2092.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal