Abstract
CD38 is a membrane-associated ecto-nicotinamide adenine dinucleotide (NAD+) glycohydrolase that is expressed on multiple hematopoietic cells. The extracellular domain of CD38 can mediate the catalysis of NAD+ to cyclic adenosine diphosphoribose (cADPR), a Ca2+-mobilizing second messenger, adenosine diphosphoribose (ADPR), and nicotinamide. In addition to its enzymatic properties, murine CD38 has been shown to act as a B-cell coreceptor capable of modulating signals through the B-cell antigen receptor. To investigate the in vivo physiological function(s) of this novel class of ectoenzyme we generated mice carrying a null mutation in the CD38 gene. CD38−/− mice showed a complete loss of tissue-associated NAD+ glycohydrolase activity, showing that the classical NAD+ glycohydrolases and CD38 are likely identical. Although murine CD38 is expressed on hematopoietic stem cells as well as on committed progenitors, we show that CD38 is not required for hematopoiesis or lymphopoiesis. However, CD38−/− mice did exhibit marked deficiencies in antibody responses to T-cell–dependent protein antigens and augmented antibody responses to at least one T-cell–independent type 2 polysaccharide antigen. These data suggest that CD38 may play an important role in vivo in regulating humoral immune responses.
© 1998 by The American Society of Hematology.
THE TYPE II membrane-associated glycoprotein CD38 is the prototypic member of the class of adenosine diphosphoribose (ADPR) transfer enzymes known as nicotinamide adenine dinucleotide (NAD+) glycohydrolases.1CD382-4 and the classical NAD+glycohydrolases5,6 are multifunctional ectoenzymes able to catalyze the net hydrolysis of NAD+ to nicotinamide and ADPR,7 as well as to catalyze both the synthesis and hydrolysis of cylic adenosine diphosphoribose (cADPR). Thus, in addition to their intrinsic NAD+ hydrolysis (NADase) activity, these enzymes possess both adenine diphosphate (ADP)-ribosyl cyclase and cADPR hydrolase activities. The possibility that these ectoenzymes might be involved in the metabolism of cADPR is intriguing given that cADPR is a potent inositol triphosphate (IP3)-independent Ca2+-mobilizing agent8-10 believed to be involved in Ca2+-induced Ca2+ release in multiple mammalian cell types, including pancreatic β cells11 and neuronal cells.12,13 cADPR has also been shown to augment the proliferative response of activated murine B lymphocytes,2 as well as to mediate the Ca2+release associated with adenosine triphosphate (ATP)-activated potassium currents in alveolar macrophages,14 suggesting that cADPR may function as a signaling second messenger in multiple hematopoietic cell types.
All of the mammalian NAD+ glycohydrolases that have been identified to date, including CD38,15 the bone marrow stromal cell surface molecule BP-3/BST-1,16,17 and the T-cell differentiation marker RT-6,18 are highly expressed on cells of hematopoietic origin. Although originally identified as a lymphocyte surface antigen,19 CD38 is now known to be expressed by many hematopoietic cell types including murine bone marrow-derived stem cells, B cells throughout ontogeny, subsets of developing and mature T cells, natural killer cells, macrophages, granulocytes, neutrophils, and platelets, as well as by pancreatic β cells and in organs such as the brain, liver, and kidney.15,20-22 Clinically, CD38 has been recognized for many years as a marker for certain human malignancies,19,23,24 and recent studies have suggested that CD38 may be a useful prognostic indicator of human immunodeficiency virus disease progression.25 26
In addition to serving as a marker for different cell types, CD38 has been shown to have a number of immunologically relevant functional activities in vitro. For example, CD38 has been implicated as an adhesion molecule capable of binding endothelial cells.20In addition, ligation of CD38 by specific monoclonal antibodies can induce cytokine production by human peripheral blood mononuclear cells,27 enhance murine macrophage antigen presenting cell (APC) function (N. Solvason et al, manuscript in preparation), inhibit B lymphopoiesis,28 protect mature B lymphocytes from apoptosis,20,29 and induce proliferation of mature T and B lymphocytes.15,20 More recently, murine CD38 was shown to act as a coreceptor for the B-cell antigen receptor (BCR) capable of either augmenting or depressing BCR-mediated B-cell activation30,31 in a manner similar to that observed for CD19.32 CD38, in combination with interleukin-5 (IL-5), has also been shown to be a potent costimulatory signal for IgM and IgG1 production by mature splenic B lymphocytes,33 further implicating CD38 in the regulation of signals delivered through the BCR. Although the exact mechanism(s) by which CD38 modulates lymphocyte responses is still to be determined, it has been shown that signaling through CD38 in various lymphoid and myeloid cell populations involves the activation and tyrosine phosphorylation of numerous intracellular substrates including phospholipase C-γ, c-cbl, syk, btk, lyn, fyn, and ZAP-70.33-35 Interestingly, CD38 ligation on human immature B cells was recently shown to induce tyrosine phosphorylation of CD19 and the subsequent association of CD19 with lyn and phosphatidylinositol 3 (PI3)-kinase.36 Taken together, these data suggest that CD38 might use the signal transduction pathways associated with CD19 to mediate certain B-cell responses. Even more recent data have shown that CD38 can potentiate signals through (Gi)-coupled chemotactic formyl-Met-Leu-Phe receptors on human myeloid cells37 suggesting that G-protein–coupled signal transduction pathways might also be involved in CD38-mediated intracellular signaling.
In the present study we generated CD38-deficient mice to elucidate the biological function(s) of CD38 in vivo, as well as to extend our understanding of the functional heterogeneity and physiological role of NAD+ glycohydrolases. Our initial studies presented here show that CD38−/− mice exhibit altered humoral immune responses, supporting our recent in vitro findings that CD38 is a coreceptor for the BCR.30
MATERIALS AND METHODS
Generation of CD38 gene-targeted mice.
The murine CD38 gene from exons 1 through 6 was cloned from a 129SvEv mouse λ genomic library (Stratagene, La Jolla, CA). The CD38 targeting vector was generated by subcloning isolated genomic fragments into a vector containing the neomycin resistance gene, and the HSV-TK gene. 129Ola-derived E14-1 embryonic stem (ES) cells (kindly provided by Drs Klaus Rajewsky and Ralf Kuhn, Institute for Genetics, University of Cologne, Cologne, Germany) were transfected with aCla I linearized targeting vector, and 2 of 300 (1 of 150) G418r/gancr colonies (310 mg/mL active G418, 2 mmol/L gancyclovir) screened were determined to be correctly targeted by Southern blot analysis. CD38+/− ES clones were injected into C57BL/6J blastocysts, blastocysts were implanted into pseudopregnant B6.CBA F1 females, and resulting chimeras were crossed to C57BL/6J mice to establish germline transmission. CD38+/− F1 mice were intercrossed, and F2 breeding pairs were established from CD38+/+ and CD38−/− mice. 129Ola × C57BL/6J F3 mice were used for all experiments shown. Both homologous recombinant clones (236 and 2832) transmitted the CD38 mutation to the germline, and experiments confirmed in both clones are indicated.
Assay of NAD+ glycohydrolase activity.
Membrane fractions were prepared from spleen, liver, and brain by homogenization of whole organs at 4°C in 1 mL of 50 mmol/L potassium phosphate buffer, pH 6.8, using a glass Dounce homogenizer. The total protein concentration was determined by the BCA* protein assay (Pierce, Rockford, IL) by using bovine serum albumin as the standard. NAD+ glycohydrolase and nucleotide pyrophosphatase activity determinations were made using sensitive fluorometric enzyme assays. The reactions were performed at 37°C, in a 2-mL final volume of 50 mmol/L potassium phosphate buffer, pH 6.8, and the reaction progress was followed by monitoring the increase in fluorescence at 410 nm (excitation at 310 nm). This pH value minimizes the self-inactivation of the murine NAD+glycohydrolase.1 NAD+ glycohydrolase activity was measured with 1, N6-etheno-NAD+ as substrate under saturating conditions (250 μmol/L final concentration).38 Nucleotide pyrophosphatase activity was measured under the same experimental conditions using as substrate pyridine 1, N6-ethenoadenine dinucleotide (62.5 μmol/L final concentration), a poorly NADase-hydrolyzable analog.39 40 This activity was determined because it can contribute to the hydrolytic cleavage of 1, N6-etheno-NAD+, potentially leading to an overestimation of NADase activity. The NAD+ glycohydrolase values shown in Table 1 represent real NAD+ glycohydrolase activities, derived by subtracting the nucleotide pyrophosphatase activity from the total measured NAD+ glycohydrolase activity. Enzyme activity measurements determined by fluorometric enzyme assays were confirmed by analysis of the reaction products by high-performance liquid chromatography (HPLC). HPLC analysis was performed on Microcon 10 (Amicon, Beverly, MA) concentrated aliquots of the reaction media by using a Waters HPLC system (Waters Chromatography, Milford, MA). Chromatography was performed on a 300 × 3.9 mm μBondpack C18column (Waters Chromatography) operated at ambient temperature at a flow rate of 1 mL/min. The compounds were eluted isocratically with a 10-mmol/L ammonium phosphate buffer, pH 5.5, containing 1.5% (vol/vol) acetonitrile and were detected by ultraviolet absorbance at 260 nm.
NAD+ Hydrolysis Activities in CD38+/+ and CD38−/− Mice
| . | NAD+Glycohydrolase Activity-150 Vm (nmoles/min/mg protein) . | Nucleotide Pyrophosphatase Activity-150 Vm (nmoles/min/mg protein) . | ||
|---|---|---|---|---|
| CD38+/+ . | CD38−/− . | CD38+/+ . | CD38−/− . | |
| Spleen (n = 3) | 87.2 ± 4.1 | 0.59 ± 0.15 | 0.34 ± 0.1 | 0.33 ± 0.14 |
| Liver (n = 3) | 19.3 ± 1.6 | ND | 0.63 ± 0.23 | 0.63 ± 0.20 |
| Brain (n = 3) | 22.5 ± 1.7 | ND | 0.49 ± 0.19 | 0.46 ± 0.19 |
| . | NAD+Glycohydrolase Activity-150 Vm (nmoles/min/mg protein) . | Nucleotide Pyrophosphatase Activity-150 Vm (nmoles/min/mg protein) . | ||
|---|---|---|---|---|
| CD38+/+ . | CD38−/− . | CD38+/+ . | CD38−/− . | |
| Spleen (n = 3) | 87.2 ± 4.1 | 0.59 ± 0.15 | 0.34 ± 0.1 | 0.33 ± 0.14 |
| Liver (n = 3) | 19.3 ± 1.6 | ND | 0.63 ± 0.23 | 0.63 ± 0.20 |
| Brain (n = 3) | 22.5 ± 1.7 | ND | 0.49 ± 0.19 | 0.46 ± 0.19 |
NAD+ glycohydrolase and nucleotide pyrophosphatase activity measurements were made on tissue homogenates prepared from individual 12-week-old 129Ola × C57BL/6J F3 CD38−/−mice and CD38+/+ littermate controls. Data shown represent the mean ± standard deviation of three individual mice per determination.
Abbreviation: ND, not detected.
NAD+ glycohydrolase and nucleotide pyrophosphatase activity measurements were determined by fluorometric enzyme assays as described in the Materials and Methods.
Long-term reconstitution assays.
The repopulating ability of CD38−/− bone marrow was determined in a competitive repopulation assay.41 Bone marrow was obtained from the femurs and tibias of CD38+/+and CD38−/− (Ly5.2) 129Ola x C57BL/6J mice. C57BL/6J (Ly5.1) recipient mice were irradiated with 950 rad from an x-ray source operated at 200 kV delivering 85 rad/min. Mice were irradiated in a split dose administered 4 to 5 hours apart. A total of 5 × 106 bone marrow cells from each source were injected retroorbitally into irradiated recipients. After irradiation and reconstitution, the recipient animals were maintained on antibiotic-containing water (polymixin B sulfate 106 U/L and neomycin sulfate 1.1 g/L) for at least 6 weeks. Reconstituted mice were analyzed at 12 weeks by fluorescence-activated cell sorting (FACS) staining of peripheral blood for the lineage antigens B220, CD3, Mac-1, and GR-1, as well as for the donor marker Ly5.2. The percentage of Ly5.2+ cells in each lineage was determined by integration by using FACS Desk software (Stanford University, Stanford, CA).
Immunizations and measurement of antigen-specific serum immunoglobulin levels.
For immunization with T-cell–dependent (TD) protein antigens, 8- to 10-week-old mice were immunized intraperitoneally with either 10 μg or 1 μg of alum-precipitated 2,4,6-trinitrophenyl conjugated to keyhole limpet hemocyanin (TNP5-KLH), or 10 μg of complete Freud’s adjuvant (CFA)-precipitated 4-hydroxy-3-nitrophenylacetyl coupled to chicken γ-globulin (NP20-CG) on day 0 for a primary immunization, and again on day 21 (TNP5-KLH) or day 28 (NP20-CG) for a secondary immunization. Mice were bled, and serum was collected on days 0, 7, 10, 14, 21, 28, 31, and 35 for the TNP5-KLH immunizations, and on days 0, 7, 10, 14, 28, 38, and 42 for the NP20-CG immunizations. TNP-specific IgM, IgG1, IgE, IgG2a, IgG2b, IgG3, and IgA antibody titers were assayed by enzyme-linked immunosorbent assay (ELISA)42 (limit of detection 10 ng/mL). NP-specific λ-bearing and IgG1 antibody titers were assayed by ELISA43 (limit of detection 64 ng/mL). For immunization with T-cell–independent type 2 (TI-2) polysaccharide antigens, 8- to 10-week-old mice were immunized intraperitoneally with 50 μg of α1→3 dextran or 10 μg of 4-hydroxy-3-nitrophenylacetyl conjugated to Ficoll (NP27-Ficoll). Mice were bled, and serum was collected on days 0 and 7. The titers of λ-bearing α1→3 dextran-specific serum antibody were determined by ELISA,44 with the modification that the secondary goat antimouse antibody was conjugated to horseradish peroxidase (1:1,000; Southern Biotechnology Associates Inc, Birmingham, AL). The titers of λ-bearing NP-specific serum antibody were determined by ELISA.43
RESULTS
Establishment of CD38-deficient mice and analysis of NAD+ glycohydrolase activity.
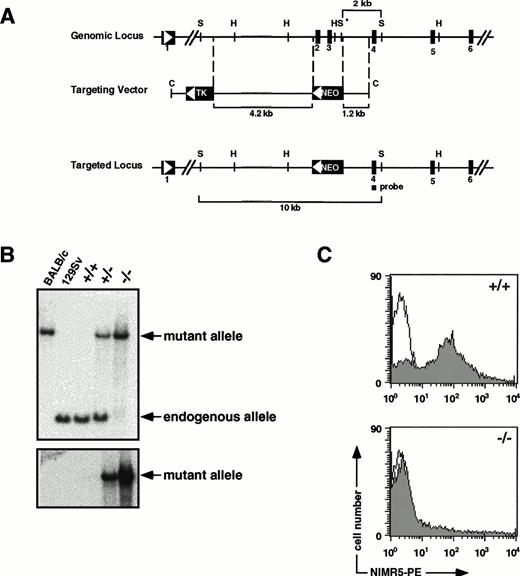
Homologous recombination in ES cells resulted in two ES clones in which exons encoding the putative active site for CD38 NAD+hydrolysis activity45 were replaced by the neomycin resistance gene (Fig 1A and B). Resultant CD38−/− mice lacked CD38-specific mRNA transcripts (data not shown) and immunoreactive CD38 (Fig 1C). In addition, B cells from these mice were unresponsive to the proliferative effects of anti-CD38 antibodies (data not shown). CD38−/− mice were comparable with CD38+/+ littermate controls in appearance and behavior and were capable of living to at least 8 months of age without the development of overt histological or pathological abnormalities.
Generation of CD38 gene-targeted mice. (A) Schematic diagram of the CD38 genomic locus, targeting vector, and targeted locus. Exons, lengths of regions of CD38 homology, lengths of diagnostic restriction fragments, and the position of the exon 4-specific probe are indicated. Restriction enzyme sites are indicated (H, HindIII; C, Cla I; S, Sac I; S*,Sac I polymorphism between the 129SvEv and BALB/c strains of mice). Arrows indicate the transcriptional orientation of the CD38, HSV-TK, and neomycin resistance genes. Homologous recombination resulted in replacement of a 1.6-kb CD38 genomic region that included the putative NAD+ glycohydrolase enzyme catalytic site. (B) Southern blot analysis used for screening genomic DNA from recombinant clones (not shown), and 129Ola × C57BL/6J CD38+/+, CD38+/−, and CD38−/− mice. Probing of blots with a 174-bp polymerase chain reaction–derived exon-4–specific probe (top panel) shows the predicted 2-kb and 10-kb Sac I fragments diagnostic of the CD38 endogenous and mutant alleles, respectively. As a consequence of theSac I polymorphism in the BALB/c locus, a Sac I digest of BALB/c genomic DNA provides a control for the approximate size of the mutant allele fragment. Probing of blots with a neo probe (lower panel) shows hybridization specifically to the 10-kb Sac I fragment characteristic of the mutant allele. (C) FACS staining of total splenocytes with the phycoerythrin (PE)-conjugated rat antimouse CD38 monoclonal antibody NIMR5 (0.5 μg/mL, shaded), or an appropriate PE-conjugated rat IgG2a isotype control (unshaded), was performed according to standard methods.
Generation of CD38 gene-targeted mice. (A) Schematic diagram of the CD38 genomic locus, targeting vector, and targeted locus. Exons, lengths of regions of CD38 homology, lengths of diagnostic restriction fragments, and the position of the exon 4-specific probe are indicated. Restriction enzyme sites are indicated (H, HindIII; C, Cla I; S, Sac I; S*,Sac I polymorphism between the 129SvEv and BALB/c strains of mice). Arrows indicate the transcriptional orientation of the CD38, HSV-TK, and neomycin resistance genes. Homologous recombination resulted in replacement of a 1.6-kb CD38 genomic region that included the putative NAD+ glycohydrolase enzyme catalytic site. (B) Southern blot analysis used for screening genomic DNA from recombinant clones (not shown), and 129Ola × C57BL/6J CD38+/+, CD38+/−, and CD38−/− mice. Probing of blots with a 174-bp polymerase chain reaction–derived exon-4–specific probe (top panel) shows the predicted 2-kb and 10-kb Sac I fragments diagnostic of the CD38 endogenous and mutant alleles, respectively. As a consequence of theSac I polymorphism in the BALB/c locus, a Sac I digest of BALB/c genomic DNA provides a control for the approximate size of the mutant allele fragment. Probing of blots with a neo probe (lower panel) shows hybridization specifically to the 10-kb Sac I fragment characteristic of the mutant allele. (C) FACS staining of total splenocytes with the phycoerythrin (PE)-conjugated rat antimouse CD38 monoclonal antibody NIMR5 (0.5 μg/mL, shaded), or an appropriate PE-conjugated rat IgG2a isotype control (unshaded), was performed according to standard methods.
In an attempt to understand the relationship between the classical NAD+ glycohydrolase activities that have been extensively studied1 and the more recently isolated NAD+glycohydrolases, such as CD38,2,3BP-3/BST-1,16,17 and RT6,46-48 we assessed the status of NAD+ glycohydrolase activity in CD38−/− mice. NAD+ hydrolysis activities in the spleen, liver, and brain, organs known to be rich in classical NAD+ glycohydrolase activity, were determined by using a fluorometric assay with 1, N6-etheno-NAD+ as substrate. The results in Table 1 show that in the spleens of CD38−/−mice the NAD+ glycohydrolase activity was dramatically reduced to less than 1% of the activity detected in the spleens of CD38+/+ littermate controls. The remaining NAD+hydrolysis activity present in the spleens of CD38−/− mice presumably reflects a minor contribution from other NAD+ glycohydrolases previously detected in this tissue.16-18 However, it is unlikely that the residual activity in the spleens of CD38−/−mice is contributed by B lymphocytes since we found no detectable NAD+ glycohydrolase activity remaining in sort purified B220+ splenic B cells from these mice (data not shown). In contrast to the spleen, in the liver and brain of CD38−/− mice no NAD+ glycohydrolase activity was detected. The total lack of NAD+glycohydrolase activity in the liver and brain of these mice is consistent with the fact that CD38 is the only NAD+glycohydrolase that has been detected in these tissues to date.16 18 Taken together, these data provide the first convincing evidence that, at least in the spleen, liver, and brain, CD38 and the classical NAD+ glycohydrolases are likely to be identical, and identify CD38 as the predominant NAD+glycohydrolase in these tissues.
Effect of CD38 deficiency on hematopoiesis in vivo.
Because CD38−/− mice are dramatically depleted of NAD+ glycohydrolase activity, they provide a valuable model for elucidating the physiological role of this class of enzyme, particularly within the hematopoietic compartment where CD38 is widely expressed.15,22 Studies in both the human49-51and murine22 systems have shown that CD38 is a useful marker for identifying populations of hematopoietic progenitor cells. Furthermore, in the murine system, CD38 can be used in combination with other markers to define a population of bone marrow stem cells that possess long-term reconstituting potential. These observations raise the interesting possibility that, in addition to serving as a useful marker for bone marrow progenitor cells, CD38 might play a role in hematopoietic stem cell function. To address this question, competitive repopulation assays were performed whereby irradiated Ly5.1+ recipient mice were competitively repopulated with equal numbers of bone marrow cells derived from Ly5.1+congenic mice, and either Ly5.2+ CD38+/+ or Ly5.2+ CD38−/− mice. The results in Table 2 show that at 12 weeks postreconstitution, bone marrow cells derived from CD38−/− mice had repopulated the peripheral T-cell, B-cell, granulocyte, and macrophage lineages in a manner that was indistinguishable from that observed with bone marrow cells derived from CD38+/+ littermate controls.
Competitive Repopulating Ability of Bone Marrow Derived From CD38+/+ and CD38−/− Mice
| Bone Marrow Donor . | % Donor-Derived (Ly 5.2/total) . | |||
|---|---|---|---|---|
| T . | B . | M . | G . | |
| CD38+/+ | 73 ± 13 | 54 ± 9 | 70 ± 11 | 70 ± 11 |
| CD38−/− | 61 ± 6 | 48 ± 8 | 57 ± 9 | 53 ± 12 |
| Bone Marrow Donor . | % Donor-Derived (Ly 5.2/total) . | |||
|---|---|---|---|---|
| T . | B . | M . | G . | |
| CD38+/+ | 73 ± 13 | 54 ± 9 | 70 ± 11 | 70 ± 11 |
| CD38−/− | 61 ± 6 | 48 ± 8 | 57 ± 9 | 53 ± 12 |
Competitive repopulation assays were performed by mixing 5 × 106 bone marrow cells from individual CD38+/+or CD38−/− Ly5.2 mice (129Ola × C57BL/6J), with 5 × 106 competitor bone marrow cells from C57BL/6J Ly5.1 congenic mice. 50:50 mixtures of bone marrow cells were introduced by intravenous injection into irradiated C57BL/6J Ly5.1 congenic recipients, and competitive repopulation was assessed at 12 weeks postreconstitution. The competitive repopulating ability of donor-derived bone marrow was assessed by determining the percent of donor-derived lineage-specific cells among all cells within that lineage. Cell numbers within the T-cell (T), B-cell (B), macrophage (M), and granulocyte (G) lineages were determined by FACS analysis of peripheral blood from individual recipient mice as described in the Materials and Methods. Data shown represent the mean ± standard deviation of the percent donor reconstitution of three individual mice.
Consistent with these findings, CD38−/− mice exhibited normal peripheral blood cell counts and hematopoietic organ cellularities (data not shown). In addition, flow cytometric analysis of tissues from 4- and 8-week-old CD38−/− mice indicated a normal distribution and ratio of immature B220+IgM− and mature B220+IgM+ B cells in the bone marrow and spleen, as well as B220+CD5+ B-1 B cells in the peritoneal cavity (data not shown). T lymphocyte subpopulations including CD4+CD8+ double positive thymocytes, and CD4+ or CD8+ single positive thymocytes and peripheral T cells were also present in normal numbers and ratios, as were cells of the independent lineage of αβ T-cell receptor (TCR)+CD4−CD8−thymocytes which uniquely express CD3852 (data not shown). Normal numbers of macrophages, granulocytes, and neutrophils were also present in the bone marrow, spleen, and peritoneal cavity of CD38−/− mice (data not shown). Taken together, these data indicate that despite the prevalence of enzymatically active CD38 on a wide range of hematopoietic cells, this ecto-NAD+glycohydrolase does not appear to be required for the development or maintenance of either hematopoietic stem cells or committed lineage-specific cell populations.
In vivo modulation of TD and TI-2 antibody responses in CD38-deficient mice.
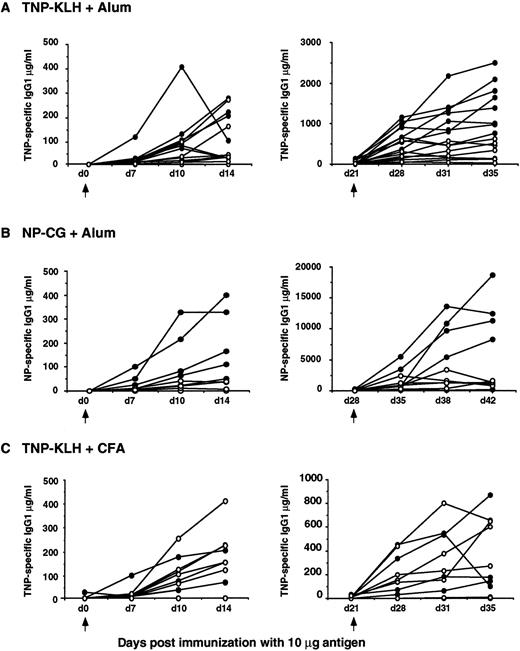
Because CD38 has been implicated as a B lymphocyte coreceptor capable of influencing both the threshold and the level of signaling through the BCR,30 we assessed the immune response of CD38−/− mice after immunization with either major histocompatibility complex (MHC) class II-restricted TD protein antigens, or TI-2 polysaccharide antigens. In response to immunization with 10 μg of the TD antigen TNP5-KLH in alum adjuvant, CD38−/− mice mounted normal hapten-specific IgG2a, IgG2b, IgG3, and IgA responses, but decreased hapten-specific IgM, IgG1, and IgE responses (Fig 2A and data not shown). The most striking defect was in the ability of CD38−/− mice to mount or sustain a secondary hapten-specific IgG1 response, with IgG1 titers consistently remaining at the level observed after a primary immunization (Fig 2A, right panel). Immunization with the same dose of a second TD antigen, NP20-CG in alum adjuvant, produced similar results (Fig2B). In addition, the impaired hapten-specific IgG1 response to both TNP5-KLH and NP20-CG were confirmed in CD38−/− mice derived from a second, independently targeted ES clone (data not shown).
Immune responses of 129Ola × C57BL/6J F3 CD38−/− mice (open symbols) and CD38+/+ littermate controls (closed symbols) to TD antigens. Titers of hapten-specific IgG1 serum antibody at various time points after a primary (left), and secondary (right) immunization with 10 μg alum-precipitated TNP5-KLH (A), 10 μg alum-precipitated NP20-CG (B), or 10 μg CFA-precipitated TNP5-KLH (C). Arrows indicate the time of the primary and secondary immunizations. The data shown are representative of one of eight TNP5-KLH in alum immunization experiments, one of two NP20-CG in alum immunization experiments, and one of three TNP5-KLH in CFA immunization experiments, in which each experiment included five to eight mice per group.
Immune responses of 129Ola × C57BL/6J F3 CD38−/− mice (open symbols) and CD38+/+ littermate controls (closed symbols) to TD antigens. Titers of hapten-specific IgG1 serum antibody at various time points after a primary (left), and secondary (right) immunization with 10 μg alum-precipitated TNP5-KLH (A), 10 μg alum-precipitated NP20-CG (B), or 10 μg CFA-precipitated TNP5-KLH (C). Arrows indicate the time of the primary and secondary immunizations. The data shown are representative of one of eight TNP5-KLH in alum immunization experiments, one of two NP20-CG in alum immunization experiments, and one of three TNP5-KLH in CFA immunization experiments, in which each experiment included five to eight mice per group.
The impaired TD antibody responses in CD38−/−mice could reflect impaired B-cell class switching, decreased B-cell responsiveness, insufficient T-cell priming/activation, inefficient antigen presentation, or some combination of these possibilities. However, serum immunoglobulin isotype levels were normal in CD38−/− mice (data not shown), suggesting that B lymphocytes from these mice are not generally impaired in their ability to undergo immunoglobulin class switching. In addition, B cells from CD38−/− mice, when stimulated in vitro with either lipopolysaccharide, anti-CD40 antibodies, or anti-immunoglobulin antibodies, proliferated and upregulated expression of MHC class II, CD80, and CD86 (data not shown). T cells from CD38−/− mice also proliferated in vitro in response to either anti-CD3, or anti-CD3 plus anti-CD28 antibody stimulation (data not shown). These data indicate that both B and T lymphocytes from CD38−/− mice respond normally to in vitro polyclonal activation signals, as well as to contact-dependent signals important for cognate T- or B-cell interactions.
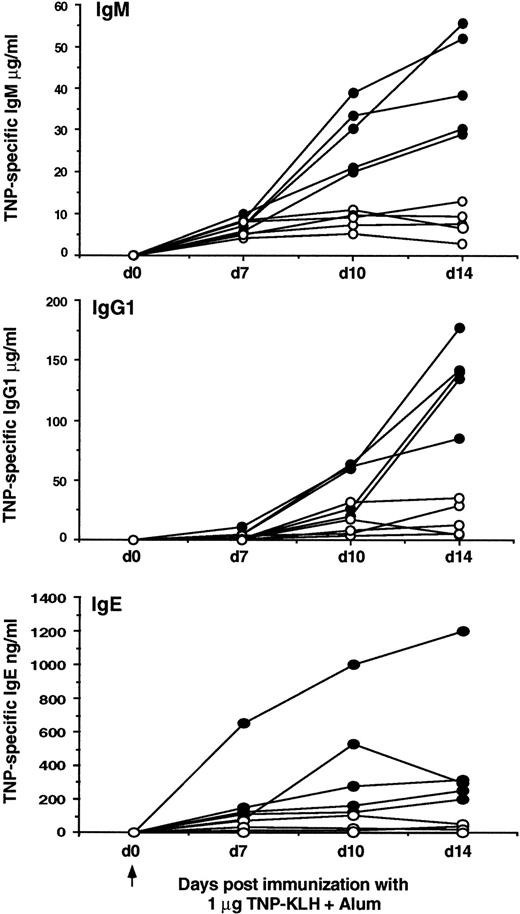
As an alternative consideration, the impaired antibody responses observed in CD38-deficient mice may reflect an alteration in sensitivity to BCR signaling, consistent with our data that CD38 serves as a coreceptor for the BCR.30 To test this possibility, the same types of immunization experiments described previously were performed by using TNP5-KLH in Freund’s adjuvant, which is a much more potent adjuvant than alum.53 Under these experimental conditions we found no differences in the primary or secondary antibody responses of CD38−/− mice compared with CD38+/+ littermate controls (Fig 2C). In one experiment in which mice were similarly immunized with NP20-CG in Freund’s adjuvant, we found that the primary antibody responses of CD38−/− mice were also not significantly different than that observed with CD38+/+littermate controls (data not shown). To pursue this further, we next measured the response of CD38−/− mice to immunization with decreasing amounts of TNP5-KLH in alum. Interestingly, the hapten-specific antibody responses were even more impaired after immunization with 1 μg of TNP5-KLH in alum compared with that observed after immunization with 10 μg of antigen. As shown in Fig 3, immunization with a lower dose of antigen now revealed marked deficiencies in the ability of CD38−/− mice to mount primary hapten-specific IgM, IgG1, and IgE responses. Consistent with the results shown in Fig 2, these mice failed to mount significant secondary hapten-specific antibody responses to either 1 μg or 10 μg of antigen (data not shown). Taken together, these results indicate that, at least in response to the antigens tested, immune responses in CD38−/− mice are critically dependent on the dose and the strength of the immunizing antigen.
Immune responses of 129Ola × C57BL/6J F3 CD38−/− mice (open symbols) and CD38+/+littermate controls (closed symbols) to a limiting dose of the TD antigen TNP5-KLH in alum. In two of the eight TNP5-KLH in alum immunization experiments described in Fig2, the hapten-specific responses to different doses of antigen were compared (1 μg compared with 10 μg). The data shown are representative of these experiments, and illustrate the titers of hapten-specific IgM, IgG1, and IgE serum antibody at various time points after a primary immunization with 1 μg alum-precipitated TNP5-KLH (10 μg, data not shown). Arrow indicates the time of primary immunization.
Immune responses of 129Ola × C57BL/6J F3 CD38−/− mice (open symbols) and CD38+/+littermate controls (closed symbols) to a limiting dose of the TD antigen TNP5-KLH in alum. In two of the eight TNP5-KLH in alum immunization experiments described in Fig2, the hapten-specific responses to different doses of antigen were compared (1 μg compared with 10 μg). The data shown are representative of these experiments, and illustrate the titers of hapten-specific IgM, IgG1, and IgE serum antibody at various time points after a primary immunization with 1 μg alum-precipitated TNP5-KLH (10 μg, data not shown). Arrow indicates the time of primary immunization.
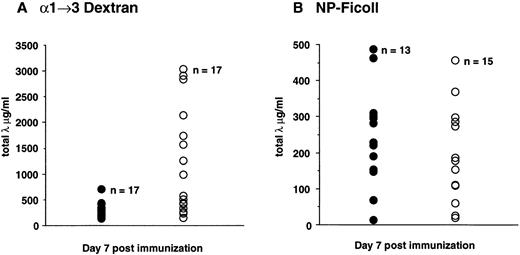
Because the loss of CD38 resulted in impaired TD immune responses, we next examined the role of CD38 in TI-2 responses. In contrast to their reduced antibody responses to TD antigens, CD38−/− mice showed elevated antibody responses to the TI-2 antigen α1→3 dextran. In fact, immunization of CD38−/− mice with α1→3 dextran produced an augmented antigen-specific total λ response that was, on average, fivefold greater than that observed in CD38+/+littermate controls (Fig 4A). Although this TI-2 response was significantly increased in CD38−/− mice, the response to a second TI-2 antigen, NP27-Ficoll was unaltered (Fig 4B). One possible explanation for this difference could be that while the NP27-Ficoll response is mediated by conventional B cells, the α1→3 dextran response is mediated by B-1 B cells.54 55 However, CD38−/− mice showed no difference in absolute numbers or surface marker phenotype of B-1 B cells compared with CD38+/+ littermate controls (data not shown). Moreover, not all B-1 B-cell responses were augmented in these mice because CD38−/− mice showed no upregulation of circulating autoantibody levels to antigens such as double-stranded DNA even at 6 months of age (data not shown). Taken together, these data suggest that CD38 plays a complex role in regulating humoral immune responses in vivo.
Immune responses of 129Ola × C57BL/6J F3 CD38−/− mice (open symbols) and CD38+/+littermate controls (closed symbols) to TI-2 antigens. Titers of λ-bearing 1→3 dextran-specific serum antibody (A), or λ-bearing NP-specific serum antibody (B) in individual mice at day 7 after immunization with 50 μg of 1→3 dextran, or 10 μg of NP27-Ficoll, respectively. The 1→3 dextran data shown represent the composite results from four independent immunization experiments and include 17 CD38−/− mice (mean = 1131.1 μg/mL) and 17 CD38+/+ littermate controls (mean = 247.3 μg/mL). The NP27-Ficoll data shown represent the composite results from three independent immunization experiments and include 15 CD38−/− mice (mean = 172.4 μg/mL), and 13 CD38+/+ littermate controls (mean = 233.9 μg/mL).
Immune responses of 129Ola × C57BL/6J F3 CD38−/− mice (open symbols) and CD38+/+littermate controls (closed symbols) to TI-2 antigens. Titers of λ-bearing 1→3 dextran-specific serum antibody (A), or λ-bearing NP-specific serum antibody (B) in individual mice at day 7 after immunization with 50 μg of 1→3 dextran, or 10 μg of NP27-Ficoll, respectively. The 1→3 dextran data shown represent the composite results from four independent immunization experiments and include 17 CD38−/− mice (mean = 1131.1 μg/mL) and 17 CD38+/+ littermate controls (mean = 247.3 μg/mL). The NP27-Ficoll data shown represent the composite results from three independent immunization experiments and include 15 CD38−/− mice (mean = 172.4 μg/mL), and 13 CD38+/+ littermate controls (mean = 233.9 μg/mL).
DISCUSSION
In the present study we describe the generation and analysis of a mouse knockout model for the ecto-NAD+ glycohydrolase CD38. Our analysis of these CD38−/− mice has led to two principal observations. First, these mice have enabled us to determine that CD38 and the classical NAD+ glycohydrolases that have been studied for many years,1 but whose function has remained largely unknown, are likely identical molecules. Secondly, we show that one prominent phenotype associated with CD38 deficiency is a marked alteration in humoral immune responses to both TD and TI-2 antigens. Although one might have predicted a more critical role for this widely in vivo distributed, multifunctional NAD+glycohydrolase, these findings are nonetheless consistent with the recognized role of CD38 as an immunoregulatory molecule and support our previous in vitro observation that CD38 can act as a coreceptor for the BCR, in a manner similar to that observed for other B-cell coreceptors such as CD19.32
Several observations would have predicted an in vivo role for CD38 in bone marrow hematopoiesis and B lymphopoiesis. CD38 is widely expressed on cells of hematopoietic origin, including hematopoietic stem cells, and studies in both the human49-51 and murine22systems have used CD38 as a phenotypic marker for different hematopoietic progenitor subsets. In addition, functional experiments using anti-CD38 antibodies have shown that signaling through CD38 can inhibit human B lymphopoiesis and expansion.28 However, analysis of CD38−/− mice has shown that this ecto-NAD+ glycohydrolase is not required for the development or maintenance of either hematopoietic stem cells or committed lineage-specific cell populations. The competitive repopulation experiments shown in Table 2 showed that bone marrow derived from CD38−/− mice exhibited normal repopulating ability. Consistent with these findings, CD38−/− mice exhibited a normal distribution and ratio of B- and T-lymphocyte subpopulations, as well as normal numbers of granulocytes, macrophages, and neutrophils (data not shown). The fact that the hematopoietic compartment has remained unaltered in CD38-deficient mice suggests that CD38 is not critical to hematopoiesis or lymphopoiesis in mice. However, it is equally possible that in CD38−/− mice additional CD38-like NAD+ glycohydrolases, such as the bone marrow stromal cell surface molecule BP-3/BST-1,16 17 might compensate for CD38 function in vivo. Given that it is still unclear whether the enzymatic properties of molecules such as CD38 or BP-3/BST-1 are required for their in vivo functional activity, it is too early to predict whether such a functional compensation may be important to the maintenance of a normal hematopoietic compartment. The generation of mice carrying targeted mutations in both the CD38 and BP-3/BST-1 genes should enable us to address this issue.
In contrast, CD38 does appear to play a functional role in mature lymphocytes. CD38−/− mice exhibited marked deficiencies in antibody responses to TD protein antigens, and augmented antibody responses to at least one TI-2 polysaccharide antigen. In response to two separate TD antigens, CD38−/− mice failed to mount normal hapten-specific IgG1 responses, and to a lesser extent IgM and IgE responses (Figs 2 and 3 and data not shown), although the serum immunoglobulin levels in these mice were normal (data not shown). These data suggest that in vivo signals delivered through CD38 are not critical for the maintenance of normal serum immunoglobulin, but instead are important for maintaining antigen-driven responses of specific immunoglobulin isotypes. Interestingly, recent experiments from Yasue et al33 showed that CD38-mediated signaling in B cells results in the preferential induction of specific immunoglobulin isotypes. In this study, it was shown that ligation of murine splenic B cells with anti-CD38 antibodies and IL-5 induced a marked induction of IgM and IgG1 isotypes but not IgA or IgG2a. Because a similar stimulation of B cells with anti-CD38 and interleukin-4 (IL-4) did not induce significant IgG1 production, it was suggested that there might be two independent pathways for polyclonal IgG1 production: one that is dependent on IL-4 and a second that is dependent on CD38 and IL-5.33 Based on these observations, it is possible that the diminished hapten-specific IgM and IgG1 responses observed in CD38−/− mice may be caused by the loss of a CD38-dependent IL-5 signaling pathway.
The deficiencies in hapten-specific antibody responses observed in CD38−/− mice were apparent when the immunizing antigen was presented in alum adjuvant but not when it was presented in the stronger complete Freund’s adjuvant, and these deficiencies were influenced by the dose of the immunizing antigen (Figs 2 and 3). These observations are consistent with our recent in vitro findings that coengagement of CD38 and the BCR can lower the amount of antigen receptor crosslinking required to signal through the BCR.30Based on these data we would propose that, at least in response to the TD antigens tested, CD38 deficiency leads to a reduced sensitivity to signals delivered through the BCR, resulting in a requirement for a higher antigen dose to induce B-cell activation. The fact that CD38−/− mice mounted normal hapten-specific antibody responses to TD antigens in Freund’s adjuvant (Fig 2 and data not shown), and to the TI-2 antigen NP27-Ficoll (Fig 4B) is also consistent with this hypothesis. B cells that have been activated by strong adjuvants or by antigens capable of extensive BCR crosslinking, such as polysaccharide TI-2 antigens, may not require additional CD38-mediated costimulatory signals. If this hypothesis is correct, one might expect that CD38-deficient mice should mount normal antigen-specific responses to all antigens that induce extensive BCR crosslinking and activation. However, immunization of CD38−/− mice with a second TI-2 antigen, α1→3 dextran, resulted in an augmented antigen-specific response (Fig 4A). One striking difference between the immune response to α1→3 dextran, and the immune response to TD antigens or the TI-2 antigen NP27-Ficoll is that the response to α1→3 dextran is mediated by B-1 B cells, whereas immune responses to the other antigens are controlled by conventional B cells.54,55 Therefore, it is possible that CD38 performs functionally distinct roles on conventional versus B-1 B cells. For example, on conventional B cells CD38 may function to augment signaling through the BCR, whereas on B-1 B cells the function of CD38 may be to downmodulate signals through this same receptor complex. In vitro experiments on mature splenic B cells have in fact shown that while coengagement of CD38 and the BCR can augment B-cell activation, independent ligation of these receptors results in a depressed response.30,31 In addition, CD38-mediated signaling can result in different functional responses on conventional and B-1 B cells, as evidenced by the fact that, although anti-CD38 antibodies provide a potent growth costimulatory signal for conventional B cells, this is not the case for B-1 B cells.56 B-1 B cells also fail to proliferate in response to stimulation through the BCR,56 57 suggesting that signaling through CD38 and the BCR may be coordinately controlled on B-1 B cells.
In any case, delineating the events associated with CD38-mediated B-cell signaling will be critical to understanding the mechanism(s) by which CD38 influences B lymphocyte responses. A number of laboratories have now shown that engagement of CD38 by specific antibodies can induce tyrosine phosphorylation and activation of intracellular signal transduction mediators.33-35 Interestingly, many of the proteins that are phosphorylated upon CD38 ligation are also phosphorylated after BCR engagement,33,36,58-60 suggesting that there may be extensive crosstalk between CD38 and the BCR. Of particular interest is the recent finding of Kitanaka et al,36 that ligation of CD38 on human immature B cells induces the tyrosine phosphorylation of CD19 and the subsequent association of CD19 with lyn and PI3-kinase. Based on these observations, it was suggested that CD19 may function as a component of the CD38-mediated signaling pathway, providing CD38 with access to intracellular tyrosine kinase cascades. If this hypothesis is correct, it suggests that CD38 may modulate mature B lymphocyte responses by influencing the signaling pathway of a second B-cell coreceptor such as CD19. The fact that CD19−/− mice had a similar but more profound impairment in humoral immune responsiveness than that observed in CD38−/− mice would be supportive of this notion.61 62
Because antibody responses to both TD and TI-2 antigens result from complex interactions between multiple cell types, many of which express CD38, further experiments will be required to delineate the exact cellular mechanism(s) responsible for the impaired humoral immunity in these mice. Although there is strong supporting evidence that the compromised immune responses observed in CD38−/− mice results from a loss of CD38-mediated BCR coreceptor activity, it is also possible that these compromised responses result from altered T-cell and/or APC function. The fact that CD38-mediated signaling can induce cytokine production by human peripheral blood mononuclear cells,27enhance murine macrophage APC function (N. Solvason et al, manuscript in preparation), and induce the activation of tyrosine kinases normally associated with the TCR35 is at least suggestive of a role for CD38 in modulating additional responses important for TD and TI-2 antibody responses. Whether CD38 might serve an analogous function on T cells as it does on B cells, and act as a coreceptor for signaling through the TCR remains to be determined. The fact that the immunoglobulin isotypes most severely affected in the TD responses of these mice (ie, IgG1 and IgE) are those normally supported by the Th2 subpopulation of helper T lymphocytes63 might also suggest that the observed phenotype in these mice can be explained by a failure to induce or maintain antigen-specific Th2 cell responses. However, data from preliminary experiments has shown that CD38−/− mice produced normal responses following sensitization with either Nippostrongylus brasiliensis or Aspergillus fumigatus (data not shown), responses that are normally Th2 T-helper–cell mediated. Alternatively, it remains a possibility that the skewing towards deficiencies in antigen-specific IgG1 and IgE isotype responses may simply reflect the dominance of these isotypes after immunization with alum adjuvant.
Although our study clearly shows that a loss of CD38 impacts on immune responses to experimental antigens, it is unclear whether this defect is caused by a loss of CD38-associated ectoenzyme activity or to some other function mediated by CD38. Determining the relationship between the enzymatic activities, and the in vivo functional activities of CD38 will be one focus of future studies. It is also clear from our data that CD38 is the primary, if not the only, NAD+glycohydrolase in the liver and brain of mice. Thus, whereas our studies have focused primarily on the role of CD38 in hematopoiesis and immune regulation, it will also be of interest to evaluate CD38-deficient mice with respect to the physiological functions of other organ systems that express CD38 enzymatic activity, such as the pancreas, liver, and brain.
ACKNOWLEDGMENT
We gratefully acknowledge Tom McNeil for microinjection and blastocyst implantation, Drs Klaus Rajewsky and Werner Müller for the NP20-CG and NP27-Ficoll reagents, Dr John Kearney for the α1→3 dextran reagents, Dr Robert Coffman for the TNP5-KLH reagents, and Nisha Kabra for her work on the construction of the CD38 gene-targeting vector.
DNAX Research Institute is fully funded by Schering Plough Corporation.
Address reprint requests to Debra A. Cockayne, PhD, Center for Biological Research, Neurobiology Unit, Roche Bioscience, 3401 Hillview Ave, Palo Alto, CA 94304; e-mail: debra.cockayne@roche.com.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked "advertisement" is accordance with 18 U.S.C. section 1734 solely to indicate this fact.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal