Abstract
Although thrombocytopenia associated with the use of histamine H2 receptor (H2R) antagonists has been described, a drug-dependent, platelet-reactive antibody has not previously been identified in such cases. We studied serum from a patient who developed acute, severe thrombocytopenia after exposure to the H2 receptor antagonist, ranitidine, and identified an antibody that reacted with normal platelets in the presence of this drug at pharmacologic concentrations. In flow cytometric and immunoprecipitation studies, the antibody was shown to be specific for the glycoprotein Ib/IX complex (GPIb/IX). From the pattern of monoclonal antibody (MoAb) inhibition and the reactions of antibody with Chinese hamster ovary (CHO) cells transfected with GPIX and GPIbβ, we found that the patient's antibody is specific for an epitope on GPIX close to, or identical with a site recognized by the MoAb SZ1 that is a common target for antibodies induced by quinine and quinidine, drugs structurally unrelated to ranitidine. These findings provide evidence that immune thrombocytopenia can be caused by sensitivity to an H2 R antagonist and suggest that the SZ1 binding site on GPIX may be a common target for drug-induced antibodies. Further studies of the epitope for which SZ1 is specific may provide clues to the mechanism(s) by which drugs promote tight binding of antibody to a membrane glycoprotein and cause platelet destruction in patients with drug sensitivity.
HUNDREDS OF DIFFERENT medications have been implicated as triggers for acute, immunologically mediated thrombocytopenia.1-3 In some instances, antibodies that bind to normal platelets in the presence of drug have been convincingly demonstrated in the laboratory, providing strong evidence that thrombocytopenia was, in fact, caused by drug sensitivity. Medications for which this type of evidence has been obtained include the cinchona alkaloids, quinidine and quinine,4,5 the sulfonamide antibiotics, sulfamethoxazole and sulfisoxazole,6 and others.2,3 For many drugs implicated as causes of drug-induced thrombocytopenia (DITP), drug-dependent, platelet-reactive antibodies have not been found, however, leaving open the question of whether thrombocytopenia was actually drug-induced except in rare instances in which a causative role for drug was documented by accidental or deliberate rechallenge of an affected patient.2 The H2 histamine receptor (H2R) antagonists ranitidine, famotidine, and cimetidine, are among the medications implicated in drug-induced immune thrombocytopenia without convincing laboratory documentation.7-9 We recently encountered a patient who developed acute, severe thrombocytopenia while taking the H2R antagonist ranitidine in whom a ranitidine-dependent antibody reactive with normal platelets was detected by in vitro testing. Because several studies have suggested that human platelets may express histamine receptors,10 11 we wondered whether this antibody was specific for ranitidine bound to an H2R and performed studies to identify the platelet membrane component for which it is specific. We were unable to identify a specific platelet H2R as the target, but found that the antibody recognized platelet glycoprotein IX at a site identical with or very close to one that appears to be a favored target for antibodies associated with quinidine- and quinine-induced thrombocytopenia.
MATERIALS AND METHODS
Case Report
A 68-year-old woman (JH) had taken ranitidine intermittently for about 3 years for gastric distress. Six months after her last known exposure to ranitidine, after eating dinner at a Chinese restaurant, she took a single 150 mg tablet. About 1 hour later, she noted a nonpruritic rash on her lower extremities. The next morning, she sought medical help and was found to have an extensive petechial rash over the upper and lower extremities and the abdomen. Blood studies showed a platelet level of 7,000/μL, hemoglobin 12.1 g/dL and white blood cell count (WBC) 5,500 with normal differential. She was given prednisone, 50 mg/d, and her platelet count returned to normal in about 4 days. She took no ranitidine after this episode, and her platelet count has remained normal.
The patient had one previous episode of severe thrombocytopenia (platelets 5,000/μL) about 18 months previously, at which time she had been taking amitriptyline, atenolol, propoxyphene, and acetaminophen. These medications were discontinued and platelets returned to normal in a few days, but no studies for drug-dependent antibodies were done at that time. She was uncertain whether she had taken rantidine immediately before this incident.
Reagents
Monoclonal antibodies (MoAbs) used were AP1 and MBC 142.11 (anti-GPIbα), AP2 (anti-GPIIb/IIIa complex), AP3 (anti-GPIIIa) all from the Monoclonal Antibody Core Laboratory of the Blood Research Institute, Milwaukee, WI; Tab (anti-GPIIb) from Dr Rodger McEver, University of Oklahoma (Oklahoma City, OK); GR-P and FMC 25 (anti-GPIX) from Serotech, Inc (Harlan, Indianapolis, IN); SZ1 (anti-GPIX) from Immunotech, Inc (Chicago, IL); and 1D9 (anti-GPV), a gift from Dr Kingo Fujimara, Hiroshima, Japan. Purified glycocalicin was provided by Dr Philip Kroner of the Blood Research Institute. Chinese hamster ovary (CHO) cells stably transfected with GPIX and GPIbβ were obtained from Dr Jose Lopez (Houston, TX), and have been described previously.12 Antibodies from two patients who experienced quinine-induced immune thrombocytopenia (Q1 and Q2) had previously been shown to contain high titer, drug-dependent antibodies specific for the GPIb/IX complex together with weaker antibodies specific for GPIIb/IIIa.13 At the serum dilutions used in these studies, the latter antibodies were not detectable.
Platelet Samples
Platelets were isolated from EDTA-anticoagulated blood of normal donors by differential centrifugation and three washes in phosphate-buffered saline (PBS), pH 6.8 containing 2 mmol/L EDTA and 0.25% bovine serum albumin (BSA). Platelets from a patient with the Bernard-Soulier syndrome were recovered from platelet-rich plasma (PRP) after overnight gravity sedimentation of red blood cells. The molecular basis of the genetic defect and the extent to which GPIb/IX/V is expressed on platelets from this patient have been reported previously.14 Platelets from a patient with Type I Glanzmann's thrombasthenia containing no detectable amounts of glycoproteins IIb and IIIa were obtained from a frozen repository where they had been stored at −80°C in 5% dimethylsulfoxide.6 Informed consent, as approved by the Human Research Review Committee of The Blood Center of Southeastern Wisconsin, was obtained for all studies.
Flow Cytometry
Drug-dependent binding of antibody to target platelets was determined by flow cytometry, as described previously.5 In a typical experiment, 5 × 106 platelets in PBS-BSA, 35 μL patient serum or plasma, and 5 μL of drug (10 mmol/L) were incubated in a total volume of 50 μL in the wells of a 96-well microtiter tray (Falcon; Fisher, Itasca, IL). After incubation for 40 minutes at room temperature, the plates were centrifuged at 2,000g for 4 minutes and the supernatant fluid was discarded by decantation. The platelet buttons were washed three times in 200 μL PBS-BSA and were resuspended in 50 μL of fluorescein isothiocyanate (FITC)-labeled goat F(ab')2 antihuman IgG (H+L) (Jackson Laboratories, West Grove, PA) diluted 1:80 in PBS. The mixture was incubated for 30 minutes at room temperature in the dark and was then suspended in 0.5 mL of the same buffer. Platelet-bound fluorescence was analyzed by flow cytometry (FACStar; Becton-Dickinson, Mountain View, CA). In some experiments, FITC-labeled [goat F(ab')2 ] anti-IgA, IgM, or IgG (Jackson Laboratories) were used as secondary probes. For detection of platelet-associated MoAbs, the second incubation was performed with FITC-labeled (goat) antimouse IgG (Jackson Laboratories).
Flow cytometry experiments on CHO cells were performed as described by Lopez et al12 with minor modifications. Briefly, 5 × 105 cells, detached from tissue culture flasks with 0.54 mmol/L of EDTA were processed as described for the platelet studies. After incubation with the secondary probe, the CHO cells were kept at 4°C in the dark until analyses were performed.
Inhibition of antibody binding by MoAbs.
The binding site for the drug-dependent antibody detected in serum from JH was studied with platelets preincubated with selected MoAbs specific for GPIX, GPIbα, GPV, and GPIIb/IIIa. In these studies, the MoAbs were used at a concentration of 2.0 μg/mL, found in preliminary studies to be in excess of the amount required to achieve saturation of their targets.
Immunoprecipitation and Immunoblotting
The techniques used have been described previously.6 13 In a typical experiment, 108 platelets were incubated for 1 hour at room temperature with 100 μL plasma or serum containing antibody in the presence or absence of 1 mmol/L drug. The sensitized platelets were then washed three times in PBS-EDTA-BSA containing drug at the same concentration as the primary mixture. Washed platelets were solubilized in 200 μL, 1% Triton X-100, in 25 mmol/L Tris-buffered saline (TBS), pH 7.8, containing a protease inhibitor cocktail (Boehringer Mannheim, Indianapolis, IN). The mixture was incubated for 30 minutes in an ice bath, centrifuged at 16,000g for 15 minutes at 4°C, and the supernatant (platelet lysate) was aspirated. Protein A-Sepharose CL-4 beads (Pharmacia, Piscataway, NJ) were preincubated in saline containing 1% BSA and 0.05% Tween-20 for 30 minutes at room temperature, washed, and resuspended at a 50% concentration. A 50-μL aliquot of beads was then incubated with the platelet lysate for 2 hours at 4°C, washed four times in PBS containing 0.5% Triton X-100 with or without 1 mmol/L ranitidine, and resuspended in Laemmli sample buffer. The samples were then boiled for 5 minutes and the eluted proteins were subjected to sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) in a 5% to 15% gel gradient under reducing or nonreducing conditions. The gel was then equilibrated in TRIS-glycine-methanol buffer, pH 8.3, and transferred to a PDVF microporous membrane (Millipore, Bedford, MA) using a Genie electrophoretic blotter (Idea Scientific, Minneapolis, MN). The membrane was blocked with 2.5% BSA in washing solution (25 mmol/L TBS, 0.75% Tween-20, pH 7.3) and incubated with MoAbs specific for platelet membrane glycoproteins. After washing, the membrane was incubated with horseradish peroxidase-labeled, goat antimouse IgG (Jackson Laboratories) for 40 minutes at room temperature, washed again, and coated with chemiluminescence substrate mixture (ECL, Amersham, Des Plaines, IL). The plastic-wrapped membrane was covered with a sheet of x-ray film (Hyperfilm, Amersham), which was exposed for various lengths of time and then developed.
RESULTS
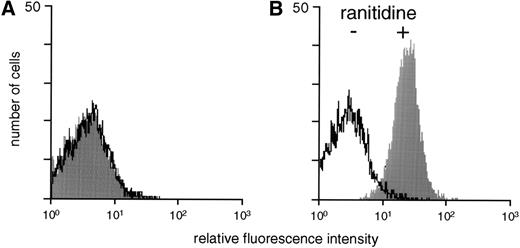
The patient's serum contained a ranitidine-dependent IgG antibody that reacted with normal platelets at pharmacologic concentrations of drug.
As shown in Fig 1, JH plasma, but not normal plasma, reacted with normal target platelets in the presence, but not in the absence, of ranitidine. Using Ig class-specific probes, positive reactions were obtained with anti-IgG, but not with anti-IgA or anti-IgM. Binding of the antibody to platelets occurred at concentrations of ranitidine as low as 0.3 μmol/L, significantly less than the peak level of ranitidine (about 1.3 μmol/L) achieved after ingestion of a standard 150-mg dose of drug15 (data not shown). There was no reduction in IgG binding at the highest concentration of ranitidine used (3.0 mmol/L), ie, no evidence of hapten-inhibition. The antibody failed to react with washed erythrocytes or peripheral blood mononuclear cells in the presence or absence of drug (data not shown). Platelets preincubated with 1 mmol/L ranitidine and washed three times in the absence of drug still reacted weakly with the patient's plasma, but not with normal plasma, in contrast to the behavior of quinine and quinidine-dependent, platelet reactive antibodies, which failed to react with platelets pretreated with drug and washed in its absence (data not shown.) These findings suggested that ranitidine binds tightly to one or more platelet membrane components to create epitope(s) for which the antibody is specific.
Reactions of control serum (A) and serum from patient JH (B) with normal platelets in the presence (+) and absence (−) of 1.0 mmol/L ranitidine.
Reactions of control serum (A) and serum from patient JH (B) with normal platelets in the presence (+) and absence (−) of 1.0 mmol/L ranitidine.
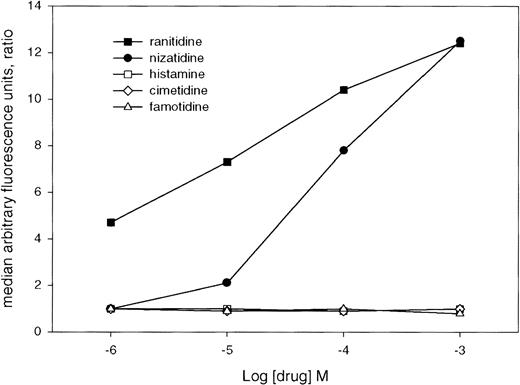
Nizatidine, but not other H2 receptor antagonists, also promoted binding of antibody to platelets.
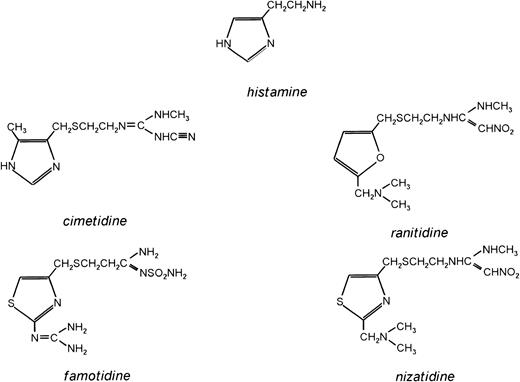
The structure of ranitidine, three other H2 R antagonists used clinically, and histamine are shown in Fig 2. The patient's antibody reacted with normal platelets in the presence of nizatidine, but only at concentrations of drug about one log higher than the amounts of ranitidine required to promote equivalent antibody binding (Fig 3). No reactions were obtained with famotidine, cimetidine, or histamine at a wide range of concentrations. Famotidine binds more tightly to H2 R (dissociation constant 17 nmol/L) than ranitidine (dissociation constant 200 nmol/L),16 but preincubation of platelets with 1.0 mmol/L famotidine had no significant effect on ranitidine-dependent binding of antibody to platelets at concentrations of ranitidine as low as 1.0 μmol/L . This finding argued against the possibility that ranitidine reacted with a conventional H2 receptor on the platelet surface to create a site for antibody binding.
The structures of histamine and four H2R antagonists approved for use in the US and many European countries.
The structures of histamine and four H2R antagonists approved for use in the US and many European countries.
Binding of antibody from patient JH to normal platelets at various concentrations of histamine, ranitidine, and three other H2R antagonists. Ratio of the fluorescent signal obtained in the presence of drug to that obtained in its absence is shown on the ordinate. Of the compounds tested other than ranitidine, only nizatidine promoted antibody binding. Values shown are the averages of duplicate determinations, which did not vary from one another by more than 5%.
Binding of antibody from patient JH to normal platelets at various concentrations of histamine, ranitidine, and three other H2R antagonists. Ratio of the fluorescent signal obtained in the presence of drug to that obtained in its absence is shown on the ordinate. Of the compounds tested other than ranitidine, only nizatidine promoted antibody binding. Values shown are the averages of duplicate determinations, which did not vary from one another by more than 5%.
Specificity of the antibody for the GPIb/IX/V complex was demonstrated by flow cytometry, immunoprecipitation, and MoAb inhibition.
In flow cytometry, the patient's serum reacted as strongly with platelets from a patient with Type I Glanzmann's thrombasthenia that expressed no detectible amounts of GPIIb or GPIIIa as with normal platelets. However, only weak reactions were obtained with platelets from a patient with the Bernard-Soulier syndrome, despite their larger than normal size. Platelets from this patient are known to express the GPIb/IX/V complex at levels about 25% to 40% of normal.14These findings suggested that antibody JH recognized a component of the GPIb/IX/V complex in the presence of ranitidine. Drug-dependent binding of the antibody to normal platelets was unaffected by prior incubation of antibody with the glycocalicin fragment of GPIbα at 2 μg/mL, at which concentration binding of the glycocalicin-specific monoclonal MBC 142.11, also used at 2.0 μg/mL, was totally inhibited (data not shown). This finding argued against the possibility that GPIbα was the target for antibody JH.
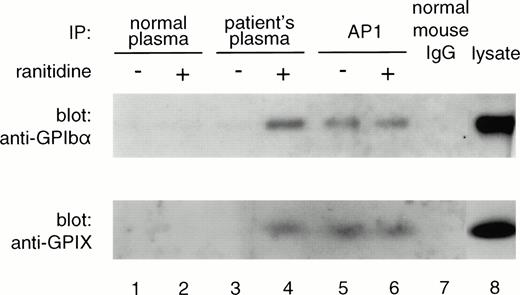
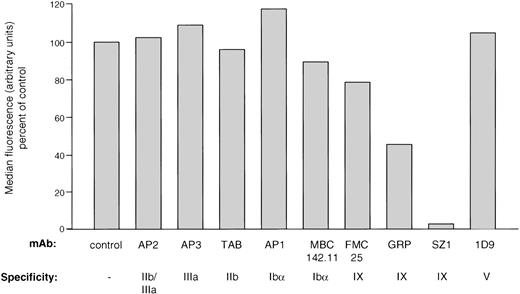
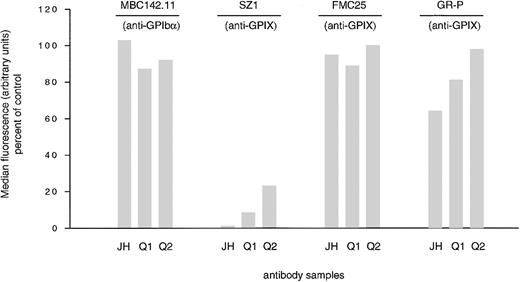
Immunoprecipitation studies showed that the GPIb/IX complex was precipitated by antibody in the presence, but not in the absence, of drug (Fig 4). To localize the antibody binding site more precisely, the ability of various MoAbs to block binding of the patient's antibody was determined. As shown in Fig 5, MoAbs specific for the IIb/IIIa complex (AP2, AP3, and Tab), the glycocalicin region of GPIb (AP1 and MBC142.1), and GPV (1D9) were without effect. One MoAb specific for GPIX (FMC25) also failed to inhibit binding, but a second (SZ1) blocked binding of the patient's antibody completely. Partial inhibition was seen with a third GPIX-specific MoAb, GR-P. These findings were of interest because of a previous report that SZ1, but not FMC25, commonly inhibits the binding to GPIX of antibodies from patients with quinine- and quinidine-induced thrombocytopenia.17 We therefore studied the effects of the GPIX-specific MoAbs on the binding to platelets of two quinine-dependent antibodies (Q1 and Q2). As shown in Fig 6, the pattern of inhibition of Q1 and Q2 by MoAbs SZ1, FMC25, and GR-P was essentially the same as for the ranitidine-dependent antibody in that binding was almost completely blocked by SZ1, but was relatively unaffected by FMC25 and GR-P.
Platelet GPIbα and GPIX were precipitated by antibody JH in the presence (lane 4), but not in the absence (lane 3), of ranitidine. Monoclonal AP1, specific for GPIbα precipitated GPIbα and GPIX both in the presence (lane 6) and absence (lane 5) of drug. No bands were precipitated by normal plasma (lanes 1 and 2) or by normal mouse IgG (lane 7). GPIbα and GPIX were demonstrated by Western blotting with monoclonals MBC142.11 and GR-P, under reducing and nonreducing conditions, respectively.
Platelet GPIbα and GPIX were precipitated by antibody JH in the presence (lane 4), but not in the absence (lane 3), of ranitidine. Monoclonal AP1, specific for GPIbα precipitated GPIbα and GPIX both in the presence (lane 6) and absence (lane 5) of drug. No bands were precipitated by normal plasma (lanes 1 and 2) or by normal mouse IgG (lane 7). GPIbα and GPIX were demonstrated by Western blotting with monoclonals MBC142.11 and GR-P, under reducing and nonreducing conditions, respectively.
Effects of preincubating platelets with various MoAbs on ranitidine-dependent binding of subsequently added antibody JH (flow cytometry). Complete inhibition was obtained only with the GPIX-specific MoAb SZ1. Values shown are the average of triplicate determinations that did not vary from one another by more than 10%.
Effects of preincubating platelets with various MoAbs on ranitidine-dependent binding of subsequently added antibody JH (flow cytometry). Complete inhibition was obtained only with the GPIX-specific MoAb SZ1. Values shown are the average of triplicate determinations that did not vary from one another by more than 10%.
Effects of MoAbs specific for GPIbα and GPIX on drug-dependent binding of antibody JH and quinine-induced antibodies (Q1, Q2) to normal platelets (flow cytometry). Pronounced inhibition of binding was obtained only with the GPIX-specific MoAb SZ1. Values shown are the average of triplicate determinations that did not vary from one another by more than 10%.
Effects of MoAbs specific for GPIbα and GPIX on drug-dependent binding of antibody JH and quinine-induced antibodies (Q1, Q2) to normal platelets (flow cytometry). Pronounced inhibition of binding was obtained only with the GPIX-specific MoAb SZ1. Values shown are the average of triplicate determinations that did not vary from one another by more than 10%.
In further attempts to demonstrate an antibody in JH plasma that was specific for the putative platelet H2 receptor, we performed immunoprecipitation studies using platelets that were surface-labeled with biotin.6 Although bands corresponding to GPIb and GPIX were precipitated when ranitidine was present in the incubation mixture, no bands were identified in the range of 40 to 50 kD, the molecular weight predicted for the human H2R on the basis of its peptide sequence18 19 (data not shown).
Specificity of the antibody for GPIX was demonstrated with transfected CHO cells.
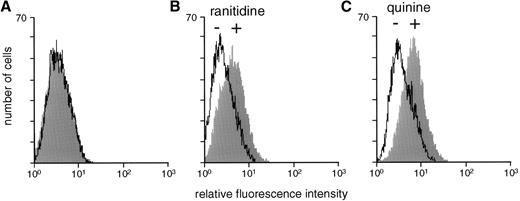
Preliminary studies with CHO cells stably transfected with GPIX and GPIbβ showed that they reacted with the anti-GPIX MoAbs FMC 25, SZ1, and GR-P, but not with AP1, specific for GPIbα (data not shown). As shown in Fig 7, antibody JH reacted with CHO cells stably transfected with GPIX and GPIbβ in the presence, but not in the absence, of ranitidine. Similar reactions were obtained with antibodies Q1 (Fig 7) and Q2 (data not shown) in the presence and absence of quinine.
Reactions of normal serum (A), antibody JH (B), and antibody Q1 (C) with CHO cells expressing GPIX and GPIbβ (flow cytometry). Antibody binding was observed only in the presence of drug. Reactions shown are typical of three independent experiments.
Reactions of normal serum (A), antibody JH (B), and antibody Q1 (C) with CHO cells expressing GPIX and GPIbβ (flow cytometry). Antibody binding was observed only in the presence of drug. Reactions shown are typical of three independent experiments.
DISCUSSION
Previous reports of cytopenias induced by ranitidine and other H2R antagonists have suggested that cell destruction is mediated by drug-induced antibodies,7-9,20-25 but this type of antibody has not previously been demonstrated convincingly by in vitro studies. In a few instances, cytopenia associated with exposure to H2R antagonists was thought to have been the result of hematosuppression.24,26 27 The rapid onset of thrombocytopenia after exposure of patient JH to ranitidine and our finding that her antibody reacts with platelets at a concentration of drug comparable to that seen in plasma after ingestion of a single 150-mg tablet provide strong evidence that the episode of severe thrombocytopenia experienced by JH was caused by a drug-dependent antibody. An unusual feature of this case is that the patient could not recall having taken the implicated drug for about 6 months prior to the exposure that appears to have induced thrombocytopenia, a length of time sufficient for many drug-induced antibodies to disappear. However, her antibody was still detectable in plasma obtained 9 months after the thrombocytopenic episode. Therefore, she appears to belong to a minority of patients with drug sensitivity who continue to produce antibody long after the last previous drug exposure.
Because of reports suggesting that platelets possess functional histamine receptors,10,11 we wondered whether antibody JH might recognize ranitidine bound to such a receptor. However, ranitidine-dependent antibody binding was unaffected by pretreatment of platelets with the H2 R antagonist, famotidine, which has a kD for H2 R about one tenth that of ranitidine16 and would be expected to compete with ranitidine for receptor binding. In addition, the drug-dependent antibody in JH plasma failed to precipitate any proteins approximating 40 kDa, the predicted molecular weight of the human H2R18,19 and did not react detectably with peripheral blood mononuclear cells, known to carry H2 receptors that are probably functional.28 29
Our subsequent studies with normal platelets, Bernard-Soulier platelets, and transfected CHO cells using flow cytometry and immunoprecipitation showed that antibody JH reacts with the GPIX and/or GPIbβ component of the GPIb/IX/V platelet membrane glycoprotein complex. Lopez et al,12 using CHO cells transfected with combinations of GPIbα, GPIbβ, and GPIX obtained evidence that MoAb SZ1 recognizes a conformational determinant formed on GPIX when it is complexed with GPIbβ or GPIbα.12 In previous studies, it was shown that FMC25 inhibits the binding of SZ1 by about 30% and that SZ1 inhibits the binding of FMC25 by about 80%, indicating that the binding sites for these two MoAbs are close to each other on GPIX.30 The epitope recognized by SZ1 is of particular interest because of the finding by Chong et al17that SZ1 completely blocked the binding to platelets of six quinine-induced antibodies, but that MoAb FMC25, was without effect. In the same study, five of six quinidine-induced antibodies were also blocked completely by SZ1, but were only partially inhibited by FMC25. We obtained similar results with two other quinine-dependent antibodies (Fig 6). Thus, antibody JH appears to bind at, or very close to a site on GPIX commonly recognized by quinine- and quinidine-induced antibodies. Although quinidine and quinine, being diastereoisomers, are structurally similar, ranitidine bears no structural resemblance to either of these compounds. Therefore, our findings suggest the possibility that the domain on GPIX recognized by SZ1 is a favored target for drug-induced antibodies, independent of the structure of the sensitizing compound. The components of the membrane-associated complex made up of GPIX, GPV, GPIbβ, and GPIbα have been sequenced and, although crystallographic data are not yet available, models of how the constituent glycoproteins interact have been proposed.31 32Further studies of the region of GPIX recognized by SZ1 may provide clues to the mechanism, still unresolved, by which drugs that bind only weakly and reversibly, if at all, to antibody or glycoprotein, promote a high affinity interaction between these macromolecules and cause thrombocytopenia in certain patients with drug sensitivity.
Nizatidine, which differs from ranitidine only in having a thiazole rather than a furan ring (Fig 2), also promoted binding of antibody JH to platelets (Fig 3), but famotidine and cimetidine, which carry slightly different side chains attached to thiazole and imidazole rings, respectively, were inactive. These findings extend those of Christie et al33 of quinine- and quinidine-induced antibodies in which it was found that a seemingly very minor structural change can completely abolish the ability of a drug to promote binding of an antibody to its target. Clinical observations have shown that patients sensitive to one drug can often be treated safely with a second, pharmacologically equivalent drug that has a different structure.3 It seems likely that patient JH could have tolerated cimetidine or famotidine, but not nizatidine as an alternative to ranitidine, had further treatment with an H2R antagonist been necessary.
ACKNOWLEDGMENT
We are indebted to Robert F. Abel, Medical Center of Delaware, for help in obtaining platelets from a patient with the Bernard-Soulier syndrome, Dr Dermot Kenny, Blood Research Institute, for facilitating access to transfected CHO cells, and the Word Processing Department of The Blood Center for their help in manuscript preparation.
Supported by Grant No. HL-13629 from the Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD.
Address reprint requests to R.H. Aster, MD, Blood Research Institute, The Blood Center of Southeastern Wisconsin, 8727 Watertown Plank Rd, Milwaukee, WI 53226-3548.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked "advertisement" is accordance with 18 U.S.C. section 1734 solely to indicate this fact.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal