Abstract
Chronic myelocytic leukemia (CML) is a common neoplasm of hematopoietic pluripotent stem cells. Although the evolution from chronic phase to blast crisis (BC) in CML patients is an inevitable clinical feature, little is understood about the mechanisms responsible for the transformation. We have previously performed allelotype analysis in CML BC and have detected frequent loss of heterozygosity (LOH) on the short arm of chromosome 1. To know the common region of LOH where a putative tumor suppressor gene may reside, deletional mapping was performed using 33 microsatellite markers spanning chromosome 1 in 30 patients with CML BC (21 myeloid and 9 lymphoid). DNA was extracted from slides of bone marrow smears or from bone marrow mononuclear cells. In each patient, DNA from chronic phase was analyzed alongside DNA from either their BC or accelerated phase. Allelic loss on 1p was observed in 14 of the 30 individuals (47%): 10 of the 21 myeloid and 4 of the 9 lymphoid BC cases. Serial cytogenetic information was available in 10 cases with LOH on 1p; interestingly, deletions in this region were not detected. Two samples showed LOH at all informative loci on 1p, whereas the other 12 samples showed LOH on at least one but not all loci on 1p. The common region of LOH resided proximal to D1S508 and distal to D1S507 (1p36). Our results suggest that a tumor suppressor gene that frequently plays an important role in the evolution to BC resides on 1p36 in CML.
© 1998 by The American Society of Hematology.
SEVERAL LINES OF evidence have shown that inactivation of tumor suppressor genes is intimately associated with tumorigenesis in a wide variety of human tumors.1 The two-mutation hypothesis suggested that both alleles of a tumor suppressor gene are inactivated in tumors.2 In fact, such inactivation of a tumor suppressor gene has been commonly caused by a mutation of one allele accompanied by loss of the second allele. To date, loss of heterozygosity (LOH) has been reported to occur on various chromosomal regions in diverse tumor types. Furthermore, several tumor suppressor genes have been identified and characterized from some of these regions showing frequent LOH in tumors.
Chronic myelocytic leukemia (CML) is a common hematologic neoplasm of pluripotent hematopoietic stem cells. More than 90% of CML cases show the characteristic Philadelphia chromosome (Ph), which results in the fusion of sequences of the ABL gene from chromosome 9 with sequences of the BCR gene from chromosome 22.3,4 In the absence of effective therapy, the progression from chronic phase to blast crisis (BC) in CML patients is an inevitable clinical feature and results in a fatal process. Abnormalities of the tumor suppressor genes, such as mutations of the p53 gene, absence of RB protein, and homozygous deletions of the p16INK4agene, have been reported to occur during this process in a subset of CML cases.5-8 Abnormalities of other tumor suppressor genes may also lead to blastic transformation of CML.
Allelotype analysis is a powerful method to identify the regions that have LOH.9-11 We have previously performed allelotype analysis in 30 patients with CML BC and have detected frequent LOH at two loci on the short arm of chromosome 1.12 To define a common region of allelic loss that may harbor putative tumor suppressor gene(s), we performed deletional mapping of chromosome arm 1p in CML BC.
MATERIALS AND METHODS
Samples.
Paired bone marrow samples of chronic phase and either BC or accelerated phase (AP) were obtained from each patient with CML. Clinical information was available for all 30 patients as shown in Table 1. Seventeen patients were male and 13 patients were female. Twenty-one patients had myeloid crisis and 9 had lymphoid crisis. Twenty-six BC and 4 AP samples were obtained from the 30 patients. The mean percentage of blasts for the BC or AP samples was 54.4% (range, 10% to 90%). Cytogenetic data were available for 29 patients.
Clinical Characteristics of CML Patients
| Sample . | Age . | Sex . | Phenotype . | Blast (%)-150 . | Karyotype-151 . |
|---|---|---|---|---|---|
| CML1 | 48 | M | Myeloid | 20 | 46,XY,t(9;22)(q34:q11) |
| CML2 | 69 | F | Myeloid | 85 | 46,XX,t(9;22)(q34:q11) |
| CML3 | 39 | F | Myeloid | 50 | NA |
| CML4 | 33 | M | Myeloid | 30 | 46,XY,t(9;22)(q34:q11) |
| CML5 | 45 | M | Myeloid | 10 | 46,XY,t(9;22)(q34:q11) |
| CML6 | 45 | M | Myeloid | 65 | 47,XY,t(9;22)(q34:q11),+der(22)t(9;22)(q34:q11) |
| CML7 | 19 | M | Myeloid | 30 | 47,XY,t(9;22)(q34:q11),+der(22)t(9;22)(q34:q11) |
| CML8 | 33 | F | Myeloid | 21 | NA |
| CML9 | 38 | M | Myeloid | NA | 46,XY,der(3)t(3;7)(p13;p13),der(7)t(3;7)(p23;p13),t(9;22)(q34:q11) |
| CML10 | 39 | F | Myeloid | 16 | 46,XX,del(2)(q?),t(9;22)(q34:q11),add(11)(q?),add(15)(q?) |
| CML11 | 60 | F | Myeloid | 90 | 46,XX,t(9;22)(q34:q11) |
| CML12 | 60 | M | Myeloid | 75 | 46,XY |
| CML13 | 52 | M | Myeloid | 70 | 45,X,−Y,t(9;22)(q34:q11) |
| CML14 | 50 | M | Myeloid | 60 | 46,XY |
| CML15 | 73 | M | Myeloid | 57 | 46,XY,t(9;22)(q34:q11) |
| CML16 | 52 | M | Myeloid | 66 | 48,XY,+8,t(9;22)(q34:q11),+der(22)t(9;22)(q34:q11) |
| CML17 | 52 | F | Myeloid | 58 | 46,XX,t(9;22)(q34:q11) |
| CML18 | 61 | F | Myeloid | 64 | 46,XX,t(9;22)(q34:q11) |
| CML19 | 57 | F | Myeloid | 72 | 46,XX,t(1;21)(q32;q21),t(9;22)(q34:q11) |
| CML20 | 50 | M | Myeloid | 70 | 46,XY,t(9;22)(q34:q11) |
| CML21 | 53 | F | Myeloid | 90 | 46,XX,t(9;22)(q34:q11) |
| CML22 | 62 | M | Lymphoid | 40 | NA |
| CML23 | 38 | M | Lymphoid | 82 | 47,XY,+?der(1)t(1;20)(q21;q11.2)del(1)(p11),−9,t(9;22)(q34:q11),+18, der(20)t(1;20)(q21;q11.2) |
| CML24 | 38 | F | Lymphoid | 60 | 47,XX,t(9;22)(q34:q11),+i(17)(q10) |
| CML25 | 31 | M | Lymphoid | 90 | 46,XY,t(9;22)(q34:q11) |
| CML26 | 34 | F | Lymphoid | 10 | 46,XX,t(9;22)(q34:q11) |
| CML27 | 48 | M | Lymphoid | 65 | 46,XY,t(9;22)(q34:q11) |
| CML28 | 60 | M | Lymphoid | 40 | 46,XY,t(9;22)(q34:q11) |
| CML29 | 38 | F | Lymphoid | 45 | 46,XX,t(9;22)(q34:q11) |
| CML30 | 52 | F | Lymphoid | 46 | 46,XX,t(9;22)(q34:q11) |
| Sample . | Age . | Sex . | Phenotype . | Blast (%)-150 . | Karyotype-151 . |
|---|---|---|---|---|---|
| CML1 | 48 | M | Myeloid | 20 | 46,XY,t(9;22)(q34:q11) |
| CML2 | 69 | F | Myeloid | 85 | 46,XX,t(9;22)(q34:q11) |
| CML3 | 39 | F | Myeloid | 50 | NA |
| CML4 | 33 | M | Myeloid | 30 | 46,XY,t(9;22)(q34:q11) |
| CML5 | 45 | M | Myeloid | 10 | 46,XY,t(9;22)(q34:q11) |
| CML6 | 45 | M | Myeloid | 65 | 47,XY,t(9;22)(q34:q11),+der(22)t(9;22)(q34:q11) |
| CML7 | 19 | M | Myeloid | 30 | 47,XY,t(9;22)(q34:q11),+der(22)t(9;22)(q34:q11) |
| CML8 | 33 | F | Myeloid | 21 | NA |
| CML9 | 38 | M | Myeloid | NA | 46,XY,der(3)t(3;7)(p13;p13),der(7)t(3;7)(p23;p13),t(9;22)(q34:q11) |
| CML10 | 39 | F | Myeloid | 16 | 46,XX,del(2)(q?),t(9;22)(q34:q11),add(11)(q?),add(15)(q?) |
| CML11 | 60 | F | Myeloid | 90 | 46,XX,t(9;22)(q34:q11) |
| CML12 | 60 | M | Myeloid | 75 | 46,XY |
| CML13 | 52 | M | Myeloid | 70 | 45,X,−Y,t(9;22)(q34:q11) |
| CML14 | 50 | M | Myeloid | 60 | 46,XY |
| CML15 | 73 | M | Myeloid | 57 | 46,XY,t(9;22)(q34:q11) |
| CML16 | 52 | M | Myeloid | 66 | 48,XY,+8,t(9;22)(q34:q11),+der(22)t(9;22)(q34:q11) |
| CML17 | 52 | F | Myeloid | 58 | 46,XX,t(9;22)(q34:q11) |
| CML18 | 61 | F | Myeloid | 64 | 46,XX,t(9;22)(q34:q11) |
| CML19 | 57 | F | Myeloid | 72 | 46,XX,t(1;21)(q32;q21),t(9;22)(q34:q11) |
| CML20 | 50 | M | Myeloid | 70 | 46,XY,t(9;22)(q34:q11) |
| CML21 | 53 | F | Myeloid | 90 | 46,XX,t(9;22)(q34:q11) |
| CML22 | 62 | M | Lymphoid | 40 | NA |
| CML23 | 38 | M | Lymphoid | 82 | 47,XY,+?der(1)t(1;20)(q21;q11.2)del(1)(p11),−9,t(9;22)(q34:q11),+18, der(20)t(1;20)(q21;q11.2) |
| CML24 | 38 | F | Lymphoid | 60 | 47,XX,t(9;22)(q34:q11),+i(17)(q10) |
| CML25 | 31 | M | Lymphoid | 90 | 46,XY,t(9;22)(q34:q11) |
| CML26 | 34 | F | Lymphoid | 10 | 46,XX,t(9;22)(q34:q11) |
| CML27 | 48 | M | Lymphoid | 65 | 46,XY,t(9;22)(q34:q11) |
| CML28 | 60 | M | Lymphoid | 40 | 46,XY,t(9;22)(q34:q11) |
| CML29 | 38 | F | Lymphoid | 45 | 46,XX,t(9;22)(q34:q11) |
| CML30 | 52 | F | Lymphoid | 46 | 46,XX,t(9;22)(q34:q11) |
Abbreviations: M, male; F, female; NA, not available.
Blast (%) at BC or AP.
Karyotype at BC or AP.
All but two individuals (CML nos. 12 and 14) had Ph chromosome at diagnosis. Rearrangement of the BCR gene was detected at diagnosis by Southern blot analysis for CML nos. 12 and 14. Four samples were from AP patients (CML nos. 1, 5, 10, and 26).
Extraction of DNA.
DNA was extracted from slides of bone marrow smears derived from each patient. Cells were stripped off slides with disposable scalpels, washed once with xylene, washed twice with absolute ethanol, and were lysed with 50 mmol/L Tris-HCL (pH 8.5), 1 mmol/L EDTA, 0.5% Tween 20, and proteinase K in a final concentration of 100 μg/mL at 37°C overnight. DNA was extracted twice with phenol and once with chloroform, and was precipitated in ethanol. The DNA pellets were dissolved in 40 μL of TE (10 mmol/L Tris-HCL pH 7.4, 1 mmol/L EDTA). DNA was extracted from bone marrow mononuclear cells from 7 patients after obtaining their informed consent (CML nos. 5 through 7, CML nos. 23 through 26).13
LOH analysis.
Polymerase chain reaction (PCR)-amplification of microsatellite sequences was used to determine LOH. Primers for microsatellite sequences were obtained from Research Genetics (Huntsville, AL).14 15 Each PCR reaction contained 10 ng of DNA, 5 pmole of each primer, 1 nmole of each dNTP (Pharmacia, Stockholm, Sweden), 0.3 U of Taq DNA polymerase (GIBCO-BRL, Gaithersburg, MD), 2 μCi of [α-32P]dCTP (ICN, Irvine, CA) in 10 μL of the specified buffer with 1.5 mmol/L MgCl2. Thirty-two cycles of denaturing for 40 seconds at 94°C, annealing for 30 seconds at 55°C, and extending for 35 seconds at 72°C were performed in a Programmable Thermal Controller (MJ Research Inc, Watertown, MA). After amplification, PCR samples were diluted in the loading buffer containing 20 mmol/L EDTA, 96% formamide, 0.05% of both bromophenol blue and xylene cyanol. The products were heated to 94°C for 5 minutes and chilled on ice. Three microliters of the dilutions was applied to a 5% to 6% polyacrylamide gel containing 8.3 mol/L urea and separated for 2 to 3 hours at 75 Watts. The gel was dried and subjected to autoradiography using Kodak (Eastman Kodak Company, Rochester, NY) XAR film at either room temperature or −80°C. LOH was scored in informative cases if a significant reduction (≥50%) in the signal of the allele from the BC or AP sample was visually noted in comparison to the corresponding allele from the chronic phase of the same individual. Where necessary, LOH was assessed by densitometry. In most samples showing LOH, PCR amplification and analysis were repeated to assure consistency. For several markers that showed frequent homozygosity in chronic-phase samples, we performed duplex semiquantitative PCR with the markers on 1p and markers from chromosome arms other than 1p.
RESULTS
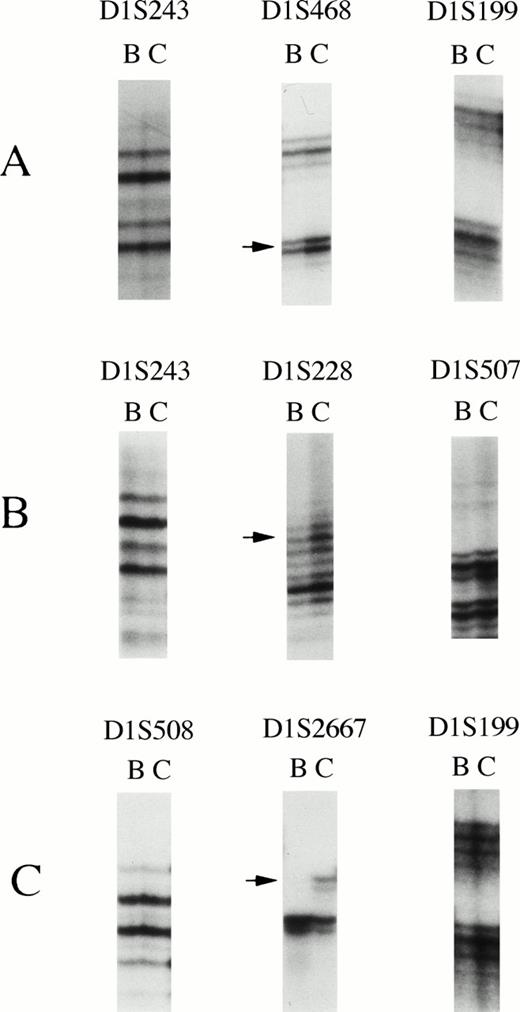
We screened 30 paired CML samples for LOH with a panel of 33 highly informative microsatellite markers spanning chromosome 1. Thirty markers were located on 1p and 3 were on 1q. Each sample was analyzed at every marker. Some samples were not informative at several loci because of a shortage of DNA. All patients were informative at multiple loci on chromosome arm 1p. We performed duplex semiquantitative PCR at several loci that showed frequent homozygosity in chronic phase samples, and we did not find occult hemizygosity. Allelic loss on 1p was observed in 14 of the 30 cases of BC or AP (47%). The most frequent LOH (8 of 15 informative cases; 53%) was observed at theD1S468 locus on chromosome band 1p36. Figure 1 shows examples of allelic loss. The lower allele was deleted at the D1S468 locus in CML no. 11 (Fig 1A). Heterozygosity was retained at D1S243 andD1S199. In Fig 1B, LOH was observed at D1S228, whereas heterozygosity was retained at D1S243 and D1S507 (CML no. 24). LOH was detected at D1S2667, whereas heterozygosity was retained at D1S508 and D1S199 (Fig 1C, CML no. 1). No instability was observed in this study.
Loss of heterozygosity on chromosome arm 1p in CML. (A) LOH was detected on D1S468 in CML no. 11. Heterozygosity was retained at D1S243 and D1S199. (B) Allelic loss was observed at D1S228, whereas heterozygosity was retained atD1S243 and D1S507 (CML no. 24). (C) LOH was found atD1S2667, whereas heterozygosity was retained at D1S508and D1S199 (CML no. 1). The locus symbol is shown on the top. Arrow indicates allele lost. B, blast crisis; C, chronic phase.
Loss of heterozygosity on chromosome arm 1p in CML. (A) LOH was detected on D1S468 in CML no. 11. Heterozygosity was retained at D1S243 and D1S199. (B) Allelic loss was observed at D1S228, whereas heterozygosity was retained atD1S243 and D1S507 (CML no. 24). (C) LOH was found atD1S2667, whereas heterozygosity was retained at D1S508and D1S199 (CML no. 1). The locus symbol is shown on the top. Arrow indicates allele lost. B, blast crisis; C, chronic phase.
Two of the 14 cases showed LOH at all informative loci on chromosome arm 1p. Twelve cases showed LOH on at least one marker on 1p but not at some other markers on this arm. Figure 2shows the deletional map on chromosome 1 in the 14 cases of LOH. CML no. 1 showed allelic loss at D1S2667 and D1S2672, and showed retention of heterozygosity at D1S508 andD1S436. For CML no. 24, LOH was detected at D1S450 andD1S228, and retention of heterozygosity was observed atD1S2663 and D1S507. The consensus region of allelic loss was determined to reside proximal to D1S508 and distal toD1S507 (1p36). This region is estimated to encompass 19 centimorgans (cM) of genetic distance.
Deletional map of chromosome 1 in CML. The common region of LOH was located proximal to D1S508 and distal toD1S507. Vertical bar indicates the common region of LOH. The locus symbols are shown on the left. Three loci are located on 1q (D1S196, D1S215, and D1S202). The sample name is on the top. Black box indicates LOH. White box indicates retained heterozygosity. Hatched box denotes not informative.
Deletional map of chromosome 1 in CML. The common region of LOH was located proximal to D1S508 and distal toD1S507. Vertical bar indicates the common region of LOH. The locus symbols are shown on the left. Three loci are located on 1q (D1S196, D1S215, and D1S202). The sample name is on the top. Black box indicates LOH. White box indicates retained heterozygosity. Hatched box denotes not informative.
Cytogenetic information of BC as well as chronic phase was available for 10 of the 14 cases with LOH on 1p; however, deletions on 1p were not detected (Table 1). Clinical information was available for all 30 patients (Table 1). Allelic loss on 1p was observed in both myeloid (10 out of 21; 48%) and lymphoid (4 out of 9; 44%) BC.
DISCUSSION
The molecular genetic changes of CML have been well studied in the chronic phase. In contrast, little is known about the mechanisms responsible for BC. To understand the role of genetic changes in the evolution of CML, we performed deletional mapping of chromosome 1 using highly informative microsatellite markers. Frequent allelic loss was observed on chromosome arm 1p in 14 of the 30 cases of BC (47%).
The common region of allelic loss resided proximal to D1S508and distal to D1S507 (1p36). Frequent LOH has been reported in the same region in several types of tumors, such as neuroblastoma, colorectal, breast and hepatocellular carcinomas, parathyroid adenoma, and melanoma.16-21 Allelic loss of 1p was associated with unfavorable outcome in neuroblastoma.22 The common region of allelic loss in the present study partly overlapped with common regions of LOH in these solid tumors.23 However, to date no altered tumor suppressor gene responsible for these tumors has been identified on chromosome region 1p36. Cloning of candidate gene(s) will define whether either a single or multiple tumor suppressor genes are clustered on 1p and are commonly involved in these types of tumors.
The p18INK4c gene is located on 1p32 and it is regarded as a tumor suppressor gene.24 Homozygous deletions of the p16INK4a gene, which is a homolog of thep18INK4c gene, were reported in lymphoid BC of CML.6 While the common region of LOH in the present study was more distal (1p36), 9 of the 14 samples also showed LOH in the region, including the p18INK4cgene locus. Therefore, we looked for mutations of thep18INK4c gene by PCR-SSCP analysis; however, no mobility shifts were detected in the 30 cases (data not shown). Thep18INK4c gene may not be affected in the transformation of CML. However, we cannot rule out the possibility that homozygous deletions of the gene had occurred, because we were unable to analyze these samples for the gene by Southern blot analysis.
Recently the p73 gene was identified, and it maps to 1p36.25 The gene is one of the candidates for tumor suppressor gene on 1p in neuroblastoma. However, the p73 locus is more distal to the D1S508 locus, and no p73 mutations were detected in neuroblastoma.25 In addition, although we screened p73 mutations in various kinds of cell lines and fresh samples, no mutations were observed (unpublished data). Analysis of the expression will be helpful to understand the role of the p73gene in CML.
In 23 of the 30 samples, DNA was extracted from bone marrow smears and it probably contained both blast and chronic phase cells. Although LOH was found in a sample of a bone marrow aspirate containing 21% blast cells (CML no. 8), we may have underestimated the true incidence of LOH. Similarly, we may have missed homozygous deletions because of the possible contamination of chronic-phase cells in our BC or AP samples. Homozygous deletions for a polymorphic marker may appear as retention of heterozygosity as a consequence of amplification of DNA from the contaminating chronic phase cells.
Ph has been observed in more than 90% of CML cases. However, chromosomal deletions or monosomy of chromosome 1 has not been characterized in CML.4,8,26 27 In our study, cytogenetic data were available from 29 patients. Because cytogenetic analysis did not show either 1p deletions or monosomy of chromosome 1 in any of the cases with LOH on 1p, our findings suggest that either mitotic nondisjunction with duplication or mitotic recombination is the frequent mechanism that resulted in LOH on 1p. The observation that heterozygosity was retained on 1q in 11 of 12 informative samples with LOH on 1p suggests that mitotic recombination is the most frequent mechanism of alteration. Small cytogenetically undetectable deletions may be present in some of the samples showing LOH on 1p. Nevertheless except for CML nos. 1, 11, and 24, the LOH covered such a large region that a deletion would have been detectable cytogenetically.
Cloning and characterization of the affected gene from chromosome arm 1p in progressive CML will help clarify the genesis of blastic transformation and provide insights into novel therapies.
ACKNOWLEDGMENT
We thank Dr M. Okada (Chromosome Laboratory, Shiseikai Dai-ni Hospital, Japan) for the help with analysis of the karyotypes.
Supported in part by grants from the National Institutes of Health and the Parker Hughes Fund. H.P.K. is a member of the Jonsson Comprehensive Cancer Center and holds the Mark Goodson Chair in Oncology Research.
Address reprint requests to Naoki Mori, MD, Department of Medicine, Division of Hematology and Oncology, Cedars-Sinai Medical Center, UCLA School of Medicine, 8700 Beverly Blvd, B208, Los Angeles, CA 90048.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked "advertisement" is accordance with 18 U.S.C. section 1734 solely to indicate this fact.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal