Lupus anticoagulants (LA) are a family of autoantibodies that are associated with in vitro anticoagulant activity but a strong predisposition to in vivo thrombosis. They are directed against plasma phospholipid binding proteins, including prothrombin. We found that a murine monoclonal antiprothrombin antibody and 7 of 7 LA IgGs tested enhanced binding of prothrombin to 25:75 phosphatidyl serine:phosphatidyl choline vesicles in a concentration-dependent manner. We hypothesized that enhanced binding of prothrombin to phospholipid in the presence of LA IgG might result in increased thrombin production when reactions are performed in flow. Thrombin production by purified prothrombinase components was measured in a phospholipid-coated flow reactor. The flow reactor was incubated with prothrombin, calcium ions, and the IgGs and then perfused with prothrombin, calcium ions, the IgGs, factor Va, and factor Xa. A murine monoclonal antiprothrombin antibody and 4 of 6 LA IgGs from patients with a history of thrombosis increased thrombin production up to 100% over control in the first 15 minutes. In summary, LA IgGs concentrate prothrombin on a phospholipid surface that can augment thrombin production by prothrombinase in flow. These observations suggest that LA might propagate coagulation in flowing blood by facilitating prothrombin interaction with the damaged blood vessel wall.
THE LUPUS ANTICOAGULANT (LA) phenomenon remains one of the conundrums of clinical medicine: a phenomenon that is due to a family of autoantibodies that are associated with in vitro anticoagulant activity on the one hand and a powerful predisposition to in vivo thrombosis on the other. There has been debate as to whether the prothrombotic association with LA and anticardiolipin antibodies (ACA) is fortuitous, with the antibodies not necessarily being responsible for thrombosis, but rather being markers for as yet undefined antibody activities. However, the weight of evidence, both clinical and experimental, favors a causative role. Almost every conceivable mechanism has been invoked in the effort to explain the thrombotic tendency in patients with LA and ACA. These include pathological activation of platelets,1 disturbance of endothelial cell function,2-4 interference with protein C and protein S,5,6 and interaction with heparan sulphate proteoglycans with consequent reduction in antithrombin activity.7 8 None of these explanations has been entirely convincing, and in most cases there has been no satisfactory mechanism defined experimentally.
The discovery that what were regarded as antiphospholipid antibodies were in fact directed at the phospholipid binding proteins β2-glycoprotein 1 (β2-GP1) in the case of ACA9,10 and prothrombin and/or β2-GP1 in the case of LA11-13 opened the way to more logical approaches to determining prothrombotic mechanisms. The focus has been largely on demonstrating antibody binding to these proteins, with and without phospholipid, and to defining potential inhibitory activity as a result of such binding.14-17
Little attention has been given to the obverse, namely that LA Ig and ACA Ig enhance the binding of phospholipid binding proteins to phospholipid surfaces. In the case of prothrombin such binding may result in concentration of prothrombin at the site of vascular injury or platelet activation. A recent report described increased binding of prothrombin to phospholipid and umbilical vein endothelial cell monolayers in the presence of LA IgG.18
It is clear that LA IgGs prolong phospholipid dependent clotting time in most in vitro assays. A feature common to in vitro coagulation tests is the static conditions under which they are performed. In contrast, thrombus formation occurs in flowing blood. We reasoned that the effects of LA IgGs on coagulation might be different when examined under flow conditions, which is more representative of the in vivo situation.
We hypothesized that enhanced binding of prothrombin to phospholipid in the presence of LA IgG would result in increased thrombin production by prothrombinase when reactions are performed in flow. We now report that a murine monoclonal antiprothrombin antibody and 7 of 7 LA IgGs tested enhanced binding of prothrombin to phospholipid vesicles and that the monoclonal antibody (MoAb) and 4 of 6 LA IgGs from patients with a history of thrombosis augmented thrombin production by purified prothrombinase components in flow. These observations suggest that LA might propagate coagulation in flowing blood by facilitating prothrombin interaction with the damaged blood vessel wall.
MATERIALS AND METHODS
Reagents and proteins.
Human prothrombin (II), factor Xa, and factor V were from Enzyme Research (South Bend, IN). Human α-thrombin (IIa) was a gift from Dr Paul Bock (Vanderbilt University Medical Center, Nashville, TN) 1,2-dioleoyl-sn-glycero-3-phosphatidylcholine (DOPC) and 1,2-dioleoyl-sn-glycero-3-phosphatidylserine (DOPS) were from Avanti Polar Lipids (Alabaster, AL), and N-((6-(biotinoyl)amino)hexanoyl)-1,2-dihexadecanoyl-sn-glycero-3-phosphoethanolamine (biotin-DHPE) was from Molecular Probes (Eugene, OR). n-octyl-β-D-glucopyranoside and D-Phe-Pro-Arg-CH2Cl were from Sigma (St Louis, MO).
Patients and control subjects.
IgG fractions were prepared from 7 patients with LA diagnosed on the basis of the accepted criteria of the ISTH Subcommittee on Lupus Anticoagulants/Phospholipid-dependent Antibodies19 and in all cases displaying prolongation of the Kaolin clotting time (KCT) and the dilute Russell’s viper venom test (dRVVT). Blood samples were obtained after informed consent, in accordance with NH&MRC guidelines. The criteria for selection were repeated, unequivocal LA positivity; all LAs were present for 0.5 to 3.5 years; availability and willingness to provide blood; and patients were unselected, apart from LA5, who was chosen because of the high titer antiprothrombin antibody. LA5 was grossly hypoprothrombinaemic (0.08 U/mL) and, in fact, presented with severe menorrhagia. Five control subjects were laboratory staff with no evident illness. ACA, both IgG and IgM, were assayed with a commercially available enzyme-linked immunosorbent assay (ELISA; Medical Innovations, Artarmon, New South Wales, Australia) using the Harris Standards as described in Shi et al.14 Binding of the LA antibodies to plastic-adsorbed DOPS in the presence of prothrombin, to plastic-adsorbed prothrombin, or to plastic-adsorbed β2-GP1 was measured exactly as described by Galli et al,13 including the use of Linbro high-activated PVC plates.
Preparation of antibodies.
The purified antihuman prothrombin murine MoAb (anti-II MoAb) was from Enzyme Research. The antibody recognizes prothrombin fragment 2 (residues 156-271) in solid-phase ELISA. A purified isotype-matched murine MoAb against bovine protein disulfide isomerase was used as a control. Total IgG was prepared from control and patient sera using protein G sepharose (Pharmacia, Uppsala, Sweden). After application of serum, the protein G sepharose was washed with 20 mmol/L sodium phosphate, pH 7, buffer containing 1 mol/L NaCl. After re-equilibration of the column with 20 mmol/L sodium phosphate, pH 7, the IgG was eluted with 0.1 mol/L glycine, pH 2.7, and the pH was neutralized immediately with 1 mol/L Tris, pH 9, buffer. The IgGs were aliquoted and stored at −20°C.
Preparation of phospholipid vesicles.
DOPC, DOPS, and biotin-DHPE were combined in the molar ratio 74:25:1, and the solvent was evaporated under argon. Unilamellar vesicles with an average diameter of approximately 200 nm were prepared according to Mimms et al.20 Phospholipid concentration was determined by measuring organic phosphate as described by Bartlett.21
Binding of prothrombin to phospholipid vesicles.
Binding of iodinated prothrombin to phospholipid vesicles was measured by separating bound from free prothrombin in an air-fuge.22Prothrombin was iodinated using immobilized iodogen according to the manufacturer’s instructions (Pierce, Rockford, IL) to a specific activity of 40,000 counts per minute (CPM)/μg.125I-prothrombin (100,000 CPM), prothrombin (0.1 to 10 μmol/L), 74:25:1 DOPC:DOPS:biotin-DHPE vesicles (15 μmol/L), and control or anti-II MoAb or LA IgG (0 to 50 μmol/L) was added to polyallomer centrifuge tubes containing 50 mmol/L HEPES, 125 mmol/L NaCl, 10 mmol/L CaCl2, 5 mg/mL bovine serum albumin (BSA), pH 7.4, buffer. The reactions were incubated for 20 minutes and the phospholipid vesicles were sedimented in an air-fuge (Beckman, Palo Alto, CA) for 20 minutes. Measurement of the phospholipid content21 of the supernatant after centrifugation indicated that the air-fuge sedimented ≥95% of the phospholipid vesicles. The supernatant was aspirated and bound, and free125I-prothrombin was determined using a Packard Crystal II γ counter (Packard Instrument Co, Meriden, CT). Nonspecific binding of 125I-prothrombin to control tubes not containing phospholipid vesicles represented ≤20% of the binding to phospholipid vesicles in the presence of 10 μmol/L control IgG. The moles of prothrombin bound to phospholipid vesicles was calculated from the total prothrombin and the ratio of bound versus total125I-prothrombin. Fab fragments were prepared from control and LA IgG using a Fab Preparation Kit (Pierce) according to the manufacturer’s instructions.
Activation of factor V.
Factor V (0.74 μmol/L) was activated by α-thrombin (0.01 μmol/L) for 15 minutes at room temperature in 25 mmol/L Tris, 5 mmol/L CaCl2, 0.5 mol/L NaCl, 50% glycerol, pH 7.5, buffer. The reaction was quenched by the addition of D-Phe-Pro-Arg-CH2Cl to a final concentration of 1 μmol/L, and the factor Va stored at −20°C until use.
Measurement of thrombin production in flow conditions.
Glass capillaries (0.65 [internal diameter] × 127 mm; Brand, Wertheim, Germany) were cleaned as described by Billy et al.23 Capillaries were dried under a stream of nitrogen; filled with 100 μg/mL Neutralite avidin (Molecular Probes) in 15 mmol/L Na2CO3, 35 mmol/L NaHCO3, 0.02% NaN3, pH 9.6, buffer; and incubated overnight at 4°C in a humid chamber. The capillaries were drained, filled with approximately 1.5 mmol/L 74:25:1 DOPC:DOPS:biotin-DHPE vesicles, and incubated at room temperature for 2 hours before connection to a gas-tight syringe (Hamilton, Reno, NV). Flow was controlled by a model sp100i syringe pump (World Precision Instruments, Sarasota, FL). Capillaries were washed with 50 mmol/L HEPES, 125 mmol/L NaCl, 3 mmol/L CaCl2, 0.5 mg/mL BSA, pH 7.4, buffer (HEPES buffer) for 2 minutes at a flow rate of 1 mL/min to remove nonbound phospholipid. Three types of experiment were performed.
Phospholipid-coated capillaries were filled with prothrombin (0.1 μmol/L), factor Va (0.1 nmol/L), and control or anti-II MoAb (0.4 μmol/L) or LA IgG (5 to 50 μmol/L) in HEPES buffer and incubated for 1 hour at room temperature. The capillaries were then perfused with 20 pmol/L factor Xa without or with the anti-II MoAb (0.4 μmol/L) or LA IgG (5 to 50 μmol/L) in HEPES buffer at a flow rate of 30 μL/min. Alternatively, phospholipid-coated capillaries were incubated with prothrombin (0.1 μmol/L) and control or anti-II MoAb (0.4 μmol/L) or LA IgG (5 to 50 μmol/L) and then perfused with factor Xa (20 pmol/L) and factor Va (0.1 nmol/L) without or with the anti-II MoAb or LA IgG.
Phospholipid-coated capillaries were filled with prothrombin (0.1 μmol/L) and control or anti-II MoAb (0.4 μmol/L) or LA IgG (5 to 50 μmol/L) in HEPES buffer and incubated for 1 hour at room temperature and then perfused with prothrombin (0.1 μmol/L), factor Xa (1 nmol/L), factor Va (2 nmol/L), and control or anti-II MoAb (0.4 μmol/L) or LA IgG (5 to 50 μmol/L) in HEPES buffer at a flow rate of 30 μL/min.
Normal human plasma was collected in citrate, depleted of IgG using protein G sepharose, and dialyzed against 50 mmol/L Tris-HCl, 0.1 mol/L NaCl, 1 mmol/L EDTA, pH 7.4, buffer to remove citrate. D-Phe-Pro-Arg-CH2Cl (10 μmol/L), CaCl2 (10 mmol/L), and control or LA IgG (25 μmol/L) was added to the plasma, which was incubated in phospholipid-coated capillaries for 1 hour at room temperature. The plasma was diluted 1:2 with 50 mmol/L Tris-HCl, 0.1 mol/L NaCl, pH 7.4, buffer. Capillaries were perfused with 2 capillary volumes of HEPES buffer at a flow rate of 30 μL/min to wash away plasma and D-Phe-Pro-Arg-CH2Cl, followed by factor Xa (1 nmol/L) and factor Va (2 nmol/L) in the HEPES buffer at the same flow rate.
The reaction products were collected into wells of 96-well plates containing 50 mmol/L Tris, 175 mmol/L NaCl, 20 mmol/L EDTA, 0.5 mg/mL BSA, pH 7.9, buffer. Thrombin concentration was determined by adding N-p-Tosyl-Gly-Pro-Arg-p-nitroanilide (TGPRpNA; Sigma) to a final concentration of 100 μmol/L and measuring the initial rate of p-nitroaniline formation at 405 nm using a Thermomax Kinetic Microplate Reader (Molecular Devices, Menlo Park, CA).22
The results of the flow experiments were very reliable and reproducible on a given day. There was some quantitative variation from day to day; however, the qualitative differences were very consistent. All of the experiments were performed at least twice, and on most occasions 3 to 6 times. A phospholipid capillary was only used once, because it was difficult to ensure that all reactants from a previous experiment were removed.
Measurement of thrombin production in static conditions.
Phospholipid vesicles (5 μmol/L), prothrombin (0.1 μmol/L), factor Va (0.1 nmol/L), and control or LA IgG (5 to 50 μmol/L) in HEPES buffer was incubated for 1 hour at room temperature. Factor Xa was added to a final concentration of 20 pmol/L to initiate the reaction. Aliquots of the reaction were removed at discrete time intervals and diluted 40-fold into 50 mmol/L Tris-HCl, 175 mmol/L NaCl, 20 mmol/L EDTA, 0.5 mg/mL BSA, pH 7.9, buffer to quench the reaction. Thrombin concentration was calculated as described above.
RESULTS
Characteristics of the anti-II MoAb and LA IgGs.
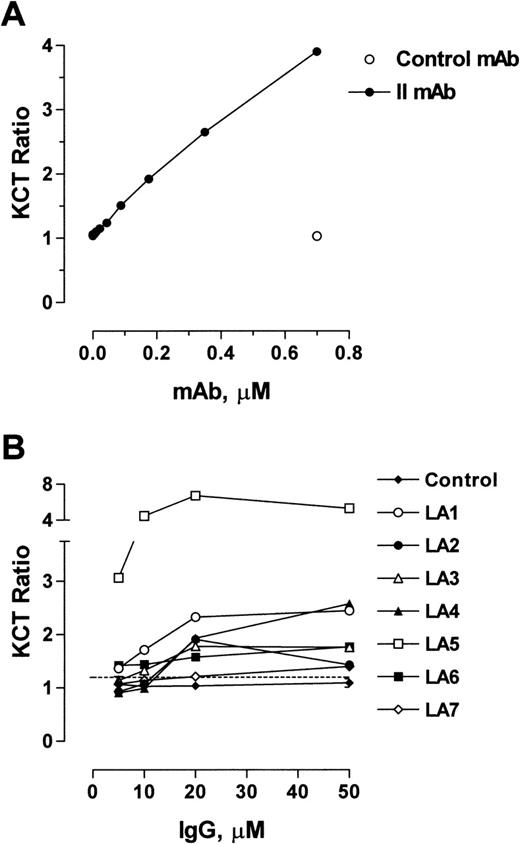
The antihuman II murine MoAb recognizes prothrombin fragment 2 (residues 156-271) adsorbed to ELISA plate wells. The effect of the anti-II MoAb on the KCT of normal plasma was determined. The anti-II MoAb prolonged the clotting of normal plasma in a concentration-dependent manner (Fig 1A). A control MoAb had no effect.
Effect of anti-II MoAb and LA IgGs on the KCT of normal plasma. (A) A control MoAb or anti-II MoAb was added to an equal volume of normal plasma and the KCT was determined.14 The normal plasma was depleted of IgG using protein G sepharose. The anti-II MoAb prolonged the KCT of normal plasma in a concentration-dependent manner, whereas the control MoAb had no effect. (B) To confirm the LA activity of the IgG preparations from the 7 patient plasmas, they were added to an equal volume of normal plasma and the KCT was determined.14 The normal plasma was depleted of IgG using protein G sepharose. Values for LA IgGs are expressed as a proportion of the KCT for normal plasma, with values greater than 1.2 (indicated by a horizontal line) being positive for LA. Control values were combined and are expressed as the mean ± SE (n = 5). The IgG prepared from control subjects’ serum showed no LA activity at the concentrations tested, whereas all of the patients’ IgGs resulted in prolongation of the KCT at final concentrations of 20 μmol/L and greater.
Effect of anti-II MoAb and LA IgGs on the KCT of normal plasma. (A) A control MoAb or anti-II MoAb was added to an equal volume of normal plasma and the KCT was determined.14 The normal plasma was depleted of IgG using protein G sepharose. The anti-II MoAb prolonged the KCT of normal plasma in a concentration-dependent manner, whereas the control MoAb had no effect. (B) To confirm the LA activity of the IgG preparations from the 7 patient plasmas, they were added to an equal volume of normal plasma and the KCT was determined.14 The normal plasma was depleted of IgG using protein G sepharose. Values for LA IgGs are expressed as a proportion of the KCT for normal plasma, with values greater than 1.2 (indicated by a horizontal line) being positive for LA. Control values were combined and are expressed as the mean ± SE (n = 5). The IgG prepared from control subjects’ serum showed no LA activity at the concentrations tested, whereas all of the patients’ IgGs resulted in prolongation of the KCT at final concentrations of 20 μmol/L and greater.
The median age for 7 patients with LA was 32 years, with a range of 14 to 62 years (Table 1). Five healthy subjects had no history of thrombosis, whereas 6 of the 7 patients had a history of arterial (acute myocardial infarction [AMI] and cerebrovascular accident [CVA]) or venous thrombotic events, including deep vein thrombosis (DVT) with or without pulmonary embolus (PE). The other patient (LA5) had no thrombotic history but presented with a severe bleeding diathesis associated with hypoprothrombinaemia. The KCT of a 20% patient:80% normal plasma mixture as a ratio with the KCT of a normal plasma for each patient varied from 1.3 to greater than 2 (ratios >1.2 are positive for LA). IgG ACA were present in the plasma of 4 of the 7 patients (LA2, LA3, LA4, and LA5), and 4 had mild to moderate thrombocytopenia. Using the assay methodology of Galli et al,13 3 patients had antibodies that reacted with either plastic-adsorbed DOPS in the presence of prothrombin or plastic-adsorbed prothrombin (LA4, LA5, and LA7), and 2 had antibodies that reacted with plastic-adsorbed β2-GP1 (LA2 and LA4). Only 2 patients (LA1 and LA5) were found to have diagnostic lupus serology with positive antinuclear factor and antibodies for double-stranded DNA.
Summary of LA Characteristics and Patient Histories
| Patient No. . | Sex . | Age (yrs) . | Plasma KCT Ratio* . | Serum ACA† (U/mL) . | ANA . | dsDNA‡ . | Platelet Count (×109/L) . | ELISA Reactivity . | History of Thrombosis . | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| IgG . | IgM . | II1-153 . | β2GP11-155 . | ||||||||
| Control | 2 F, 3 M | 25-37 | ≤1.1 | ≤2.8 | ≤5.8 | — | — | — | − | − | Nil |
| LA1 | M | 25 | 1.5 | 8.5 | 3.4 | 1:640 | + | 136 | − | − | DVT |
| LA2 | F | 32 | 2.5 | 200 | 47.4 | 1:360 | − | 82-111 | − | + | Nonhemorrhagic CVA |
| Atrial appendage thrombus | |||||||||||
| LA3 | F | 17 | 1.8 | 62 | 9.3 | — | − | 124 | − | − | DVT and PE |
| LA4 | F | 50 | 1.3 | 80 | 13.1 | — | − | ND | + | + | Nonhemorrhagic CVA |
| LA5 | F | 14 | >2 | 58 | 31 | 1:2,560 | + | 254 | + | − | Hemorrhage and menorrhagia |
| LA6 | M | 62 | 2.1 | 1.5 | 39 | 1:80 | ND | 114-123 | − | − | AMI 8 yrs before |
| LA7 | M | 32 | 1.9 | ND | ND | ND | ND | 232 | + | − | Axillary vein thrombus |
| Patient No. . | Sex . | Age (yrs) . | Plasma KCT Ratio* . | Serum ACA† (U/mL) . | ANA . | dsDNA‡ . | Platelet Count (×109/L) . | ELISA Reactivity . | History of Thrombosis . | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| IgG . | IgM . | II1-153 . | β2GP11-155 . | ||||||||
| Control | 2 F, 3 M | 25-37 | ≤1.1 | ≤2.8 | ≤5.8 | — | — | — | − | − | Nil |
| LA1 | M | 25 | 1.5 | 8.5 | 3.4 | 1:640 | + | 136 | − | − | DVT |
| LA2 | F | 32 | 2.5 | 200 | 47.4 | 1:360 | − | 82-111 | − | + | Nonhemorrhagic CVA |
| Atrial appendage thrombus | |||||||||||
| LA3 | F | 17 | 1.8 | 62 | 9.3 | — | − | 124 | − | − | DVT and PE |
| LA4 | F | 50 | 1.3 | 80 | 13.1 | — | − | ND | + | + | Nonhemorrhagic CVA |
| LA5 | F | 14 | >2 | 58 | 31 | 1:2,560 | + | 254 | + | − | Hemorrhage and menorrhagia |
| LA6 | M | 62 | 2.1 | 1.5 | 39 | 1:80 | ND | 114-123 | − | − | AMI 8 yrs before |
| LA7 | M | 32 | 1.9 | ND | ND | ND | ND | 232 | + | − | Axillary vein thrombus |
Abbreviations: ND, not determined; ANA, antibodies to nuclear antigens.
Plasma KCT ratio.14
Serum ACA.14
Antibodies to dsDNA.
Reactivity against plastic-adsorbed phosphatidylserine in the presence of prothrombin.13 The same reactivity was observed against plastic-adsorbed prothrombin.13
Reactivity against plastic-adsorbed β2-GP1.13
The total IgG from the plasmas of the 7 patients with LA were purified on protein G sepharose. The LA IgGs were not contaminated by coagulation factors, as determined by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and functional assays (not shown). The purpose of this study was to examine the net properties of the LA IgGs on the binding and conversion of prothrombin on phospholipid vesicles in both static and flow conditions. No attempt was made to affinity purify the antiprothrombin Igs, because these Igs would have not necessarily reflected the net properties of the total Ig population on prothrombin binding and conversion. For instance, only 3 of the 7 LA IgGs reacted with plastic-adsorbed DOPS in the presence of prothrombin (Table 1); therefore, only 3 of the 7 LA IgG antiprothrombin antibodies would have been expected to bind to an immobilized DOPS column in the presence of prothrombin. The specificity of effects in the experiments described herein was conferred by using purified coagulation factors rather than by attempting to purify Ig populations.
To confirm the LA activity of the LA IgGs, they were added to normal plasma and the KCT was determined. The IgG prepared from control subjects’ serum showed no LA activity at the concentrations tested, whereas all of the patients’ IgGs resulted in prolongation of the KCT at final concentrations of 20 μmol/L and greater (Fig 1B). The effect of the LA IgGs on the KCT was probably a combination of antiprothrombin antibodies and anti-β2GP1 antibodies (Table 1).
Effect of an anti-II MoAb and LA IgGs on binding of prothrombin to phospholipid vesicles.
In addition to recognizing phospholipid-bound prothrombin, LA IgGs have been shown to enhance interaction of prothrombin with plastic-adsorbed phospholipid and to cultured human umbilical vein endothelial cells.18 We found that the anti-II MoAb and LA IgGs also enhanced binding of prothrombin to phospholipid bilayers.
Prothrombin was incubated with unilamellar 200-nm diameter 74:25:1 DOPC:DOPS:biotin-DHPE phospholipid vesicles in the presence of control or anti-II or LA IgG and bound prothrombin determined by sedimenting the vesicles in an air-fuge. The effect of increasing control, anti-II MoAb, or LA IgG concentration on binding of prothrombin to phospholipid vesicles is shown in Fig 2. The anti-II MoAb and all of the LA IgGs enhanced prothrombin binding to phospholipid vesicles in a concentration-dependent manner. Neither the control MoAb nor the control IgG had any significant effect on prothrombin binding. These results are similar to those reported by Rao et al,18 who found that all 4 IgG preparations tested increased the affinity of binding of 125I-prothrombin to immobilized phospholipid.
Effect of anti-II MoAb and LA IgGs on binding of II to phospholipid vesicles. Binding of prothrombin to 200 nm 74:25:1 DOPC:DOPS:biotin-DHPE unilamellar vesicles was measured by separating bound from free prothrombin in an air-fuge.22 (A) Effect of control MoAb or anti-II MoAb on binding of 0.1 μmol/L prothrombin to phospholipid vesicles. The data are expressed as the fraction of total prothrombin bound. Data points and error bars represent the mean and SE of 3 experiments. (B) Effect of control or LA IgGs on binding of 0.1 μmol/L prothrombin to phospholipid vesicles. The data are expressed as the fraction of total prothrombin bound.
Effect of anti-II MoAb and LA IgGs on binding of II to phospholipid vesicles. Binding of prothrombin to 200 nm 74:25:1 DOPC:DOPS:biotin-DHPE unilamellar vesicles was measured by separating bound from free prothrombin in an air-fuge.22 (A) Effect of control MoAb or anti-II MoAb on binding of 0.1 μmol/L prothrombin to phospholipid vesicles. The data are expressed as the fraction of total prothrombin bound. Data points and error bars represent the mean and SE of 3 experiments. (B) Effect of control or LA IgGs on binding of 0.1 μmol/L prothrombin to phospholipid vesicles. The data are expressed as the fraction of total prothrombin bound.
The bivalency of the LA IgG was required to enhance binding of prothrombin to phospholipid, because Fab fragments of LA2, LA4, and LA5 IgGs did not promote prothrombin binding (Chesterman et al, submitted for publication). The other LA Fab fragments were not tested. This dependence on LA antibody bivalency for prothrombin binding parallels the requirement for ACA bivalency for high-affinity binding of β2-GP1 to lipid membranes.24-26
Effect of the anti-II MoAb and LA IgGs on thrombin production in a tubular flow reactor coated with phospholipid vesicles.
To investigate the effects of the anti-II MoAb and LA IgGs on thrombin production and conversion in flow, tubular flow reactors were used. The reactors consisted of glass capillaries whose interior surfaces were coated with unilamellar 74:25:1 DOPC:DOPS:biotin-DHPE phospholipid vesicles by linking the biotin-labeled PE to adsorbed avidin. Initially, we tested whether the effects of the anti-II MoAb and LA IgGs on prothrombin binding to soluble phospholipid vesicles shown in Fig 2 were reflected in the thrombin production on the interior surface of the phospholipid-coated capillaries.
Phospholipid-coated capillaries were incubated with prothrombin, factor Va, and control or anti-II MoAb or LA IgG and were then perfused with factor Xa. Alternatively, the capillaries were incubated with prothrombin and control or anti-II MoAb or LA IgG and were then perfused with factor Xa and factor Va. The thrombin content of the eluate from the capillaries was measured from the initial rate of hydrolysis of the tripeptidyl p-nitroanilide substrate, TGPRpNA. Reversing the introduction of factor Va did not significantly influence the results with the anti-II MoAb and all LA IgGs tested (not shown).
The anti-II MoAb markedly increased thrombin production in the phospholipid-coated capillary. The pattern of thrombin production is shown in Fig 3 for an MoAb concentration of 0.4 μmol/L. Under the flow conditions of the assay, there was very little thrombin production in the presence of the control MoAb, which probably reflected the relatively weak binding of prothrombin to phospholipid vesicles (dissociation constant, ∼1 μmol/L27) and the concentration of prothrombin used in the assays (0.1 μmol/L).
Effect of anti-II MoAb on thrombin production in a tubular flow reactor coated with phospholipid vesicles. Glass capillaries were coated with phospholipid vesicles and incubated with 0.1 μmol/L prothrombin, 0.1 nmol/L factor Va, and 0.4 μmol/L of control or anti-II MoAb for 1 hour. The capillaries were perfused with 20 pmol/L factor Xa at a flow rate of 30 μL/min. Two-minute fractions were collected and the thrombin concentration was determined by the rate of hydrolysis of N-p-Tosyl-Gly-Pro-Arg-p-nitroanilide.
Effect of anti-II MoAb on thrombin production in a tubular flow reactor coated with phospholipid vesicles. Glass capillaries were coated with phospholipid vesicles and incubated with 0.1 μmol/L prothrombin, 0.1 nmol/L factor Va, and 0.4 μmol/L of control or anti-II MoAb for 1 hour. The capillaries were perfused with 20 pmol/L factor Xa at a flow rate of 30 μL/min. Two-minute fractions were collected and the thrombin concentration was determined by the rate of hydrolysis of N-p-Tosyl-Gly-Pro-Arg-p-nitroanilide.
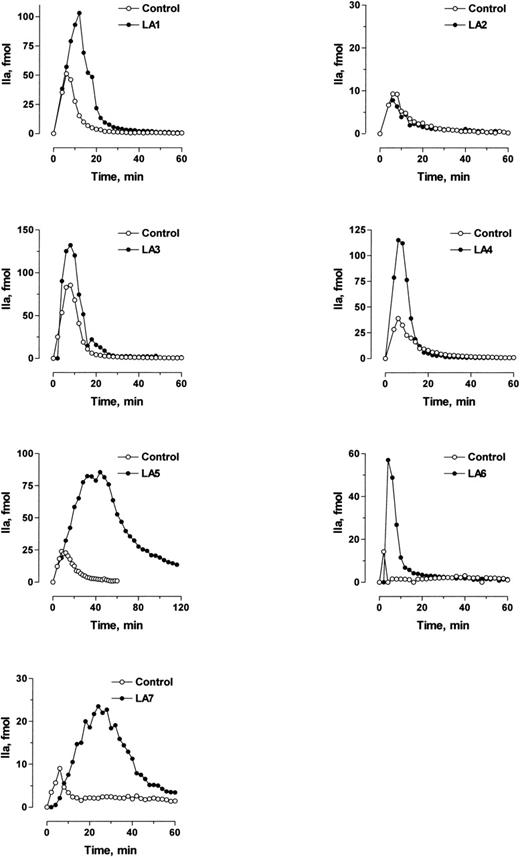
The LA IgGs also resulted in a net increase in thrombin production, with the exception of LA2. The patterns of thrombin production are shown in Fig 4 for selected LA IgG concentrations. There was a small amount of thrombin production in the presence of control IgG, which increased with increasing control IgG concentration. However, there was a marked difference between control and LA IgG for 6 of the 7 LA IgGs.
Effect of LA IgGs on thrombin production in the phospholipid-coated flow reactor. Glass capillaries were coated with phospholipid vesicles and incubated with 0.1 μmol/L prothrombin, 0.1 nmol/L factor Va, and control or LA IgG for 1 hour. The LA IgG and corresponding control IgG concentrations were 5 μmol/L for LA4 and LA7; 10 μmol/L for LA2, LA5, and LA6; 20 μmol/L for LA1; and 50 μmol/L for LA3. The capillaries were perfused with 20 pmol/L factor Xa at a flow rate of 30 μL/min. Two-minute fractions were collected and the thrombin concentration was determined by the rate of hydrolysis of N-p-Tosyl-Gly-Pro-Arg-p-nitroanilide.
Effect of LA IgGs on thrombin production in the phospholipid-coated flow reactor. Glass capillaries were coated with phospholipid vesicles and incubated with 0.1 μmol/L prothrombin, 0.1 nmol/L factor Va, and control or LA IgG for 1 hour. The LA IgG and corresponding control IgG concentrations were 5 μmol/L for LA4 and LA7; 10 μmol/L for LA2, LA5, and LA6; 20 μmol/L for LA1; and 50 μmol/L for LA3. The capillaries were perfused with 20 pmol/L factor Xa at a flow rate of 30 μL/min. Two-minute fractions were collected and the thrombin concentration was determined by the rate of hydrolysis of N-p-Tosyl-Gly-Pro-Arg-p-nitroanilide.
Capillaries were incubated with prothrombin, factor Va, and LA IgG for either 5 minutes or 1 hour before perfusion with factor Xa, with the timing having little effect on the outcome (not shown). The results shown in Figs 3 and 4 were the same relative to control whether factor Xa and factor Va concentrations of either 20 pmol/L and 0.1 nmol/L or 1 nmol/L and 2 nmol/L, respectively, were used (not shown).
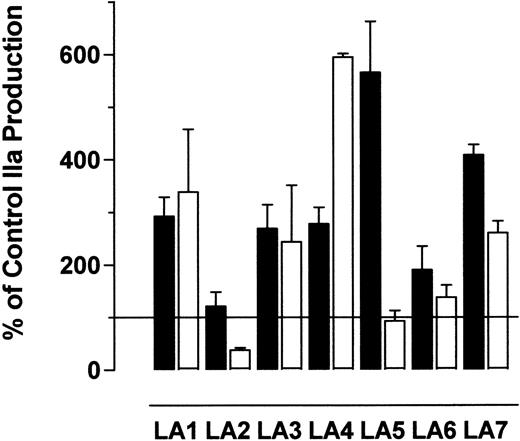
The dependence of thrombin production on LA IgG concentration is shown in Fig 5. The LA IgG concentration that gave maximum thrombin production varied for the different patient IgGs. Thrombin production peaked at 5 to 10 μmol/L for some LA IgGs, whereas others peaked at 20 to 50 μmol/L LA IgG. Enhancements in thrombin production of 1.2- to 5.6-fold (median, 2.8-fold; n = 7) over control IgG were observed. These results probably reflected enhanced binding of prothrombin to the phospholipid-coated capillary similar to that observed using phospholipid vesicles (Fig 2).
Effect of varying LA IgG concentration on thrombin production in the phospholipid-coated flow reactor. Glass capillaries were coated with phospholipid vesicles and incubated with 0.1 μmol/L prothrombin, 0.1 nmol/L factor Va, and 5 to 50 μmol/L control or LA IgGs for 1 hour. The capillaries were perfused with 20 pmol/L factor Xa at a flow rate of 30 μL/min. Total thrombin production was calculated for each LA IgG concentration from the area under the curve of profiles of the type shown in Fig 4. Thrombin production is expressed as a percentage of the mean control value for each IgG concentration. Data points and error bars represent the mean and SE of 5 experiments.
Effect of varying LA IgG concentration on thrombin production in the phospholipid-coated flow reactor. Glass capillaries were coated with phospholipid vesicles and incubated with 0.1 μmol/L prothrombin, 0.1 nmol/L factor Va, and 5 to 50 μmol/L control or LA IgGs for 1 hour. The capillaries were perfused with 20 pmol/L factor Xa at a flow rate of 30 μL/min. Total thrombin production was calculated for each LA IgG concentration from the area under the curve of profiles of the type shown in Fig 4. Thrombin production is expressed as a percentage of the mean control value for each IgG concentration. Data points and error bars represent the mean and SE of 5 experiments.
Effect of continual LA IgGs on thrombin production in the phospholipid-coated flow reactor.
To determine whether thrombin production was perturbed by the continual presence of the LA IgGs, phospholipid-coated capillaries were incubated with prothrombin, factor Va, and control or LA IgG and then perfused with both factor Xa and LA IgGs (Fig 6). The thrombin content of the eluate from the capillaries was measured from the hydrolysis of TGPRpNA.
Effect of continual LA IgGs on thrombin production in the phospholipid-coated flow reactor. Glass capillaries were coated with phospholipid vesicles and incubated with 0.1 μmol/L prothrombin, 0.1 nmol/L factor Va, and control or LA IgG for 1 hour. The concentration of LA IgG used in the experiment was that which resulted in maximal prothrombin binding (see Fig 5): 5 μmol/L for LA4 and LA7; 10 μmol/L for LA2, LA5, and LA6; 20 μmol/L for LA1; and 50 μmol/L for LA3. The capillaries were perfused with either 20 pmol/L factor Xa or 20 pmol/L factor Xa and LA IgG at a flow rate of 30 μL/min. Two-minute fractions were collected and the thrombin concentration was determined by the rate of hydrolysis of N-p-Tosyl-Gly-Pro-Arg-p-nitroanilide. Total thrombin production was calculated for each LA IgG and is expressed as a percentage of the mean control value for each IgG concentration (see Fig 5). Data points and error bars represent the mean and SE of 5 experiments. (▪) Results from perfusion with 20 pmol/L Xa alone; (□) results from perfusion with both 20 pmol/L Xa and LA IgG.
Effect of continual LA IgGs on thrombin production in the phospholipid-coated flow reactor. Glass capillaries were coated with phospholipid vesicles and incubated with 0.1 μmol/L prothrombin, 0.1 nmol/L factor Va, and control or LA IgG for 1 hour. The concentration of LA IgG used in the experiment was that which resulted in maximal prothrombin binding (see Fig 5): 5 μmol/L for LA4 and LA7; 10 μmol/L for LA2, LA5, and LA6; 20 μmol/L for LA1; and 50 μmol/L for LA3. The capillaries were perfused with either 20 pmol/L factor Xa or 20 pmol/L factor Xa and LA IgG at a flow rate of 30 μL/min. Two-minute fractions were collected and the thrombin concentration was determined by the rate of hydrolysis of N-p-Tosyl-Gly-Pro-Arg-p-nitroanilide. Total thrombin production was calculated for each LA IgG and is expressed as a percentage of the mean control value for each IgG concentration (see Fig 5). Data points and error bars represent the mean and SE of 5 experiments. (▪) Results from perfusion with 20 pmol/L Xa alone; (□) results from perfusion with both 20 pmol/L Xa and LA IgG.
The presence of LA IgG in the perfusate reduced thrombin production by approximately half for LA7, to control levels for LA5, and to less than control for LA2. In contrast, thrombin production increased 2-fold in the presence of solution phase LA4. The presence of LA1, LA3, or LA6 in the perfusate only marginally enhanced or inhibited thrombin production. Therefore, the presence of solution phase LA IgGs significantly changed the nature of prothrombin conversion for 4 of the 7 LA IgGs.
Effect of LA IgGs on thrombin production in flow.
A growing thrombus is continually supplied with prothrombin from the flowing blood. To determine whether the anti-II MoAb and LA IgGs could enhance thrombin production in flow in the presence of a continuous supply of prothrombin, phospholipid-coated capillaries were preincubated with prothrombin and LA IgGs and then perfused with factor Xa, factor Va, LA IgGs, and prothrombin. The concentrations of prothrombin, calcium ions, factor Va, and factor Xa were 0.1 μmol/L, 3 mmol/L, 1 nmol/L, and 2 nmol/L, respectively. The wall shear rate was 18.5 s−1, which is similar to that of large veins.28
The anti-II MoAb was tested at a concentration of 0.4 μmol/L, whereas all LA IgGs were tested at the concentrations that produced maximum effects in the experiments shown in Figs 4 and 5. The anti-II MoAb enhanced thrombin production by 70% over control in the first 10 minutes (Fig 7). LA1, LA4, and LA7 IgG enhanced thrombin production up to 100% over control in the first 5 to 10 minutes, whereas LA3 enhanced both initial thrombin production and the final steady state production of thrombin by approximately 100% over control (Fig 8). LA2 and LA6 IgG were not different from control, and LA5 IgG prolonged the approach to steady state thrombin production. This is in keeping with the inhibitory effect of LA5 IgG shown in Fig 6 and this patient’s clinical bleeding rather than thrombosis. The steady state rates of thrombin production were not significantly different from control for all LA IgG, except for LA3, which was increased by approximately 100%. In addition, Fab fragments of LA3 IgG did not enhance thrombin production (Chesterman et al, submitted for publication), which is consistent with the requirement for antibody bivalency to enhance prothrombin interaction with phospholipid vesicles.
Effect of an anti-II MoAb on thrombin production in flow. A glass capillary was coated with phospholipid vesicles and incubated with 0.1 μmol/L prothrombin and 0.4 μmol/L control or anti-II MoAb and was then perfused with 0.1 μmol/L prothrombin, 0.4 μmol/L control or anti-II MoAb, 2 nmol/L factor Va, and 1 nmol/L Xa at a flow rate of 30 μL/min (collecting 15-second fractions every 30 seconds). Thrombin concentration was determined by the rate of hydrolysis of N-p-Tosyl-Gly-Pro-Arg-p-nitroanilide.
Effect of an anti-II MoAb on thrombin production in flow. A glass capillary was coated with phospholipid vesicles and incubated with 0.1 μmol/L prothrombin and 0.4 μmol/L control or anti-II MoAb and was then perfused with 0.1 μmol/L prothrombin, 0.4 μmol/L control or anti-II MoAb, 2 nmol/L factor Va, and 1 nmol/L Xa at a flow rate of 30 μL/min (collecting 15-second fractions every 30 seconds). Thrombin concentration was determined by the rate of hydrolysis of N-p-Tosyl-Gly-Pro-Arg-p-nitroanilide.
Effect of LA IgGs on thrombin production in flow. Glass capillaries were coated with phospholipid vesicles and incubated with 0.1 μmol/L prothrombin and control or LA IgG and were then perfused with 0.1 μmol/L prothrombin, control, or LA IgG; 2 nmol/L factor Va; and 1 nmol/L Xa at a flow rate of 30 μL/min (collecting 15-second fractions every 30 or 60 seconds). Thrombin concentration was determined by the rate of hydrolysis of N-p-Tosyl-Gly-Pro-Arg-p-nitroanilide. The concentration of LA IgG used in the experiment was that which resulted in maximal prothrombin binding (see Fig 5): 5 μmol/L for LA4 and LA7; 10 μmol/L for LA2, LA5, and LA6; 20 μmol/L for LA1; and 50 μmol/L for LA3.
Effect of LA IgGs on thrombin production in flow. Glass capillaries were coated with phospholipid vesicles and incubated with 0.1 μmol/L prothrombin and control or LA IgG and were then perfused with 0.1 μmol/L prothrombin, control, or LA IgG; 2 nmol/L factor Va; and 1 nmol/L Xa at a flow rate of 30 μL/min (collecting 15-second fractions every 30 or 60 seconds). Thrombin concentration was determined by the rate of hydrolysis of N-p-Tosyl-Gly-Pro-Arg-p-nitroanilide. The concentration of LA IgG used in the experiment was that which resulted in maximal prothrombin binding (see Fig 5): 5 μmol/L for LA4 and LA7; 10 μmol/L for LA2, LA5, and LA6; 20 μmol/L for LA1; and 50 μmol/L for LA3.
Effect of LA IgGs on thrombin production in static conditions.
The results of the experiments described in Fig 8 indicate that prothrombin is a competent substrate for prothrombinase in flow despite the presence of LA IgGs. Considering the anticoagulant effect of LAs in in vitro clotting tests, we compared the results in flow with the effect of the LA IgGs on progress curves for thrombin formation by prothrombinase in static conditions. The LA IgGs were tested at the concentrations that produced maximum effects in the experiments shown in Figs 4 and 5, which were the same concentrations used in the flow experiments in Fig 8.
LA2 and LA4 did not significantly effect the rate of thrombin formation, whereas LA1, LA3, LA5, LA6, and LA7 all significantly inhibited the rate of thrombin formation (Fig 9). LA5 was the most inhibitory of the LA IgGs in the static conditions, which is in keeping with its inhibitory effect in flow and this patient’s bleeding diathesis.
Effect of LA IgGs on thrombin production in static conditions. Phospholipid vesicles (5 μmol/L), prothrombin (0.1 μmol/L), factor Va (0.1 nmol/L), and control or LA IgG (5 to 50 μmol/L) in HEPES buffer was incubated for 1 hour at room temperature. Factor Xa was added to a final concentration of 20 pmol/L to initiate the reaction. Aliquots of the reaction were removed at discrete time intervals and thrombin concentration was determined by the rate of hydrolysis of N-p-Tosyl-Gly-Pro-Arg-p-nitroanilide. The concentration of LA IgG used in the experiment was that which resulted in maximal prothrombin binding (see Fig 5): 5 μmol/L for LA4 and LA7; 10 μmol/L for LA2, LA5, and LA6; 20 μmol/L for LA1; and 50 μmol/L for LA3. Data points and error bars represent the mean and SE of triplicate determinations.
Effect of LA IgGs on thrombin production in static conditions. Phospholipid vesicles (5 μmol/L), prothrombin (0.1 μmol/L), factor Va (0.1 nmol/L), and control or LA IgG (5 to 50 μmol/L) in HEPES buffer was incubated for 1 hour at room temperature. Factor Xa was added to a final concentration of 20 pmol/L to initiate the reaction. Aliquots of the reaction were removed at discrete time intervals and thrombin concentration was determined by the rate of hydrolysis of N-p-Tosyl-Gly-Pro-Arg-p-nitroanilide. The concentration of LA IgG used in the experiment was that which resulted in maximal prothrombin binding (see Fig 5): 5 μmol/L for LA4 and LA7; 10 μmol/L for LA2, LA5, and LA6; 20 μmol/L for LA1; and 50 μmol/L for LA3. Data points and error bars represent the mean and SE of triplicate determinations.
LA2 had little effect on thrombin formation in either static or flow conditions, whereas LA4 did not effect thrombin formation in static conditions but enhanced thrombin formation in flow. In contrast, LA1, LA3, LA6, and LA7 inhibited thrombin formation in the static conditions, but enhanced (LA1, LA3, and LA7) or did not effect (LA6) thrombin formation in flow.
Effect of LA IgGs in plasma on thrombin production in the phospholipid-coated flow reactor.
Our hypothesis is that LA IgG might propagate coagulation in flowing blood by facilitating prothrombin interaction with the damaged blood vessel wall. It was important, therefore, to determine whether the LA IgGs would also promote thrombin production with the phospholipid-coated flow reactor in the complex plasma environment.
Phospholipid-coated capillaries were incubated with normal plasma containing calcium ions and physiological concentrations of control or LA IgGs and were then perfused with factor Xa and factor Va. The effects of control and LA IgGs on thrombin production is shown in Fig 10. Similar effects of the LA IgGs as shown in Fig 4 on thrombin production were observed when plasma was used as the prothrombin source. Interestingly, the relative effects of the LA IgGs differed when purified prothrombin rather than plasma prothrombin was used (compare Figs 5 and 10). This probably reflected the different IgG to prothrombin ratios used in the 2 experiments. However, plasma proteins such as β2-GP1 may have also contributed to the differing effects.
Effect of LA IgGs in plasma on thrombin production in the phospholipid-coated flow reactor. (A) Phospholipid-coated capillaries were incubated with 50% normal plasma containing 10 μmol/L D-Phe-Pro-Arg-CH2Cl, 10 mmol/L CaCl2, and 25 μmol/L control or LA IgG for 1 hour. The capillaries were washed with 2 capillary volumes of HEPES buffer and were then perfused with 1 nmol/L factor Xa and 2 nmol/L factor Va at a flow rate of 30 μL/min. One-minute fractions were collected and the thrombin concentration was determined by the rate of hydrolysis of N-p-Tosyl-Gly-Pro-Arg-p-nitroanilide. Results for LA1, LA5, and LA7 IgG are shown. (B) Total thrombin production was calculated for each LA IgG from the area under the curve of profiles of the type shown in (A).
Effect of LA IgGs in plasma on thrombin production in the phospholipid-coated flow reactor. (A) Phospholipid-coated capillaries were incubated with 50% normal plasma containing 10 μmol/L D-Phe-Pro-Arg-CH2Cl, 10 mmol/L CaCl2, and 25 μmol/L control or LA IgG for 1 hour. The capillaries were washed with 2 capillary volumes of HEPES buffer and were then perfused with 1 nmol/L factor Xa and 2 nmol/L factor Va at a flow rate of 30 μL/min. One-minute fractions were collected and the thrombin concentration was determined by the rate of hydrolysis of N-p-Tosyl-Gly-Pro-Arg-p-nitroanilide. Results for LA1, LA5, and LA7 IgG are shown. (B) Total thrombin production was calculated for each LA IgG from the area under the curve of profiles of the type shown in (A).
DISCUSSION
Rao et al18 described increased binding of prothrombin to plastic-adsorbed phospholipid and umbilical vein endothelial cell monolayers in the presence of LA IgG. We have extended these observations to unilamellar 200-nm diameter synthetic phospholipid vesicles comprising 74% DOPC, 25% DOPS, and 1% biotin-DHPE. An anti-II MoAb and 7 of 7 LA IgGs tested enhanced prothrombin binding to phospholipid vesicles in a concentration-dependent manner. The precise mechanism of this effect is unknown, although antibody bivalency was essential for those LA IgGs tested (Chesterman et al, submitted for publication). It is noteworthy that only 3 of the 7 LA IgGs reacted with plastic-adsorbed DOPS in the presence of prothrombin (Table 1). This probably reflected differences in presentation of prothrombin epitope(s) for LA IgG when prothrombin was bound to plastic-adsorbed DOPS versus bound to fluid bilayer phospholipid vesicles. Based on these observations, we hypothesized that concentration of prothrombin on a damaged blood vessel wall by LA might augment thrombin production in flowing blood that could explain the link between LA and thrombosis.
To investigate the effects of the LA IgGs on thrombin production in flow, tubular flow reactors coated with phospholipid were used. These reactors were of similar design to those described by Andree et al29 and Billy et al,23 with the exception of how the phospholipid was immobilized. The flow reactors consisted of glass capillaries whose interior surface was coated with unilamellar 74:25:1 DOPC:DOPS:biotin-DHPE phospholipid vesicles by linking the biotin-labeled PE to adsorbed avidin. The phospholipid coated in this way presented a mobile unilamellar bilayer to the flowing phase.
The ability of the anti-II MoAb and LA IgGs to promote prothrombin binding to soluble phospholipid vesicles corresponded to enhanced thrombin production in the phospholipid-coated reactor. The enhanced thrombin production in the flow reactor was probably a consequence of enhanced prothrombin binding to the phospholipid surface in the presence of the anti-II MoAb and LA IgGs. The effect of LA IgG on thrombin production in the phospholipid-coated reactor was dependent on the antibody concentration. Measurement of thrombin production as a function of LA IgG concentration resulted in bell-shaped isotherms for 5 of the 7 LA IgGs tested. This prozone effect is not uncommon in antibody studies and is probably a consequence of antibody bivalency.30 Importantly, prothrombinase converted prothrombin to thrombin in the phospholipid-coated reactor in the presence of LA IgG. This finding led us to investigate whether the LA IgGs could augment thrombin production in flow conditions resembling the in vivo situation.
Thrombus formation proceeds in an environment that is continually supplied with prothrombin from the flowing blood. In addition, we anticipate that exposed phospholipid would be bathed in prothrombin and LA IgGs before formation of factor Va and factor Xa and assembly of prothrombinase. With this in mind, we tested whether the anti-II MoAb and LA IgGs could augment thrombin production when phospholipid-coated capillaries were preincubated with prothrombin and LA IgGs and then perfused with factor Xa, factor Va, LA IgGs, and prothrombin. The wall shear rate was 18.5 s−1, which approximated that of large veins.28 The anti-II MoAb enhanced thrombin production by 70% over control in the initial 10 minutes. Four of the 6 LA IgGs from patients with a history of thrombosis enhanced thrombin production up to 100% over control in the initial 5 to 10 minutes, and 1 of these increased the final steady state production of thrombin by approximately 100% over control. Therefore, the majority of the LA IgGs tested could augment thrombin production in flow. The augmentation in thrombin production was probably a consequence of enhanced prothrombin binding to the phospholipid surface in the presence of the anti-II MoAb and LA IgGs. Billy et al23demonstrated that the rate of thrombin production in flow is controlled by the rate of transfer of prothrombin to the phospholipid surface when prothrombinase densities exceed 1 fmol/cm2. Preincubation of prothrombin with the LA IgGs concentrated prothrombin on the phospholipid surface, thus circumventing the limiting transfer of prothrombin in the initial phase of the flow reaction. In effect, there was more prothrombin bound to the phospholipid surface in the initial phase, which resulted in more thrombin production.
Our results imply that prothrombin was a catalytically competent substrate for prothrombinase in flow despite the presence of LA IgGs. Four of the 7 LA IgGs inhibited thrombin formation in static conditions but enhanced or did not effect thrombin formation in flow. Also, all of the LA IgGs prolonged the KCT of normal plasma. The reason why prothrombin was a competent substrate for prothrombinase in flow but not in static conditions in the presence of LA IgG may relate to the Km of prothrombin for prothrombinase. A striking feature of prothrombinase assembly on phospholipid vesicles in flow is the low Km for prothrombin (3 nmol/L), which is approximately 60-fold lower than the Km for prothrombin binding to prothrombinase on small unilamellar phospholipid vesicles in a static system (170 nmol/L).23 The concentration of prothrombin used in the studies herein was 0.1 μmol/L. Therefore, prothrombinase activity was anticipated to be zero order with respect to the prothrombin concentration in the flow system, ie, prothrombin was saturating. This was in contrast to the static system in which prothrombin concentration was anticipated to be less than the Km. This means that thrombin production in the static system would have been sensitive to effects of LA IgG on Kmfor prothrombin, whereas in flow an increase in Km by say even 10-fold would have had negligible effects on thrombin production.
The concept that LA IgG can augment thrombin production in flow through enhancement of prothrombin binding is worthy of investigation. An attractive feature of this model is that it may be generally applicable to LA antibodies, because the net effect of all 7 LA IgGs tested was to promote prothrombin binding to phospholipid. The challenge now is to determine whether this principle operates in flowing blood exposed to a procoagulant phospholipid surface. The observation that LA IgGs promoted thrombin production in the phospholipid-coated reactor when incubated with plasma is one line of support for this proposal. Another line of support is that thrombin production is increased in patients with LA.31 In particular, Musial et al32 showed that thrombin generation was enhanced in blood flowing ex vivo during the 3 minutes after a skin bleeding time incision with antiphospholipid antibody positive patients.
ACKNOWLEDGMENT
The authors thank Dr Kerry Taylor (Mater Hospital Brisbane, Queensland, Australia) for supplying a patient blood sample and clinical details and Margaret Aboud (Royal North Shore Hospital, New South Wales, Australia) for supplying clinical details.
Supported by grants from the National Health and Medical Research Council of Australia, the National Heart Foundation of Australia, and an Infrastructure Grant from the NSW Health Department.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Philip J. Hogg, PhD, Centre for Thrombosis and Vascular Research, School of Pathology, University of New South Wales, Sydney, NSW, 2052 Australia; e-mail:p.hogg@unsw.edu.au.








This feature is available to Subscribers Only
Sign In or Create an Account Close Modal