To analyze inherited antithrombin deficiency as a risk factor for venous thromboembolism in various conditions with regard to the presence or absence of additional genetic or acquired risk factors, we compared 48 antithrombin-deficient individuals with 44 nondeficient individuals of 14 selected families with inherited antithrombin deficiency. The incidence of venous thromboembolism for antithrombin deficient individuals was 20 times higher than among nondeficient individuals (1.1% v 0.05% per year). At the age of 50 years, greater than 50% of antithrombin-deficient individuals had experienced thrombosis compared with 5% of nondeficient individuals. Additional genetic risk factors, Factor V Leiden and PT20210A, were found in more than half of these selected families. The effect of exposure to 2 genetic defects was a 5-fold increased incidence (4.6% per year; 95% confidence interval [CI], 1.9% to 11.1%). Acquired risk factors were often present, determining the onset of thrombosis. The incidence among those with exposure to antithrombin deficiency and an acquired risk factor was increased 20-fold (20.3% per year; 95% CI, 12.0% to 34.3%). In conclusion, in these thrombophilia families, the genetic and environmental factors interact to bring about venous thrombosis. Inherited antithrombin deficiency proves to be a prominent risk factor for venous thromboembolism. The increased risks among those with exposure to acquired risk factors should be considered and adequate prophylactic anticoagulant therapy in high-risk situations seems indicated in selected families with inherited antithrombin deficiency.
SINCE THE ASSOCIATION of familial antithrombin deficiency and venous thromboembolism was described by Egeberg in 1965,1 many single cases and families have been reported in the literature. Based on these reports, the clinical manifestations of inherited antithrombin deficiency have been assessed in reviews.2-5 The frequency of a history of venous thromboembolism was estimated to be 51% among deficient individuals in one of these reviews.5 This risk of venous thrombosis should be viewed as that among highly thrombosis- prone families, ie, families who were diagnosed and selected to be reported.
An extensive study of one very large family was performed by Demers et al.5 The risk of venous thromboembolism in this selected family was less than 20% (6/31) in deficient family members; 0 of 36 nondeficient family members had had a thrombotic event.5 In a population-based case control study, the association of antithrombin deficiency and venous thromboembolism was assessed in unselected outpatients with venous thrombosis. Because of the rarity of the defect, only a small number of 5 patients and 1 control with antithrombin deficiency were diagnosed in this study (Leiden Thrombophilia Study).6 In this setting, the relative risk for thrombosis was 5.0 (95% confidence interval [CI], 0.7 to 34).6 The only family study of pedigrees not selected on a high frequency of venous thromboembolism has been performed among healthy blood donors.7 In blood donors diagnosed with an inherited deficiency of antithrombin or protein C and their relatives, the thrombosis rate was low. Only 4% (2/51) of individuals with antithrombin deficiency had experienced venous thrombosis and 1 subject experienced a recurrence.7 One might argue that here there is some selection on absence of disease.
Apparently, differences in selection lead to very different risks between relatives of healthy carriers, relatives of consecutive outpatients, and relatives of selected families with familial thrombophilia (the latter display the highest risk).8 These differences are likely not just to be stochastic phenomena, but to have a biological basis and to be the result of the simultaneous presence, or absence, of other risk factors. It is becoming increasingly clear that thrombosis is a multicausal disease and that several factors, acquired and genetic, interact to bring about thrombosis.9-12
Because clinicians will have to offer guidelines to individuals from families with thrombophilia, in which the risk appears highest, knowledge of factors contributing to the risk is essential. To date, no risk estimates for thrombosis in antithrombin deficiency based on a large number of families were available. Therefore, we set out to determine the risk of thrombosis in families with thrombophilia and antithrombin deficiency to assess the interaction with other risk factors, genetic and acquired.
MATERIALS AND METHODS
Participants of this family study were identified through family trees of 15 probands diagnosed with type I antithrombin deficiency. The parents, siblings, and children of the proband were invited to participate, as well as siblings of the affected parent and the children of affected siblings. Ten of the 15 probands had been referred for tests because of unexplained thrombosis and recurrent thrombosis, thrombosis occurring at a relatively young age, or a family history for thrombosis. Three probands were registered in our hospital with familial thrombophilia due to antithrombin deficiency. We included 1 proband referred because of high doses of heparin for treatment of recurrent thrombotic episodes and therefore screened. One proband had been referred to our center because of a positive family history; simultaneously, he participated and was identified again, independently, in a population-based patient control study, the Leiden Thrombophilia Study (LETS).6 Two probands were found to have a common ancestor.
Each family member was interviewed, and a detailed history of thromboembolic diseases was obtained by the same physician (H.H.v.B.) using a standardized questionnaire. Family members were questioned specifically about history of venous thromboembolism, ie, deep venous thrombosis and pulmonary embolism. If an individual reported such a problem, information about the method of diagnosis was obtained as well as clinical risk factors for thrombosis at the time of or preceding the event. Risk factors were defined a priori as surgery, hospitalization, immobilization, major trauma, plaster casts, pregnancy, postpartum state, and use of oral contraceptives. The criteria used for the diagnosis of previous venous thromboembolism were hospitalization or treatment. The clinical diagnosis of the physician was confirmed with objective diagnostic techniques in 71% of the first venous thromboembolic event of the relatives.
Venepuncture was performed in each participant. Blood samples were collected from the antecubital vein in 1/10 vol of 0.11 mmol/L trisodium citrate. Plasma was prepared by centrifugation for 10 minutes at 2,000g at 10°C and stored at −70°C until use. Antithrombin antigen concentration was measured by immunoelectropheresis according to the method of Laurell.13Amidolytic heparin cofactor assays (Chromogenix, Mölndal, Sweden) were used for antithrombin activity measurement. Genomic DNA was isolated from blood leukocytes by standard methods. DNA analysis in 9 of the 14 families had elucidated different defects in the antithrombin gene in 7 families.14 Genetic analysis for the prothrombin 20210 A allele (PT20210A) and Factor V Leiden (FVL) was performed as described previously.15,16 Available DNA samples of 12 families had been screened in a collaborate study described elsewhere.12
The occurrence of venous thrombosis was assessed for antithrombin-deficient subjects and nondeficient subjects. In all analyses of relative risks and risk factors for thrombosis, the probands were excluded to eliminate bias. Median age of onset and thrombosis-free survival curves were constructed according to the Kaplan and Meier method. To compare the 2 curves, we used the logrank rest, resulting in a χ2 distribution with 1 degree of freedom. Confidence intervals for the thrombosis-free survival rates were calculated based on a binomial distribution.
The incidence of first thrombotic events in antithrombin-deficient subjects and nondeficient subjects was calculated by counting patient-years of observation and dividing the number of events in each group by the sum of observation-years of all the individuals in the group. Similarly, incidence rates were calculated as the number of thromboses in the years that surgery, immobilization (including hospital admissions, plaster casts, and immobilization longer than 2 weeks), pregnancy, and the postpartum period took place. The time window was 1 year, and incidence rate ratios were calculated as the incidence rate in 1 year over the incidence rate in all other years. CIs for incidences and incidence rate ratios were calculated by the assumption of a Poisson distribution. Multivariate analysis was performed using the Poisson method for aggregate data. With multivariate analysis, it is possible to determine the effect of one variable, while the other variables are adjusted for.
RESULTS
Diagnosis and thrombotic events (relatives only).
In all 14 families affected, individuals had antithrombin activity and antigen levels less than 80 U/mL (type I antithrombin deficiency). Of 107 eligible family members, 90 individuals (84%) participated: 5 nonrespondents lived abroad and 3 subjects were in poor health; 6 asymptomatic individuals, of whom 4 had been tested as nondeficient before, were not interested in further investigations and 3 family members could not be contacted because the proband had no contacts. In total, 46 individuals proved to be antithrombin-deficient (19 men and 27 women; average age, 43 years; age range, 15 to 88 years); 44 individuals were normal (23 men and 21 women; average age, 44 years; age range, 18 to 86 years). Before this study, the diagnosis of antithrombin deficiency was known to 67% of all participants.
Of 46 antithrombin-deficient individuals, 18 subjects had experienced 1 or more venous thromboembolic events. The first clinical manifestation was mostly deep venous thrombosis of the legs (12/18); 1 individual presented with symptoms of pulmonary embolism, whereas 5 individuals presented with manifestations of pulmonary embolism and deep venous thrombosis. One of 44 nondeficient individuals had experienced venous thromboembolism.
Precipitating risk factors.
Only 2 first episodes (2/18) occurred apparently spontaneously. Before 16 first thromboembolic episodes, 1 or 2 of the following risk factors were present: postpartum period (n = 4), surgery (n = 4), immobilization (n = 1), plaster cast (n = 2), hospital admission (n = 1), oral contraceptive use (n = 2), long travel by air (n = 3), and FVL or PT20210A (n = 5). The 1 nondeficient individual who had experienced venous thrombosis had had recent surgery and proved to be a carrier of FVL.
Overall, there were no differences in exposure to predisposing acquired risk factors between antithrombin-deficient individuals and normal individuals (surgery/trauma, immobilization and for women oral contraceptive use, pregnancy, and childbirth). Additional genetic factors, FVL and PT20210A, were found in 7 of the 14 families.
Risk of venous thromboembolism.
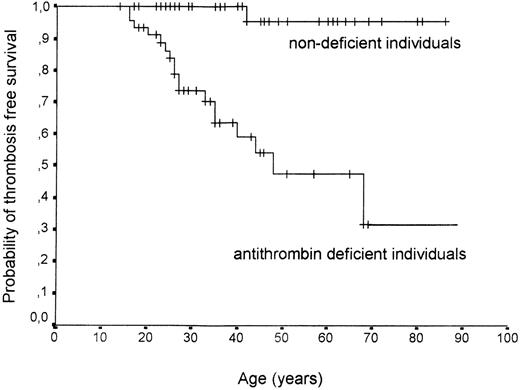
The median age of onset was 27 years (range, 16 to 68 years) for antithrombin-deficient individuals (the age of onset was 42 years of age for the symptomatic individual without antithrombin deficiency). Notably, the median age of onset for carriers of 2 defects was 17 years (range, 16 to 25 years). According to Kaplan and Meier survival analysis, the median thrombosis-free survival for antithrombin-deficient individuals was 48 years (Fig 1). Overall, men more often experienced venous thromboembolism than women: 9 of 19 men (47%; median age of onset, 27 years; range, 16 to 48 years), whereas 9 of 27 women were symptomatic (33%; median age of onset, 26 years; range, 16 to 68 years).
Venous thrombosis-free survival curve in antithrombin-deficient individuals and nondeficient individuals (probands excluded). Probability of freedom from venous thrombotic events is presented. Steps in curves indicate events; short vertical lines indicate censoring.
Venous thrombosis-free survival curve in antithrombin-deficient individuals and nondeficient individuals (probands excluded). Probability of freedom from venous thrombotic events is presented. Steps in curves indicate events; short vertical lines indicate censoring.
The incidence of (first) thrombotic event was 1.1% per year (95% CI, 0.7% to 1.8%) in the antithrombin-deficient individuals, which is more than 20 times greater than among nondeficient individuals (0.05% per year; 95% CI, 0.01% to 0.4%). The incidence of first thrombotic events was equal in men and women up to 25 years of age (0.7% per year in men v 0.6% per year in women); after 25 years of age, incidence was twice as high in men as in women (at 26 to 45 years of age, 3.0% per year in men v 1.7% per year in women; at >46 years of age, 2.2% per year in men v 1.4% per year in women).
Interaction with other risk factors.
We compared the annual incidence of venous thromboembolism in relatives with exposure to other genetic and acquired risk factors. The risk among antithrombin-deficient subjects exposed to surgery (12.7% per year; 95% CI, 5.7% to 28.4%) was much larger than the increased risk of antithrombin deficiency (0.8% per year; 95% CI, 0.4% to 1.4%) or surgery (1.6% per year; 95% CI, 0.2% to 11.3%) separately. Table 1 shows that, overall, the incidence rates were less than 1% per year for individuals exposed to inherited antithrombin deficiency only. Among those with exposure to 2 genetic defects, the incidence rate increased to 4.6% per year (95% CI, 1.9% to 11.1%). Combined exposure to antithrombin deficiency and an acquired risk situation led to even higher incidence rates of 20.3% in the year of the risk event (95% CI, 12.0% to 34.3%).
Incidences of Venous Thromboembolism: Exposure to Inherited Antithrombin Deficiency and the Effect of Acquired or Genetic Risk Factors (Men and Women, Univariate)
| Acquired Risk Factor* . | Antithrombin Deficiency . | Years . | Patient . | VT† (%/yr) . | Ic† (95% CI) . |
|---|---|---|---|---|---|
| + | + | 69 | 14 | 20.3 | (12.0-34.3) |
| + | − | 81 | 1 | 1.2 | (0.2-8.8) |
| − | + | 1,534 | 4 | 0.3 | (0.1-0.7) |
| − | − | 1,820 | 0 | 0 | |
| Other Genetic Risk Factor‡ | Antithrombin Deficiency | Years | Patient | VT† (%/yr) | Ic† (95% CI) |
| + | + | 108 | 5 | 4.6 | (1.9-11.1) |
| + | − | 401 | 1 | 0.3 | (0.1-1.8) |
| − | + | 1,495 | 13 | 0.9 | (0.5-1.5) |
| − | − | 1,500 | 0 | 0 |
| Acquired Risk Factor* . | Antithrombin Deficiency . | Years . | Patient . | VT† (%/yr) . | Ic† (95% CI) . |
|---|---|---|---|---|---|
| + | + | 69 | 14 | 20.3 | (12.0-34.3) |
| + | − | 81 | 1 | 1.2 | (0.2-8.8) |
| − | + | 1,534 | 4 | 0.3 | (0.1-0.7) |
| − | − | 1,820 | 0 | 0 | |
| Other Genetic Risk Factor‡ | Antithrombin Deficiency | Years | Patient | VT† (%/yr) | Ic† (95% CI) |
| + | + | 108 | 5 | 4.6 | (1.9-11.1) |
| + | − | 401 | 1 | 0.3 | (0.1-1.8) |
| − | + | 1,495 | 13 | 0.9 | (0.5-1.5) |
| − | − | 1,500 | 0 | 0 |
Surgery, trauma, plaster cast, hospital admittance, immobilization more than 2 weeks before thrombosis. A time window of 1 year after the acquired risk situation was used.
Episodes of venous thromboembolism (VT), incidence rates per 100 patient years with 95% confidence intervals.
Factor V Leiden or PT20210A.
For women, exposure to pregnancy, the postpartum period, and use of oral contraceptives were analyzed separately (women only). Use of oral contraceptives by antithrombin-deficient women was associated with an incidence rate of 4.1% per year (95% CI, 1.0% to 16.3%); the postpartum period conferred the highest risk for women (incidence rate of 14.3% per year; 95% CI, 1.0% to 16.3%). When we looked at pregnancies and postpartum periods in hitherto asymptomatic women without anticoagulation prophylaxis, no pregnancies (0/28) but 15% of postpartum periods (4/27) were complicated by venous thromboembolism (Table 2). During pregnancy, only 1 antithrombin-deficient woman developed recurrences of venous thrombosis (twice, in 2 pregnancies). Pregnancies and postpartum periods of symptomatic antithrombin-deficient women, without anticoagulant prophylaxis, were complicated frequently by venous thromboembolism, ie, 20% (2/10 pregnancies) and 50% (4/8 postpartum periods), respectively (Table 2).
Pregnancies, Postpartum Periods, and Number of Miscarriages
| . | Antithrombin Deficient . | No Antithrombin Deficiency . | ||
|---|---|---|---|---|
| All . | Symptomatic . | |||
| No . | Yes . | |||
| All women | 27 | 18 | 9 | 21 |
| Women ever with miscarriage | 9 | 5 | 4 | 5 |
| No. of miscarriages | 9 | 5 | 4 | 7* |
| Women ever with abortion | 2 | 2 | 0 | 0 |
| No. of abortions | 2 | 2 | 0 | 0 |
| Women ever pregnant | 17 | 11 | 6 | 15 |
| No. of pregnancies | 45 | 34 | 11 | 49 |
| Pregnancies without anticoagulant therapy† | 38 | 28 | 10 | 49 |
| With thrombosis‡ | 2 (5%) | 0 (0%) | 2 (20%) | 0 (0%) |
| No. of postpartum periods | 45 | 34 | 11 | 49 |
| Postpartum periods without anticoagulant therapy† | 35 | 27 | 8 | 47 |
| Postpartum periods with thrombosis2-153 | 8 (23%) | 4 (15%) | 4 (50%) | 0 (0%) |
| . | Antithrombin Deficient . | No Antithrombin Deficiency . | ||
|---|---|---|---|---|
| All . | Symptomatic . | |||
| No . | Yes . | |||
| All women | 27 | 18 | 9 | 21 |
| Women ever with miscarriage | 9 | 5 | 4 | 5 |
| No. of miscarriages | 9 | 5 | 4 | 7* |
| Women ever with abortion | 2 | 2 | 0 | 0 |
| No. of abortions | 2 | 2 | 0 | 0 |
| Women ever pregnant | 17 | 11 | 6 | 15 |
| No. of pregnancies | 45 | 34 | 11 | 49 |
| Pregnancies without anticoagulant therapy† | 38 | 28 | 10 | 49 |
| With thrombosis‡ | 2 (5%) | 0 (0%) | 2 (20%) | 0 (0%) |
| No. of postpartum periods | 45 | 34 | 11 | 49 |
| Postpartum periods without anticoagulant therapy† | 35 | 27 | 8 | 47 |
| Postpartum periods with thrombosis2-153 | 8 (23%) | 4 (15%) | 4 (50%) | 0 (0%) |
One woman had 3 missed abortions.
Prophylactic anticoagulant therapy was used during 7 pregnancies and 10 postpartum periods of antithrombin-deficient women and during 2 postpartum periods of nondeficient women.
One woman suffered recurrent thrombosis in her second and third pregnancy.
Four episodes were first events and 4 episodes were recurrences of thromboembolic events.
Multivariate analysis.
The incidence rate ratios computed with multivariate analysis by Poisson analysis are listed in Table 3. For each factor, the relative risk is shown compared with the absence of that factor, which is adjusted for all other variables. In these families, the most prominent risk factor is antithrombin deficiency, increasing the incidence 26-fold in multivariate analysis. Other genetic risk factors (FVL and PT20210A) were strong risk factors, too, with relative risks of 5 to 7. Well-established acquired risk factors, such as surgery and immobilization, were associated with a relative risk of 10. For women, the postpartum state accounted for the highest relative risk when recalculated to an annual risk (Table 3). These results were almost comparable to our univariate analysis; due to small numbers, unfortunately, the estimates for interaction between risk factors could not be calculated.
Adjusted Incidence Rate Ratios for Potential Genetic and Acquired Risk Factors (Multivariate by Poisson Analysis)
| Risk Factor . | Incidence Rate Ratio (95% CI)3-150 . |
|---|---|
| Antithrombin deficiency | 25.9 (3.1-216) |
| 20210 A allele | 4.6 (0.9-21.4) |
| FVL | 7.2 (1.9-27.6) |
| Surgery, immobilization3-151 | 10.9 (3.9-29.8) |
| Pregnancy and postpartum state3-152 | 48.6 (9.1-260.7) |
| Use of oral anticonceptives3-152 | 5.3 (0.6-48.1) |
| Risk Factor . | Incidence Rate Ratio (95% CI)3-150 . |
|---|---|
| Antithrombin deficiency | 25.9 (3.1-216) |
| 20210 A allele | 4.6 (0.9-21.4) |
| FVL | 7.2 (1.9-27.6) |
| Surgery, immobilization3-151 | 10.9 (3.9-29.8) |
| Pregnancy and postpartum state3-152 | 48.6 (9.1-260.7) |
| Use of oral anticonceptives3-152 | 5.3 (0.6-48.1) |
The incidence rate ratios are adjusted for age, calendar time, and sex.
Surgery, trauma, plaster cast, hospital admittance, immobilization more than 2 weeks before thrombosis.
Women only in regression analysis.
Thrombotic disease in the probands.
In all prior analyses, the probands were excluded to avoid ascertainment bias. In probands, severity of disease was indeed impressive: the 14 probands of these families, 9 men and 5 women (average age, 51 years; age range, 24 to 77 years) had all suffered recurrent thromboembolism. The median age of onset was 33 years of age (age range, 19 to 55 years). One proband presented spontaneously with mesenterial thrombosis, and 1 proband developed mesenterial thrombosis as a recurrence after surgery. The most frequent clinical presentation was deep venous thrombosis of the leg with pulmonary embolism.
Six of 14 episodes of onset (43%) and 9 of 19 recurrences (47%) had occurred in the absence of an additional precipitating risk factor. An additional genetic defect, FVL, was identified in 1 female proband only. Acquired risk factors such as surgery and immobilization were the precipitating risk factor in men. Among the female probands, pregnancy, postpartum period, and oral contraceptive use were present before two thirds of all episodes (onset and recurrences). Four female probands had developed venous thromboembolism within 3 months after first prescription of oral contraceptives.
DISCUSSION
Venous thromboembolism is a multicausal disorder. Age, surgery, immobilization, oral contraceptive use, and postpartum state are well-known predisposing factors for venous thromboembolism. In thrombophilia families, the genetic and environmental factors interact to bring about venous thrombosis. This family study showed a 20-fold increased risk for venous thromboembolism in antithrombin-deficient individuals versus nondeficient individuals. The risks became extremely high in the simultaneous presence of other genetic or environmental risk factors.
Acquired and genetic risk factors were often present simultaneously at the onset of thrombosis. The annual incidence increased 10- to 20-fold among individuals who had been exposed to an acquired risk factor and inherited antithrombin. The incidence rate was less than 1% per year among individuals exposed to inherited antithrombin deficiency only. Thus, environmental risk factors lead to interaction as the effect of antithrombin deficiency and environmental risk factors together was greater than the sum of the effect of each of these risk factors separately (Table 1). Similarly, a 5-fold increase of the annual incidence was found due to gene-gene interactions. Summarized, both gene-environmental interactions and gene-gene interactions play an important role in the onset of venous thromboembolism in inherited antithrombin deficiency.
Most families in this study were referred to our center, therefore representing high-risk families. Overall, our risk estimates should be viewed as the risks for antithrombin-deficient individuals, who are thrombosis-prone and referred for thrombophilia work-up. Families with inherited antithrombin deficiency selected differently may very well display different, ie, lower, risks.
When thrombophilia is viewed as a multicausal disorder, highly thrombosis-prone families are identified, because common genetic defects are present simultaneously in those families. In this study, DNA analysis showed the presence of 2 common genetic factors in 7 of the 14 families with inherited antithrombin deficiency. When thrombosis occurred in a patient at a young age, an additional genetic defect, the FVL or PT20210A, was most often present. In the other individuals, interaction with environmental risk factors had led to high risks. Although these risk factors are not genetic, they may, even when present coincidentally, make a family stand out that is then recognized as thrombophilic.
It is believed that antithrombin deficiency confers a higher risk than protein C, protein S, and FVL. Again, a comparison between families seems only justified when the investigated families are selected under similar criteria. Lensen et al8 showed that, when uniform selection criteria were applied, no differences in median age of onset were observed between selected families with protein C deficiency or activated protein C (APC) resistance. The selection criteria used in the study by Lensen et al8 were similar to the criteria of our selection of families with inherited antithrombin deficiency. After making a comparison, the median ages of onset in our antithrombin-deficient families approximated the median ages of onset of families with protein C deficiency and APC resistance. The median age of onset was 26 years (range, 16 to 50 years) for probands and 35 years (range, 17 to 65 years) for relatives with protein C deficiency; in high-risk families with APC resistance, the median age of onset was, respectively, 29.5 years (range, 21 to 46 years) and 29 years (range, 16 to 63 years); in our families, the median age of onset was, respectively, 33 years (range, 19 to 55 years) and 27 years (range, 16 to 68 years). The median ages of onset in protein C deficiency, APC resistance, and antithrombin deficiency suggest that differences between thrombophilia disorders may be minor compared with the effect of selection.
We also compared our data with a study of families with protein C deficiency, in which the applied selection criteria were again quite similar.17 The risk estimates comprised a 9 times higher incidence of venous thrombosis among protein C-deficient individuals than among nondeficient individuals (crude odds ratio, 9.2; 95% CI, 5 to 16.8); the age-related incidence rates were a little lower, but the incidence rates after surgery (incidence rate ratio, 9.2; 95% CI, 3.5 to 24.9) differed little from the incidence rates in the antithrombin-deficient families. We suggest that antithrombin deficiency is not different from protein C deficiency or other thrombophilia disorders: the risk of antithrombin deficiency is often enhanced simultaneously by other factors, both environmental and genetic. For that reason too, the risk of inherited antithrombin deficiency is unlikely to be much higher than for the other deficiencies, because, in that case, there would be no or less need for additional enhancing risk factors.
For this study, we only included the thromboembolic episodes that required hospitalization and treatment with anticoagulant therapy. The detailed history of thromboembolic diseases was obtained using a standardized questionnaire, which was proven to be a valuable tool for the diagnosis of personal past episodes of venous thromboembolism.18 The majority of the clinically suspected first episodes of venous thromboembolism (71%) were confirmed by reliable objective tests. It seems likely therefore that our data are accurate and not overestimated. The probands were rightly excluded from the analysis because of ascertainment bias. Their clinical manifestations pointed to a higher (recurrence) risk of venous thromboembolism. It was remarkable that we observed almost no additional genetic defects in the probands. Given their impressive thrombotic histories, additional yet unknown factors seem likely.
We studied the highly thrombosis-prone and referred families. The heterogeneity of the molecular basis of antithrombin deficiency in these families was in accordance with reported mutations in other families.14 In the absence of other risk factors, we found that the annual incidence was less than 1% per year. This implies that, even in the worst case, lifelong prophylactic therapy cannot be justified, because higher annual risks of bleeding complications have been consistently reported.19 20 In contrast, with gene-environmental interaction, incidence rates in high-risk situations exceeded the reported risks of bleeding complications. The use of prophylaxis has to be considered carefully but seems indicated as short-term prophylactic anticoagulant therapy in all high-risk situations. The postpartum period showed to be the most prominent acquired risk factor for onset of venous thromboembolism in women. The risk was also greater in the puerperium than during pregnancy (Table3). Based on these data, adequate prophylactic anticoagulant therapy for asymptomatic pregnant women may be confined to the postpartum state only.
In conclusion, venous thromboembolism in inherited antithrombin deficiency proved to be multicausal. Inherited antithrombin deficiency was a strong risk factor. In the presence of other precipitating risk factors, interactive effects strongly determined the risk of thrombosis for an individual. In selected families with young symptomatic family members, additional genetic factors should be assessed. The risks of acquired risk factors should be considered and adequate prophylactic anticoagulant therapy seems indicated only during high-risk situations. Further study is needed to assess whether similar risks are found in unselected families.
ACKNOWLEDGMENT
The authors are grateful to Dr H.R. Büller, Dr J.W. ten Cate, and Dr M.V. Huisman for permitting us to study a family with inherited antithrombin deficiency. We thank E.W.M. Vogels and S.R. Poort, who performed the DNA analysis.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to F.R. Rosendaal, MD, Department of Clinical Epidemiology, University Hospital, Bldg 1, CO-P45, PO Box 9600, 2300 RC Leiden, The Netherlands.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal