Abstract
Hydroxychloroquine (HCQ), a lysosomotropic amine, is an immunosuppressive agent presently being evaluated in bone marrow transplant patients to treat graft-versus-host disease. While its immunosuppressive properties have been attributed primarily to its ability to interfere with antigen processing, recent reports demonstrate HCQ also blocks T-cell activation in vitro. To more precisely define the T-cell inhibitory effects of HCQ, the authors evaluated T-cell antigen receptor (TCR) signaling events in a T-cell line pretreated with HCQ. In a concentration-dependent manner, HCQ inhibited anti-TCR–induced up-regulation of CD69 expression, a distal TCR signaling event. Proximal TCR signals, including inductive protein tyrosine phosphorylation, tyrosine phosphorylation of phospholipase C γ1, and total inositol phosphate production, were unaffected by HCQ. Strikingly, anti-TCR-crosslinking–induced calcium mobilization was significantly inhibited by HCQ, particularly at the highest concentrations tested (100 μmol/L) in both T-cell lines and primary T cells. HCQ, in a dose-dependent fashion, also reduced a B-cell antigen receptor calcium signal, indicating this effect may be a general property of HCQ. Inhibition of the calcium signal correlated directly with a reduction in the size of thapsigargin-sensitive intracellular calcium stores in HCQ-treated cells. Together, these findings suggest that disruption of TCR-crosslinking–dependent calcium signaling provides an additional mechanism to explain the immunomodulatory properties of HCQ.
Graft-versus-host disease (GvHD) is a significant cause of morbidity and mortality in allogeneic bone marrow transplantation. While the pathogenesis of GvHD is not fully understood, activated T cells are likely to mediate this process. In GvHD, T-cell activation occurs following recognition of host antigens through the T-cell antigen receptor (TCR) on donor T cells. Many pharmacologic agents used to prevent and treat GvHD inhibit T-cell activation and/or remove T cells from the circulation. These agents include glucocorticoids, cyclosporin A (CsA), anti-thymocyte globulin, and methotrexate. These drugs have been used alone or in combination with varying degrees of success, and each is associated with potentially significant side effects owing to systemic toxicity.
Hydroxychloroquine (HCQ) is a 4-aminoquinoline antimalarial drug that has been used for many years to treat autoimmune disorders.1 HCQ exhibits relatively limited systemic toxicity with extended use at doses at or below 6.5 mg/kg per day, or up to 12 mg/kg per day for 2 years. A recent clinical trial suggests this agent may be useful for the treatment of chronic GvHD.2 The immunosuppressive properties of HCQ relate, in part, to its interference with normal antigen processing and presentation. In vitro, HCQ appears to alter antigen processing by increasing the pH of intracellular vacuoles, resulting in dissociation of the invariant chain from the major histocompatibility complex class II molecule and inhibition of antigen binding.3 More recently, HCQ has also been shown to block proliferative responses to T-cell mitogens and alloantigens and to reduce the release of various cytokines, including interleukin (IL)-6 and tumor necrosis factor.4 5 These recent findings suggest that HCQ may function as an immunosuppressant by blocking one or more steps in the T-cell–activation pathway.
TCR engagement with antigen, or experimentally with anti-TCR antibodies, results in the initiation of a signal transduction cascade (or cascades) leading to T-cell activation. The earliest measurable biochemical events in this cascade are activation of nonreceptor protein tyrosine kinases (PTKs), including p56lck, p59fyn, and ZAP-70. This is followed by tyrosine phosphorylation of multiple intracellular substrates, including SLP-76, LAT, VAV, SHC, and phospholipase C (PLC) γ1.6,7 Phosphorylation of PLCγ1 enhances its catalytic activity, leading to hydrolysis of phosphatidylinositol 4,5-bisphosphate (PIP2) to inositol 1,4,5-triphosphate (IP3) and diacylglycerol.8 These “second messengers” lead to an increase in intracellular calcium and activation of protein kinase C (PKC), respectively. Elevated intracellular calcium levels are crucial for the activation of calmodulin, which binds to and activates the serine phosphatase calcineurin. Calcineurin, a primary target of CsA, controls the nuclear translocation of transcription factors of the NFAT (nuclear factor of activated T cells) family.9 Downstream events following NFAT activation include up-regulation of CD69 (an early activation marker) and production and secretion of IL-2.
The present study was undertaken to determine if the immunomodulatory properties of HCQ are mediated through inhibition of specific TCR-crosslinking–dependent signaling events. We demonstrate that HCQ, in a dose-dependent manner, inhibits TCR-mediated calcium mobilization and other downstream events, including CD69 expression. In contrast, calcium-independent proximal TCR signaling events, including inductive protein tyrosine phosphorylation, mitogen-associated protein (MAP) kinase phosphorylation, and production of inositol phosphates, appear to be unaffected by HCQ. Because the site of action of HCQ is distinct from that of other immunosuppressive agents, HCQ may have synergistic properties when used in combination with other immunosuppressants, leading to an enhanced anti-GvHD effect.
Materials and methods
Reagents
Hydroxychloroquine was kindly provided by Sanofi Pharmaceuticals (New York, NY) and solubilized in sterile water. Phorbol 12-myrisate 13-acetate (PMA) (Sigma, St Louis, MO) was used at 50 ng/mL, while thapsigargin (Gibco/BRL, Coon Rapids, MN) was used at 1 μmol/L. Anti-TCR monoclonal antibody (mAb) C305 ascites, clonotypic for the TCR expressed on Jurkat cells, was generously provided by A. Weiss (University of California, San Francisco). Commercial antibodies included anti-CD69 (Leu23a) (Becton Dickinson, Mountain View, CA), biotinylated anti-CD3 (OKT3) (PharMingen, San Diego, CA), fluorescein isothiocyanate (FITC)–conjugated goat antimouse secondary antibody (Cappel, West Chester, PA), polyclonal antiphosphotyrosine antibody (4G10) (Upstate Biotechnology, Lake Placid, NY), polyclonal rabbit antirat ERK-2 (Upstate Biotechnology), mixed mouse monoclonal antibovine PLCγ1 (Upstate Biotechnology), rabbit and goat antimouse immunoglobulin (Jackson Immunoresearch Laboratories, West Grove, PA), and a horseradish peroxidase (HRPO)–conjugated rabbit antimouse antibody (Bio-Rad, Chicago, IL).
Cells
Jurkat T cells (clone E6-1) and Ramos B cells (American Type Culture Collection, Rockville, MD) were maintained in complete RPMI medium (10% fetal calf serum, penicillin 1000 U/mL, streptomycin 1000 U/mL, and glutamine 20 mmol/L). Human peripheral blood mononuclear cells (PBMCs) from healthy volunteers were isolated by Ficoll-Hypaque gradient centrifugation. Following isolation, cells were plated at a density of 1 to 2 × 106/mL and left in tissue culture flasks at 37°C in 5% CO2 for 2 hours to remove adherent cells.
Flow cytometry and CD69 expression
Jurkat cells were pretreated with HCQ for 24 hours and then stimulated with RPMI alone (control), PMA (50 ng/mL), or C305 (1:2000) for an additional 24 hours. Cells were then washed and stained with FITC-conjugated anti-CD69, and fluorescence intensity was measured on a FACScan (Becton Dickinson).
Analysis of intracellular free calcium concentration
Jurkat T cells or Ramos B cells were loaded with the calcium-sensitive indicator dye calcium green-1-am(C-3012) (Molecular Probes, Eugene, OR) 5 μg/mL, in RPMI (10 mmol/L HEPES, 2% fetal calf serum) for 30 minutes at 37°C. Excess dye was washed away with Hanks' Balanced Salt Solution (HBSS) supplemented with 1.3 mmol/L CaCl2 supplemented with 10 mmol/L HEPES). Loaded cells were resuspended in HBSS and kept at 4°C and protected from light prior to analysis. Intracellular calcium measurements were monitored by the use of 530 nm fluorescence emission following 506 nm excitation by means of a bulk spectrofluorimeter (Photon Technology International, Monmouth Junction, NJ). Following 20 seconds of data acquisition, 5 × 105 Jurkat/mL was activated by the addition of anti-TCR mAb C305 (1:2000 dilution of ascites fluid), and Ca++ mobilization was monitored. Ramos B cells were activated by addition of 10 μg/mL of goat anti-immunoglobulin (Ig)M antibody (2020-01) (Southern Biotech, Birmingham, AL). Residual peak calcium response was evaluated by addition of 1 μmol/L ionomycin. Thapsigargin-sensitive calcium stores were evaluated in the presence of 4 mmol/L egtazic acid (EGTA) by addition of 1 μmol/L thapsigargin (586005) (Calbiochem, San Diego, CA). For calcium studies in primary human T cells, HCQ-treated or untreated PBMCs (5 × 107/mL) were loaded with calcium green-1-AM and fura-red-AM (F3021) (Molecular Probes) at a final dye concentration of 10 μmol/L for 30 minutes at 37°C. Loaded cells were washed once in calcium buffer (25 mmol/L HEPES, 125 mmol/L NaCl, 5 mmol/L KCl, 1 mmol/L Na2HPO4, 0.1% glucose, 500 μmol/L MgCl2, 10 mmol/L CaCl2, 0.1% bovine serum albumin, pH 7.4), resuspended at 1.5 × 106/mL in calcium buffer, and immediately placed on ice. Prior to activation, cells were warmed to 37°C for 15 minutes. Following 30 seconds of data acquisition, cells were activated by addition of biotinylated anti-CD3 (40 μg/mL), followed after 10 seconds by avidin (10 μg/mL). The calcium green versus fura-red fluorescence ratio of individual cells was measured by means of a FACScan flow cytometer (Becton Dickinson) before and after the addition of activators and analyzed by means of the FlowJo FACS software. Data are presented in arbitrary units as a function of fluorescence (relative intracellular calcium) versus time.
Notably, initial measurements of intracellular calcium made with the UV-light–excitable calcium indicator dyes fura-2 or indo-1 were found to be unreliable owing to interference of HCQ with either the excitation or the emission properties of these dyes (data not shown). Briefly, with the use of fura-2–loaded Jurkat cells, excitation scan analysis of HCQ-treated cells indicated a significantly reduced absorbance, between approximately 300 nm and 350 nm. Because the calcium-bound excitation occurs at approximately 340 nm, this artifact led to an underestimate of intracellular free Ca++concentrations. With the use of indo-1–loaded cells, emission scan analysis of HCQ-treated cells (or of free HCQ in HBSS) indicated that HCQ emits intensely from approximately 375 nm to 425 nm. Because the calcium-bound emission of this indicator occurs at approximately 400 nm, this artifact would lead to an overestimate of intracellular free Ca++. In contrast to these findings, HCQ did not interfere with either calcium-bound or unbound excitation or emission spectra of either calcium green-1 or fura-red (data not shown). For this reason, calcium green-1, or calcium green-1 and fura-red, were used as the indicator dyes for all the experiments described.
Measurement of soluble inositol phosphate generation
Jurkat cells were incubated with various concentrations of HCQ for 24 hours, then loaded with [3H] myoinositol (40 μCi/mL) (Amersham, Arlington Heights, IL) for 3 hours in phosphate-buffered saline. Duplicate samples were stimulated with media alone (control) or C305 (1:2000) for 10 minutes, then lysed in a 1:1 mixture of chloroform/methanol. Soluble inositol phosphates were extracted and separated by anion exchange as previously described and were quantified by liquid scintillation counting.10
Immunoprecipitation and Western blotting
Following stimulations, Jurkat cells were pelleted, supernatant aspirated, and 1× lysis buffer (1% NP-40, 150 mmol/L NaCl, 20 mmol/L Tris base, pH 7.4) containing protease (50 mg/mL aprotinin, 10 mg/mL leupeptin, 50 mg/mL pepstatin A, 1 mmol/L PMSF) and phosphatase (400 mmol/L sodium orthovanadate, 10 mmol/L sodium fluoride, 10 mmol/L sodium pyrophosphate) inhibitors was added to a final concentration of 5 × 107 cells/mL. Samples were left on ice for 30 minutes and were centrifuged at 12 000g for 15 minutes, and supernatant was saved. For immunoprecipitation of PLCγ1, 40 μL of protein A (Sigma) was prearmed with 5 μL rabbit antimouse immunoglobulin overnight at 4°C. The prearmed protein A and 1 μL of anti-PLCγ1 were added simultaneously to the clarified lysate and rotated for 2 hours at 4°C. Immunoprecipitated complexes were washed 5 times in ice-cold lysis buffer. For PLCγ1 immunoprecipitates, a fraction was immunoblotted with either anti-PLCγ1 (5 × 106 cell equivalents) or antiphosphotyrosine (2 × 107 cell equivalents). In experiments examining inductive protein tyrosine phosphorylation or phosphorylation of MAP kinase, whole-cell lysates were prepared by pelleting rapidly 106 cells and lysing in 1× sodium dodecyl sulfate sample (SDS) buffer. Immunoprecipitates or proteins from whole-cell lysates were subjected to SDS–polyacrylamide gel electrophoresis (SDS-PAGE) and transferred electrophoretically to nitrocellulose paper. Nitrocellulose membranes were blocked 2 hours in a Tris-buffered saline solution containing 3% bovine serum albumin, and primary antibodies were added for 4 hours at 4°C. Immunoreactive bands were visualized by means of enhanced chemiluminescence (Amersham) or BCIP/NBT (Promega, Madison, WI) according to the manufacturer's instructions.
Results
HCQ inhibits TCR-activation–induced CD69 expression
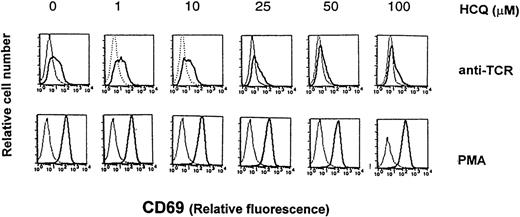
Initial experiments were undertaken in Jurkat cells, a human leukemic T-cell line, to determine whether HCQ alters downstream TCR-signal-transduction–dependent events. Cells were preincubated for 24 hours in the presence of various concentrations of HCQ, stimulated an additional 24 hours with clonotypic anti-TCR mAb (C305) or phorbol esters (PMA), then assayed for up-regulation of CD69 by flow cytometry. Up-regulation of CD69 provides a quantitative measure of T-cell activation and occurs 12 to 24 hours following TCR ligation or PKC activation with PMA.11 12 In non–HCQ-treated control cells, C305 up-regulated CD69 receptor expression, as indicated by an approximately 0.5 log shift in mean fluorescence intensity compared with untreated controls (Figure 1). Treating cells with increasing concentrations of HCQ resulted in a 60%-80% reduction in the expression of CD69 following anti-TCR stimulation. In contrast, PMA markedly up-regulated CD69 receptor expression (∼1.5 log shift; Figure 1, lower panel), although HCQ treatment had minimal effect on this TCR-independent event. Notably, HCQ also exerted no appreciable effect on cell viability during the course of these experiments, even at high concentrations (100 μmol/L HCQ), and no alterations were noted in the level of cell surface expression of TCR/CD3, CD4, and CD45 (data not shown).
HCQ down-regulates TCR-induced CD69 expression.
Jurkat T cells were cultured for 24 hours with varying concentrations of HCQ, then incubated an additional 12 hours in 24-well plates (1 × 106/mL) in medium alone (dotted lines), PMA (50 ng/mL), or anti-TCR mAb C305 (ascites, 1:2000). Cells were then harvested and stained with FITC-conjugated anti-CD69, and fluorescence intensity was measured on a FACScan. Cell counts and viability were indistinguishable in untreated and HCQ-treated cell populations. Representative data from more than 5 similar experiments are shown.
HCQ down-regulates TCR-induced CD69 expression.
Jurkat T cells were cultured for 24 hours with varying concentrations of HCQ, then incubated an additional 12 hours in 24-well plates (1 × 106/mL) in medium alone (dotted lines), PMA (50 ng/mL), or anti-TCR mAb C305 (ascites, 1:2000). Cells were then harvested and stained with FITC-conjugated anti-CD69, and fluorescence intensity was measured on a FACScan. Cell counts and viability were indistinguishable in untreated and HCQ-treated cell populations. Representative data from more than 5 similar experiments are shown.
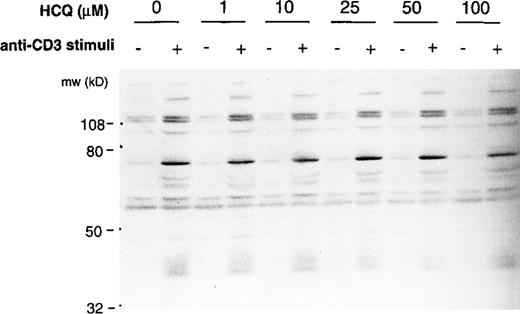
HCQ does not inhibit anti-TCR–induced protein tyrosine kinase activation, tyrosine phosphorylation of PLCγ1, or inositol phosphate production
The observation that HCQ significantly inhibited TCR-dependent CD69 up-regulation but did not interfere with PMA-induced CD69 expression suggested a block in the TCR signal transduction cascade. We initially determined if HCQ-mediated inhibition of TCR signals was a consequence of limited PTK activation or of a reduced capacity to phosphorylate critical protein substrates. To assay PTK activation, proteins from detergent lysates of resting or anti-TCR–stimulated Jurkat cells were separated by SDS-PAGE, transferred to nitrocellulose, and immunoblotted with antiphosphotyrosine antibodies. Pretreating cells with HCQ for 24 hours did not appreciably alter the magnitude, global pattern, or kinetics of anti-TCR–induced protein tyrosine phosphorylation (Figure2 and data not shown). These results suggested that the PTKs operative in proximal TCR signaling were largely intact in HCQ-treated cells.
HCQ does not inhibit TCR-mediated inductive protein tyrosine phosphorylation.
Jurkat T cells (1 × 106) were treated with varying concentrations of HCQ for 24 hours, stimulated with C305 for 5 minutes, and then lysed in NP-40 detergent. Proteins from whole-cell lysates were separated by 10% SDS-PAGE, transferred to nitrocellulose, and immunoblotted with antiphosphotyrosine antibody (4G10). Immunoreactive bands were visualized by enhanced chemiluminescence. Representative data from more than 3 similar experiments are shown. A more extended kinetic analysis of protein tyrosine phosphorylation in untreated and HCQ-treated cell populations gave similar results (data not shown).
HCQ does not inhibit TCR-mediated inductive protein tyrosine phosphorylation.
Jurkat T cells (1 × 106) were treated with varying concentrations of HCQ for 24 hours, stimulated with C305 for 5 minutes, and then lysed in NP-40 detergent. Proteins from whole-cell lysates were separated by 10% SDS-PAGE, transferred to nitrocellulose, and immunoblotted with antiphosphotyrosine antibody (4G10). Immunoreactive bands were visualized by enhanced chemiluminescence. Representative data from more than 3 similar experiments are shown. A more extended kinetic analysis of protein tyrosine phosphorylation in untreated and HCQ-treated cell populations gave similar results (data not shown).
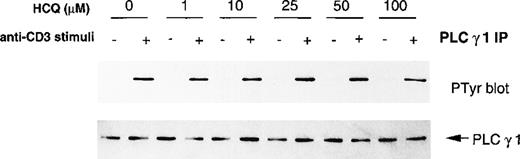
Tyrosine phosphorylation of PLCγ1 following TCR engagement enhances its intrinsic enzymatic activity, leading to increased production of IP3 and release of Ca++ from IP3-receptor–gated calcium stores.13 14 To determine whether HCQ altered PLCγ1 activation, Jurkat cells were pretreated with varying concentrations of HCQ for 24 hours, stimulated with C305 for 15 minutes, and then lysed. PLCγ1 immunoprecipitates from detergent lysates were subjected to Western blotting with either anti-PLCγ1 or antiphosphotyrosine antibodies. Equivalent amounts of PLCγ1 were immunoprecipitated from both untreated and HCQ-treated cells (Figure3, lower panel). Inductive tyrosine phosphorylation of PLCγ1 was also unaltered following pretreatment with HCQ (Figure 3, upper panel). To indirectly investigate PLCγ1 enzymatic activity, HCQ-treated Jurkat cells were stimulated with C305, and total inositol phosphate production was quantified. As shown in Figure 4, C305 stimulation resulted in an equivalent increase in total inositol phosphates in both untreated Jurkat cells and Jurkat cells pretreated with varying concentrations of HCQ (stimulation index = ∼4-5). In addition, HCQ did not alter C305-induced specific IP3 production as measured by radioreceptor assay (data not shown). Together, these findings suggest that proximal TCR signaling events, including PLCγ1 activation and inositol phosphate production, are intact in T cells treated with HCQ.
HCQ does not alter TCR-induced PLCγ1 tyrosine phosphorylation.
Jurkat T cells were treated with varying concentrations of HCQ for 24 hours, stimulated with C305 for 15 minutes, and then lysed in NP-40 detergent. PLCγ1 was immunoprecipitated from 5 × 107 cell equivalents, and immunoprecipitates were blotted with either antiphosphotyrosine (upper panel) or anti-PLCγ1 (lower panel), and immunoreactive bands were visualized by enhanced chemiluminescence. Representative data from more than 3 similar experiments are shown.
HCQ does not alter TCR-induced PLCγ1 tyrosine phosphorylation.
Jurkat T cells were treated with varying concentrations of HCQ for 24 hours, stimulated with C305 for 15 minutes, and then lysed in NP-40 detergent. PLCγ1 was immunoprecipitated from 5 × 107 cell equivalents, and immunoprecipitates were blotted with either antiphosphotyrosine (upper panel) or anti-PLCγ1 (lower panel), and immunoreactive bands were visualized by enhanced chemiluminescence. Representative data from more than 3 similar experiments are shown.
HCQ does not inhibit TCR-induced inositol phosphate production.
Jurkat T cells were treated with varying concentrations of HCQ for 24 hours and then loaded with [3H] myoinositol for 3 hours. Cells were left untreated (none) or were stimulated with C305 for 15 minutes, and were then lysed in chloroform. Soluble inositol phosphates were extracted by anion exchange and quantitated by liquid scintillation counting. Mean data from 3 separate experiments are expressed as stimulation indices: (cpm stimulated/cpm unstimulated) ± SD.
HCQ does not inhibit TCR-induced inositol phosphate production.
Jurkat T cells were treated with varying concentrations of HCQ for 24 hours and then loaded with [3H] myoinositol for 3 hours. Cells were left untreated (none) or were stimulated with C305 for 15 minutes, and were then lysed in chloroform. Soluble inositol phosphates were extracted by anion exchange and quantitated by liquid scintillation counting. Mean data from 3 separate experiments are expressed as stimulation indices: (cpm stimulated/cpm unstimulated) ± SD.
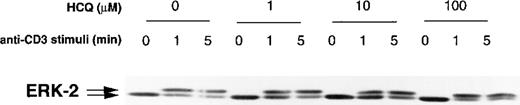
HCQ does not inhibit anti-TCR–induced ras signaling
The ras-dependent signaling pathway in T cells leads to a calcium-independent activation of the MAP kinase cascade.15-17 The integrity of this pathway can be monitored experimentally by the appearance of p42 and p44 phosphorylated MAP kinase species (ERK1 and ERK2) with the use of anti-ERK Western blotting of TCR-stimulated cell lysates.18 19 To assess the effect of HCQ on this signaling pathway, Jurkat cells were pretreated with HCQ, stimulated with C305 for 0 to 5 minutes, and then assayed for the appearance of phosphorylated forms of ERK2. In both control cells and cells treated with varying concentrations of HCQ, TCR stimulation consistently resulted in the appearance of equivalent amounts of p44 ERK2 (Figure5). These results indicated that HCQ does not significantly limit the signals leading from TCR to MAP kinase activation.
HCQ does not alter MAP kinase activation.
Jurkat T cells were treated with varying concentrations of HCQ for 24 hours, stimulated with C305 for 0 to 5 minutes, and then lysed in NP-40 detergent. Proteins from whole-cell lysates were subjected to 12% SDS-PAGE and were transferred to nitrocellulose, and membranes were immunoblotted with anti-ERK-2. Immunoreactive bands were visualized by enhanced chemiluminescence. Representative data from more than 3 similar experiments are shown.
HCQ does not alter MAP kinase activation.
Jurkat T cells were treated with varying concentrations of HCQ for 24 hours, stimulated with C305 for 0 to 5 minutes, and then lysed in NP-40 detergent. Proteins from whole-cell lysates were subjected to 12% SDS-PAGE and were transferred to nitrocellulose, and membranes were immunoblotted with anti-ERK-2. Immunoreactive bands were visualized by enhanced chemiluminescence. Representative data from more than 3 similar experiments are shown.
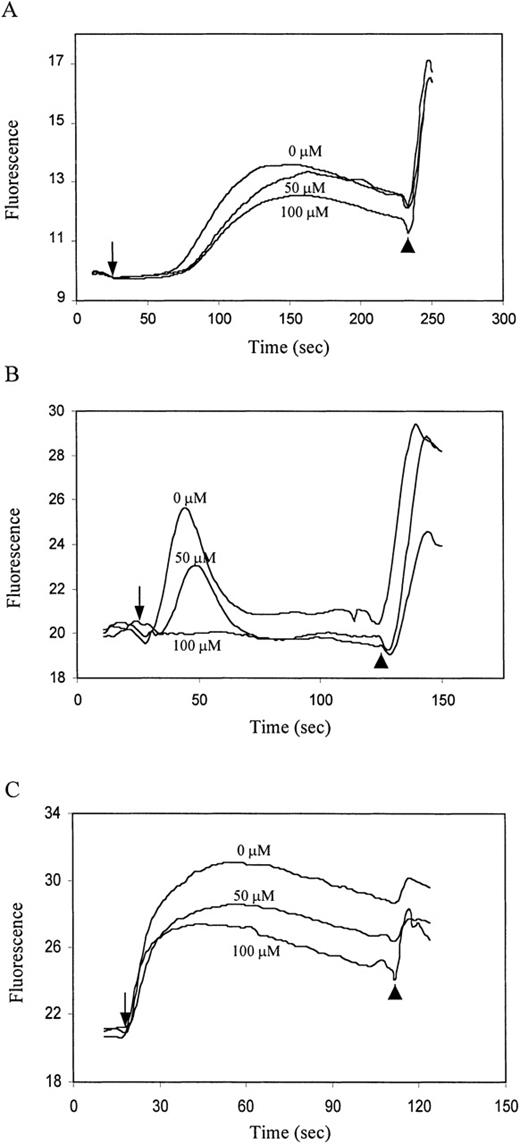
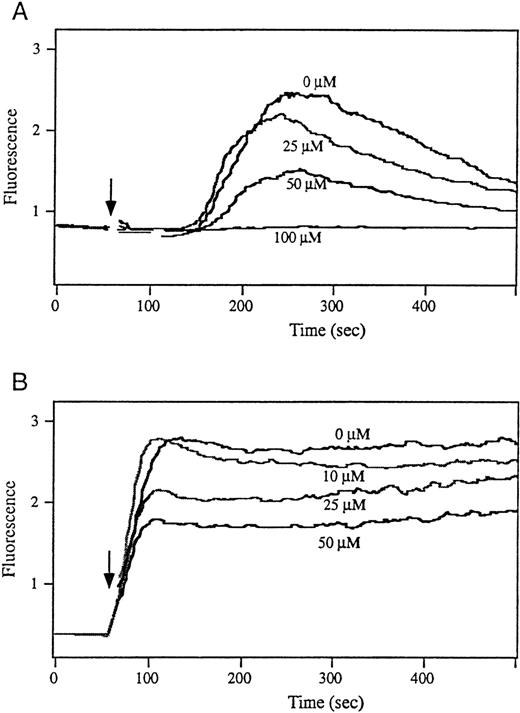
HCQ inhibits TCR-mediated intracellular calcium flux
TCR crosslinking results in a biphasic calcium flux. This consists of an initial phase increase in intracellular calcium released from IP3-receptor–gated stores followed by a secondary, sustained phase of extracellular Ca++ influx. This latter phase is controlled primarily through depletion of intracellular calcium stores.13,14 20-22 To determine if HCQ affects TCR-dependent calcium signaling, Jurkat cells were treated with varying concentrations of HCQ for 24 hours and assayed for their ability to flux calcium. Strikingly, as shown in Figure6A, total TCR-mediated intracellular calcium mobilization was inhibited by HCQ in a dose-dependent fashion. Blunted calcium signaling was consistently observed at concentrations of 25 μmol/L HCQ and higher. To determine if HCQ-dependent alterations in calcium responses also occurred in nontransformed T-cell populations, we evaluated the effect of HCQ treatment on freshly isolated human T cells from healthy donors. PBMCs were left untreated or were treated for 18 hours with varying concentrations of HCQ, loaded with the calcium-sensitive dyes calcium green-1 and fura-red, and monitored for intracellular Ca++flux by means of flow cytometry (Figure7A). Consistent with the effect in Jurkat T cells, HCQ treatment resulted in a dose-dependent reduction in the calcium response following CD3 crosslinking with nearly complete loss of the response to receptor engagement at doses of 100 μmol/L HCQ. Finally, to determine if inhibition of receptor-mediated calcium mobilization is a general property of HCQ, we also evaluated the effect of HCQ on a B-cell line (Ramos). HCQ treatment resulted in a significant reduction in the calcium signal initiated by engagement of the B-cell antigen receptor (BCR). At doses of 100 μmol/L HCQ, complete inhibition of the intracellular response was observed (Figure 6B).
HCQ inhibits antigen-receptor–dependent intracellular calcium mobilization and alters the size of intracellular calcium stores.
Jurkat T cells or Ramos B cells were pretreated with varying concentrations of HCQ for 24 hours and then loaded with the calcium-sensitive dye calcium green-1. Changes in intracellular Ca++ concentration (fluorescence) versus time (seconds) were monitored by bulk spectrofluorometry. (A) Jurkat T cells were activated with the clonotypic anti-TCR mAb C305 (as indicated by the arrow) followed by addition of 1 μmol/L ionomycin (arrowhead). (B) Ramos B cells were activated by IgM crosslinking (arrow) followed by the addition of 1 μmol/L ionomycin (arrowhead). (C) Jurkat cells were stimulated with 1 μmol/L thapsigargin, as indicated by arrow, in the presence of 1.8 mmol/L EGTA. Residual calcium response was evaluated by addition of 1 μmol/L ionomycin (arrowhead). Results are representative of more than 5 separate experiments.
HCQ inhibits antigen-receptor–dependent intracellular calcium mobilization and alters the size of intracellular calcium stores.
Jurkat T cells or Ramos B cells were pretreated with varying concentrations of HCQ for 24 hours and then loaded with the calcium-sensitive dye calcium green-1. Changes in intracellular Ca++ concentration (fluorescence) versus time (seconds) were monitored by bulk spectrofluorometry. (A) Jurkat T cells were activated with the clonotypic anti-TCR mAb C305 (as indicated by the arrow) followed by addition of 1 μmol/L ionomycin (arrowhead). (B) Ramos B cells were activated by IgM crosslinking (arrow) followed by the addition of 1 μmol/L ionomycin (arrowhead). (C) Jurkat cells were stimulated with 1 μmol/L thapsigargin, as indicated by arrow, in the presence of 1.8 mmol/L EGTA. Residual calcium response was evaluated by addition of 1 μmol/L ionomycin (arrowhead). Results are representative of more than 5 separate experiments.
HCQ inhibits intracellular calcium mobilization in primary T cells.
Peripheral blood T cells from healthy volunteers were pretreated with varying concentrations of HCQ for 18 hours and were then loaded with calcium-sensitive dyes calcium green-1 and fura-red. Cells were stimulated, as indicated by arrow, with (A) biotinylated OKT3 (40 μg/mL) plus avidin (10 μg/mL) or (B) 1 μmol/L ionomycin. Changes in intracellular Ca++ concentration (fluorescence) versus time (seconds) were monitored by fluorescence-activated cell sorter, and results are representative of 3 separate experiments.
HCQ inhibits intracellular calcium mobilization in primary T cells.
Peripheral blood T cells from healthy volunteers were pretreated with varying concentrations of HCQ for 18 hours and were then loaded with calcium-sensitive dyes calcium green-1 and fura-red. Cells were stimulated, as indicated by arrow, with (A) biotinylated OKT3 (40 μg/mL) plus avidin (10 μg/mL) or (B) 1 μmol/L ionomycin. Changes in intracellular Ca++ concentration (fluorescence) versus time (seconds) were monitored by fluorescence-activated cell sorter, and results are representative of 3 separate experiments.
The inhibition of intracellular calcium mobilization in HCQ-treated cells correlated with a reduced response following addition of the calcium ionophore, ionomycin (arrowhead in Figure 6A-C, arrow in Figure7B). Ionomycin-dependent calcium release was reduced after both TCR and BCR activation, and the reduction of this response correlated with the HCQ dose. These findings suggested that the intracellular calcium store size was altered in HCQ-treated cells. Eukaryotic cells sequester Ca++ within intracellular calcium stores, including dynamic Ca++ stores capable of both rapid Ca++ release in response to IP3-receptor engagement and rapid Ca++re-uptake via sarcoplasmic or endoplasmic reticulum Ca++-ATPases (SERCA) pumps.14,23,24 The sesquiterpene lactone, thapsigargin, selectively inhibits Ca++ re-uptake via SERCAs.25,26 In the absence of extracellular calcium, thapsigargin can be used to block the refilling of these intracellular calcium stores and measure their relative size without initiation of store-operated calcium influx.27 28 We therefore evaluated the potential effects of HCQ on the relative size of this dynamic calcium store in Jurkat T cells. Strikingly, thapsigargin-sensitive intracellular calcium stores were significantly reduced in cells pretreated with HCQ. This effect was HCQ-dose–dependent and was observed both before and after TCR crosslinking (Figure 6C, and data not shown). Together, these data demonstrate that HCQ treatment significantly reduces TCR-dependent calcium signaling and that this effect is controlled, at least in part, by alteration in the size of the IP3-gated intracellular calcium store.
Discussion
Quinolines are a group of drugs with newly recognized immunosuppressive properties. Recent studies have suggested that HCQ may be useful in the treatment of chronic GvHD in humans.2In addition, the closely related drug chloroquine can prevent acute GvHD in murine models.29 As diprotic bases, these agents pass through the lipid cell membrane and preferentially concentrate in acidic cytoplasmic vesicles. The resulting pH change within these vesicles in macrophages disrupts antigen processing, a mechanism of action previously proposed to explain the immunomodulatory properties of these drugs.30 More recently, both HCQ4,31and chloroquine32 have been shown to have T-cell–specific effects. These agents inhibit tetanus-toxoid– and mitogen-induced proliferative responses in vitro and have been used in combination with CsA to synergistically inhibit T-cell responses in vitro.31 32
To better understand how HCQ inhibits T-cell activation, we evaluated the effects of this agent at various points in the TCR signal transduction cascade. Consistent with previous studies suggestive of T-cell–specific inhibitory effects,4,31 HCQ inhibited TCR-induced up-regulation of CD69. Assessment of multiple proximal TCR-mediated signaling events, including TCR-induced PTK activation, inositol phosphate production, and MAP kinase activation, failed to demonstrate an inhibitory effect of HCQ. In contrast, TCR-induced intracellular calcium mobilization was significantly inhibited by HCQ in a dose-dependent fashion. Both TCR-crosslinking–dependent initial calcium release (peak response) and extracellular calcium influx (sustained response) were inhibited by HCQ. Most notably, HCQ pretreatment was associated with a dose-dependent reduction in thapsigargin-sensitive intracellular calcium stores. TCR-crosslinking–dependent depletion of these stores activates the calcium-release–activated calcium (ICRAC) channel in T cells, leading to a sustained influx of extracellular calcium.21 Together, our data suggest that HCQ limits both the initial peak calcium response and store-operated calcium influx via ICRAC channels by altering thapsigargin-sensitive, endoplasmic reticulum calcium store size.
The reduction in the TCR-dependent CD69 up-regulation in HCQ-treated cells is consistent with previous studies suggesting a role for a sustained calcium signal (in addition to ras/MAP kinase activation) in this transcriptional response.12 Consistent with this model, activation of Jurkat T cells with both PMA and ionomycin leads to a significant increase in CD69 induction relative to PMA alone (data not shown). The consequences of altered calcium signaling in B and T lymphoid cells have been extensively characterized. Both peak threshold and sustained increases in [Ca++]i are critical for the induction of the transcription factors NF-AT and NF-κB and for T-cell proliferation and differentiation in response to TCR crosslinking.33-36 In B cells, subthreshold oscillations in [Ca++]i result in activation of only a subset of downstream transcription signals and can lead to anergy and/or cell death via apoptosis.37 38 Because calcium-dependent signaling events in T and B cells are highly conserved, subthreshold calcium signals are likely to similarly down-regulate T-cell transcriptional events. Interestingly, BCR-induced intracellular calcium mobilization is also inhibited by HCQ in a dose-dependent fashion. This inhibition also correlates with a reduction in the size of thapsigargin-sensitive calcium stores (R.M.K. and D.J.R., unpublished observations). While the consequences of these changes on B-cell activation and differentiation are currently being evaluated, these findings suggest HCQ treatment may alter TCR-, BCR-, and T- and B-dependent functional immune responses at several levels.
The mechanism by which HCQ exerts its effects on calcium store size remains unclear. Our data are consistent with either a reduced store capacity, reduced store refilling, or a combination of both effects. Previous studies of the effect of chloroquine on G-protein–coupled receptor-dependent calcium signaling suggested reduced size of thapsigargin-sensitive calcium stores in fibroblast lines and macrophages.39 Furthermore, chloroquine was also shown to alter the capacity of IP3-gated receptors to bind IP3 in these cells. These data are difficult to interpret, however, because they used the calcium indicator dye Fura-2. This indicator leads to an underestimate of intracellular calcium concentration because of interference with the calcium-bound excitation spectra (see “Material and methods”). If we assume that similar results would be obtained with an alternative (eg, calcium green-1, or calcium green-1 and fura-red) measurement, these earlier studies are consistent with our results demonstrating reduced intracellular calcium mobilization in HCQ-treated cells. In both situations, this alteration in calcium signaling occurred despite equivalent levels of PLCγ1 activation and IP3 production in drug-treated and untreated cells. Finally, it has also been reported that chloroquine can reduce calcium currents in other cell types, including Paramecium40 and frog atrial trabeculae.41 Given the similar structures of these pharmacologic agents, it is not surprising that HCQ could exert similar effects on calcium currents in human T cells.
Patients receiving HCQ in a trial for treatment of chronic GvHD have been targeted to have a whole-blood level of 5 to 15 μmol/L. While this “therapeutic” concentration of HCQ did not consistently inhibit TCR-induced calcium responses in vitro, we were able to observe a modest but consistent decrease in TCR-induced CD69 up-regulation at these concentrations. Our observations that HCQ inhibits TCR-mediated signals in vitro may partially explain its ability to control chronic GvHD. Because the mechanism of action of HCQ differs from that of other immunosuppressants, including CsA and glucocorticoids, it may be well suited to complement these agents in combination drug therapy for chronic GvHD. Additional studies are required to fully characterize the effect of HCQ on calcium signaling in T cells and to assess the TCR-signaling pathway in T cells from patients with chronic GvHD receiving HCQ.
Acknowledgments
We wish to thank Drs Gary Koretzky and Gail Bishop for their critical review and useful suggestions, Justin Fishbaugh for flow cytometry assistance, and Marsha Jensen for preparation of this article.
Supported by National Institutes of Health (NIH) grant 5P30HD27748; by the Carver Medical Trust Funds and grant IN-122Q from the American Cancer Society, administered through the University of Iowa Cancer Center (F.D.G.); and in part by NIH grants HD37091 and AR01912, the American Cancer Society, and the facilities of the UCLA Jonsson Comprehensive Cancer Center (D.J.R.). D.J.R is recipient of a McDonnell Scholar Award; a Leukemia Society of America Scholar Award; UCLA Child Health, HHMI, and Pennington Research Awards; and the Joan J. Drake Grant for Excellence in Cancer Research.
Reprints:Frederick D. Goldman, Department of Pediatrics, Division of Hematology/Oncology, University of Iowa Hospitals and Clinics, Iowa City, IA 52242; e-mail:frederick-goldman@uiowa.edu.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.

![Fig. 4. HCQ does not inhibit TCR-induced inositol phosphate production. / Jurkat T cells were treated with varying concentrations of HCQ for 24 hours and then loaded with [3H] myoinositol for 3 hours. Cells were left untreated (none) or were stimulated with C305 for 15 minutes, and were then lysed in chloroform. Soluble inositol phosphates were extracted by anion exchange and quantitated by liquid scintillation counting. Mean data from 3 separate experiments are expressed as stimulation indices: (cpm stimulated/cpm unstimulated) ± SD.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/95/11/10.1182_blood.v95.11.3460/6/m_bloo01126004x.jpeg?Expires=1769165971&Signature=AY1zBEugQc~KljEgLGTvLX5ZjI6gkGrD4uIcC8ksZnefZ9kE4k45Dl~TCFK7b5vVK5oR1Lg246pfVdmU6nJd0C~L7H5eAl2u-s~5rNVQFz9WdQvvgr2a7b0-6crLtOoMjm4dvR-gl2jGy2MnB9hAsBJcurCjDZI0EEHEI5HEsVKPJNVzgO5rvsiNRBqGHQF3Gxs76JuhzPM~8LYDuTbviX85U0gYBRFCt5t~ZLFYYBQ0QUXZxIB-Nvbvd30LSfipWsHEGchQ2Usf3G~UT-gmQeTkxzc1Zj-HxjwGnkD20CVTglcQczGngZw9E3lb4im94bEcAj5G4-y4Y5oowTCd3g__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal