Abstract
Compounds that inhibit protein kinases are currently undergoing clinical evaluation for the treatment of a variety of malignancies. The kinase inhibitors flavopiridol and 7 hydroxy-staurosporine (UCN-01) were examined for their effects on B-cell chronic lymphocytic leukemia (B-CLL) cells in vitro (n = 49). Flavopiridol and UCN-01 induced concentration-dependent apoptosis of most B-CLL samples tested, with greater than 50% cell killing occurring at concentrations of less than 1 μmol/L, and with flavopiridol displaying more potent activity than UCN-01. Flavopiridol (0.1 μmol/L) and UCN-01 (1 μmol/L) also induced striking decreases in the levels of the antiapoptosis proteins Mcl-1, X-linked inhibitor of apoptosis (XIAP), and BAG-1 in nearly all cases of B-CLL and of Bcl-2 in approximately half of B-CLL specimens evaluated. In contrast, expression of the proapoptotic proteins Bax and Bak was not significantly influenced by these kinase inhibitors. Flavopiridol-induced decreases in the levels of antiapoptosis proteins Mcl-1 and XIAP preceded apoptosis and were not substantially affected by the addition of caspase inhibitors to cultures. In contrast, UCN-01–stimulated decreases in antiapoptosis proteins were slower, occurred concurrently with apoptosis, and were partially prevented by caspase inhibitors. The findings suggest that flavopiridol and UCN-01 induce apoptosis of B-CLL cells through different mechanisms. The potent apoptotic activities of flavopiridol and UCN-01 against cultured B-CLL cells suggest that they may be effective as single agents in the treatment of B-CLL or for sensitizing B-CLL cells to conventional cytotoxic drugs.
Chronic lymphocytic leukemia (CLL) is presently an incurable disease, representing the most common form of leukemia in North America and Europe.1 These malignant cells are most commonly comprised of CD5+ mature B-lymphocytes that gradually accumulate in the patient because of defective programmed cell death rather than accelerated cell division.2 The underlying defect in apoptosis in B-cell CLL (B-CLL) is undefined, but most cases express the antiapoptotic protein Bcl-2 at high levels.3 Higher levels of Bcl-2 or increased ratios of Bcl-2 relative to its proapoptotic antagonist Bax have been correlated with refractory disease, disease progression, and shorter survival.4-8 Higher levels of the antiapoptotic protein Mcl-1 have also been correlated with failure to achieve complete remission in patients treated with alkylating agents or purine nucleosides.9 The underlying defect in programmed cell death in B-CLL cells presumably accounts for the general chemoresistance of this disease. Although more than half of patients respond initially to single agent therapy, B-CLL cells almost uniformly progress to refractory disease given sufficient time.10 11Thus, a need exists for novel agents that can overcome blocks to apoptosis in B-CLL, particularly in treatment of refractory patients.
Flavopiridol and 7 hydroxy-staurosporine (UCN-01) are small molecule compounds that inhibit selected protein kinases by interacting with their adenosine triphosphate (ATP)–binding sites. Flavopiridol is a novel semisynthetic flavone derivative of the alkaloid rohitukine, originally identified as a cyclin-dependent kinase inhibitor.12 UCN-01 is a derivative of the nonselective protein kinase inhibitor staurosporine, which may have selective inhibitory activity against protein kinase (PK) C family members at low concentrations but which is probably capable of inhibiting a wide variety of protein kinases.13 Both of these agents are presently undergoing clinical evaluation for the treatment of a variety of cancers, including B-cell malignancies.11 These agents have been shown to induce apoptosis of B-CLL cells in vitro (reviewed in Byrd et al11), but the mechanisms responsible are unclear. Here, we demonstrate that flavopiridol and UCN-01 potently down-regulate the levels of several antiapoptosis proteins in B-CLLs at doses estimated to be within or near the range tolerated in vivo.
Patients, materials, and methods
Kinase inhibitors
Flavopiridol and UCN-01 were obtained from the Developmental Therapeutics Branch of the National Cancer Institute (E. Sausville) with permission from Hochest Marion Roussel, Inc, and Kyowa Hakko Kogyo Co, respectively. Flavopiridol was dissolved in dimethyl sulfoxide (DMSO) at 1 mmol/L and stored at room temperature. UCN-01 was dissolved in DMSO at 10 mmol/L and stored at −20°C.
Patient specimens
Heparinized peripheral blood was obtained from both untreated (n = 30) and previously treated (n = 19) patients diagnosed with CD5+ B-CLL according to standard criteria.14 Of the 49 specimens evaluated, 12, 17, 12, and 8 were derived from patients with Rai stage 0, 1, 2, and 3 disease, respectively. Lymphocytes were isolated by ficoll density–gradient centrifugation9 and verified by immunofluroescence flow cytometry to be composed of more than 95% CD5+CD19+ B-cells. Except for some Rai 0 stage patients, B-CLL cells represented more than 95% of the isolated lymphocytes, based on flow-cytometric analysis.
Cell culture and apoptosis assays
B-CLL cells were cultured at 2 × 106 per mL in Iscove's Modified Dulbecco's Medium containing 20% fetal calf serum, 1 mmol/L L-glutamine, and antibiotics as described.9 Various concentrations of flavopiridol or UNC-01 were added at the initiation of cultures, with or without 100 μmol/L benzoylcarbonyl-valine-alanine-asparte-fluoro-methyl-ketone (zVAD-fmk) (Calbiochem-Novabiochem, San Diego, CA), and cells were recovered by centrifugation at various times thereafter for evaluation of the percentage of apoptotic cells with the use of a fluorescence-based DNA end-labeling (TUNEL) method with flow-cytometry analysis or were lysed in RIPA buffer (10 mmol/L Tris pH 7.4, 150 mmol/L NaCl, 1% Triton X-100, 1% deoxycholate, 0.1% sodium dodecyl sulfate [SDS], 5 mmol/L EDTA plus protease inhibitors, including phenyl-methyl sulfonyl fluoride, aprotinin, leupeptin benzamidine, and pepstatin) for immunoblot analysis as described in detail previously.9 Correlations with Rai stage and prior therapy were made by analysis of variance methods.
Immunoblot analysis of apoptosis-regulatory proteins
Cell lysates were normalized for total protein content (25 μg) and subjected to SDS–polyacrylamide gel electrophoresis (SDS-PAGE) (12% gels) immunoblot assay.9,15 Primary antibodies included polyclonal rabbit antisera specific for Bcl-2, Mcl-1, Bax, and Bak16-18 and murine monoclonal antibodies specific for BAG-1,19 β-actin (Sigma Immunochemicals), poly(adenosine 5′-diphosphate–ribose) polymerase PARP20 (gift of N. A. Berger), and X-linked inhibitor of apoptosis (XIAP) (Transduction Laboratories, San Diego, CA). Immunodetection was accomplished with the use of horseradish-peroxidase–conjugated secondary antibodies and an enhanced chemiluminescence (ECL) method (Amersham) involving exposure to x-ray film (Kodak XAR, Rochester, NY). Multiple reprobings of blots were achieved by the MAD method.15 Data were quantified from x-ray films by scanning densitometry by means of the National Institutes of Health image 1.57 program and compared for untreated and drug-treated specimens by paired t test. Correlations with Rai stage and prior therapy were made by the Fisher exact test.
Results
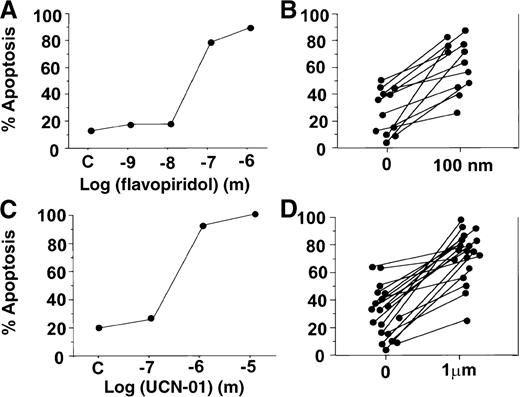
Treatment of B-CLL cells with flavopiridol or UCN-01 in vitro resulted in increased apoptosis in most specimens evaluated. Dose-response analysis performed for CLL specimens with flavopiridol and UCN-01 revealed increases in the percentage of TUNEL-positive B-CLLs beginning at concentrations of more than 0.01 μmol/L for flavopiridol and more than 0.1 μmol/L for UCN-01 (Figure1). The cytotoxic actions of flavopiridol and UCN-01 generally reached plateau or near plateau levels at 0.1 μmol/L and 1.0 μmol/L, respectively (Figure 1). Among the 49 B-CLL specimens employed throughout the studies reported here, quantification of flavopiridol and UCN-01 effects on apoptosis was performed by TUNEL assay for 12 and 19 specimens, respectively (Figure 1B,D). Although the percentage of leukemic cells undergoing spontaneous apoptosis during cell culture varied among B-CLL specimens tested, 0.1 μmol/L flavopiridol and 1 μmol/L UCN-01 induced at least 10% further increases in the percentage of TUNEL-positive B-CLLs in 10 of 12 (83%) and in 17 of 19 (89%) B-CLL patient specimens tested, respectively (Figure 1B,D).
Flavopiridol and UCN-01 induce apoptosis of B-CLL cells in vitro.
B-CLL cells were cultured in the presence or absence of flavopiridol (panels A and B) or UCN-01 (panels C and D) at the concentrations indicated. After 3 days, the percentage of apoptotic cells was determined by fluorescence-activated cell sorter–based TUNEL assay. Panels A and C show representative examples of dose-response data. Panels B and D show compilation of data for B-CLL specimens tested, contrasting the percentage of apoptosis that occurred in vitro during 2 days' culture in the absence or presence of kinase inhibitors (flavopiridol, P < .005; UCN-01, P < .0005).
Flavopiridol and UCN-01 induce apoptosis of B-CLL cells in vitro.
B-CLL cells were cultured in the presence or absence of flavopiridol (panels A and B) or UCN-01 (panels C and D) at the concentrations indicated. After 3 days, the percentage of apoptotic cells was determined by fluorescence-activated cell sorter–based TUNEL assay. Panels A and C show representative examples of dose-response data. Panels B and D show compilation of data for B-CLL specimens tested, contrasting the percentage of apoptosis that occurred in vitro during 2 days' culture in the absence or presence of kinase inhibitors (flavopiridol, P < .005; UCN-01, P < .0005).
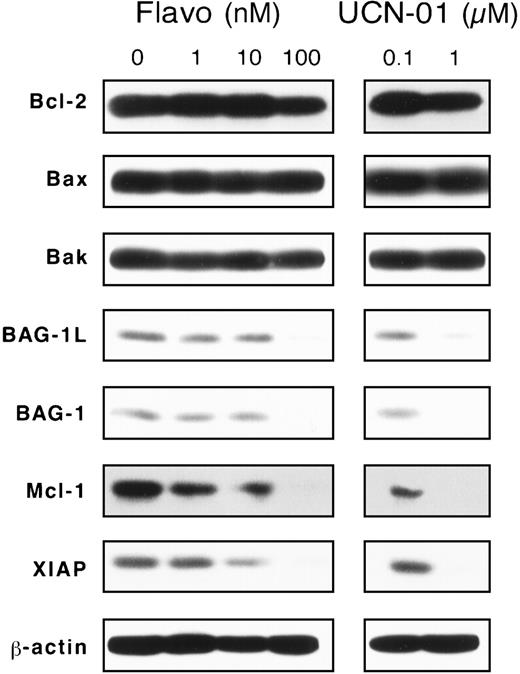
Analysis of several apoptosis-regulatory proteins in B-CLLs by immunoblotting revealed striking changes induced by flavopiridol and UCN-01. As demonstrated by the representative immunoblots presented in Figure 2, flavopiridol and UCN-01 induced concentration-dependent reductions in the levels of the antiapoptosis proteins Mcl-1, BAG-1, and XIAP without significantly affecting the levels of β-actin (control) or the proapoptotic proteins Bax and Bak. The concentrations of kinase inhibitors required for down-regulation of antiapoptotic proteins coincided roughly with the doses needed to increase apoptosis (compare Figures 1 and 2). Less consistent reductions in the steady-state levels of Bcl-2 were also observed in some B-CLLs (see below).
Flavopiridol and UCN-01 down-regulate antiapoptotic proteins.
Representative immunoblot data show down-regulation of antiapoptosis proteins by kinase inhibitors. B-CLL cells were cultured with or without 0.1 μmol/L flavopiridol or 1 μmol/L UCN-01 for 2 days. Whole cell lysates were then prepared, normalized for protein content (25 μg), and subjected to SDS-PAGE/immunoblot analysis with the use of antibodies specific for Bcl-2, Mcl-1, Bax, Bak, BAG-1, XIAP, and β-actin with ECL-based detection. Data illustrate a representative B-CLL sample and are derived from a single blot by means of the MAD immunoblotting method. Note that B-CLLs express both long (BAG-1L) and short (BAG-1) isoforms of BAG-119 and that both were down-regulated by kinase inhibitors.
Flavopiridol and UCN-01 down-regulate antiapoptotic proteins.
Representative immunoblot data show down-regulation of antiapoptosis proteins by kinase inhibitors. B-CLL cells were cultured with or without 0.1 μmol/L flavopiridol or 1 μmol/L UCN-01 for 2 days. Whole cell lysates were then prepared, normalized for protein content (25 μg), and subjected to SDS-PAGE/immunoblot analysis with the use of antibodies specific for Bcl-2, Mcl-1, Bax, Bak, BAG-1, XIAP, and β-actin with ECL-based detection. Data illustrate a representative B-CLL sample and are derived from a single blot by means of the MAD immunoblotting method. Note that B-CLLs express both long (BAG-1L) and short (BAG-1) isoforms of BAG-119 and that both were down-regulated by kinase inhibitors.
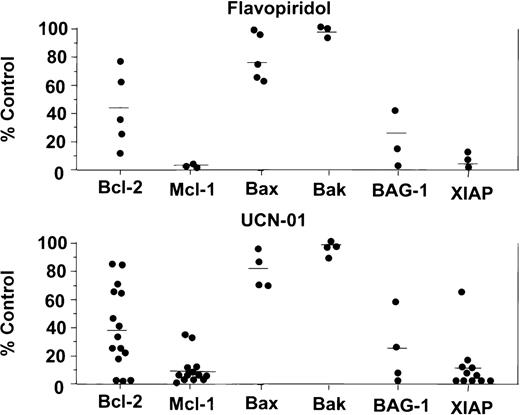
When B-CLLs were treated for 48 hours with 0.1 μmol/L flavopiridol, reductions of greater than 80% in the steady-state levels of Mcl-1 (n = 3; P < .0001), BAG-1 (n = 3;P < .05), and XIAP (n = 5; P < .005) were observed in all specimens tested (Figure 3, top), whereas reductions of 50% or more in Bcl-2 protein levels were observed in 3 (60%) of the 5 B-CLLs evaluated (P = .01). In contrast, no significant changes were observed in the levels of proapoptotic proteins Bax (n = 5) and Bak (n = 3) (Figure 3, top). Indeed, along with β-actin, these proapoptotic proteins served as additional controls, verifying that equivalent amounts of total protein were loaded for each sample.
Comparison of effects of kinase inhibitors on apoptosis-regulatory proteins in B-CLL.
B-CLLs were cultured for 2 days with or without (control) 0.1 μmol/L flavopiridol or 1 μmol/L UCN-01. Immunoblot data were quantified by scanning densitometry to obtain rough estimates of the relative amounts of proteins. Data are expressed as a percentage relative to untreated (control) B-CLLs after normalization for β-actin. Bars indicate mean.
Comparison of effects of kinase inhibitors on apoptosis-regulatory proteins in B-CLL.
B-CLLs were cultured for 2 days with or without (control) 0.1 μmol/L flavopiridol or 1 μmol/L UCN-01. Immunoblot data were quantified by scanning densitometry to obtain rough estimates of the relative amounts of proteins. Data are expressed as a percentage relative to untreated (control) B-CLLs after normalization for β-actin. Bars indicate mean.
Similarly, culturing B-CLLs with 1 μmol/L UCN-01 for 48 hours resulted in decreases of 90% or more in the steady-state levels of Mcl-1 in 11 of 13 (85%) specimens tested (P < .0001) and in the levels of XIAP (P < .0001) and BAG-1 (P < .05) in all (n = 4) B-CLLs evaluated (Figure 3, bottom). Bcl-2 protein levels were reduced by more than 50% in 10 of 15 (67%) of B-CLLs cultured with UCN-01 (P < .0001), whereas Bax (n = 5) and Bak (n = 3) protein levels were unchanged (Figure 3, bottom). No significant correlations were observed between Rai stage or prior therapy and the effects of kinase inhibitors on apoptosis or gene expression.
Time-course studies demonstrated that decreases in antiapoptosis protein levels preceded apoptosis induced by flavopiridol. Figure4 presents representative data for XIAP and Mcl-1. Note that greater than 50% decreases in XIAP and Mcl-1 protein levels were achieved in flavopiridol-treated B-CLL cells at times (3 to 6 hours) when little induction of apoptosis had occurred, as determined by DNA fragmentation (TUNEL assay) (Figure 4A,B). In contrast to flavopiridol, decreases in antiapoptosis protein levels in UCN-01–treated B-CLL cells were slower, occurring almost concomitantly with apoptosis. (Figure 4C, D).
Time-course of flavopiridol- and UCN-01–induced decreases in XIAP and Mcl-1 protein levels.
B-CLL cells were cultured with (shaded symbols) or without (open symbols) 0.1 μmol/L flavopiridol (panels A and B) or 1 μmol/L UCN-01 (panels C and D). At various times, cells were recovered from cultures, and either lysates were prepared for immunoblot analysis (circles) with the use of antibodies specific for XIAP (panels A and C) or Mcl-1 (panels B and D) and the data were expressed as a percentage of untreated cells, or apoptosis was determined by TUNEL assay (squares). Data are representative of results obtained from 3 consecutive B-CLL specimens.
Time-course of flavopiridol- and UCN-01–induced decreases in XIAP and Mcl-1 protein levels.
B-CLL cells were cultured with (shaded symbols) or without (open symbols) 0.1 μmol/L flavopiridol (panels A and B) or 1 μmol/L UCN-01 (panels C and D). At various times, cells were recovered from cultures, and either lysates were prepared for immunoblot analysis (circles) with the use of antibodies specific for XIAP (panels A and C) or Mcl-1 (panels B and D) and the data were expressed as a percentage of untreated cells, or apoptosis was determined by TUNEL assay (squares). Data are representative of results obtained from 3 consecutive B-CLL specimens.
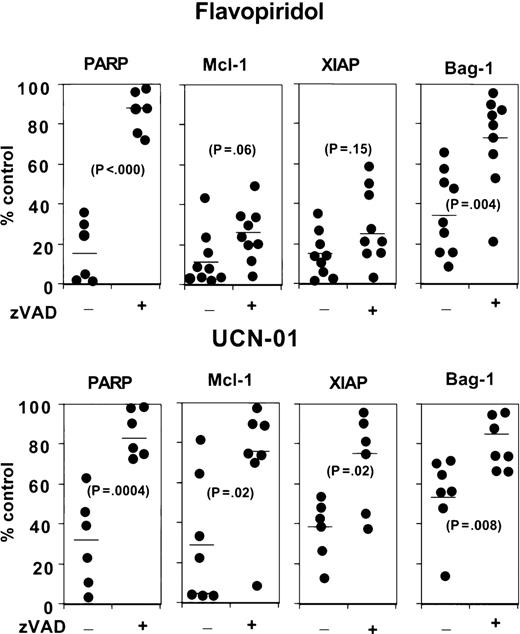
To explore whether the decreases in antiapoptosis proteins induced by flavopiridol and UCN-01 are dependent on caspase activation, B-CLL cells were cultured with the broad-spectrum irreversible caspase inhibitor zVAD-fmk. Comparisons were made by immunoblot analysis of the effects of flavopiridol and UCN-01 on levels of XIAP, Mcl-1, and BAG-1 in the presence and absence of zVAD-fmk (Figure5). As a control, levels of a prominent caspase substrate, PARP, were also examined to monitor the disappearance of the approximately 110-kd PARP protein, which undergoes cleavage by caspases to generate an approximately 85-kd proteolytic fragment.21 As summarized in Figure 5, flavopiridol- and UCN-01–induced cleavage of PARP was significantly inhibited by zVAD-fmk. In contrast, flavopiridol-induced decreases in the steady-state levels of XIAP and Mcl-1 were not significantly affected by zVAD-fmk. However, the decline in BAG-1 levels induced by flavopiridol was partially prevented by zVAD-fmk, implying that reductions in the levels of this protein represent a postcaspase activation event. Unlike flavopiridol, decreases in the steady-state levels of XIAP, Mcl-1, and BAG-1 triggered by UCN-01 were largely inhibited by zVAD-fmk, suggesting a caspase-dependent process. Levels of Bax, Bak, and β-actin were unaffected by zVAD-fmk, flavopiridol, UCN-01, or combinations of these reagents during these experiments (not shown).
Effects of caspase inhibitor zVAD-fmk on changes in apoptosis protein levels induced by flavopiridol and UCN-01 in B-CLL cells.
B-CLL cells derived from 6 to 9 patients were cultured with (+) or without (−) 100 μmol/L zVAD-fmk and either 0.1 μmol/L flavopiridol (top) or 1 μmol/L UCN-01 (bottom). After 18 to 24 hours, cell lysates were prepared, normalized for total protein content, and analyzed by immunoblotting with the use of antibodies specific for PARP, Mcl-1, XIAP, or Bag-1. Data were quantified by scanning densitometry and expressed as a percentage relative to control: untreated B-CLL cells. PARP data refer to loss of the full-length 110 kd protein, which undergoes caspase-mediated cleavage. Data were compared by means of a paired t test (Pvalues shown). Bars indicate mean of data points.
Effects of caspase inhibitor zVAD-fmk on changes in apoptosis protein levels induced by flavopiridol and UCN-01 in B-CLL cells.
B-CLL cells derived from 6 to 9 patients were cultured with (+) or without (−) 100 μmol/L zVAD-fmk and either 0.1 μmol/L flavopiridol (top) or 1 μmol/L UCN-01 (bottom). After 18 to 24 hours, cell lysates were prepared, normalized for total protein content, and analyzed by immunoblotting with the use of antibodies specific for PARP, Mcl-1, XIAP, or Bag-1. Data were quantified by scanning densitometry and expressed as a percentage relative to control: untreated B-CLL cells. PARP data refer to loss of the full-length 110 kd protein, which undergoes caspase-mediated cleavage. Data were compared by means of a paired t test (Pvalues shown). Bars indicate mean of data points.
Discussion
Flavopiridol and UCN-01 potently and reproducibly down-regulated the levels of several antiapoptotic proteins in B-CLL cells in vitro, without modulating expression of the proapoptotic proteins Bax and Bak. The apoptosis-regulatory proteins examined here contain representatives from several classes of proteins. Bcl-2, Mcl-1, Bax, and Bak are all members of the Bcl-2 family of apoptosis-regulating proteins (reviewed in Reed22 and Kroemer23). The relative ratios of antiapoptotic (Bcl-2 and Mcl-1) and proapoptotic (Bax and Bak) Bcl-2 family proteins determine the sensitivity or resistance of cells to a broad variety of cell death stimuli, including most anticancer drugs.24 Gene transfer–mediated overexpression of either Bcl-2 or Mcl-1 has been reported to increase resistance to apoptosis induction by chemotherapeutic drugs (reviewed in Reed24,25). Bcl-2 family proteins may have multiple biochemical functions, including modulation of mitochondrial responses to cellular damage induced by anticancer drugs (reviewed in Reed26).
BAG-1, in contrast, is a regulator of the Hsp70 family of molecular chaperones that confers resistance to a variety of stimuli that induce apoptosis or that produce cellular stress.27 Recently, it has been suggested that Hsp70 controls a distal apoptosis checkpoint downstream of Bcl-2.28 Moreover, the nuclear-targeted longer isoforms of BAG-1 reportedly bind steroid hormone receptor complexes; BAG-1 family protein interactions with glucocorticoid receptors and retinoic acid receptors confer resistance to apoptosis induction by these steroids.29 30
Finally, XIAP is a member of the inhibitor-of-apoptosis (IAP) family of apoptosis suppressors that directly binds to and inhibits selected members of the caspase family of cell death proteases.31 Elevated expression of XIAP and other IAP-family proteins has been reported to confer increased resistance to apoptosis induced by multiple stimuli, including chemotherapeutic drugs (reviewed in Deveraux et al32). However, because these proteins directly inhibit caspases, they may be particularly important for avoidance of apoptosis mechanisms employed by immune cells, including caspase-activating members of the tumor necrosis–factor family of cytokine receptors and caspase-activating granzymes used by cytolytic T-cells for inducing apoptosis in target cells.
The protein kinase targets of flavopiridol and UCN-01 that are relevant to apoptosis induction in B-CLLs remain to be identified. Given the nonproliferative nature of B-CLL, it seems unlikely (though not impossible) that cyclin-dependent kinases are the major targets in this disease. Candidates, however, include PKC family members, PKA, and Akt/PKB, which have all been associated with apoptosis suppression in various cellular contexts. Whatever the kinase target(s), flavopiridol appears to be approximately 1 log more potent than UCN-01 at down-regulating the levels of apoptosis proteins in B-CLLs, at least in vitro. Moreover, flavopiridol-induced decreases in XIAP and Mcl-1 were caspase-independent, unlike UCN-01 where reductions in the levels of these proteins represented a postcaspase activation event. Thus, these kinase inhibitors induce apoptosis through different mechanisms in B-CLL cells.
It remains to be determined what the molecular basis is for the observed down-regulation of Bcl-2, Mcl-1, BAG-1, and XIAP protein levels in B-CLLs treated with flavopiridol or UCN-01. Conceivably, reduced production of these proteins owing to suppression of transcription or translation could be involved, as well as accelerated degradation of their messenger RNAs (mRNAs) or the proteins. Of these antiapoptosis proteins, Bcl-2 was the most variable in the influence of kinase inhibitors, which possibly could be due to its long half-life. Upon cessation of Bcl-2 mRNA production, it is not uncommon for Bcl-2 protein to remain in cells for a day or longer (reviewed in Reed33). In contrast, Mcl-1 is thought to be a short-lived protein because of PEST motifs present within this Bcl-2 family member.34 Likewise, BAG-1 contains a ubiquitin-like domain that could provide a mechanism for its rapid degradation.35 XIAP also appears to be a short-lived protein (unpublished data). Again, however, because down-regulation of Mcl-1 and XIAP protein levels by flavopiridol and UCN-01 was differentially affected by caspase inhibitors, it is clear that these kinase inhibitors use alternative mechanisms for reducing the levels of these particular apoptosis-suppressing proteins.
In summary, we have observed that flavopiridol directly, and UCN-01 indirectly, down-regulate the levels of several antiapoptotic proteins in B-CLLs in vitro. The reductions in antiapoptotic proteins induced by UCN-01, however, appear to occur as a result of caspase activation, presumably after commitment to apoptosis. In contrast, flavopiridol-induced decreases in XIAP and Mcl-1 precede apoptosis and occur independently of caspase activation. Consequently, flavopiridol-induced down-regulation of these survival proteins should render B-CLLs more vulnerable to apoptosis induced by a variety of stimuli, including cytotoxic anticancer drugs, glucocorticoids, and immune-mediated attack. Further preclinical and clinical evaluation of flavopiridol, UCN-01, and other kinase inhibitors in B-CLL is warranted.
Acknowledgments
The authors thank Ed Sausville (National Cancer Institute), Hochest Marion Roussel, and Kyowa Hakko Kogyo for kinase inhibitors; N. A. Berger for anti–PARP antibody; and S. Farrar, R. Cornell, T. Brown, E. Smith, and A. Majors for manuscript preparation.
Supported by National Institutes of Health grants CA-55164, CA67329, CA69381, AG15402, and CA81534. J.M.Z. is a Lymphoma Research Foundation Fellow.
Reprints:John C. Reed, The Burnham Institute, 10901 North Torrey Pines Rd, La Jolla, CA 92037; e-mail: jreed@burnham-inst.org.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal