Abstract
Recently, a marked extramedullary myelopoiesis in Fas/CD95- or FasL/CD95L-deficient mice has been reported. In the present in vitro study, the mechanisms underlying Fas-induced apoptosis of normal peripheral colony-forming unit-C (CFU-C) progenitors in the spleen were analyzed. Surprisingly, it was found that clonogenic progenitors were protected from γIFN plus Fas-induced programmed cell death when Lin+ cells were removed from cultured splenocytes. The cells that rendered CFU-C sensitive to the activation of the Fas pathway did not belong to the T or the myelocytic–monocytic lineage but comprised a non–B-cell subset expressing the activation marker B220. Among CD19− B220+ splenocytes, nearly half were natural killer (NK) 1.1+ cells whose in vivo depletion or deficiency in RAG2-γc−/− mice abrogated the effect of Fas cross-linking. NK cells exerted their accessory function, at least in part, through tumor necrosis factor–α (TNF-α), which they readily produced during pretreatment with the anti-Fas/CD95 monoclonal antibody and IFN-γ and whose addition could compensate for the loss of sensitivity. In conclusion, this study provides evidence that peripheral clonogenic progenitors are not directly responsive to Fas cross-linking, even in the presence of IFN-γ, but require NK cells as a source of TNF-α to make them susceptible to this death pathway.
Introduction
Fas/CD95/Apo-1 is a transmembrane protein of the TNF death receptor family expressed by a variety of tissues and several mature hematopoietic lineages, such as T and B lymphocytes,1,2 monocytes, and granulocytes at different stages of maturation.3-5 On interaction with its ligand (FasL/CD95L), Fas undergoes trimerization and recruits the adaptor molecule FADD (MORT1), which, in turn, activates procaspase 8, thus initiating a cascade of proteases ultimately leading to the disassembly of cell structure and death.6
The importance of the Fas death pathway in the regulation of the immune response has been widely acknowledged.7,8 More recently, it has become evident that apoptosis through Fas/FasL interactions occurs also in early hematopoietic progenitor cells, in which it might be instrumental in ensuring the homeostasis of blood cells. It has been reported that Fas is spontaneously expressed on primitive CD34+CD38− progenitors in human fetal liver and is induced in response to interferon γ (IFN-γ), tumor necrosis factor–α (TNF-α), or both on clonogenic bone marrow cells.9,10 Furthermore, its functionality has been demonstrated by the diminution of colony-forming cells in response to Fas cross-linking.11
Fas expression has also been demonstrated on murine progenitor-enriched Lin− c-kit+ bone marrow cells after cytomegalovirus infection12 and after stimulation with TNF-α in vitro.13 We have recently shown that Fas or FasL deficiency in mice of the lpr or thegld genotype results in increased fetal and extramedullary hematopoiesis.14 The number of hematopoietic progenitors in the bone marrow of these mutant strains was only slightly and transiently increased shortly after birth, suggesting either that these cells cannot accumulate in this organ and thus emigrate into the periphery or that they are less sensitive to apoptosis in the medullary environment.
The purpose of the present study was to analyze the molecular and cellular interactions that make colony-forming cells in the spleen susceptible to Fas-induced apoptosis, perhaps explaining why they are more sensitive to this death pathway than their medullary counterpart. Our results emphasize the importance of the environment and the cytokines generated for enabling hematopoietic progenitor cells to enter the Fas-dependent apoptosis pathway. They are of particular relevance during the immune response, when pro-inflammatory cytokines become readily available in the spleen.
Materials and methods
Animals
Six- to 12-week-old specific pathogen-free, male or female C57BL/6-+/+, C57BL/6-lpr/lpr, C57BL/6-β2m−/−, and C57BL/6-RAG2−/− mice were bred in our animal facility. C57BL/6-RAG2-γc−/−mice were established as previously described.15
Cytokines and antibodies
Murine recombinant (mr) IFN-γ (specific activity, 5 × 106 U/mg, as measured by an antiviral assay using L-929 cells infected with encephalomyocarditis virus), mrTNF-α and mr(s)TNFRI/Fc chimera were purchased from R&D Systems (Abingdon, United Kingdom). Hamster antimouse CD95 (Fas, Apo-1) (clone Jo2) (unlabeled or phycoerythrin (PE)-conjugated), rat antimouse CD19 (1D3, unlabeled and PE-conjugated), fluorescein isothiocyanate (FITC)-conjugated CD45R (B220) (RA3-6B2), mouse antimouse natural killer (NK) 1.1 (PK 136) (unlabeled or biotinylated), isotype controls, and PE-conjugated anti–TNF-α monoclonal antibody (mAb; clone MP6-XT22) for intracellular staining were purchased from Pharmingen (San Diego, CA). Thy-1.2 (53-2.1), CD11b (M1/70), GR-1 (8C5), CD45R (B220) (RA3-6B2), and TER-119 hybridoma supernatants were used for the depletion of splenic Lin+ cells. FITC-conjugated mouse antirat F(ab')2 mAb (The Jackson Laboratory, Bar Harbor, ME) and APC- or CyChrome-streptavidin (Pharmingen, San Diego, CA) were used to reveal Lin+ and NK.1.1+ cells, respectively.
In vivo treatment, cell preparations, and induction of apoptosis
Six-week-old C57BL/6-β2m−/−mice (chosen for their lack of NKT cells) received 2 intraperitoneal injections of 0.5 mg NK1.1 mAb per mouse one day before and 2 hours before death, compared with mice injected with isotype control. Spleens were removed, suspended in Hanks' balanced salt solution (Gibco, Grand Island, NY) by gentle teasing with forceps, and homogenized with a syringe. After centrifugation, cells were adjusted to a final concentration of 107/mL in minimum essential medium (MEM) supplemented with 1% sodium pyruvate 100×, 1% L-glutamine, 100 IU/mL penicillin, 100 μg/mL streptomycin, and 10% horse serum (all from Gibco), referred to as the culture medium. Mononuclear spleen cell suspensions from C57BL/6-+/+ mice were incubated for 20 minutes on ice with a cocktail of 5-fold diluted hybridoma supernatants (Thy1.2, CD11b, GR-1, CD45R, TER119) recognizing specific lineage markers. Splenocytes were then washed twice and incubated for another 20 minutes with sheep antirat IgG-coated magnetic beads (Dynabeads M-450; Dynal AS, Oslo, Norway), according to the manufacturer's instructions. Labeled cells were withdrawn against the inner wall of the test tube using a strong magnet, and unbound Lin− cells were collected. The same experimental setup was used to deplete spleen cells for one particular subset (B220+, Mac1+). Total NK1.1+ cells and their B220+ and B220− subsets were sorted from a spleen population magnetically depleted of CD19+ and Thy1.1+ cells using a FACSVantage sorter (Becton Dickinson, Mountain View, CA).
For Fas cross-linking, total spleen cells (107/mL), fractions depleted from a particular cell lineage (107cells/mL), and the progenitor-enriched Lin− population (106 cells/mL) were plated in Falcon 3047 multiwell plates (BD Biosciences, Le Pont de Claix, France) (2 mL/well) or Falcon 3072 microtiter plates (200 μL/well) and incubated for 24 hours in the presence of control hamster IgG (5 μg/mL), IFN-γ (100 U/mL), anti-CD95(Fas) mAb (5 μg/mL), or both IFN-γ and anti-CD95 (Fas) mAb with or without TNF-α (10 ng/mL) in a humidified atmosphere of 95% air and 5% CO2. In some experiments, Fas cross-linking was performed in the presence of the irreversible caspase 3 inhibitor fmk-DEVD (50 μM) (Bachem, Bubendorf, Switzerland). Spleen cells from mutant strains, deficient of Fas (C57BL/6-lpr/lpr) mature T and B cells (C57BL/6-RAG2−/−) or T, B, and NK cells (C57BL/6-RAG2-γc−/−) were compared with the wild type. The NK cell–deficient spleen population from the latter strain was supplemented in some cases with sorted total, B220+, or B220− NK cells (ratio, 5:1) with or without 1 ng/mL mr(s)TNFRI/Fc chimera.
In vitro colony-forming assay
After pretreatment, total colony-forming unit-C (CFU-C) was quantified in complete methylcellulose medium with recombinant cytokines and erythropoietin (Methocult M3434; Stemcell Technologies, Vancouver, Canada) or in MethoCult M3230 (Stemcell Technologies) supplemented routinely with optimal concentrations of murine recombinant IL-3 (1 ng/mL), stem cell factor (100 ng/mL), IL-6 (100 U/mL), and erythropoietin (2 U/mL). Total and sorted cell populations were plated in a final volume of 1 mL at concentrations ranging from 0.2 to 5 × 105 cells per culture dish (Falcon 1008). Colonies were scored on day 7 or 8.
Flow cytometry analysis and intracellular cytokine staining
Cell suspensions were incubated on ice in the presence of rat antimouse CD16/CD32 mAb 2.4G2 (hybridoma supernatant) to block Fc receptor functions before specific staining. Subsequently, cells were washed, pelleted, and labeled with the appropriate antibodies with the use of 3-color immunofluorescence. For intracellular and membrane-associated staining of TNF-α, spleen cells were incubated for 4, 8, and 16 hours in culture medium alone or together with IFN-γ (100 U/mL) and anti-Fas mAb (5 μg/mL). For intracellular staining, brefeldin A (10 nM) was added to prevent protein transport. After incubation, splenocytes were washed twice and were incubated with biotinylated NK1.1 mAb followed by staining with FITC-conjugated anti-CD3 mAb and streptavidin-CyChrome as a second-step reagent. After fixation with 4% PFA for 5 minutes, cells were washed in staining buffer that was supplemented or not supplemented with 0.5% saponin for cell permeabilization. They were then treated for 30 minutes at room temperature with 100-fold diluted PE-conjugated anti–TNF-α mAb or its isotype control in the same buffer. After washing, cells were resuspended in staining buffer to allow membrane closure. To reveal membrane-associated TNF-α, cells were incubated in the same conditions but with the omission brefeldine A and were labeled with the above-mentioned mAbs without fixation and permeabilization. Cells were acquired on a FACScan or a FACSCalibur cytometer (Becton Dickinson, Mountain View, CA) and were analyzed with Cellquest software. At least 10 000 gated cells were acquired in each run.
Statistical analyses
The standard Student t test was used to establish statistical significance.
Results
Effect of anti-Fas mAb plus IFN-γ on CFU-C from total and fractionated spleen cell populations
Starting from our previous evidence for Fas expression and Fas-induced decrease of CFU-C in the presence of IFN-γ,14 we set out to analyze the mechanisms of this process in the murine spleen. We chose this extramedullary site of hematopoiesis because of the increased peripheral myelopoiesis in Fas- or FasL-deficient mice of the lpr or gldgenotype, respectively, as reported earlier.14
As shown in Table 1, the decrease of splenic CFU-C after a 24-hour pre-incubation with anti-Fas mAb and IFN-γ did not occur when cells with lineage-specific markers (CD11b, GR-1, TER119, Thy1.1, B220) were magnetically removed from the total population. This observation suggested that splenic hematopoietic progenitor cells were not directly responsive to Fas activation but required the participation of some mature cell population. Sequential depletion of particular spleen cell subsets revealed that the loss of B220+ cells rendered clonogenic cells as unresponsive to Fas-induced apoptosis as that of all Lin+ cells (Table 1). The population involved did not belong to the B-cell lineage because hematopoietic progenitors from B- and T-cell–deficientRAG2−/− mice decreased as much in response to the treatment with anti-Fas mAb plus IFN-γ as those derived from the wild type (45.8% ± 3.3% in RAG2−/− mice versus 41.9% ± 3.1% in C57BL/6 controls; mean ± SD from 2 separate experiments). As already suggested by this result and confirmed by the normal response of spleen cells from CD3-deficient mice to Fas cross-linking in the presence of IFN-γ (data not shown), T cells did not take part in this process. The same applied to the Mac-1 spleen subset, whose elimination had no effect on Fas-induced apoptosis of CFU-C (data not shown).
Loss of sensitivity of CFU-C to Fas cross-linking after depletion of mature or B220+ spleen cells
| . | CFU-C/106 cells . | ||
|---|---|---|---|
| Total spleen . | Lin− . | B220− . | |
| Medium | 48.3 ± 8.8 | 1133.3 ± 233.3 | 82.7 ± 8.9 |
| IFN-γ | 33.3 ± 4.4 | 1633.3 ± 438.3 | 135.0 ± 9.5 |
| Anti-Fas mAb | 40.0 ± 10.0 | 1533.3 ± 233.3 | 95.7 ± 4.9 |
| Anti-Fas mAb + IFN-γ | 16.7 ± 1.7* | 1100.0 ± 208.0NS | 110.0 ± 5.2NS |
| . | CFU-C/106 cells . | ||
|---|---|---|---|
| Total spleen . | Lin− . | B220− . | |
| Medium | 48.3 ± 8.8 | 1133.3 ± 233.3 | 82.7 ± 8.9 |
| IFN-γ | 33.3 ± 4.4 | 1633.3 ± 438.3 | 135.0 ± 9.5 |
| Anti-Fas mAb | 40.0 ± 10.0 | 1533.3 ± 233.3 | 95.7 ± 4.9 |
| Anti-Fas mAb + IFN-γ | 16.7 ± 1.7* | 1100.0 ± 208.0NS | 110.0 ± 5.2NS |
Total or magnetically depleted Lin− or B220− spleen cells were preincubated for 24 hours at a concentration of 107, 106, or 107cells/mL, respectively. Total and sorted cell populations were plated in a final volume of 1 mL MethoCult at concentrations ranging from 0.2 to 5 × 105 cells per culture dish and scored for colonies on day 7 or 8. Data represent means ± SEM from triplicate determinations of a typical experiment reproduced twice.
NS, not significant in comparison with controls.
P < .05.
Involvement of NK cells in Fas-induced apoptosis of splenic CFU-C
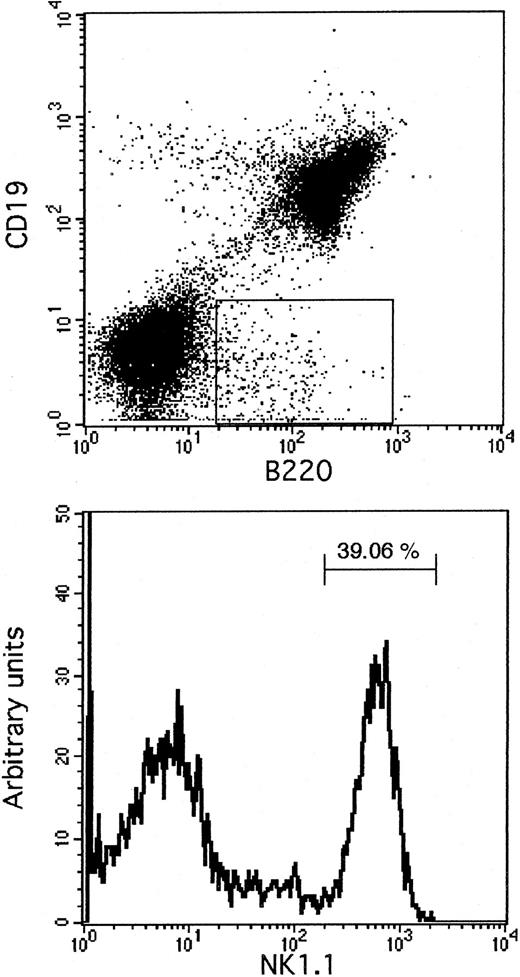
Knowing that the B220 antigen has been described as an activation marker displayed on NK cells,16 17 we analyzed the B220+CD19− spleen cell population for NK1.1 expression. Figure 1 illustrates that 40% of the cells thus gated were positive for this antigen and could therefore represent an NK-cell subset. In contrast, only 3% of the CD19−B220− population was NK1.1+.
NK1.1 expression on spleen cells gated from the B220+CD19− population.
Erythrocyte-depleted spleen cells were treated with Fcγ receptor blocker and labeled with rat antimouse PE-conjugated CD19 and FITC-conjugated CD45R (B220). NK1.1 expression was analyzed using biotinylated mouse antimouse NK1.1 (PK 136) mAb and streptavidin–CyChrome as a second-step reagent.
NK1.1 expression on spleen cells gated from the B220+CD19− population.
Erythrocyte-depleted spleen cells were treated with Fcγ receptor blocker and labeled with rat antimouse PE-conjugated CD19 and FITC-conjugated CD45R (B220). NK1.1 expression was analyzed using biotinylated mouse antimouse NK1.1 (PK 136) mAb and streptavidin–CyChrome as a second-step reagent.
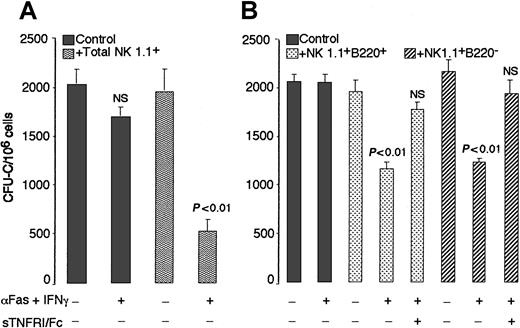
The participation of NK cells in the decrease of splenic CFU-C was confirmed by their in vivo depletion from NKT-deficientβ2m−/− mice, which rendered hematopoietic progenitors unresponsive to Fas cross-linking (Table2). It was further corroborated by the fact that the lack of NK cells in C57BL/6-RAG2-γc−/−mice15 abolished the susceptibility of splenic progenitor cells to Fas-induced apoptosis in the presence of IFN-γ (Figure 2A). Moreover, as shown in the same figure, NK1.1 cells sorted from wild-type spleens and added at a ratio of 1:5 restored the sensitivity of CFU-C from C57BL/6-RAG2-γc−/− mice to Fas cross-linking. Interestingly, this accessory function was not restricted to the B220+ NK subset but was shared by the B220− fraction (Figure 3B).
Loss of sensitivity of splenic CFU-C to Fas-induced apoptosis after in vivo depletion of NK cells
| . | CFU-C/106 cells . | |
|---|---|---|
| Total spleen cells . | NK1.1-depleted . | |
| Medium | 60.7 ± 3.2 | 50.6 ± 3.3 |
| IFN-γ | 74.4 ± 7.0 | 59.3 ± 5.9 |
| Anti-Fas mAb | 65.6 ± 6.6 | 57.8 ± 3.7 |
| Anti-Fas mAb + IFN-γ | 31.1 ± 2.5* | 54.4 ± 5.1NS |
| . | CFU-C/106 cells . | |
|---|---|---|
| Total spleen cells . | NK1.1-depleted . | |
| Medium | 60.7 ± 3.2 | 50.6 ± 3.3 |
| IFN-γ | 74.4 ± 7.0 | 59.3 ± 5.9 |
| Anti-Fas mAb | 65.6 ± 6.6 | 57.8 ± 3.7 |
| Anti-Fas mAb + IFN-γ | 31.1 ± 2.5* | 54.4 ± 5.1NS |
Six-week-old C57BL/6-β2m−/− mice (chosen for their lack of NKT cells) received 2 intraperitoneal injections of 0.5 mg NK1.1 mAb per mouse 1 day and 2 hours before death compared with mice injected with isotype control. Data are means ± SEM from 3 individual mice.
NS, not significant in comparison with control.
P < .001.
sTNFRI/Fc chimera blocks the sensitization of CFU-C from NK cell–deficientRAG2-γc−/−spleens to Fas-induced apoptosis on the addition of sorted NK cells.
(A) Total splenocytes (106 cells/mL) from NK cell–deficient mice were incubated for 24 hours in culture medium or anti-Fas mAb (5 μg/mL) plus IFN-γ (100 U/mL) with or without sorted NK1.1+ cells (2 × 105 cells /mL) from wild-type mice. Cells were then recovered and evaluated for colony growth in methylcellulose. Data are means ± SEM from triplicate determinations and represent the typical results of 1 of 2 experiments. (B) The same experiment was performed with sorted B220+ and B220− NK cell subsets with or without sTNFRI/Fc chimera (10 ng/mL). Data are means ± SEM from triplicate determinations. NS, not significant in comparison with controls.
sTNFRI/Fc chimera blocks the sensitization of CFU-C from NK cell–deficientRAG2-γc−/−spleens to Fas-induced apoptosis on the addition of sorted NK cells.
(A) Total splenocytes (106 cells/mL) from NK cell–deficient mice were incubated for 24 hours in culture medium or anti-Fas mAb (5 μg/mL) plus IFN-γ (100 U/mL) with or without sorted NK1.1+ cells (2 × 105 cells /mL) from wild-type mice. Cells were then recovered and evaluated for colony growth in methylcellulose. Data are means ± SEM from triplicate determinations and represent the typical results of 1 of 2 experiments. (B) The same experiment was performed with sorted B220+ and B220− NK cell subsets with or without sTNFRI/Fc chimera (10 ng/mL). Data are means ± SEM from triplicate determinations. NS, not significant in comparison with controls.
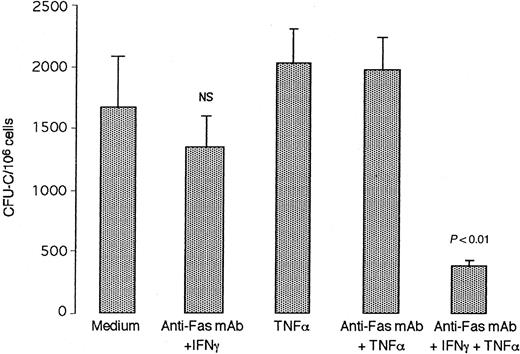
Exogenous TNF-α restores the susceptibility of splenic CFU-C from NK cell–deficient
RAG2-γc−/−mice to Fas cross-linking. Spleen cells were incubated for 24 hours in culture medium alone, TNF-α (10 ng/mL), or anti-Fas mAb (5 μg/mL) combined with IFN-γ (100 U/mL), TNF-α, or both. Cells were then recovered and evaluated for colony growth in methylcellulose. Data are means ± SEM from triplicate determinations.
Exogenous TNF-α restores the susceptibility of splenic CFU-C from NK cell–deficient
RAG2-γc−/−mice to Fas cross-linking. Spleen cells were incubated for 24 hours in culture medium alone, TNF-α (10 ng/mL), or anti-Fas mAb (5 μg/mL) combined with IFN-γ (100 U/mL), TNF-α, or both. Cells were then recovered and evaluated for colony growth in methylcellulose. Data are means ± SEM from triplicate determinations.
Role of NK cell–derived TNF-α in the susceptibility of CFU-C to Fas-induced apoptosis
The requirement of NK cells for the sensitization of CFU-C to the Fas pathway raised the question of their mechanism of action. Because TNF-α/LT– and TNF-αRI–deficient mice did not respond to Fas cross-linking in the presence of IFN-γ (data not shown), we postulated that NK cells might produce sufficient amounts of this cytokine endogenously to make CFU-C responsive to the Fas death pathway. To test this hypothesis, we added TNF-α during the 24-hour preincubation and verified whether, in these conditions, CFU-C from NK-deficient mice recovered their susceptibility to the treatment. As shown in Figure 3, the biologic effect reappeared when splenocytes from C57BL/6-RAG2-γc−/− mice were exposed to anti–Fas-mAb and IFN-γ in the presence of TNF-α, which had no significant effect on its own or in combination with anti-Fas mAb or IFN-γ alone. Furthermore, B220+ and B220− sorted NK cells were no longer effective in the presence of soluble TNFRI/Fc chimera, which acts as a TNFRI antagonist (Figure 2B). It is noteworthy that exogenous TNF-α enhanced the sensitivity of splenic CFU-C of the wild type in some experiments in which Fas cross-linking in the presence of IFN-γ alone had only a slight effect (17.0% ± 4.6% inhibition after pretreatment with anti-Fas mAb + IFN-γ versus 51.4% ± 8.2% on the addition of TNF-α; mean ± SEM from 3 separate experiments). The action of exogenous TNF-α was strictly Fas-dependent because CFU-C from C57BL/6-lpr/lpr spleens decreased neither in response to anti-Fas mAb plus IFN-γ alone nor in combination with TNF-α (data not shown).
The generation of endogenous TNF-α was assessed by intracellular and membrane staining with PE-conjugated anti–TNF-α mAb. As shown in Figure 4, CD3−NK1.1+ cells gated from total splenocytes expressed significant intracellular amounts of the cytokine after 8 hours in culture medium alone or together with anti-Fas mAb plus IFN-γ, whereas freshly isolated cells were not labeled by the antibody or its isotype control. TNF-α was not detected after a 4-hour incubation, and the membrane-associated form appeared only within 16 hours (Figure4). There was no significant difference between the cells exposed to anti-Fas plus IFN-γ and those exposed to culture medium alone. Soluble TNF-α was not detected by enzyme-linked immunosorbent assay in either condition. The preponderance of the membrane-associated form of TNF-α could account for our failure to abrogate the decrease of CFU-C in response to Fas cross-linking with neutralizing anti–TNF-α mAb, which might not have recognized the molecule in this conformation.
Sequential expression of intracellular and membrane-associated TNF-α by NK1.1+ CD3−cells gated from splenocytes.
After 8 hours and 16 hours of incubation in culture medium alone (Ci) or together with anti-Fas mAb (5 μg/mL) plus IFN-γ (100 U/mL) (Cii), intracellular staining of TNF-α was performed according to the manufacturer's instructions (Di and Dii). The membrane-associated form of the cytokine was revealed in the same conditions, except fixation of the cells with PFA and treatment with saponin and brefeldin A. Broken lines represent the isotype control. Intracellular staining of TNF-α in NK1.1+CD3− cells (B) gated from freshly isolated NK cells (A) is shown for comparison.
Sequential expression of intracellular and membrane-associated TNF-α by NK1.1+ CD3−cells gated from splenocytes.
After 8 hours and 16 hours of incubation in culture medium alone (Ci) or together with anti-Fas mAb (5 μg/mL) plus IFN-γ (100 U/mL) (Cii), intracellular staining of TNF-α was performed according to the manufacturer's instructions (Di and Dii). The membrane-associated form of the cytokine was revealed in the same conditions, except fixation of the cells with PFA and treatment with saponin and brefeldin A. Broken lines represent the isotype control. Intracellular staining of TNF-α in NK1.1+CD3− cells (B) gated from freshly isolated NK cells (A) is shown for comparison.
Modulation of Fas expression and implication of caspase 3 in CFU-C apoptosis
We have previously reported that Fas is expressed on progenitor-enriched Lin− cells of the spleen after a 24-hour incubation with IFN-γ.14 We verified in the present study whether, at earlier time points, exogenous TNF-α could affect the expression of this receptor. As shown in Figure5, we observed a significant up-regulation of Fas expression on progenitor-enriched Lin− cells after a 15-hour incubation with IFN-γ or TNF-α that was further enhanced when both factors were present together. Yet, these factors merely accelerated the Fas expression that occurred on all Lin− cells after 24-hour exposure to culture medium alone, possibly because of the participation of endogenous TNF-α (data not shown).
Up-regulation of Fas expression on progenitor-enriched Lin− spleen cells.
Splenocytes were incubated overnight (15 hours) in culture medium alone (broken line) or together with IFN-γ (100 U/mL) (A), TNF-α (10 ng/mL) (B), or both (solid line) (C). Cells bearing lineage markers were labeled with a cocktail of 5-fold diluted hybridoma supernatants (B220, Thy1, TER119, and GR-1) revealed by mouse antirat F(ab')2. After staining with PE-conjugated anti-Fas mAb (Jo2) (broken and solid line) or isotype control (dotted line), Fas expression was analyzed on gated Lin− cells.
Up-regulation of Fas expression on progenitor-enriched Lin− spleen cells.
Splenocytes were incubated overnight (15 hours) in culture medium alone (broken line) or together with IFN-γ (100 U/mL) (A), TNF-α (10 ng/mL) (B), or both (solid line) (C). Cells bearing lineage markers were labeled with a cocktail of 5-fold diluted hybridoma supernatants (B220, Thy1, TER119, and GR-1) revealed by mouse antirat F(ab')2. After staining with PE-conjugated anti-Fas mAb (Jo2) (broken and solid line) or isotype control (dotted line), Fas expression was analyzed on gated Lin− cells.
To evaluate the implication of the caspase cascade in the activation of the Fas pathway in hematopoietic progenitor cells, we performed the pre-incubation with anti-Fas mAb and IFN-γ in the presence of FMK-DEVD, an irreversible inhibitor of caspase 3, which holds a central position in this transduction pathway. It is clear from Figure6 that the decrease of CFU-C is caspase 3–dependent because it did not occur when its activation was blocked. It is also noteworthy that the specific inhibitor abrogated the effect of the cross-linking in the presence of IFN-γ alone or together with TNF-α, indicating that the amplifying effect of the latter involved the same signal transduction pathway.
Irreversible caspase 3 inhibitor fmk-DEVD abrogates the decrease of CFU-C in response to Fas cross-linking in the presence of IFN-γ with or without TNF-α.
Spleen cells were incubated for 24 hours in culture medium alone or in anti-Fas mAb (5 μg/mL) with or without IFN-γ (100 U/mL), TNF-α (10 ng/mL), or both. FMK-DEVD was added 2 hours before the onset of culture at a concentration of 50 μM. IFN-γ, TNF-α, or TNF-α plus anti-Fas mAb had no significant effect compared with culture medium alone (data not shown).
Irreversible caspase 3 inhibitor fmk-DEVD abrogates the decrease of CFU-C in response to Fas cross-linking in the presence of IFN-γ with or without TNF-α.
Spleen cells were incubated for 24 hours in culture medium alone or in anti-Fas mAb (5 μg/mL) with or without IFN-γ (100 U/mL), TNF-α (10 ng/mL), or both. FMK-DEVD was added 2 hours before the onset of culture at a concentration of 50 μM. IFN-γ, TNF-α, or TNF-α plus anti-Fas mAb had no significant effect compared with culture medium alone (data not shown).
Discussion
It is becoming increasingly clear that in addition to cytokine-induced differentiation and proliferation, programmed cell death or apoptosis is crucial in maintaining homeostasis in hematopoietic organs.18-20 Our studies have provided evidence that in the absence of a functional Fas pathway in Fas- or FasL-deficient C57BL/6-lpr/lpr or C57BL/6-gld/gldmice, this equilibrium is disturbed and results in a marked accumulation of hematopoietic progenitors in peripheral organs. Surprisingly, the bone marrow itself is barely affected by these changes because only primitive colony-forming cells (CFU-S) were transiently increased shortly after birth.14 This observation raised the question whether the preservation of medullary homeostasis resulted from the emigration of supernumerary hematopoietic progenitors to peripheral sites or whether clonogenic cells were eventually less susceptible to Fas-induced apoptosis in this particular environment.
The in vitro study initiated by these findings revealed that both early and more lineage-restricted progenitors (CFU-S and CFU-C, respectively) were susceptible to Fas-induced cell death in the bone marrow, provided that IFN-γ was present during the cross-linking with anti-Fas mAb.14 Yet, the treatment was generally more effective in diminishing splenic rather than medullary CFU-C, in accordance with a possible contribution of the microenvironment to this process.
In the present work we provide evidence that the depletion of mature cells from the spleen renders colony-forming progenitors insensitive to Fas cross-linking in the presence of IFN-γ. Surprisingly, the elimination of B220+ cells alone had the same effect. Yet neither B nor T lymphocytes were required for sensitization because colony-forming cells from B- and T-cell–deficient RAG2 mice responded as well to Fas-induced apoptosis as the wild-type cells. We identified the population involved as CD3−NK1.1+ cells, composed of approximately 40% cells bearing the activation marker B220. Indeed, after in vivo depletion of NK1.1+ cells or in the NK-deficientRAG2-γc−/− C57BL/6 strain, splenic CFU-C were no longer diminished after a 24-hour incubation with anti-Fas mAb plus IFN-γ. Furthermore, the addition of sorted NK1.1+ cells toRAG2-γc−/− splenocytes restored the sensitivity of CFU-C to Fas cross-linking whether they belonged to the B220+ or the B220− subset, indicating that they did not have to be activated to exert their effects.
The participation of NK cells in the regulation of hematopoiesis is not altogether surprising considering previous studies in this field.21,22 Yet their actual function has remained controversial, inasmuch as they are potentially capable of exerting both positive and negative effects on hematopoietic progenitor cells through their production of growth-promoting and growth-inhibiting cytokines, such as granulocyte macrophage–colony-stimulating factor and IFN-γ, respectively.23
NK cells are potent cytotoxic effectors that co-express several ligands of the TNF death receptor family, such as FasL, TNF-α, or TRAIL.24-26 They can kill their target cells through perforin- or death receptor–dependent mechanisms and promote ADCC.27,28 In our experimental setup, the latter possibility could be discarded because the decrease of splenic CFU-C on Fas cross-linking failed to occur in the presence of nonactivating anti-Fas mAb, whereas coated and soluble Jo2 mAb had a similar efficiency (data not shown). The implication of NK cell–derived cytokines such as TNF-α seemed a more plausible explanation for the sensitization of CFU-C to the Fas pathway. This notion was in accordance with previous evidence for the cytokine-mediated sensitization of hematopoietic progenitors to the Fas pathway.10,13 29 TNF-α involvement was also indicated because splenic CFU-C from TNFRI−/− mice did not respond to treatment with anti-Fas mAb plus IFN-γ (data not shown). Progenitors from NK cell–depleted or –deficient spleens (B220− orRAG2-γc−/−) recovered their sensitivity with the addition of exogenous TNF-α.
In the same line of evidence, the presence of antagonistic soluble TNFRI/Fc chimera prevented the CFU-C ofRAG2-γc−/− spleens from becoming susceptible to Fas-induced apoptosis with the addition of sorted NK cells. However, TNF-α was neither detected in supernatants from spleen cells incubated for 24 hours with IFN-γ alone or together with anti-Fas mAb, as assessed by enzyme-linked immunosorbent assay, nor was the decrease of CFU-C in response to Fas cross-linking abolished by neutralizing anti–TNF-α mAb. Because staining of NK cells with PE-conjugated anti–TNF-α mAb revealed both intracellular and membrane-associated TNF-α, we presume that its biologic activity is exerted through this latter form, which might not be blocked by the specific antibody. It is indeed widely acknowledged that TNF-α is highly effective as a membrane-bound molecule whose expression on freshly isolated NK cells has recently been reported.30Although other cells, such as activated macrophages, are potential TNF-α producers in the spleen, they probably play a minor role in this situation given that the elimination of the Mac-1+subset does not abolish the susceptibility of CFU-C to the Fas death pathway. TNF-α has no effect either on its own or in combination with anti-Fas mAb; it requires the presence of IFN-γ, which might eventually render CFU-C responsive to TNF-α by modulating its receptor expression.31
It has been documented that both IFN-γ and TNF-α up-regulate Fas on the surfaces of hematopoietic progenitor cells.10 13 A similar modulation occurred in our culture conditions during the first hours of incubation. This is clearly not the principal mechanism by which IFN-γ or TNF-α sensitizes CFU-C to Fas cross-linking because 24 hours in culture medium alone suffices to induce Fas expression on nearly all Lin− cells, possibly with the participation of endogenous TNF-α. Hence, the potentiating effect of IFN-γ alone or in combination with TNF-α must necessarily involve some other mode of action; the most plausible is an enhancement of the signal transduction pathway of Fas.
Indeed, it has been reported that in erythroid cells IFN-γ can activate several of these proteases, namely caspase 3.32The latter is essential in the Fas-induced decrease of CFU-C, which no longer occurred in the presence of the specific inhibitor FMK-DEVD. The biologic effect of TNF-α is likewise mediated through the caspase cascade and may eventually enhance the transduction signal by recruiting additional FADD and caspase 8.33 However, the outcome of its action is complicated by its capacity to convey both apoptotic and survival signals, depending on the sequence of proteases activated in a given target cell.34 This dual action is a possible explanation for the resistance of approximately 50% of CFU-C to Fas ligation. It is also conceivable that the cell cycle status of splenic CFU-C (nearly 50% in cycle) determines the vulnerability to Fas-mediated apoptosis.35
In conclusion, our data provide new insights into the intricate cellular and molecular network that regulates the susceptibility of hematopoietic progenitor cells to Fas-induced cell death. They underscore the importance of the environment for providing the cytokines and cellular interactions, which will determine the fate of these cells. The role of NK cells is particularly important in this context because they produce a number of cytokines and ligands in addition to receptors such as FcγRII (CD32), which have been shown to be involved in apoptosis.36 As far as Fas-induced apoptosis of extramedullary CFU-C is concerned, NK cell–derived TNF-α appears to be the determinant factor. Lower frequency of NK cells and differences in function could be among the causes for the reduced sensitivity of bone marrow CFU-C to Fas-induced cell death. Changes in the cellular environment and its state of activation might also account for a certain variability in the percentage of cell death induced by Fas cross-linking that disappeared as soon as exogenous TNF-α was provided during pre-incubation. This observation is of particular relevance during the immune response, when cytokines such as IFN-γ and TNF-α become readily available in the spleen, where they can participate in the regulation of progenitor cells by modulating their Fas-dependent apoptosis.
We thank Dr Jean Marc Cavaillon (Institut Pasteur, Paris, France) and Dr Claude Jacque (Hospital La Pitié Salpétrière, Paris, France) for kindly providing LT/TNF-α−/− and TNF-αRI−/− mice, respectively, Anne Arnould for technical assistance, and Corinne Garcia for cell sorting.
Supported in part by grant 9742 from the Association pour la Recherche contre le Cancer and a fellowship from the Fondation pour la Recherche Médicale (G.M.).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Elke Schneider, CNRS UMR 8603, Hôpital Necker, 161 rue de Sèvres, 75743 Paris, Cedex 15, France; e-mail:schneider@necker.fr.




This feature is available to Subscribers Only
Sign In or Create an Account Close Modal