Abstract
In addition to myelosuppression, anticancer drugs cause rapid and persistent depletion of lymphocytes, possibly by direct apoptosis induction in mature T and B cells. Induction of apoptosis regulators was analyzed in peripheral blood lymphocytes from pediatric patients undergoing first-cycle chemotherapy for solid tumors. In vivo chemotherapy induced a significant increase in lymphocyte apoptosis ex vivo. The activation of initiator caspase-8 and effector caspase-3 and the cleavage of caspase substrates was detected 12 to 48 hours after the onset of therapy. Caspase inhibition by Z-VAD-fmk did not reduce ex vivo lymphocyte apoptosis in all patients, indicating the additional involvement of caspase-independent cell death. No evidence for the involvement of activation-induced cell death was found in the acute phase of lymphocyte depletion as analyzed by activation marker expression and sensitivity for CD95 signaling. Lymphocyte apoptosis in vivo appeared to be predominantly mediated by the mitochondrial pathway because a marked decrease of mitochondrial membrane potential (ΔΨM) was detected after 24 to 72 hours of treatment, preceded by the increased expression of Bax. Interestingly, despite the use of DNA-damaging agents, p53 remained completely undetectable throughout treatment. In contrast, in vitro treatment with cytarabine and etoposide induced p53 protein, CD95 receptor expression, CD95 sensitivity, and CD95 receptor-ligand interaction in stimulated cycling lymphocytes, but no such induction was seen in resting cells. These data suggest that chemotherapy-induced lymphocyte depletion involves distinct mechanisms of apoptosis induction, such as direct mitochondrial and caspase-dependent pathways in resting cells and p53-dependent pathways in cycling lymphocytes.
Introduction
Anticancer drugs used in chemotherapy for tumors and leukemias inhibit proliferation and induce cell death in malignant cells. In addition to the therapeutic effect on malignant cells, chemotherapy causes severe toxicity in normal tissue, leading to side effects such as mucositis, hair loss, and myelosuppression. In addition, chemotherapy induces acute lymphopenia and chronic depletion of CD4 T cells, leading to increased susceptibility to opportunistic infection.1 2 The molecular mechanisms by which cytotoxic drugs induce depletion of lymphocytes have not been defined and may involve proliferative arrest in lymphocyte precursor compartments or, alternatively, direct induction of apoptosis in mature cells.
Regulation of apoptosis or programmed cell death involves different molecular compartments, such as death receptors,3 Bcl-2 family member proteins,4 mitochondria,5 p53, and caspases.6 In tissue culture cell lines, cytotoxic drugs induce the molecular regulators of physiologic apoptosis7,8 Cytotoxic drug-induced apoptosis in leukemia9 and carcinoma28 cell lines critically depends on the activation of caspases. Caspases are activated by death receptor signaling or are a consequence of mitochondrial alterations including the release of apoptogenic signaling molecules.10
Cross-linking of the CD95 (APO-1, Fas) death receptor forms a death-inducing signaling complex containing FADD. This complex recruits the initiator caspase-8, leading to the activation of caspase-8 and the cleavage of downstream caspases such as caspase-3 and substrates.11 Diverse anticancer drugs such as cisplatin, doxorubicin, mitomycin, fluorouracil, and camptothecin have been found to induce or increase CD95 expression in some tumor cell lines and to increase the sensitivity for CD95-induced apoptosis. In cytostatic drug-induced apoptosis in human T-cell leukemia12 and other tumor cell lines,13-15 doxorubicin and other anticancer drugs have been found to induce CD95 ligand, including CD95 receptor–ligand interaction, a mechanism identified for activation-induced cell death in T cells.16 Death receptor–independent cleavage of the proximal caspase-8, however, has also been found in drug-induced apoptosis.17
Mitochondria-directed apoptotic stimuli induce a variety of mitochondrial changes, among them the production of oxygen radicals and the opening of membrane pores, thereby releasing apoptogenic factors such as cytochrome-c or apoptosis-inducing factor (AIF). By formation of the apoptosome complex, deregulated mitochondria initiate the activation of the caspase cascade through the activation of caspase-9 and caspase-3. Mitochondria-related apoptosis is regulated by Bcl-2 family members, which are involved in cellular response to a variety of apoptotic stimuli including chemotherapeutic agents.18 Cytotoxic drugs induce Bax expression,19 and reduction of the mitochondrial membrane potential—antagonized by Bcl-xL and Bcl-2—is a prerequisite for drug-induced apoptosis,20,21 Activated by DNA-damaging agents,22,23 p53 induces apoptosis pathways by its positive transcriptional activity on pro-apoptotic molecules such as Bax24 and CD95 and its negative regulation of Bcl-2.25 DNA damage and p53 activation may be initial events in cytotoxic drug-induced cytotoxicity.
The diversity of apoptosis pathways involved in drug-induced cytotoxicity has so far been investigated in established tumor cell lines. In this study, we aimed to identify apoptosis pathways activated in the acute depletion of peripheral blood lymphocytes (PBLs) during in vivo chemotherapy. We found that in vivo chemotherapy directly induces apoptosis in mature PBLs involving activation of caspases-3 and -8, reduction of the mitochondrial membrane potential, and induction of Bax. Lymphocytes were activated and highly sensitive to CD95 after chemotherapy, but no involvement of CD95-mediated, activation-induced death could be detected in the acute phase of lymphocyte depletion, nor was p53 expression increased in resting lymphocytes during in vivo chemotherapy. In vitro treatment with cytotoxic drugs induced p53 protein and CD95 receptor–ligand interaction in stimulated, but not in resting, lymphocytes, suggesting differential activation of apoptosis pathways in mature resting, but not in activated, cycling lymphocytes.
Patients and methods
Patients
The study group was composed of 16 children with a median age of 10.25 years (range, 1.9 to 15.4 years) treated for solid tumors at the University Children's Hospital Ulm. The study was performed according to institutional guidelines after approval was given by the Committee for Human Studies. Patients were included in the study after informed consent was obtained from the parents and the child. Chemotherapy consisted of different protocols of the German Society for Pediatric Oncology and Hematology. All patients were studied at their first cycle of chemotherapy unless otherwise indicated.
Samples
Heparinized blood samples were drawn by way of implanted central venous line (Hickman catheter) and forwarded to the clinical research laboratory within 15 minutes. Mononuclear cells (MNCs) were isolated by density-gradient centrifugation (Ficoll-Hypaque; density, 1.077 g/L; Biochrome KG, Berlin, Germany) at 300g for 25 minutes at 20°C, washed twice with Hanks balanced salt solution plus 2% fetal calf serum (HBSS–FCS) at 4°C, and adjusted to 107/mL.
Analysis of activation markers and T-cell enumeration
For each test, 0.5 to 1.0 × 106 cells were incubated with combinations of 4 fluorochrome-conjugated monoclonal antibodies for 25 minutes at 4°C. Antibody combinations used for 4-color fluorescence (fluorescein isothiocyanate [FITC], R-phycoerythrin [PE], PerCP, and allophycocyanine [APC]) were CD4, CD3, CD8, CD45; CD4, HLA-DR, CD8, CD95; CD4, CD25, CD8, CD95; CD4, CD69, CD8, CD95; CD4, CD62L, CD8, CD95; CD45RA, CD95, CD4, CD45RO; CD45RA, CD95, CD8, CD45RO. Antibodies anti-CD4 FITC, -CD3 PE, -CD8 PE, -CD25 PE, -CD69 PE, and -CD45RA FITC were purchased from Coulter/Immunotech, (Krefeld, Germany); all other antibodies were purchased from Becton Dickinson, (Heidelberg, Germany). Samples were washed with HBSS with 2% bovine serum albumin (Serva, Heidelberg, Germany) and 0.2% azide (Merck, Darmstadt, Germany). Samples were fixed with 2% paraformaldehyde and immediately analyzed on a FACSCalibur Cytometer (Becton Dickinson) equipped with a 488-nm argon laser and a 650-nm red diode laser. At least 50 000 events per sample were acquired, stored in list-mode files, and subsequently analyzed with Cell Quest software (Becton Dickinson). Absolute CD4 and CD8 cell numbers were calculated from absolute leukocyte count, percentage of lymphocytes in the differential, and percentage of CD4 and CD8 cells in the lymphocyte gate.
Flow cytometric analysis of mitochondrial transmembrane potential (ΔΨm)
To measure ΔΨm in combination with surface markers, cells were labeled with anti-CD3, -CD4, -CD8, and -CD95 as described above, washed with HBSS–FCS, resuspended at a concentration of 5 × 105/mL, and incubated with 3,3′-dihexyloxacarbocyanine iodide (DiOC6(3), 460 ng/mL; FL-1) (Molecular Probes, Eugene, OR) for 12 minutes at 37°C in the dark, followed by immediate flow cytometric analysis. Incubation with carbonyl cyanide m-chlorophenyl hydrazone mClCCP (Sigma Chemical, Deisenhofen, Germany) served as control for down-regulated ΔΨm.
Ex vivo in vitro cell death assays
Mononuclear cells from patients undergoing chemotherapy were seeded onto 24-well plates at 1.0 × 106/mL in RPMI 1640 with the standard supplements—10% FCS, 200 mM L-glutamine, and 100 U/mL penicillin–streptomycin—and were incubated with 1 μg/mL apoptosis-inducing anti-CD95 (APO-1 IgG3), 1-10 μg/mL blocking anti-CD95 (anti-APO Fab2), 1 to 10 μg/mL neutralizing CD95 ligand antibody Nok2 (BD PharMingen, Heidelberg, Germany), and cytarabine (kindly provided by Pfizer, Karlsruhe, Germany) as positive control. After 24 hours, cells were washed and stained with anti-CD3, -CD4, and -CD8, and apoptosis was analyzed by phosphatidylserine externalization with annexin V–FITC (Boehringer Mannheim, Mannheim, Germany) and forward–side scatter changes.
Western blot analysis
Mononuclear cells were lysed for 30 minutes at 4°C in phosphate-buffered saline with 0.5% Triton-X 100 (Serva) and 1 mM phenylmethylsulfonyl fluoride (Sigma) followed by high-speed centrifugation. In the analyses directly ex vivo, monocytes were not depleted because the percentages of monocytes in the samples were lower than 10% and the cultivation for adherence technique or manipulation in a separation procedure would have induced apoptosis in some of the cells. Protein concentration was assayed using bicinchoninic acid (Pierce, Rockford, IL). Forty micrograms protein per lane was separated by 12% or 15% sodium dodecyl sulfate–polyacrylamide gel electrophoresis and was electroblotted onto nitrocellulose (Amersham Pharmacia, Freiburg, Germany). Equal protein loading was controlled by Ponceau red staining of membranes. After blocking for 1 hour in phosphate-buffered saline supplemented with 2% bovine serum albumin (Sigma) and 0.1% Tween 20 (Sigma), immunodetection of CD95 ligand, Bax, caspases-3 and -8, and poly (ADP-ribose) polymerase (PARP) was performed using mouse anti-CD95L monoclonal antibody (1:250; PharMingen G247) mouse anti–caspase-8 monoclonal antibody C1526 (1:5 dilution of hybridoma supernatant), mouse anti–caspase-3 monoclonal antibody (1:1000; Transduction Laboratories, Lexington, KY), rabbit anti-PARP polyclonal antibody (1:10 000; Enzyme Systems Products, Dublin, CA), and mouse anti-p53 monoclonal antibody (Transduction Laboratories). Goat anti–mouse immunoglobulin G (IgG) or goat anti–rabbit IgG (1:5000; Santa Cruz Biotechnology, Santa Cruz, CA) followed by enhanced chemiluminescence (Amersham Pharmacia) was used for detection.
In vitro studies of drug-induced apoptosis
Mononuclear cells were isolated from buffy coat of healthy blood donors, and monocytes were depleted by culture in plastic flasks for 45 minutes in RPMI 1640 and by harvest of nonadherent cells. One part of the PBLs was directly processed for culture with cytotoxic drugs, whereas the other was stimulated with 5 μg/mL phytohemagglutinin (PHA; Sigma) and 30 U/mL interleukin-2 (IL-2) (Pepro Tech) for 72 hours (day 3 blasts). After stimulation, apoptotic cells were removed by Ficoll-Hypaque density centrifugation, the blasts washed twice, resuspended in complete medium with IL-2, and cultured for 6 and 12 hours at 106 cells/mL with medium, 10 μg/mL cytarabine (kindly provided by Pfizer), and 10 μg/mL etoposide (kindly provided by Bristol Meyer Squibb, Regensburg, Germany).
Because PHA blasts were all CD4 CD45RO memory T-cell type, CD4 T memory cells were identified among PHA blasts and resting PBLs using 4-color flow cytometry with anti-CD3, -CD4, and -CD45RO, and apoptosis was measured by annexin V binding. Drug-specific apoptosis was calculated as follows: [% apoptosis in drug-treated samples − % apoptosis in untreated samples/100 − % spontaneous apoptosis]. Spontaneous apoptosis rates were 5% in resting and 18% in PHA-stimulated lymphocytes at 18 hours. Induction of p53 expression was detected by immunoblot as described above and by flow cytometry after intracellular staining with the anti-p53 antibody Do-7 (BD PharMingen) according to the manufacturer's recommendation.
For analysis of CD95 sensitivity, PBLs and PHA blasts were cultured with medium, cytarabine, and etoposide and were subsequently cultured with and without apoptosis-inducing anti–APO-1 (IgG3) for another 4 hours. Apoptosis in CD4 T memory cells was measured, and CD95-specific apoptosis was calculated as follows: [% apoptosis with anti–APO-1 − % apoptosis without anti–APO-1/100 − % spontaneous apoptosis (CD95-specific cell death)].
For analysis of CD95 receptor–ligand interaction, D3 blasts were cultured with 10 μg/mL etoposide in medium alone, with 0.1 μg/mL apoptosis-inducing anti–APO-1; 1, 5, and 10 μg/100 μL neutralizing CD95 ligand antibody NOK-2; and 10 μg/mL CD95 receptor-blocking anti–APO-1 Fab for 6 and 12 hours. Apoptosis was measured by flow cytometry in CD4 T memory cells as described above.
Results
Lymphocyte depletion and in vitro apoptosis
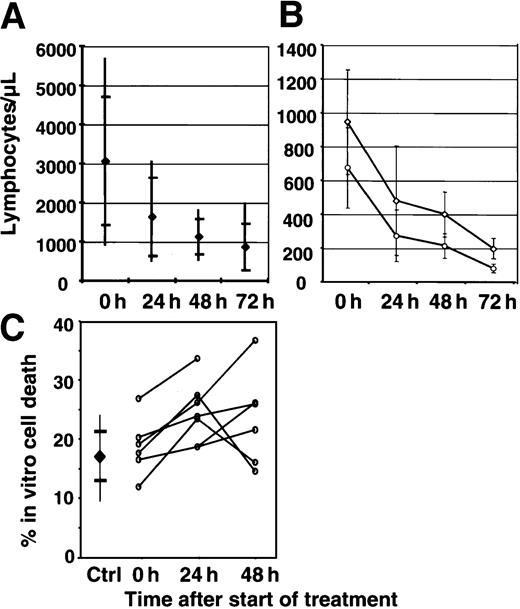
To estimate the kinetics of lymphocyte depletion in patients undergoing first-cycle chemotherapy (Table1), the absolute number of lymphocytes was calculated from PBL differential counts. Unexpectedly, we found a rapid decrease of lymphocyte numbers, from mean values of 2700/μL to 700/μL within 72 hours of treatment. Because the predominant depletion of CD4 T cells after chemotherapy has been reported,2 we investigated, whether CD4 and CD8 cells were differentially reduced. As shown in Figure1B, CD4 and CD8 cells were equally reduced in the acute phase of chemotherapy. In addition, naive resting T cells (CD4+CD45RA+) and memory T cells (CD4+CD45RO+) were equally reduced (data not shown). Thus, chemotherapy rapidly causes a reduction of mature lymphocytes in peripheral blood irrespective of the lymphocyte subtype.
Patients investigated
| Patient . | Diagnosis . | Treatment at time of analysis . |
|---|---|---|
| A1 | Ki-1 lymphoma | Cyclophosphamide, dexamethasone |
| A2 | Ewing sarcoma | Vincristine, Adriamycin, ifosfamide |
| A3 | Ewing sarcoma | Vincristine, Adriamycin, ifosfamide |
| A4 | Peripheral neuroectodermal tumor | Vincristine, actinomycin D, ifosfamide |
| A5 | Peripheral neuroectodermal tumor | Vincristine, actinomycin D, ifosfamide |
| A6 | Hodgkin disease | OEPA: vincristine, Adriamycin, etoposide, prednisolone |
| A7 | Ewing sarcoma | EVAIA: vincristine, doxorubicin, etoposide, ifosfamide |
| A8 | Germ cell tumor | Etoposide, cisplatin, ifosfamide |
| A9 | Neuroblastoma | Vindesine, cisplatin, etoposide |
| A10 | Hodgkin disease | OEPA: vincristine, Adriamycin, etoposide, prednisolone |
| B1 | Osteosarcoma | Doxorubicin |
| B2 | Osteosarcoma | Doxorubicin |
| B3 | Non-Hodgkin lymphoma | Cyclophosphamide, dexamethasone |
| B4 | Osteosarcoma | High-dose methotrexate |
| B5 | Amegakaryocytosis | Busulfan, cyclophosphamide |
| B6 | Nephroblastoma | Actinomycin D, vincristine |
| Patient . | Diagnosis . | Treatment at time of analysis . |
|---|---|---|
| A1 | Ki-1 lymphoma | Cyclophosphamide, dexamethasone |
| A2 | Ewing sarcoma | Vincristine, Adriamycin, ifosfamide |
| A3 | Ewing sarcoma | Vincristine, Adriamycin, ifosfamide |
| A4 | Peripheral neuroectodermal tumor | Vincristine, actinomycin D, ifosfamide |
| A5 | Peripheral neuroectodermal tumor | Vincristine, actinomycin D, ifosfamide |
| A6 | Hodgkin disease | OEPA: vincristine, Adriamycin, etoposide, prednisolone |
| A7 | Ewing sarcoma | EVAIA: vincristine, doxorubicin, etoposide, ifosfamide |
| A8 | Germ cell tumor | Etoposide, cisplatin, ifosfamide |
| A9 | Neuroblastoma | Vindesine, cisplatin, etoposide |
| A10 | Hodgkin disease | OEPA: vincristine, Adriamycin, etoposide, prednisolone |
| B1 | Osteosarcoma | Doxorubicin |
| B2 | Osteosarcoma | Doxorubicin |
| B3 | Non-Hodgkin lymphoma | Cyclophosphamide, dexamethasone |
| B4 | Osteosarcoma | High-dose methotrexate |
| B5 | Amegakaryocytosis | Busulfan, cyclophosphamide |
| B6 | Nephroblastoma | Actinomycin D, vincristine |
Lymphocyte depletion and in vitro apoptosis during chemotherapy.
(A) Kinetics of lymphocyte depletion in patients undergoing chemotherapy. Absolute lymphocyte counts were calculated daily from peripheral blood differentials and leukocyte counts of 7 patients. Mean, 2-sd (standard deviation), and extreme values are depicted in the graph. (B) Analysis of T-cell subset depletion. Absolute CD4 and CD8 T-cell numbers were calculated daily from the peripheral blood differentials and immunophenotyping. Mean and 1-sd values for CD4 cells (open diamonds) and CD8 cells (open circles) are depicted in the graph. (C) Increase of spontaneous in vitro cell death of CD4 T cells during in vivo chemotherapy. PBLs from 7 patients (open circles) were isolated before the start of chemotherapy (0 hour) and during treatment (24 hours, 48 hours). Lymphocytes were cultured for 24 hours in complete medium. CD3+/CD4+ T lymphocytes were analyzed for annexin V binding by flow cytometry. Percentages represent the proportion of annexin V–positive cells of CD4+ T lymphocytes. Mean and 1-sd values of 7 healthy controls are given for the same culture conditions.
Lymphocyte depletion and in vitro apoptosis during chemotherapy.
(A) Kinetics of lymphocyte depletion in patients undergoing chemotherapy. Absolute lymphocyte counts were calculated daily from peripheral blood differentials and leukocyte counts of 7 patients. Mean, 2-sd (standard deviation), and extreme values are depicted in the graph. (B) Analysis of T-cell subset depletion. Absolute CD4 and CD8 T-cell numbers were calculated daily from the peripheral blood differentials and immunophenotyping. Mean and 1-sd values for CD4 cells (open diamonds) and CD8 cells (open circles) are depicted in the graph. (C) Increase of spontaneous in vitro cell death of CD4 T cells during in vivo chemotherapy. PBLs from 7 patients (open circles) were isolated before the start of chemotherapy (0 hour) and during treatment (24 hours, 48 hours). Lymphocytes were cultured for 24 hours in complete medium. CD3+/CD4+ T lymphocytes were analyzed for annexin V binding by flow cytometry. Percentages represent the proportion of annexin V–positive cells of CD4+ T lymphocytes. Mean and 1-sd values of 7 healthy controls are given for the same culture conditions.
Rapid reduction of mature lymphocytes suggested direct induction of lymphocyte death rather than inhibition of precursor cells. Detection of apoptosis in vivo by morphologic changes, DNA fragmentation, or phosphatidylserine externalization is prevented by the rapid clearance of apoptotic cells from peripheral blood. Therefore, we analyzed ex vivo apoptosis of PBLs after 24-hour cultivation during in vivo chemotherapy. As shown in Figure 1C, CD4 T-cell apoptosis significantly increased to above normal levels during treatment, indicating the induction of pro-apoptotic changes in mature peripheral T lymphocytes by in vivo chemotherapy. Similar results were obtained for CD8 T cells, which exhibited a higher rate of spontaneous apoptosis before therapy (data not shown).
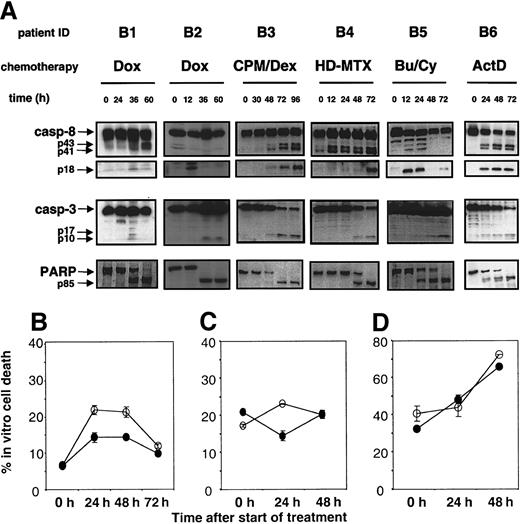
Activation of caspases
To detect caspase activity and to identify caspases activated during chemotherapy, mononuclear cells of patients undergoing chemotherapy were analyzed by immunoblot directly ex vivo. Given that the samples consisted of more than 90% lymphocytes, depletion procedures were not performed so as not to confound the results by additional in vitro manipulation. As shown in Figure2A, caspase activity was detected between 12 and 48 hours after the onset of chemotherapy by the p85 cleavage product of PARP. Activation of the effector caspase 3, shown by the appearance of p17 and p10 subunits, was detected from 36 hours after the start of chemotherapy. Caspase-8 activation, shown by the appearance of the active p18 subunit, could be detected from 12 hours (patients 2 and 5) to 48 hours (patient 3). To estimate the contribution of caspase activation to apoptosis induction in lymphocytes, the effect of caspase inhibition on ex vivo apoptosis in CD4 T cells of 7 patients during chemotherapy was studied. We observed a marked heterogeneity in apoptosis reduction by the caspase inhibitor; Figure 2B-D shows 3 representative examples. In 2 patients, we observed a pattern similar to caspase-dependent cell death of cell lines, whereby the increase of apoptosis during chemotherapy was significantly reduced on incubation with Z-VAD-fmk (Figure 2B). In other patients, caspase inhibition reduced apoptosis 24 hours after the start of chemotherapy but not later (Figure 2C). Finally, in other patients, caspase inhibition did not reduce the chemotherapy-induced increase of ex vivo apoptosis at all (Figure 2D). This heterogeneity indicates the additional involvement of caspase-independent pathways, which may depend on either individual variability or different cytotoxic drugs used for treatment.
Caspase activation by in vivo chemotherapy.
(A) Peripheral blood mononuclear cells from patients undergoing chemotherapy were isolated at different times of treatment as indicated. Caspase-8, caspase-3, and PARP were detected by immunoblot. Arrows indicate the intermediate forms of caspase-8 p43 and p41 and the active subunit p18 in the caspase-8 immunoblot. In the caspase-3 immunoblot, the active subunits p17 and p10 are indicated, whereas in the PARP assay, cleaved PARP at 85 kd is marked by the arrow. (B) Effect of caspase inhibition on spontaneous in vitro apoptosis of CD4 T cells during chemotherapy. Peripheral blood mononuclear cells were isolated at the indicated time of treatment. After cultivation for 24 hours in complete medium (filled circles) or in medium with 50 μM caspase inhibitor Z-VAD (open circles), cells were analyzed by flow cytometry for CD4 and annexin V binding. Bars represent the error of the experiment performed in triplicate. Shown are the results of 3 of 7 representative experiments.
Caspase activation by in vivo chemotherapy.
(A) Peripheral blood mononuclear cells from patients undergoing chemotherapy were isolated at different times of treatment as indicated. Caspase-8, caspase-3, and PARP were detected by immunoblot. Arrows indicate the intermediate forms of caspase-8 p43 and p41 and the active subunit p18 in the caspase-8 immunoblot. In the caspase-3 immunoblot, the active subunits p17 and p10 are indicated, whereas in the PARP assay, cleaved PARP at 85 kd is marked by the arrow. (B) Effect of caspase inhibition on spontaneous in vitro apoptosis of CD4 T cells during chemotherapy. Peripheral blood mononuclear cells were isolated at the indicated time of treatment. After cultivation for 24 hours in complete medium (filled circles) or in medium with 50 μM caspase inhibitor Z-VAD (open circles), cells were analyzed by flow cytometry for CD4 and annexin V binding. Bars represent the error of the experiment performed in triplicate. Shown are the results of 3 of 7 representative experiments.
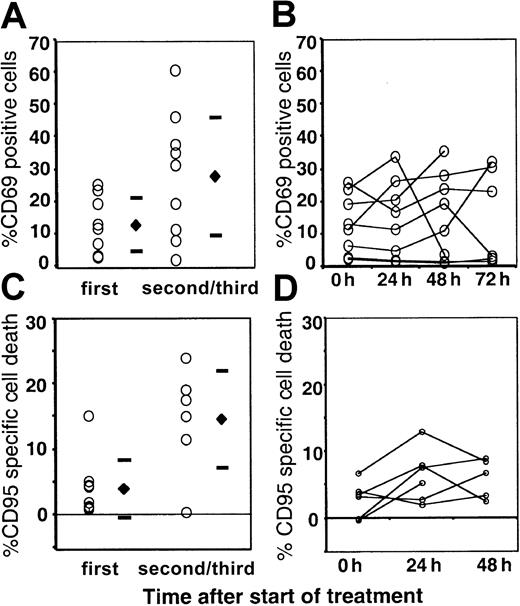
Analysis of activation and CD95-induced cell death in T cells during in vivo chemotherapy
Several investigators have reported an accumulation of activated T cells after chemotherapy with high sensitivity for activation-induced cell death. Early cleavage of caspase-8 may be indicative of CD95 receptor signaling and activation-induced death in T cells. We studied the activation of peripheral blood T cells in 10 patients (A1-A10) during in vivo chemotherapy by flow cytometry. As shown in Figure 3A, the proportion of CD4 T cells expressing CD69 was significantly higher before the second or third cycle of chemotherapy than before the first. There was, however, no increase in CD69 expression during the acute phase of lymphocyte reduction in the first course of chemotherapy (Figure 3B). Analyses were performed for the expression of HLA-DR, CD25, CD62L, and CD95 on CD4/CD45RA−, CD4/CD45RA+, and CD8 T cells with essentially the same results (data not shown). Thus, neither activation markers nor CD95 receptor expression was directly induced by chemotherapy in the acute phase of lymphocyte depletion.
Lymphocyte activation and CD95 sensitivity during chemotherapy.
PBLs were analyzed for expression of CD69 (A, B) and sensitivity for CD95-induced apoptosis (C, D) before the first (1st) and consecutive (2nd/3rd) cycles of chemotherapy (A, C) and during the acute phase of lymphocyte depletion of the first cycle (B, D). Percentage of CD69+ cells of CD4 cells is depicted (A, B). MNCs were cultured in medium with and without death-inducing anti-CD95. Percentage of CD4 cells positive for annexin V was measured after 24 hours, and the percentage of CD95-specific cell death is given in the graphs (B, D).
Lymphocyte activation and CD95 sensitivity during chemotherapy.
PBLs were analyzed for expression of CD69 (A, B) and sensitivity for CD95-induced apoptosis (C, D) before the first (1st) and consecutive (2nd/3rd) cycles of chemotherapy (A, C) and during the acute phase of lymphocyte depletion of the first cycle (B, D). Percentage of CD69+ cells of CD4 cells is depicted (A, B). MNCs were cultured in medium with and without death-inducing anti-CD95. Percentage of CD4 cells positive for annexin V was measured after 24 hours, and the percentage of CD95-specific cell death is given in the graphs (B, D).
To investigate whether in vivo chemotherapy sensitizes for the CD95 signal, we analyzed in vivo–treated lymphocytes for CD95 sensitivity. Again, sensitivity to CD95-mediated cell death was high before the second or third cycle of chemotherapy compared with the first cycle (Figure 3C), but it did not significantly increase during lymphocyte depletion of the first cycle. When we analyzed the influence of receptor blockade on the increase of spontaneous apoptosis during chemotherapy by cultivating in vivo–treated lymphocytes with blocking anti–APO (Fab)2 fragments, no reduction of increased spontaneous apoptosis was found (data not shown). In order not to miss death receptor–mediated lymphocyte apoptosis at early time points, we investigated lymphocytes at 3, 6, and 12 hours after the start of chemotherapy in single patients. Moreover, lymphocytes drawn from patients after the start of chemotherapy were incubated for 3, 6, and 18 hours and were studied for CD95 sensitivity. These results were essentially the same as those in the analysis after 24 hours. Taken together, we found no evidence of activation-induced CD95-mediated death in the acute phase of chemotherapy-induced lymphocyte depletion.
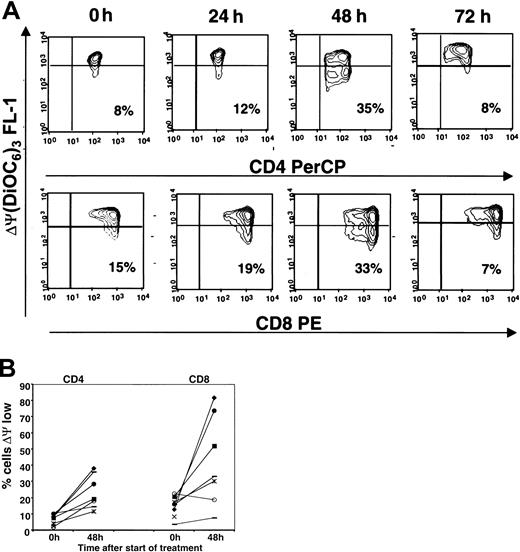
Analysis of mitochondrial membrane potential in T lymphocytes during chemotherapy
In cell lines, cytotoxic drugs induce apoptosis-related mitochondrial alterations including the mitochondrial transmembrane potential (ΔΨM), which is generated by the proton gradient over the inner mitochondrial membrane. The lipophilic cationic dye DiOC6(3) accumulates in the mitochondrial matrix driven by the ΔΨM, and reduction in fluorescence intensity indicates ΔΨM dissipation. Because a sequence of ΔΨM reduction, phosphatidylserine externalization, and cell death has been found in primary lymphocytes in vitro, we investigated whether ΔΨM reduction is induced in PBLs by in vivo chemotherapy.
In peripheral blood mononuclear cells obtained during chemotherapy, T-cell subsets were identified by expression of CD3, CD4, and CD8 and were analyzed for reduced binding of DiOC6(3), as described in “Patients and methods.” Figure 4A shows 3-color analysis of lymphocytes from patient A10 demonstrating an increasing frequency of cells with lowered mitochondrial membrane potential starting within 24 hours of chemotherapy, with a maximum at 48 hours. Using similar analysis in 7 patients (patients A4-A10), a persistent increase in the percentage of cells with low mitochondrial membrane potential during 48 hours of chemotherapy was detected in CD4 and in CD8 T lymphocytes (Figure 4B). Thus, in mature PBLs, pro-apoptotic mitochondrial alterations known to initiate caspase activation and cell death are induced by in vivo chemotherapy.
Induction of mitochondrial membrane permeability transition in CD4 and CD8 T cells by in vivo chemotherapy.
Patients' CD4 and CD8 lymphocytes were analyzed by flow cytometry for lowered uptake of DiOC6(3) indicating inner mitochondrial membrane permeability transition. (A) Contour plots of a representative analysis (patient A10). Fifty thousand cells were acquired in the lymphoid gate. Gating for CD4 and CD8 was performed in the side scatter versus fluorescence plots. Percentages represent the proportion of cells with low mitochondrial membrane potential. (B) For patients A3 to A10, the number of cells with low mitochondrial membrane potential (ΔΨ low) was assessed. The graph depicts pretreatment values (0 hour) and values after 48 hours of chemotherapy for individual patients.
Induction of mitochondrial membrane permeability transition in CD4 and CD8 T cells by in vivo chemotherapy.
Patients' CD4 and CD8 lymphocytes were analyzed by flow cytometry for lowered uptake of DiOC6(3) indicating inner mitochondrial membrane permeability transition. (A) Contour plots of a representative analysis (patient A10). Fifty thousand cells were acquired in the lymphoid gate. Gating for CD4 and CD8 was performed in the side scatter versus fluorescence plots. Percentages represent the proportion of cells with low mitochondrial membrane potential. (B) For patients A3 to A10, the number of cells with low mitochondrial membrane potential (ΔΨ low) was assessed. The graph depicts pretreatment values (0 hour) and values after 48 hours of chemotherapy for individual patients.
Induction of Bax and p53 by in vivo chemotherapy
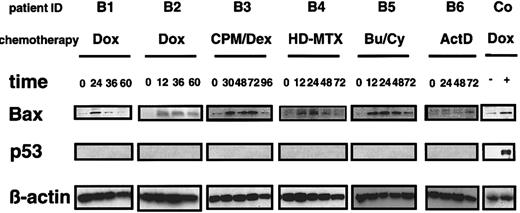
Because mitochondrial changes are regulated by pro-apoptotic Bcl-2 family members, we further investigated whether Bax and its regulator, p53, were induced by chemotherapy. Mononuclear cells obtained during chemotherapy were analyzed for Bax and p53 expression by immunoblot. As shown in Figure 5, Bax expression increased in all patients as early as 12 hours after the start of chemotherapy. Induction was most pronounced in patients B3 and B5, who were treated with the alkylating substances cyclophosphamide and busulfan. Intracellular levels of Bcl-2 measured by flow cytometry remained unchanged during the first 4 days of chemotherapy (data not shown). Interestingly, however, protein levels of p53 remained undetectable during chemotherapy in all patients analyzed. Additional flow cytometric analyses detecting cytoplasmic and nuclear accumulation of p53 confirmed the lack of p53 induction during chemotherapy (data not shown). Thus, in addition to mitochondrial alterations, in vivo chemotherapy induces Bax expression in the absence of detectable increases in p53.
Protein expression of p53 and Bax during chemotherapy.
Mononuclear cells from patients undergoing chemotherapy were isolated at different time points of treatment, as indicated. Shep cells not stimulated or stimulated with doxorubicin 1 μg/mL for 24 hours served as a positive control. Bax and p53 protein were detected by immunoblot. Actin served as control for the equal loading of protein.
Protein expression of p53 and Bax during chemotherapy.
Mononuclear cells from patients undergoing chemotherapy were isolated at different time points of treatment, as indicated. Shep cells not stimulated or stimulated with doxorubicin 1 μg/mL for 24 hours served as a positive control. Bax and p53 protein were detected by immunoblot. Actin served as control for the equal loading of protein.
Activation of p53 and CD95 by cytotoxic drugs in resting and activated peripheral blood lymphocytes in vitro
Because p53 and CD95 have been shown to be induced in drug-induced apoptosis in various tumor cell lines but were not induced in PBLs during chemotherapy, we investigated p53 and CD95 involvement in lymphocyte apoptosis in vitro. Considering that previous studies uniformly used actively cycling cells, we hypothesized that involvement of p53 and CD95 in drug-induced apoptosis might be different in resting lymphocytes than it is in cycling lymphocytes.
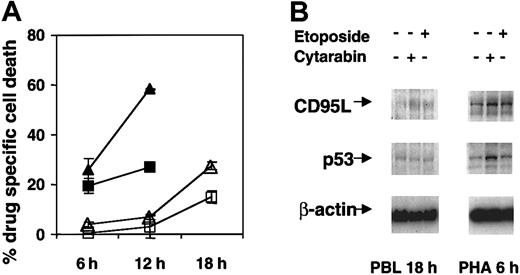
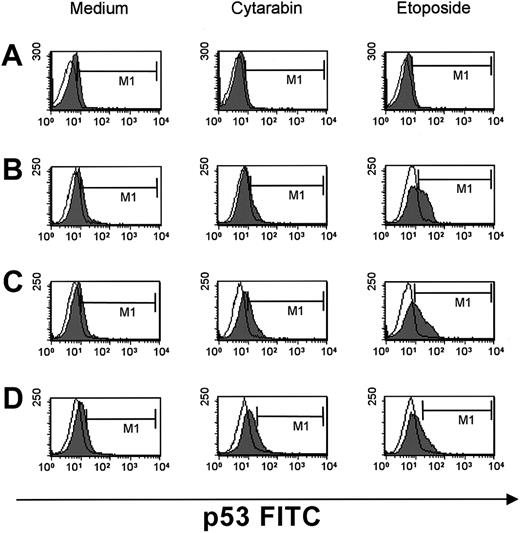
We first compared drug sensitivity in resting versus cycling lymphocytes on drug treatment in vitro. Lymphocytes were cultured with cytotoxic drugs, and drug-specific apoptosis was assessed as described in “Patients and methods.” As shown in Figure6A, stimulated lymphocytes underwent cytarabine- and etoposide-induced apoptosis within 6 hours, whereas significant drug-induced apoptosis in resting lymphocytes was not detectable before 18 hours of treatment. Although p53 protein was readily induced by cytarabine and etoposide in stimulated lymphocytes, expression in resting cells remained low (Figure 6B). We further investigated p53 induction by flow cytometric detection of nuclear and cytoplasmic p53 expression, which allows the exclusion of dead cells by electronic gating. By focusing on the live cell population, quantification of p53 by flow cytometry is more sensitive than Western blot analysis. With this method, p53 induction was detected in stimulated lymphocytes treated with cytarabine or etoposide from 6 to 18 hours (Figure 7B-D), whereas there was no such induction in resting lymphocytes (Figure 7A) as late as 18 hours. The more rapid and pronounced p53 induction in the etoposide-treated lymphocytes correlated with the higher cytotoxicity of etoposide compared to cytarabine shown in Figure 6A. Thus, by 2 independent methods we found differential p53 induction in resting and stimulated lymphocytes.
Cytotoxic drug-induced p53 expression and activation of CD95 in resting versus cycling PHA-stimulated T cells.
(A) Cytotoxic drug-induced death in resting and stimulated CD4 T cells. Unstimulated PBLs (open symbols) and lymphocytes stimulated for 72 hours with PHA and IL-2 (closed symbols) were cultured in medium, 10 μg/mL cytarabine (triangles), and 10 μg/mL etoposide (squares) for 6, 12, and 18 hours. Cells were analyzed by flow cytometry for CD3, CD4, CD45RO, and annexin V binding. Cytotoxic drug-specific cell death was calculated from the proportion of annexin-positive cells of CD4+CD45RO+ T lymphocytes in the treated and untreated samples. Bars represent the standard deviation of the experiment performed in triplicate. Results from a representative experiment of 3 independently performed experiments are shown. (B) Cytotoxic drug-induced protein expression of p53 and CD95 ligand. PBLs and stimulated lymphocytes were cultured in medium, 10 μg/mL cytarabine, and 10 μg/mL etoposide as in panel A. CD95 ligand and p53 were detected by immunoblot at 18 hours for unstimulated lymphocytes and at 6 hours for stimulated lymphocytes.
Cytotoxic drug-induced p53 expression and activation of CD95 in resting versus cycling PHA-stimulated T cells.
(A) Cytotoxic drug-induced death in resting and stimulated CD4 T cells. Unstimulated PBLs (open symbols) and lymphocytes stimulated for 72 hours with PHA and IL-2 (closed symbols) were cultured in medium, 10 μg/mL cytarabine (triangles), and 10 μg/mL etoposide (squares) for 6, 12, and 18 hours. Cells were analyzed by flow cytometry for CD3, CD4, CD45RO, and annexin V binding. Cytotoxic drug-specific cell death was calculated from the proportion of annexin-positive cells of CD4+CD45RO+ T lymphocytes in the treated and untreated samples. Bars represent the standard deviation of the experiment performed in triplicate. Results from a representative experiment of 3 independently performed experiments are shown. (B) Cytotoxic drug-induced protein expression of p53 and CD95 ligand. PBLs and stimulated lymphocytes were cultured in medium, 10 μg/mL cytarabine, and 10 μg/mL etoposide as in panel A. CD95 ligand and p53 were detected by immunoblot at 18 hours for unstimulated lymphocytes and at 6 hours for stimulated lymphocytes.
Induction of p53 in cytotoxic drug-treated resting and stimulated lymphocytes.
PBLs (A) and stimulated lymphocytes (B-D) were cultured in medium, 10 μg/mL cytarabine, and 10 μg/mL etoposide for 6 (B), 12 (C), and 18 hours (A, D). Fluorescence profiles of p53 expression (filled curve) and isotype control (open curve) are depicted.
Induction of p53 in cytotoxic drug-treated resting and stimulated lymphocytes.
PBLs (A) and stimulated lymphocytes (B-D) were cultured in medium, 10 μg/mL cytarabine, and 10 μg/mL etoposide for 6 (B), 12 (C), and 18 hours (A, D). Fluorescence profiles of p53 expression (filled curve) and isotype control (open curve) are depicted.
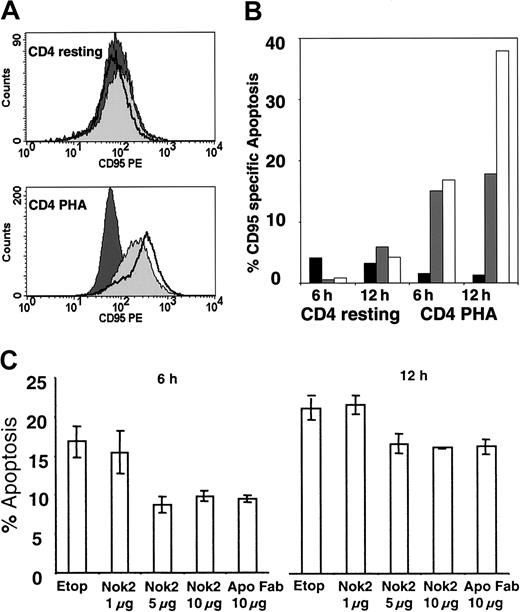
CD95 ligand protein remained unchanged in resting lymphocytes on treatment, whereas the expression of CD95L in stimulated lymphocytes was further induced by cytotoxic drugs (Figure 6B). A similar pattern was found for the CD95 death receptor (Figure8A). CD95 receptor expression was induced by cytarabine and etoposide in stimulated, but not in resting, lymphocytes. In resting lymphocytes, CD95 receptor expression on culture with various drugs, including cytarabine and etoposide, was not altered even after prolonged culture in vitro (data not shown).
Involvement of CD95 in drug-induced apoptosis of resting and activated lymphocytes.
(A) PBLs and stimulated lymphocytes were cultured in medium, cytarabine, and etoposide for 12 hours. CD95 PE fluorescence profiles of CD4+CD45RO+ T lymphocytes after 12-hour culture in medium (filled curve, dark), 10 μg/mL cytarabine (filled curve, light), and 10 μg/mL etoposide (open curve) are depicted. (B) Unstimulated and stimulated lymphocytes were cultured in medium (black), 10 μg/mL cytarabine (gray), and 10 μg/mL etoposide (white) for 6 and 12 hours and subsequently were cultured with and without apoptosis inducing anti–APO-1 (IgG3) for another 4 hours. Percentages represent specific CD95-mediated cell death of CD4+CD45RO+ T lymphocytes. Results from a representative experiment of 3 independently performed experiments are shown. (C) Stimulated lymphocytes were cultured with 10 μg/mL etoposide and neutralizing CD95 ligand antibody NOK-2 and CD95 receptor blocking anti–APO-1 Fab for 6 and 12 hours. Percentages represent the proportion of annexin V–positive cells of CD4+CD45RO+ T lymphocytes. Bars represent the error of the experiment performed in triplicate. Results from a representative experiment of 3 independently performed experiments are shown.
Involvement of CD95 in drug-induced apoptosis of resting and activated lymphocytes.
(A) PBLs and stimulated lymphocytes were cultured in medium, cytarabine, and etoposide for 12 hours. CD95 PE fluorescence profiles of CD4+CD45RO+ T lymphocytes after 12-hour culture in medium (filled curve, dark), 10 μg/mL cytarabine (filled curve, light), and 10 μg/mL etoposide (open curve) are depicted. (B) Unstimulated and stimulated lymphocytes were cultured in medium (black), 10 μg/mL cytarabine (gray), and 10 μg/mL etoposide (white) for 6 and 12 hours and subsequently were cultured with and without apoptosis inducing anti–APO-1 (IgG3) for another 4 hours. Percentages represent specific CD95-mediated cell death of CD4+CD45RO+ T lymphocytes. Results from a representative experiment of 3 independently performed experiments are shown. (C) Stimulated lymphocytes were cultured with 10 μg/mL etoposide and neutralizing CD95 ligand antibody NOK-2 and CD95 receptor blocking anti–APO-1 Fab for 6 and 12 hours. Percentages represent the proportion of annexin V–positive cells of CD4+CD45RO+ T lymphocytes. Bars represent the error of the experiment performed in triplicate. Results from a representative experiment of 3 independently performed experiments are shown.
We next investigated whether sensitivity for CD95-mediated apoptosis would be induced by cytotoxic drugs in stimulated lymphocytes. Lymphocytes were stimulated for 3 days with PHA and IL-2 (day 3 blasts). Constitutive CD95 sensitivity in these cells was still low, which is in line with previous studies reporting increased CD95 sensitivity in stimulated lymphocytes beyond day 6.27 Day 3 blasts were treated with cytotoxic drugs for 6 and 12 hours and subsequently were incubated with apoptosis-inducing anti-CD95 antibody. Cytarabine and etoposide induced a marked sensitivity for CD95-mediated apoptosis in stimulated lymphocytes, whereas no such sensitivity could be detected in resting cells (Figure8B). Finally, we investigated whether CD95-receptor/ligand-mediated cell death contributes to cytotoxic drug-induced apoptosis in stimulated lymphocytes. As shown in Figure 8C, etoposide-induced cell death at 6 and 12 hours was reduced by blocking CD95 with anti–APO-Fab or neutralizing CD95L with an antiligand antibody, indicating that receptor–ligand interaction contributes to drug-induced apoptosis in stimulated lymphocytes. Taken together, the data suggest that drug-induced apoptosis involves p53- and CD95-mediated apoptosis pathways in stimulated, but not in resting, lymphocytes.
Discussion
In the current study, we analyzed different apoptosis regulators in mature PBLs to identify apoptosis pathways activated by in vivo chemotherapy. In our patients receiving the first cycle of chemotherapy for pediatric solid tumors, lymphocytes rapidly declined within 72 hours of the onset of therapy. Considering the longevity of lymphocytes, this rapid decline of lymphocytes in the acute phase of chemotherapy was suggestive of active destruction of mature lymphocytes by apoptosis rather than proliferative arrest in lymphocyte precursors. In fact, we found increased in vitro apoptosis of PBLs during the acute phase of lymphocyte depletion. In addition, pro-apoptotic mitochondrial alterations were induced in these cells, further indicating a direct induction of apoptosis in mature lymphocytes by chemotherapy.
In tumor cell lines, cytotoxic drug-induced apoptosis strictly depends on caspase activation.28-30 In peripheral blood mononuclear cells consisting of more than 90% lymphocytes, we found increased cleavage of caspase substrates and activation of caspases-3 and -8 early after the onset of chemotherapy. However, the effect of caspase inhibition on ex vivo apoptosis of lymphocytes during chemotherapy was heterogeneous. In some patients, caspase inhibition reduced the chemotherapy-induced increase of in vitro cell death, in others, no significant effect could be detected. Interestingly, a caspase-independent pathway has recently been found for CD95-mediated apoptosis in primary T cells.31 Thus, caspase-dependent and -independent death pathways may also contribute to lymphocyte apoptosis mediated by cytotoxic drugs. Inefficiency of caspase inhibition seen in some of the patients probably reflects predominant activation of caspase-independent pathways, which could also vary with the cytotoxic drugs administered.
Activated T cells with a high propensity to apoptosis have been identified in the chronic phase of lymphocyte depletion after chemotherapy.32 33 Therefore we investigated whether chemotherapy directly induces activation of T cells and activation-induced death by way of the CD95 system. We found activation and increased CD95-specific cell death in T cells after chemotherapy. Activation and CD95 sensitivity, however, were not induced during the acute phase of lymphocyte depletion of the first cycle of chemotherapy. It cannot be excluded that activated T cells eliminated through death receptor signaling are no more detectable in peripheral blood at the time of analysis. In some cases, though, lymphocytes were analyzed as early as 3 hours to 6 hours after the onset of in vivo chemotherapy. Still, the lack of a significant number of CD95-sensitive lymphocytes during the acute phase of chemotherapy and the lack of CD95 sensitivity of in vitro–treated resting lymphocytes suggest that chemotherapy-induced acute lymphocyte depletion is largely independent of activation-induced death through CD95. This implicates that activation and CD95 sensitivity seen in PBLs after chemotherapy are not direct effects of cytotoxic drugs but are consequences of altered turnover and expansion of progenitor cells.
In addition, the data indicate that the marked activation of caspase-8 found during acute lymphocyte depletion occurred independently of CD95 receptor signaling. Death receptor–independent cleavage of caspase-8 downstream of mitochondria has been described for betulinic acid–induced apoptosis in neuroblastoma34 and cytotoxic drug induced death in T-cell leukemia cell lines.17 35 It is, therefore, conceivable that chemotherapy-induced activation of caspase-8 in lymphocytes occurs through downstream effector caspases such as caspase-3 or is directly related to mitochondrial alterations.
Mitochondrial alterations such as production of radical oxygen species, disruption of mitochondrial transmembrane potential (ΔΨM), and release of pro-apoptotic molecules from mitochondria indicate the onset of apoptosis.36 In our study, we found that in vivo chemotherapy induced reduction of the mitochondrial membrane potential in PBLs. Several investigators have shown that in primary lymphocytes, ΔΨM reduction is an early sign of apoptosis, preceding phosphatidylserine externalization and cell death. By detection of these early apoptotic mitochondrial alterations during lymphocyte depletion, we provide further evidence that in vivo chemotherapy directly induces apoptosis in mature lymphocytes. Reduced ΔΨM has also been found in T cells of patients with human immunodeficiency virus,37 38indicating that ΔΨM reduction is probably not specific for chemotherapy-induced lymphocyte death but that it may also be involved in lymphocyte apoptosis by other stimuli (eg, viral infection).
Permeability transition of the inner mitochondrial membrane indicated by ΔΨM reduction is a pivotal step in mitochondria-related apoptosis and suggests an involvement of apoptosis pathways directed at mitochondrial membrane integrity. In fact, we found increased Bax expression during in vivo chemotherapy. Cytotoxic drugs induce Bax expression in vitro,19 and Bax homodimerization is known to induce mitochondrial pore formation with a reduction in transmembrane potential and a release of cytochrome-c.39 40 We identified the involvement of mitochondria in acute lymphocyte depletion by 2 mitochondrial apoptosis regulators induced during in vivo chemotherapy.
Several studies have suggested a molecular sequence of apoptosis induction in which DNA-damaging agents induce p53 expression that in turn increases the transcription of Bax for the promotion of apoptosis.24,25 No induction of p53 protein could be detected during chemotherapy, suggesting that in PBLs, Bax, mitochondrial alterations, and caspase activation are independent of p53. In addition, we did not find direct evidence in vivo for activation of the CD95 system, which is partially regulated by p53.41 These data are different from those of several reports in cell lines demonstrating a significant contribution of p53 and the CD95 system in drug-induced apoptosis. Interestingly, marked induction of p53 and CD95 sensitivity by cytotoxic drugs, including receptor–ligand interaction, was detectable only in activated lymphocytes on in vitro stimulation. This suggests that the induction of p53 and CD95 by cytotoxic drugs requires an activated or a cycling state, which is present in cell lines and stimulated lymphocytes in vitro but not in resting lymphocytes. Thus, the lack of detectable activation of p53 or CD95 in PBLs during in vivo chemotherapy is probably caused by differential induction of p53 and CD95 in resting and cycling lymphocytes. In proliferating precursor compartments, however, which could not be analyzed in this study, these death pathways may contribute to the depletion of lymphocyte progenitors. In fact, p53-dependent regulation of recovering bone marrow precursors after chemotherapy has been shown in mice,42 and elevated expression of p53 has been found in human hematopoietic progenitors in the regenerative phase after chemotherapy.43 Recent reports have shown that anthracyclines were equally effective in apoptosis induction in resting and stimulated lymphocytes, whereas topoisomerase inhibitors and antimetabolites were more efficient in activated lymphocytes.44 This suggests that the differential sensitivity of resting and activated lymphocytes, and eventually the degree of p53 induction, may also vary with different drugs. Taken together, our data describe distinct apoptosis pathways operative in the rapid depletion of lymphocytes by in vivo chemotherapy and identify differential involvement of p53 and CD95 in resting and cycling lymphocytes.
We thank Tanja Dravits for excellent technical assistance.
Supported by grants from the Deutsche Forschungsgemeinschaft and Bundesministerium für Bildung und Forschung.
Submitted November 6, 2000; accepted July 9, 2001.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Klaus-Michael Debatin, Department of Pediatrics, University Children's Hospital, Prittwitzstr 43, 89070 Ulm Germany; e-mail: klaus-michael.debatin@medizin.uni-ulm.de.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal