Abstract
Multiple myeloma (MM) remains incurable and novel treatments are urgently needed. Preclinical in vitro and in vivo evaluations were performed to assess the potential therapeutic applications of human recombinant tumor necrosis factor (TNF)–related apoptosis-inducing ligand/Apo2 ligand (TRAIL/Apo2L) in MM. TRAIL/Apo2L potently induced apoptosis of MM cells from patients and the majority of MM cell lines, including cells sensitive or resistant to dexamethasone (Dex), doxorubicin (Dox), melphalan, and mitoxantrone. TRAIL/Apo2L also overcame the survival effect of interleukin 6 on MM cells and did not affect the survival of peripheral blood and bone marrow mononuclear cells and purified B cells from healthy donors. The status of the TRAIL receptors (assessed by immunoblotting and flow cytometry) could not predict TRAIL sensitivity of MM cells. The anti-MM activity of TRAIL/Apo2L was confirmed in nu/xid/bg mice xenografted with human MM cells; TRAIL (500 μg intraperitoneally daily for 14 days) was well tolerated and significantly suppressed the growth of plasmacytomas. Dox up-regulated the expression of the TRAIL receptor death receptor 5 (DR5) and synergistically enhanced the effect of TRAIL not only against MM cells sensitive to, but also against those resistant to, Dex- or Dox-induced apoptosis. Nuclear factor (NF)-κB inhibitors, such as SN50 (a cell-permeable inhibitor of the nuclear translocation and transcriptional activity of NF-κB) or the proteasome inhibitor PS-341, enhanced the proapoptotic activity of TRAIL/Apo2L against TRAIL-sensitive MM cells, whereas SN50 reversed the TRAIL resistance of ARH-77 and IM-9 MM cells. Importantly, normal B lymphocytes were not sensitized to TRAIL by either Dox, SN50, or PS-341. These preclinical studies suggest that TRAIL/Apo2L can overcome conventional drug resistance and provide the basis for clinical trials of TRAIL-based treatment regimens to improve outcome in patients with MM.
Introduction
The uniformly fatal outcome of multiple myeloma (MM)1-3 warrants the development of novel biologically based treatment strategies that selectively induce apoptosis of malignant plasma cells. One such approach involves tumor necrosis factor (TNF)–related apoptosis-inducing ligand or Apo2 ligand (TRAIL/Apo2L), a member of a superfamily of cell death-inducing ligands that also includes TNF-α and Fas ligand (FasL or CD95L).4 TRAIL/Apo2L induces apoptosis of malignant cells by interacting with a complex system of cell surface receptors, including the death signal-transducing receptors DR4 and DR5. These 2 receptors transmit a proapoptotic signal via interaction of their intracellular death domains with adaptor protein(s), which are not well characterized. The death effector domain of these adaptor(s) constitutively bind(s) to caspases, initiating a cascade of proteolytic activation of downstream caspases and apoptosis.5 In contrast to the DR4 and DR5 receptors, 2 other cell surface TRAIL receptors (DcR1, DcR2) lack a functional death domain and cannot transduce a proapoptotic signal; hence, they are considered “decoy receptors,” which compete with DR4 and DR5 for cell surface TRAIL binding. This complex system of TRAIL receptors, and in particular the expression of decoy receptors on normal cells, was initially postulated to be the basis for the specificity of TRAIL's proapoptotic action against cancer cells.6
TRAIL/Apo2L induces apoptosis in tumor cells of diverse origins,4,6-15 both in vitro and in various in vivo tumor models. In contrast, TRAIL/Apo2L is not toxic to most normal human cells in vitro,8-10 or to TRAIL-treated animals,4,7 even though the messenger RNAs for TRAIL receptors are expressed in a wide range of normal tissues.16 This favorable profile of TRAIL in various tumor models prompted us to investigate whether this death ligand is active against MM cells.17
In this study, we show that TRAIL/Apo2L selectively induces apoptosis of human MM cells, including MM cell lines, both sensitive and resistant to dexamethasone (Dex) and chemotherapy, as well as patient MM cells, and exhibits in vivo anti-MM activity in mice xenografted with human plasmacytomas. Moreover, doxorubicin (Dox) and agents that inhibit NF-κB augment the activity of TRAIL/Apo2L in MM cells, but not in normal B cells. These studies provide the rationale for use of TRAIL/Apo2L as a novel therapeutic agent in MM.
Materials and methods
MM cell lines and MM patient cells
The Dex-sensitive MM-1S and Dex-resistant MM-1R human MM cell lines were kindly provided by Dr Steven Rosen (Northwestern University, Chicago, IL); RPMI-8226/S cells and their doxorubicin- (Dox6, Dox40), melphalan (LR5)-, and mitoxantrone (MR20)-resistant sublines by Dr William Dalton (Lee Moffit Cancer Center, Tampa, FL); OCI-My-5 cells by Dr H. A. Messner (Ontario Cancer Institute, ON, Canada); S6B45 cells by Dr T. Kishimoto (Osaka University, Osaka, Japan); ARP-1 cells by Dr O. Bajenova (Boston University, Boston, MA); and DHL4 and DHL10 diffuse large B-cell non-Hodgkin lymphoma (NHL) lines by Dr Margaret Shipp (Dana Farber Cancer Institute, Boston, MA). U266, ARH-77, HS-Sultan, and IM-9 human MM cell lines were obtained from the American Type Culture Collection (Rockville, MD). The MM-AS and MM-SV cell lines were established from samples from 2 MM patients.18 Fresh MM cells from 5 patients, including bone marrow mononuclear cells (BMMCs) of 3 patients and leukemic plasma cells from 2 patients, were initially processed by Ficoll density centrifugation and incubated with TRAIL, either in unpurified form or following tumor cell isolation by using an EPICS cell sorter (Coulter, Hialeah, FL). Tumor cell sorting from the 2 plasma cell leukemic samples was performed following staining with anti-CD38 fluorescein isothiocyanate (FITC)–conjugated monoclonal antibody (mAb; Beckman-Coulter, Miami, FL) and anti-CD45RA-phycoerythrin (PE)–conjugated mAb (Beckman-Coulter/Immunotech, Miami, FL). Tumor cells from the BMMCs of 1 MM patient were sorted after staining for anti-CD138-PE mAb (Immunotech, Westbrook, ME) and anti-CD38 FITC mAb. Two MM BMMC samples were used in our studies in unpurified form. All sorted tumor cell samples had more than 95% purity in CD38+CD138+ or CD38+ CD45RA− cells. Immediately prior to TRAIL/Apo2L treatment studies, all tumor samples were confirmed to have more than 95% viability, by trypan blue exclusion assay. All MM cell lines and patient MM cells were cultured in RPMI 1640 medium (Gibco Laboratories, Grand Island, NY) supplemented with 10% charcoal dextran-treated fetal bovine serum (FBS; Hyclone, Logan, UT) as well as l-glutamine, penicillin, and streptomycin (Gibco Laboratories).
Reagents
Recombinant human TRAIL was obtained from Immunex Corporation (Seattle, WA), in a leucine zipper (LZ) form.4 Goat polyclonal antibodies for human DR4, DR5, and DcR1 were obtained from Santa Cruz Biotechnology (Santa Cruz, CA); mAbs for DR4, DR5, DcR1, and DcR2 were from Genentech (San Francisco, CA); mouse MsIgG1 and MsIgG2b isotype controls, as well as the annexin V-PI early apoptosis detection kit, the Apo2.7-PE mAb, and the 2H4 antihuman CD45RA-FITC mAb from Beckman Coulter/Immunotech; interleukin 6 (IL-6), goat antihuman DR4, DR5, and DcR2 polyclonal antibodies from R&D Systems (Minneapolis, MN); antihuman DcR2 rabbit polyclonal antibody from Imgenex (San Diego, CA); rabbit antihuman DcR1 polyclonal antibody from Affinity Bioreagents (Golden, CO); goat antimouse IgG (FITC)-conjugated F(ab′)2fragment, donkey antigoat IgG FITC-conjugated F(ab′)2fragment, and donkey antirabbit IgG FITC-conjugated F(ab′)2fragment from Jackson Immunoresearch Laboratories (West Grove, PA); MTT and doxorubicin from Sigma Chemical (St Louis, MO); the inhibitory peptide SN50 and its mutant control peptide SN50M from BIOMOL (Plymouth Meeting, PA); the proteasome inhibitor PS-341 from Millenium Pharmaceuticals (Cambridge, MA); complete-TM mixture of proteinase inhibitors, Ig-free normal horse serum and sodium dodecyl sulfate (SDS) from Life Technologies (Gaithersburg, MD); and the enhanced chemiluminescence (ECL) kit, which includes the peroxidase-labeled antimouse and antirabbit secondary antibodies, from Amersham (Arlington Heights, IL).
Determination of TRAIL receptor status by immunoblotting
Cell extracts from 10 MM cell lines (ARH-77, OCI-My-5, RPMI-8226/S, S6B45, U266, IM-9, HS-Sultan, MM-1S, MM-AS, and MM-SV) were examined by Western blot analysis for the expression of the DR4, DR5, DcR1, and DcR2 receptors for TRAIL/Apo2L. The Ewing sarcoma cell line SK-N-MC and the DHL-4 and DHL-10 cells served as positive controls for TRAIL/Apo2L receptor expression, as previously documented.15 Immunoblotting analysis was performed as previously described,19 and equal protein loading was confirmed by tubulin detection.
Determination of TRAIL receptor status by flow cytometric analysis
The MM cells were characterized for their surface expression of TRAIL receptors by flow cytometry. HeLa cells served as positive control for DR4/DR5 expression and as negative controls for DcR1 and DcR2 expression. SK-N-MC and CHP100S Ewing sarcoma cells served as negative controls for surface expression of DR4 and DR5, respectively. DHL-10 cells served as positive control for DcR1 and DcR2 expression. Staining was performed as previously described.20 21Briefly, for each cell line, 106 cells were incubated with the appropriate anti-TRAIL receptor antibody or a respective control (5.0 μg) for 45 minutes. Specifically, DR4 and DR5 expression was assessed with anti-DR4 and anti-DR5 mAbs (mouse IgG1 and IgG2b as respective controls) and confirmed with goat antihuman DR4 and DR5 polyclonal antibodies, using goat IgG for control staining. DcR1 and DcR2 expression was assessed with mouse anti-DcR1 and DcR2 mAbs and goat anti-DcR1 (or rabbit anti-DcR1) and goat anti-DcR2 polyclonal antibodies. Cells were then washed with phosphate-buffered saline (PBS) and incubated for 45 minutes with 2.0 μg goat antimouse IgG FITC-conjugated F(ab′)2 fragment for anti-DR4 and anti-DR5 mAb phenotypic analyses or with a donkey antigoat IgG FITC-conjugated F(ab′)2 fragment for the DcR1, DcR2, DR4, and DR5 analyses with the goat polyclonal antibodies. Cells were then washed, fixed with 1% formaldehyde PBS, and analyzed on a EPICS-XL-MCL flow cytometer (Coulter).
Survival, death, and apoptosis assays
The effect of TRAIL/Apo2L on the survival of MM cells was examined by cell cycle analyses, using propidium iodine (PI) staining to detect cells in sub-G1 gate, as previously reported22 and 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) colorimetric assays, as previously described.14 Induction of apoptosis was confirmed and quantitatively assessed by annexin V/PI staining and Apo2.7 staining.
PI staining.
For cell cycle analysis, 1 × 106 MM cells were incubated with 0.001 to 1000 ng/mL LZ-TRAIL for 24 to 48 hours. The cells were then washed twice with PBS, permeabilized with 70% ethanol in PBS for 30 minutes at 4°C, incubated with 0.5 mL of a 50-μg/mL PI solution containing 20 U/mL RNaseA (Boehringer Mannheim, Indianapolis, IN) for 30 minutes, and analyzed by flow cytometry.
MTT colorimetric assay.
Cells were plated in 48-well plates to 70% to 80% confluence and then incubated for 18 hours at 37°C with LZ-TRAIL (10-1000 ng/mL) in 2.5% or 10% bovine serum–supplemented RPMI medium. In some experiments, MM cells were preincubated with doxorubicin (250 or 500 ng/mL for 4 hours), the NF-κB inhibitory peptide SN50 (or its mutant control peptide SN50M) at 30 ng/mL for 3 hours, or the proteasome inhibitor PS341 (0.1 μM for 4 hours) prior to exposure to TRAIL. All experiments were repeated at least twice, and each experimental condition was repeated at least in quadruplicate wells in each experiment. At the end of each treatment, cells were incubated with 1 mg/mL MTT in fresh media for 4 hours at 37°C. A mixture of isopropanol and 1 N HCl (24:1, v/v) was added under vigorous pipetting to dissolve the formazan crystals. Dye absorbance (A) in viable cells was measured at 570 nm, with 630 nm as a reference wavelength.
Annexin V/PI staining.
Detection of early apoptotic cells was performed with the annexin V-PI detection kit (Immunotech/Beckman Coulter). Briefly, 106 MM cells were exposed for 4 hours to TRAIL or media, washed with Dulbecco modified Eagle medium (DMEM), incubated in the dark at 4°C with annexin V-FITC and PI for 15 minutes, and then analyzed by dual-color flow cytometry. Cells that were annexin V-FITC+ (with translocation of phosphatidylserine from the inner to the outer leaflet of the plasma membrane) and PI− (with intact cellular membrane) were considered as early apoptotic cells.
Apo2.7 staining.
Quantification of apoptosis induction was also performed by Apo2.7 immunostaining, which specifically detects the 38-kd mitochondrial membrane antigen 7A6 that is exposed on the mitochondrial membrane of apoptotic cells only and can be used as a late apoptotic marker in nonpermeabilized cells.23 24 MM cells cultured for 18 hours with TRAIL or media were labeled with the Apo2.7-PE conjugated mAb or mouse IgG1 isotype control, and subsequently analyzed by flow cytometry.
Effect of IL-6 on TRAIL-induced apoptosis
Sensitization to TRAIL-induced apoptosis by Dox, NF-κB inhibitor, and proteasome inhibitor
The MM-1S and Dex-resistant MM-1R cells, as well as the RPMI-8226/S and the Dox-resistant RPMI-8226/Dox40 cells, were preincubated with Dox (250 or 500 ng/mL) for 4 hours. MM-1S, RPMI-8226/S, ARH-77, and IM-9 cells were pretreated for 4 hours with the NF-κB inhibitory peptide SN-50 or its mutant control peptide SN-50M. MM-1S cells were also preincubated with 0.1 μM of the proteasome inhibitor PS-341 for 4 hours. Following each of these pretreatments, TRAIL (50 or 100 ng/mL) was added for 18 hours, and the samples were analyzed by MTT assay.
Effect of TRAIL on healthy donor B cells
Peripheral blood B cells were obtained from 5 healthy donors by Ficoll-Hypaque (Pharmacia) density centrifugation of peripheral blood mononuclear cells (PBMCs), depletion of monocytes by overnight adhesion on plastic, and enrichment for B cells either by removal of T cells by sheep red blood cell rosetting or by positive selection for CD19+ cells by fluorescence-activated cell sorting. B cells (> 85% CD19+) or unpurified PBMCs or BMMCs were exposed to TRAIL (10-1000 ng/mL) for 18 to 24 hours. Normal PBMCs or B cells were also pretreated with Dox, PS-341, or SN50 before exposure to TRAIL (50-100 ng/mL).
In vivo administration of TRAIL to nu/xid/bg mice xenografted with human plasmacytomas
Six- to 8-week-old male nu/xid/bg mice obtained from Jackson Laboratories (Wilmington, DE) were cared for in the animal research facility of the Dana-Farber Cancer Institute in accordance with National Institutes of Health (NIH) guidelines and those of the Animal Care and Use Committee at our institution. Mice were engrafted with 107 S6B45 human MM cells by subcutaneous injection in the right flank. On formation of a palpable tumor, mice were randomly placed into 2 cohorts of 8 mice and received either PBS or recombinant human TRAIL at 500 μg daily by intraperitoneal administration for 14 consecutive days. Tumor volumes and weights for the treated mice were obtained every other day.
Statistical analysis
The potential correlation of TRAIL receptor status profile with the sensitivity or resistance of each cell line to TRAIL was evaluated with the use of the McNemar paired χ2 test. The tumor volumes of human plasmacytoma xenografts (at days 1, 5, 8, 11, 14, and 18 after initiation of TRAIL administration) were compared with the PBS-treated controls by the Mann-Whitney U test. One-way analysis of variance and the Duncan post hoc test was performed to compare, within the TRAIL-treated cohort (or the control group), the tumor volumes at different time points of the study. Interactions between TRAIL and Dox, NF-κB inhibitory peptide, or PS-341 were classified by the fractional inhibition method, as previously described,27 and also examined by a 2-way analysis of variance, followed by the Duncan post hoc test. A P value less than .05 was considered statistically significant.
Results
TRAIL/Apo2L induces apoptosis of MM cell lines and MM patient cells
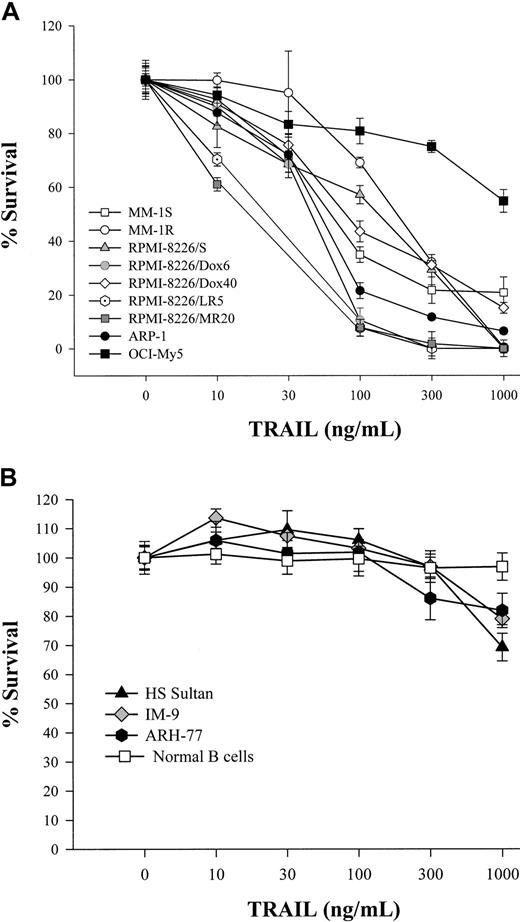
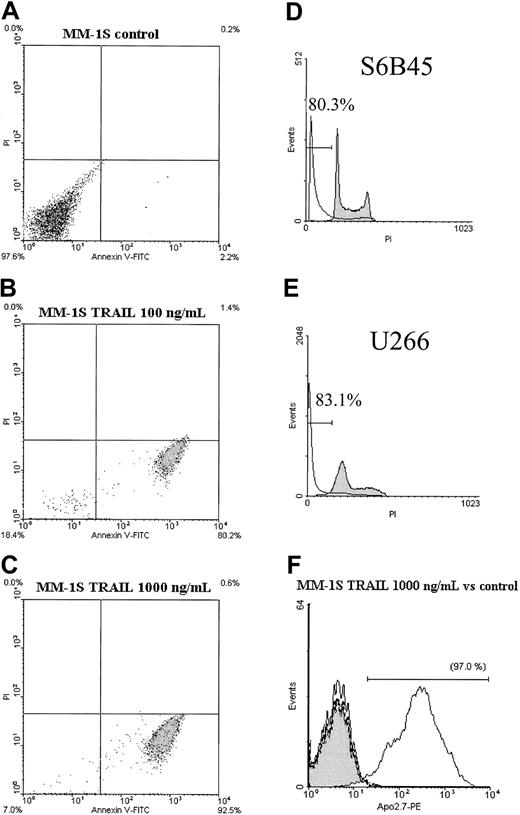
We first determined the effect of TRAIL/Apo2L on chemotherapy-sensitive and chemotherapy-resistant MM cell lines, as well as patient MM cells. In 10 of 16 lines tested (ARP-1, MM-1S, MM-1R, RPMI-8226/S, Dox6, Dox40, LR5, MR20, U266, and S6B45), TRAIL/Apo2L induced significant reductions in cell survival (with median effective dose values of < 300 ng/mL), assessed by the MTT assay (Figure 1A). Five MM lines, ARH-77, HS Sultan, IM-9 (Figure 1B), MM-AS, and MM-SV cells (data not shown) had more than 70% survival after exposure to doses of TRAIL/Apo2L as high as 1000 ng/mL and were considered TRAIL resistant. The OCI-My5 cells had an intermediate pattern of TRAIL-induced cell death, with about 50% survival at a TRAIL dose of 1000 ng/mL (Figure 1A), indicating moderate TRAIL sensitivity. The TRAIL sensitivity or resistance of MM cells was confirmed by annexin V-FITC/PI staining (for detection of early apoptotic annexin V+ PI−cells) (Figure 2A-C), cell cycle analysis following PI staining (Figure 2D,E), and staining with the Apo2.7 mAb for detection of late apoptotic cells (Figure 2F).
MTT assay of MM cells and healthy donor B cells cultured with human recombinant TRAIL.
Dose-response survival curves based on MTT colorimetric assay were generated for MM cells and healthy donor B cells cultured for 18 hours with TRAIL (10-1000 ng/mL). (A) Dose-response survival curves are shown for TRAIL-sensitive MM cell lines ARP-1; Dex-sensitive MM-1S and Dex-resistant MM-1R; RPMI-8226/S and its cytotoxic drug-resistant sublines Dox6, Dox40, MR20, and LR5; as well as the response of OCI-My5 cells, which have intermediate TRAIL sensitivity. (B) Dose-response survival curves are shown for TRAIL-resistant ARH-77, HS Sultan, and IM-9 MM cells, as well as healthy donor peripheral blood B cells.
MTT assay of MM cells and healthy donor B cells cultured with human recombinant TRAIL.
Dose-response survival curves based on MTT colorimetric assay were generated for MM cells and healthy donor B cells cultured for 18 hours with TRAIL (10-1000 ng/mL). (A) Dose-response survival curves are shown for TRAIL-sensitive MM cell lines ARP-1; Dex-sensitive MM-1S and Dex-resistant MM-1R; RPMI-8226/S and its cytotoxic drug-resistant sublines Dox6, Dox40, MR20, and LR5; as well as the response of OCI-My5 cells, which have intermediate TRAIL sensitivity. (B) Dose-response survival curves are shown for TRAIL-resistant ARH-77, HS Sultan, and IM-9 MM cells, as well as healthy donor peripheral blood B cells.
Annexin/PI staining, cell cycle analysis, and Apo2.7 staining of MM cells cultured with human recombinant TRAIL.
(A-C) MM cells were cultured with TRAIL (100 and 1000 ng/mL) for 4 hours. Representative dual staining for annexin-FITC/(PI) indicates significant induction of apoptotic cell death (annexin+PI− status) of MM-1S MM cells. (D,E) Representative PI staining of MM cells following 24-hour culture with TRAIL (1000 ng/mL) or control cultures. The percentage of cells in the sub-G1region (indicated in each graph) documents the significant TRAIL-induced cell death of S6B45 and U266 cells. (F) Detection of late apoptosis by staining with the Apo2.7 mAb. The curves corresponding to the MsIgG1-PE control for the TRAIL-treated (standard line) and control (dotted line) cultures of MM-1S cells are superimposable with the (shaded) curve for Apo2.7 staining in the control culture. In contrast, TRAIL-treated MM cells have strong staining for the Apo2.7 (unshaded curve), which is consistent with extensive induction of cell death.
Annexin/PI staining, cell cycle analysis, and Apo2.7 staining of MM cells cultured with human recombinant TRAIL.
(A-C) MM cells were cultured with TRAIL (100 and 1000 ng/mL) for 4 hours. Representative dual staining for annexin-FITC/(PI) indicates significant induction of apoptotic cell death (annexin+PI− status) of MM-1S MM cells. (D,E) Representative PI staining of MM cells following 24-hour culture with TRAIL (1000 ng/mL) or control cultures. The percentage of cells in the sub-G1region (indicated in each graph) documents the significant TRAIL-induced cell death of S6B45 and U266 cells. (F) Detection of late apoptosis by staining with the Apo2.7 mAb. The curves corresponding to the MsIgG1-PE control for the TRAIL-treated (standard line) and control (dotted line) cultures of MM-1S cells are superimposable with the (shaded) curve for Apo2.7 staining in the control culture. In contrast, TRAIL-treated MM cells have strong staining for the Apo2.7 (unshaded curve), which is consistent with extensive induction of cell death.
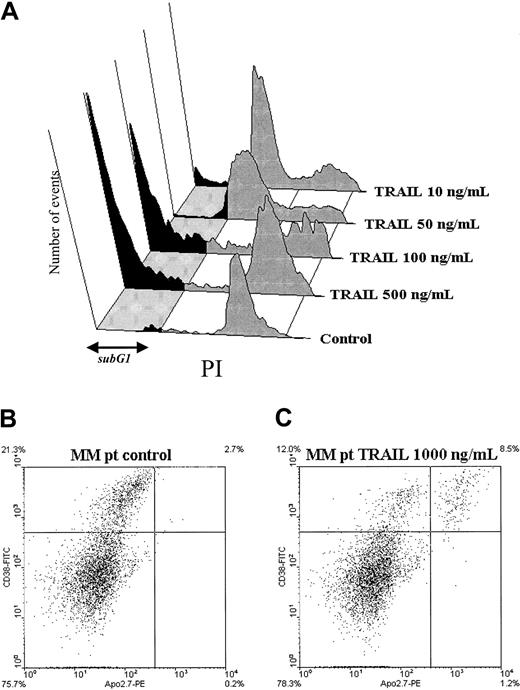
We also evaluated the effect of TRAIL/Apo2L on freshly isolated MM cells from 5 patients. MM (CD38+/CD45RA−) cells treated with TRAIL (≥ 100 ng/mL) had significant increases, compared to control, in the fraction of sub-G1 cells (Figure 3). In contrast, normal B cells were resistant to TRAIL concentrations as high as 1000 ng/mL (Figure4A). Apoptosis of MM patient BMMCs cultured for 18 hours with TRAIL (1000 and 300 ng/mL) was also assessed by dual-color flow cytometry for CD38-FITC/Apo2.7-PE (to detect late apoptotic Apo2.7+/CD38+ cells). Control cultures stained with CD38-FITC and Apo2.7-PE (Figure 3B) indicated very few late apoptotic cells in either CD38+ or CD38− BMMCs. In contrast, treatment with TRAIL at 1000 ng/mL (Figure 3C) or 300 ng/mL (data not shown) led to a distinct population of late apoptotic Apo2.7+ cells within the CD38+ fraction, which contains the MM cells; approximately 40% and 35% of CD38+ cells were also Apo2.7+after treatment with TRAIL at 1000 (Figure 3C) and 300 ng/mL (data not shown), respectively. Importantly, in none of TRAIL-treated cultures did we detect any increase in Apo2.7+ cells among the CD38− (non-MM BMMC) population (< 2.5% of Apo2.7+/CD38− cells in either TRAIL-treated or control cultures). Further analysis by staining of TRAIL-treated cells with anti-CD45RA-FITC mAb confirmed Apo2.7+ staining of only CD38+/CD45RA− BMMCs (data not shown), indicating selective killing of myeloma cells. These findings are consistent with the notion that TRAIL almost exclusively targets malignant plasma cells, but not normal BMMCs from patients with MM.
TRAIL induces cell death of freshly isolated MM patient cells.
(A) Representative 3-dimensional cell cycle profile analysis, by PI staining, of freshly isolated CD38+/CD45RA−malignant cells of a patient with plasma cell leukemia. (The longitudinal axis corresponds to intensity of PI staining and the vertical axis to number of events.) A 24-hour incubation with TRAIL induced significant cell death documented by the shift of cells to the sub-G1 region (indicated by the dark shaded portions of the cell cycle profiles). (B,C) Effect of TRAIL on freshly isolated MM patient BMMCs. Dual-color flow cytometry for CD38-FITC and Apo2.7-PE indicates that late apoptotic (Apo2.7-PE+) cells are present only in the population of CD38+ BMMCs, which contains MM plasma cells. Quadrants were set based on negative controls stained with MsIgG1-FITC and MsIgG1-PE (X-axis, Apo2.7 relative expression; Y-axis, CD38 relative expression).
TRAIL induces cell death of freshly isolated MM patient cells.
(A) Representative 3-dimensional cell cycle profile analysis, by PI staining, of freshly isolated CD38+/CD45RA−malignant cells of a patient with plasma cell leukemia. (The longitudinal axis corresponds to intensity of PI staining and the vertical axis to number of events.) A 24-hour incubation with TRAIL induced significant cell death documented by the shift of cells to the sub-G1 region (indicated by the dark shaded portions of the cell cycle profiles). (B,C) Effect of TRAIL on freshly isolated MM patient BMMCs. Dual-color flow cytometry for CD38-FITC and Apo2.7-PE indicates that late apoptotic (Apo2.7-PE+) cells are present only in the population of CD38+ BMMCs, which contains MM plasma cells. Quadrants were set based on negative controls stained with MsIgG1-FITC and MsIgG1-PE (X-axis, Apo2.7 relative expression; Y-axis, CD38 relative expression).
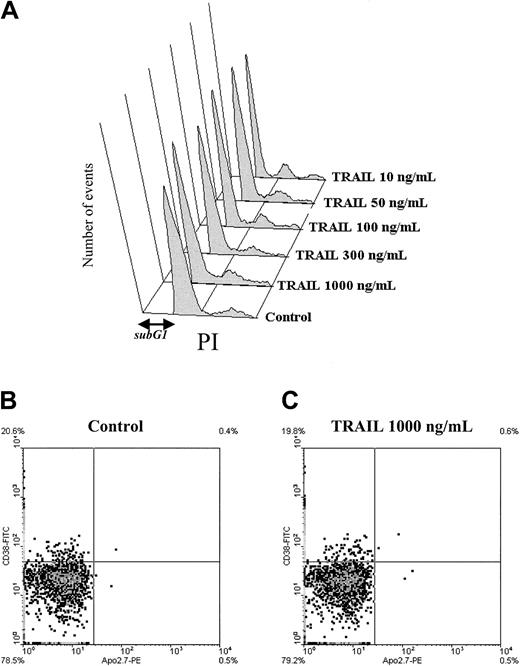
Effect of TRAIL on normal PBMCs or BMMCs.
PBMCs and BMMCs of healthy donors were treated with TRAIL (at concentrations up to 1000 ng/mL) for 24 hours. A dose-response analysis (by PI staining) of the normal B cells (A) indicates no shift of cells in the sub-G1 region, consistent with lack of TRAIL-induced cell death at concentrations up to 1000 ng/mL. Panels B and C demonstrate that healthy donor's BMMCs are resistant to even 1000 ng/mL TRAIL. Dual-color flow cytometry, for CD38+-FITC and Apo2.7-PE revealed that apoptotic cells (Apo2.7-PE+) are not detected in either the CD38+ or CD38−populations of BMMCs. (Quadrants were set based on negative controls stained with MsIgG1-FITC and MsIgG1-PE.)
Effect of TRAIL on normal PBMCs or BMMCs.
PBMCs and BMMCs of healthy donors were treated with TRAIL (at concentrations up to 1000 ng/mL) for 24 hours. A dose-response analysis (by PI staining) of the normal B cells (A) indicates no shift of cells in the sub-G1 region, consistent with lack of TRAIL-induced cell death at concentrations up to 1000 ng/mL. Panels B and C demonstrate that healthy donor's BMMCs are resistant to even 1000 ng/mL TRAIL. Dual-color flow cytometry, for CD38+-FITC and Apo2.7-PE revealed that apoptotic cells (Apo2.7-PE+) are not detected in either the CD38+ or CD38−populations of BMMCs. (Quadrants were set based on negative controls stained with MsIgG1-FITC and MsIgG1-PE.)
Effect of TRAIL/Apo2L on healthy donor B cells and BMMCs
We next investigated whether the proapoptotic effect of TRAIL/Apo2L is selective against MM cells or whether it may also affect normal hematopoietic cells. Peripheral blood normal B cells from 7 healthy donors, as well as BMMCs from another 3 donors, were incubated with LZ-TRAIL at concentrations (10-1000 ng/mL) that induce MM cell apoptosis. The percentage of dead/apoptotic (sub-G1region of the cell cycle profile) normal B cells after exposure to TRAIL/Apo2L did not differ from untreated controls (Figure 4A). MTT assays of normal donor PBMCs revealed no TRAIL-induced reduction in survival, whereas Apo2.7 staining of normal donor PBMCs with counterstaining for CD19, CD3, or CD14 revealed no reduction in the survival of B lymphocytes, T lymphocytes, and monocytes/macrophages, respectively (data not shown). Normal donor BMMCs were also treated with TRAIL (100-1000 ng/mL) for 18 hours and then analyzed by dual-color flow cytometry for CD38-FITC/Apo2.7-PE (to detect late apoptotic Apo2.7+ cells). TRAIL induced apoptosis of neither CD38+ or CD38− cells, suggesting that it does not affect the survival of normal plasma cells or other populations of normal BMMCs (Figure 4B,C).
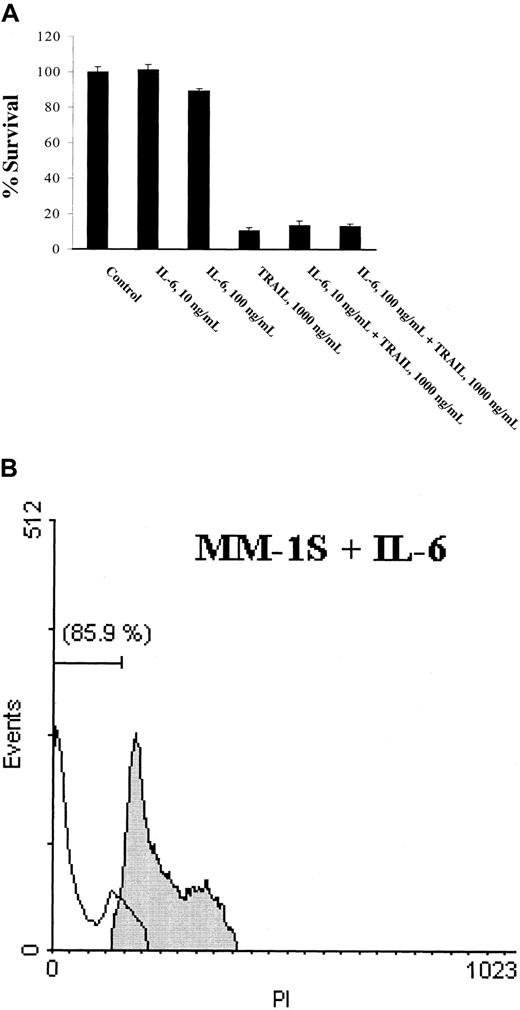
IL-6 does not confer resistance to TRAIL-induced apoptosis
Interleukin 6 is a potent growth and survival factor for MM cells and is known to inhibit apoptosis induced by Dex25 and TRAIL-related FasL.26,28 We therefore examined whether IL-6 blocks TRAIL-induced apoptosis of MM cells. MM-1S, S6B45, and RPMI-8226/S cells were cultured with TRAIL (0.001-1000 ng/mL) in the presence or absence of IL-6 (10-100 ng/mL). IL-6 did not abrogate TRAIL-induced apoptosis of S6B45, RPMI-8226/S cells, or MM-1S cells (Figure 5), even at IL-6 concentrations 2 logs higher than those shown to inhibit apoptosis in these MM cells. Moreover, TRAIL induced apoptosis of S6B45 cells, which constitutively produce IL-6 in picogram concentrations (< 10 pg/mL).29These findings indicate that IL-6 is not a pathophysiologically significant modulator of TRAIL-induced apoptosis, in contrast to its documented role in protecting MM cells against Dex-induced apoptosis.26 28
Lack of IL-6 rescue on TRAIL-induced MM cell death.
MTT colorimetric assay (A) and PI staining (B), performed in MM-1S cells cultured with TRAIL (1000 ng/mL) in the presence or absence of IL-6 (100 ng/mL), document that IL-6 does not abrogate TRAIL-induced cell death. In panel B, the shaded cell cycle profile corresponds to MM-1S cells cultured with IL-6. The unshaded profile, corresponding to cells treated with TRAIL in the presence of IL-6, is identical to the one of MM-1S cells treated with TRAIL alone (data not shown).
Lack of IL-6 rescue on TRAIL-induced MM cell death.
MTT colorimetric assay (A) and PI staining (B), performed in MM-1S cells cultured with TRAIL (1000 ng/mL) in the presence or absence of IL-6 (100 ng/mL), document that IL-6 does not abrogate TRAIL-induced cell death. In panel B, the shaded cell cycle profile corresponds to MM-1S cells cultured with IL-6. The unshaded profile, corresponding to cells treated with TRAIL in the presence of IL-6, is identical to the one of MM-1S cells treated with TRAIL alone (data not shown).
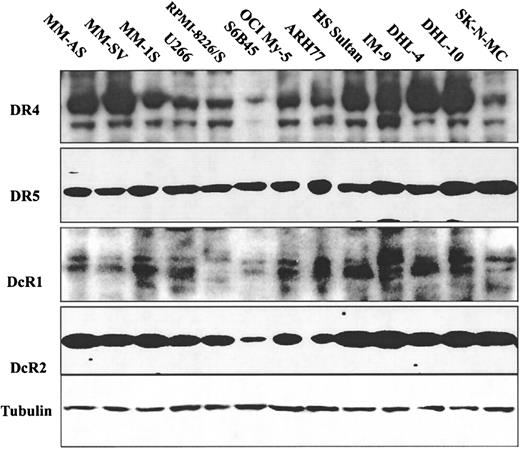
TRAIL receptor expression in MM cell lines
We investigated whether differences in MM cell sensitivity to TRAIL correlate with variations in expression of TRAIL receptors by performing immunoblotting of MM cell lysates (Figure6) and flow cytometric analysis to detect surface expression of receptors (Figure7). Immunoblotting analysis of 10 MM cell lines (MM-AS, MM-SV, MM-1S, U266, RPMI-8226/S, S6B45, OCI My-5, ARH-77, HS Sultan, and IM9) demonstrated expression of all 4 receptors in all MM lines (including high levels of DR5 and DcR2 in all lines and variable DR4 and DcR1 expression), regardless of their TRAIL sensitivity status. Some TRAIL-resistant lines (eg, ARH-77, HS Sultan, and IM-9) appeared to have high expression of DcR1 by immunoblotting. However, several TRAIL-sensitive lines (eg, MM-1S, U266, and OCI-My5) also had high levels of DcR1 expression. Therefore, the DcR1 status cannot serve to predict TRAIL sensitivity or resistance of MM cells. Furthermore, whereas surface expression (by flow cytometry) was also positive in all lines for DR5 and DcR2, it was negative for DcR1 (for all 3 different antihuman DcR1 antibodies tested), excluding any correlation of these parameters with TRAIL sensitivity. Although 2 TRAIL-resistant lines (ARH-77 and IM-9) had absent or dimly positive surface DR4 expression (despite high levels of expression in Western blots), other TRAIL-resistant cells (eg, HS Sultan; Figure 7) had strong surface expression of DR4 receptors, whereas no correlation was noted between lack of surface DR4 expression and TRAIL resistance in our panel of MM cell lines (McNemar paired χ2 test,P = .25). Although some TRAIL-sensitive MM cells (eg, RPMI-8226/S) had higher levels of surface DR5 expression than the TRAIL-resistant ARH-77 or IM-9 cells, our panel of cell lines included both strongly surface DR5+ TRAIL-resistant cells (eg, HS Sultan cells) and weakly DR5+ TRAIL-sensitive cells. This indicates lack of correlation between the levels of DR5 expression with TRAIL sensitivity. Therefore, the status of signaling or “decoy” TRAIL receptors, assessed using either immunoblotting analysis or flow cytometry, cannot serve to reliably predict the TRAIL sensitivity (or resistance) of MM cells.
Western blot analysis of TRAIL receptor expression in MM and NHL B-cell lines.
Western blot analysis for DR4 and DR5 death-signaling and DcR1 and DcR2 “decoy” TRAIL receptors was performed in lysates derived from 10 MM cell lines (MM-AS, MM-SV, MM-1S, U266, RPMI-8226/S, S6B45, OCI My-5, ARH-77, HS Sultan, and IM-9) and 2 NHL B-cell lines (DHL-4 and DHL-10). SK-N-MC Ewing sarcoma cells served as a positive control. Tubulin detection was used to confirm equal protein loading.
Western blot analysis of TRAIL receptor expression in MM and NHL B-cell lines.
Western blot analysis for DR4 and DR5 death-signaling and DcR1 and DcR2 “decoy” TRAIL receptors was performed in lysates derived from 10 MM cell lines (MM-AS, MM-SV, MM-1S, U266, RPMI-8226/S, S6B45, OCI My-5, ARH-77, HS Sultan, and IM-9) and 2 NHL B-cell lines (DHL-4 and DHL-10). SK-N-MC Ewing sarcoma cells served as a positive control. Tubulin detection was used to confirm equal protein loading.
Flow cytometric analysis for TRAIL receptor expression in MM cell lines.
Flow cytometric analyses for surface TRAIL receptors' expression in 5 representative cell lines (the TRAIL-sensitive MM-1S and RPMI-8226/S cells and the TRAIL-resistant ARH-7, IM-9, and HS Sultan cells) indicates that the status of neither the TRAIL-signaling DR4 and DR5 nor the “decoy” DcR1 and DcR2 receptors can serve to predict the TRAIL sensitivity of MM cells. The depicted graphs were obtained after staining with antihuman DR4, DR5, DcR1, and DcR2 mAbs (Genentech) and confirmed by use of the other anti-TRAIL receptor antibodies described in “Materials and methods.” Shaded curves depict isotype control staining, and unshaded peaks correspond to staining with the respective TRAIL receptor antibodies.
Flow cytometric analysis for TRAIL receptor expression in MM cell lines.
Flow cytometric analyses for surface TRAIL receptors' expression in 5 representative cell lines (the TRAIL-sensitive MM-1S and RPMI-8226/S cells and the TRAIL-resistant ARH-7, IM-9, and HS Sultan cells) indicates that the status of neither the TRAIL-signaling DR4 and DR5 nor the “decoy” DcR1 and DcR2 receptors can serve to predict the TRAIL sensitivity of MM cells. The depicted graphs were obtained after staining with antihuman DR4, DR5, DcR1, and DcR2 mAbs (Genentech) and confirmed by use of the other anti-TRAIL receptor antibodies described in “Materials and methods.” Shaded curves depict isotype control staining, and unshaded peaks correspond to staining with the respective TRAIL receptor antibodies.
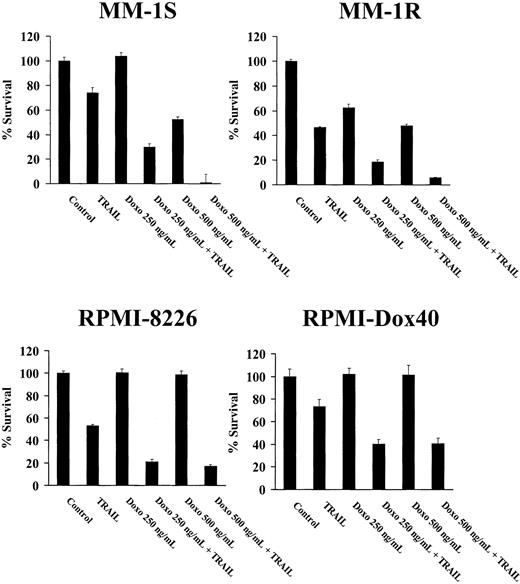
Dox enhances the in vitro proapoptotic effect of TRAIL on MM cells
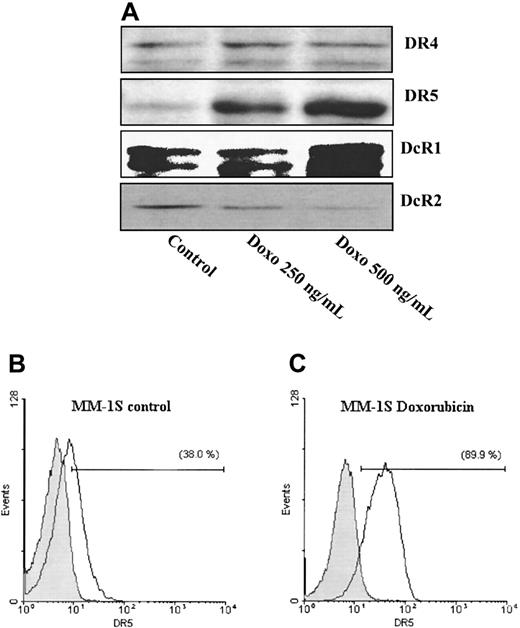
We next determined whether the cytotoxic agent Dox enhanced the proapoptotic effect of TRAIL in TRAIL-sensitive and TRAIL-resistant MM cells, because Dox has been reported to enhance the apoptotic activity of TRAIL and up-regulate the DR5 receptor in MCF-7 breast cancer cells.30 MM-1S, MM-1R, RPMI-8226/S, and RPMI-8226/Dox40 cells were pretreated with Dox (250 or 500 ng/mL) for 4 hours, and then exposed to LZ-TRAIL (50 ng/mL) for 18 hours. MTT assays (Figure8) revealed that Dox significantly enhanced the proapoptotic effect of TRAIL in these cells, reducing their survival to levels lower than expected if Dox and TRAIL had an additive interaction (P < .01, for each cell line). Western blot analysis and flow cytometry revealed that a 24-hour exposure of MM-1S cells to Dox (250 and 500 ng/mL) induced a significant dose-dependent up-regulation in the expression of DR5 and to a lesser extent of DcR1, but not of DR4 TRAIL receptor, whereas a modest decrease of DcR2 expression was also noted (Figure9).
Doxorubicin sensitizes Dex-sensitive (MM-1S) and Dex-resistant (MM-1R) cells, as well as Dox-sensitive (RPMI-8226/S) and Dox-resistant (Dox40) cells, to TRAIL.
MTT colorimetric assays demonstrate that pretreatment with Dox, as described in “Materials and methods,” enhances the TRAIL sensitivity of MM cells, including MM cells resistant to apoptosis induced by Dex (MM-1R) or Dox (Dox40).
Doxorubicin sensitizes Dex-sensitive (MM-1S) and Dex-resistant (MM-1R) cells, as well as Dox-sensitive (RPMI-8226/S) and Dox-resistant (Dox40) cells, to TRAIL.
MTT colorimetric assays demonstrate that pretreatment with Dox, as described in “Materials and methods,” enhances the TRAIL sensitivity of MM cells, including MM cells resistant to apoptosis induced by Dex (MM-1R) or Dox (Dox40).
Doxorubicin up-regulates DR5 expression of MM-1S cells.
Immunoblotting analysis (A) of Dox-treated (250 or 500 ng/mL) MM-1S cells reveals dose-dependent up-regulation of DR5 expression, confirmed by flow cytometry (B). Dox also induces a small increase in DcR1 and decrease in DcR2 expression, by immunoblotting analysis (A).
Doxorubicin up-regulates DR5 expression of MM-1S cells.
Immunoblotting analysis (A) of Dox-treated (250 or 500 ng/mL) MM-1S cells reveals dose-dependent up-regulation of DR5 expression, confirmed by flow cytometry (B). Dox also induces a small increase in DcR1 and decrease in DcR2 expression, by immunoblotting analysis (A).
NF-κB inhibition or proteasome inhibition modulate the effect of TRAIL on MM cells
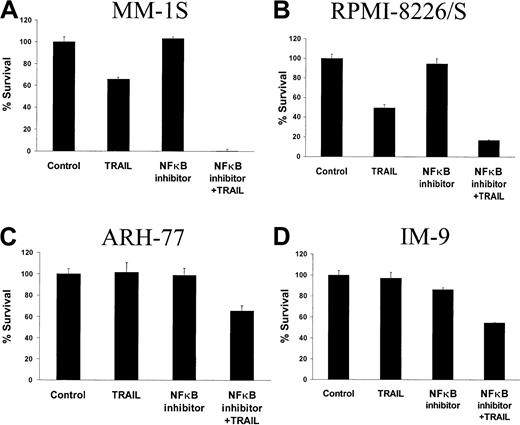
Because NF-κB may play a role in the regulation of MM cell survival,31 we investigated whether inhibition of NF-κB transcriptional activity could modulate the response of MM cells to TRAIL. MM-1S and RPMI-8226/S cells, as well as the TRAIL-resistant ARH-77 and IM-9 cells, were pretreated for 4 hours with a nontoxic concentration (30 ng/mL) of the cell-permeable peptide SN50 or with its mutant control peptide SN50M. SN50 binds to the nuclear localization sequence of NF-κB and blocks its nuclear translocation, thus inhibiting its transcriptional activity.32 As seen in Figure 10, SN50 pretreatment enhanced the sensitivity of MM-1S cells (< 5% survival) to TRAIL (50 ng/mL), in contrast to pretreatment of MM-1S with the mutant control peptide SN50M (which led to > 50% survival of MM-1S cells). Importantly, SN50 also reversed the TRAIL resistance of ARH-77 and IM-9 cells (Figure 10C,D); SN-50 pretreatment and TRAIL (50 ng/mL) led to less than 60% survival of these cells, whereas these cells were resistant even to 1000 ng/mL TRAIL without SN50 pretreatment. We also determined whether the proteasome inhibitor PS-341, which is known to inhibit the transcriptional activity of NF-κB by blocking the degradation of the IκB inhibitory protein,33 sensitized MM cells to TRAIL-induced apoptosis. MM-1S cells were preincubated with 0.1 μM PS-341 for 3 hours and then exposed to TRAIL (50 or 100 ng/mL) for 18 hours. These studies demonstrated that PS-341 preincubation augmented the sensitivity of MM-1S cells to TRAIL (Figure11).
Inhibition of NF-κB augments TRAIL sensitivity or reverses TRAIL resistance of MM cells.
MTT colorimetric assays indicate that pretreatment with the NF-κB inhibitory peptide SN50 enhances TRAIL (50 ng/mL)-induced cell death in TRAIL-sensitive MM-1S and RPMI-8226/S cells (A,B) and overcomes the TRAIL resistance of ARH-77 and IM-9 cells (C and D, respectively).
Inhibition of NF-κB augments TRAIL sensitivity or reverses TRAIL resistance of MM cells.
MTT colorimetric assays indicate that pretreatment with the NF-κB inhibitory peptide SN50 enhances TRAIL (50 ng/mL)-induced cell death in TRAIL-sensitive MM-1S and RPMI-8226/S cells (A,B) and overcomes the TRAIL resistance of ARH-77 and IM-9 cells (C and D, respectively).
The proteasome inhibitor PS-341 enhances the TRAIL sensitivity of MM cells.
Pretreatment of MM-1S cells with the proteasome inhibitor PS-341 (0.1 μM) enhances their sensitivity to TRAIL, as evidenced by MTT colorimetric assay.
The proteasome inhibitor PS-341 enhances the TRAIL sensitivity of MM cells.
Pretreatment of MM-1S cells with the proteasome inhibitor PS-341 (0.1 μM) enhances their sensitivity to TRAIL, as evidenced by MTT colorimetric assay.
Normal B cells are not sensitized to TRAIL by either Dox, PS-341, or NF-κB inhibition
We next investigated whether pretreatment of TRAIL-resistant healthy donor B cells with Dox, PS-341, or SN50 similarly sensitized these cells to TRAIL. Pretreatment with either Dox or agents that inhibit NF-κB did not sensitize normal B cells or PBMCs (data not shown) to TRAIL. Importantly, in the context of these pretreatments, B cells remained refractory to TRAIL at doses up to 300 ng/mL, in contrast to MM cells, which were sensitized by these pretreatments at doses of TRAIL as low as 50 ng/mL.
Effect of TRAIL on established human plasmacytomas in xenografted nu/xid/bg mice
We next examined whether TRAIL was active against MM in vivo by treating established human plasmacytomas in nu/xid/bg mice with either TRAIL (n = 8) or PBS (n = 8). Mean plasmacytoma volumes were not significantly different at initiation of therapy on day 1 (Figure12, P = .328 by Mann-Whitney test). Following TRAIL administration, the volume of established xenografts did not show a significant increase from baseline (P = .851, Kruskal-Wallis nonparametric one-way analysis of variance), whereas PBS-treated mice showed increasing mean tumor volumes, which became significantly greater than baseline beyond day 8 (P < .05 by Kruskall-Wallis test). Following 11 days of TRAIL administration, the mean tumor volumes for TRAIL-treated mice were significantly less than the mean tumor volumes for mice treated with PBS (P = .009 by Mann-Whitney test). Moreover, complete plasmacytoma eradication was observed in 1 of 8 TRAIL-treated animals on day 11. Significantly lower mean tumor volumes for TRAIL-treated versus PBS-treated mice were again observed on day 14 (P = .032) and on day 18 (P = .046). However, on day 18 (4 days following termination of TRAIL administration), the mean plasmacytoma volume in TRAIL-treated animals increased compared to the baseline mean tumor volume for these animals (P = .006), yet remained significantly less than that in PBS-treated mice. On day 18, the PBS-treated animals were moribund and all animals from both cohorts were euthanized in accordance with NIH and our institutional guidelines. To determine if xenografted plasmacytoma cells remained sensitive to TRAIL despite the apparent increase in tumor volume following discontinuation of TRAIL therapy, tumors from 2 animals were excised, mechanically dissociated, and cultured with LZ-human TRAIL (1000 ng/mL) for 24 hours. These studies demonstrated that the excised human plasmacytomas from 2 TRAIL-treated mice underwent apoptosis following culture with TRAIL, as assessed by PI and annexin V staining. Overall, mice treated with TRAIL tolerated therapy well, with continued display of weight gain throughout therapy (data not shown). One TRAIL-treated mouse died on day 11 of toxicity not related to TRAIL (intestinal puncture), although this mouse also exhibited a tumor response to TRAIL therapy.
Effect of human recombinant LZ-TRAIL on the growth of established human plasmacytoma xenografts in nu/xid/bg mice.
Nu/xid/bg mice were injected subcutaneously with human S6B45 MM cells. On establishment of palpable xenografts, the mice (8/cohort) received either PBS or recombinant human LZ-TRAIL (500 μg intraperitoneally daily for 14 days). TRAIL was well tolerated by the mice and suppressed the growth of the established human plasmacytomas, in contrast to the significant increase in the tumor burden generated in PBS-treated control mice.
Effect of human recombinant LZ-TRAIL on the growth of established human plasmacytoma xenografts in nu/xid/bg mice.
Nu/xid/bg mice were injected subcutaneously with human S6B45 MM cells. On establishment of palpable xenografts, the mice (8/cohort) received either PBS or recombinant human LZ-TRAIL (500 μg intraperitoneally daily for 14 days). TRAIL was well tolerated by the mice and suppressed the growth of the established human plasmacytomas, in contrast to the significant increase in the tumor burden generated in PBS-treated control mice.
Discussion
In a preliminary report, we demonstrated that TRAIL/Apo2L induced apoptosis of most MM cell lines and MM patient tumor cells,17 a finding subsequently confirmed by other groups.34-37 In this report, we demonstrate that most MM cell lines, including those that are resistant to Dex and chemotherapeutic agents, are sensitive to TRAIL/Apo2L. Moreover, TRAIL induced apoptosis of MM cells from 5 of 5 patients and did not affect non-MM BMMCs, normal B cells, and hematopoietic progenitor cells. Importantly, IL-6, a major growth and survival factor of MM cells, blocks apoptosis induced by a variety of proapoptotic agents, including Dex25 and FasL,26 38 but does not abrogate TRAIL-induced apoptosis. The differential survival effect of IL-6 in protecting from FasL-induced, but not TRAIL-induced, apoptosis may reflect differences in downstream signaling of these tumoricidal TNF-related cytokines.
Detailed analyses of our panel of MM cell lines for TRAIL receptor expression by both Western blot and flow cytometry were undertaken to discern differences that might confer TRAIL sensitivity versus resistance. The death signaling receptors DR4 and DR5 were expressed in all MM cell lines, evidenced by both Western blot and flow cytometric analyses, except for the TRAIL-resistant ARH-77 and IM-9 cell lines, which lack surface DR4 (despite strong expression by immunoblotting analysis). However, the level of surface expression of neither DR4 nor DR5 correlates with TRAIL-resistance in our panel of MM lines; some TRAIL-resistant cells (eg, HS Sultan) had very strong expression of both receptors, in comparison to some TRAIL-sensitive cells (eg, MM-1S). Mutations at the death domain of the DR5 receptor have been described in other neoplasias39,40 and could also account for TRAIL resistance in cells that lack surface DR4 expression, such as ARH-77 and IM-9 cells. However, we were able to sensitize these cells to TRAIL by NF-κB inhibition without increasing the levels of DR4 or DR5 (N. Mitsiades, manuscript in preparation), confirming that the baseline levels of DR5 expression in these MM cells are sufficient for induction of apoptosis within the context of appropriate sensitization stimuli. DcR1 and DcR2 expression has been suggested as another potential mechanism for protection of cells against TRAIL; therefore, we also investigated whether their expression correlated with TRAIL resistance in MM cells. DcR2 was uniformly expressed on all MM cells (both TRAIL sensitive and resistant) by both Western blot and flow cytometric analyses. In contrast, DcR1 was variably expressed on MM cell lines by Western blot analysis, but absent on the cell surface by flow cytometry performed with a panel of 3 anti-DcR1 antibodies. Therefore, TRAIL receptor status alone cannot serve as a reliable predictor of TRAIL sensitivity in MM cells, with the exception of lack of both DR4 and DR5 expression. This latter TRAIL receptor pattern was not observed in MM cells, although we have documented it in other neoplasias.15 This lack of correlation of TRAIL decoy receptor expression with TRAIL sensitivity in MM cells observed in our study is consistent with previous reports in various neoplasias6,16,41-44 and further suggests that the molecular mechanisms of TRAIL sensitivity or resistance may be highly complex. In this regard, the 5 TRAIL-resistant MM cell lines (ARH-77, IM-9, HS Sultan, MM-AS, and MM-SV cells) in our study may represent earlier plasmacytes or late-stage B cells, as evidenced by their expression of cell surface CD20, which is lost at late stages of plasmacytic differentiation.45 These findings, along with our data that normal B cells are resistant to TRAIL/Apo2L, suggest that TRAIL sensitivity may be acquired with late plasmacytic differentiation. Changes in the pattern of sensitivity of B-lineage cells to TRAIL during differentiation are currently under evaluation in our laboratory.
The potent and selective proapoptotic effect of TRAIL/Apo2L against MM patient cells and most MM cell lines in vitro prompted us to evaluate its in vivo anti-MM effect in nu/bg/xid mice bearing established human plasmacytoma xenografts. Importantly, TRAIL inhibited the growth of human plasmacytomas and induced complete tumor eradication in 1 of 8 TRAIL-treated animals at the dose regimen (ie, 500 μg daily for 14 days) evaluated. Following discontinuation of TRAIL, increases in the mean tumor volumes were observed in TRAIL-treated mice. However, it is unlikely that selection of TRAIL-resistant MM cells contributed to these findings because plasmacytoma cells taken from 2 mice remained sensitive to TRAIL. It is possible that the use of higher TRAIL/Apo2L doses may be more effective in further shrinking or eradicating established plasmacytomas; studies evaluating higher doses of TRAIL/Apo2L, which have been successfully used in in vivo models of other neoplasias,4,7 are currently under way in our MM murine model. Importantly, TRAIL/Apo2L appeared to be well tolerated by the mice. The observed responses and lack of toxicity of LZ-TRAIL in this human plasmacytoma model are not attributable solely to differences in cross-species activity of human LZ-TRAIL, because both human and murine TRAIL are equipotent against murine cell lines in vitro.4 However, recent reports of potential toxicity of the LZ-TRAIL to human hepatocytes46 and neuronal tissues47 suggest that other forms of TRAIL, without these adverse effects, may be preferable for future clinical use.
Concerns regarding emergence of TRAIL resistance, as well as potential TRAIL-related side effects in vivo, prompted us to investigate mechanisms to enhance the tumoricidal activity and therapeutic index of TRAIL/Apo2L-based therapies. We therefore examined whether Dox, which up-regulates the DR5 death signaling receptor48-50 and is commonly used to treat MM, could sensitize MM cells to TRAIL. We demonstrated that pretreatment of several MM cell lines with Dox, at clinically relevant concentrations, significantly enhanced the TRAIL sensitivity of MM cells. Specifically, Dox induced significant up-regulation of the DR5 receptor expression (and a much lesser increase in DcR1, as well as a small decrease in DcR2 expression) and, importantly, had a synergistic interaction with TRAIL/Apo2L in inducing apoptosis of MM-1S cells. This finding is consistent with previous reports in other malignancies.49-51 We showed that, within our panel of MM cell lines, the status of functional or “decoy” TRAIL receptors at baseline cannot per se explain why a particular cell line is TRAIL sensitive or resistant (possibly due to downstream intracellular modulators of apoptosis). However, this does not preclude the possibility that changes of surface expression of TRAIL receptor(s) in each particular cell line (eg, in the setting of Dox stimulation) may modulate its TRAIL sensitivity. Interestingly, the synergy of Dox with TRAIL was also documented against MM cells resistant to Dex- or Dox-induced apoptosis, suggesting that the molecular pathway(s) underlying this synergy are independent of classical mechanisms of drug resistance in MM cells. In particular, the Dox-induced sensitization of “Dox-resistant” MM cells to TRAIL/Apo2L suggests that Dox-induced apoptosis and sensitization to TRAIL/Apo2L constitute distinct biologic end points and are likely mediated by distinct mechanisms; therefore, intracellular Dox concentrations that cannot themselves induce apoptosis may be sufficient to sensitize MM cells to TRAIL/Apo2L. Ongoing efforts are delineating the mechanism underlying TRAIL/Apo2L sensitization and DR5 up-regulation by Dox.
We also investigated whether agents that inhibit NF-κB could also sensitize MM cells to TRAIL/Apo2L. NF-κB is a multifunctional transcription factor that serves as a nodal point for multiple converging signal transduction pathways,52 which include both antiapoptotic and proapoptotic stimuli. TRAIL/Apo2L binding to DR4 and DR5, as well as to decoy receptor DcR2, activates NF-κB53-56 by RIP-mediated activation of IκB kinase.57 NF-κB is an important constituent of cell survival pathways for MM31 and other cells,58and confers protection of tumor cells against various proapoptotic stimuli. Conversely, inhibition of NF-κB by transfection with superrepressor forms of IκB sensitized chemoresistant fibrosarcoma cells to TNF-α and the topoisomerase I inhibitor CPT-11.59 We therefore examined whether 2 agents that inhibit NF-κB activity (SN50 and PS-341) could sensitize MM cells to TRAIL/Apo2L-induced apoptosis. In several TRAIL-sensitive MM cells, pretreatment with SN50 markedly enhanced sensitivity to TRAIL. Moreover, pretreatment with SN50 reversed the TRAIL-resistant phenotype of ARH-77 and IM-9 MM cells. Pretreatment of MM-1S cells with PS-341, which also inhibits NF-κB activation, enhanced the sensitivity to TRAIL. These data suggest that NF-κB activity may be a major determinant of responsiveness to TRAIL/Apo2L in MM and an attractive target for therapeutic strategies to augment TRAIL/Apo2L efficacy or reverse TRAIL resistance in MM cells.
In anticipation of future clinical trials of TRAIL/Apo2L alone and in combination with TRAIL/Apo2L-sensitizing agents, we determined whether TRAIL-resistant normal hematopoietic cells are also sensitized to TRAIL/Apo2L by pretreatment with Dox or NF-κB inhibition. Importantly, pretreatement with Dox, SN50, or PS-341 (under the same experimental conditions that sensitized MM cells to TRAIL/Apo2L) did not sensitize normal peripheral blood B cells to TRAIL/Apo2L. These data suggest the potential utility of TRAIL-based combination therapies to selectively target MM cells.
In summary, TRAIL/Apo2L is a potent and selective inducer of apoptosis in drug-sensitive and drug-resistant MM cell lines, as well as in patient MM cells. TRAIL/Apo2L-induced apoptosis of MM cells is not abrogated by IL-6, a major growth and survival factor for MM cells. Factors other than TRAIL receptor status likely account for patterns of TRAIL sensitivity and resistance in MM cells and are currently being evaluated in our laboratory. TRAIL exhibited anti-MM activity in vivo in mice xenografted with human plasmacytomas. Lastly, Dox and agents inhibiting NF-κB sensitized MM cells, but not normal B cells, to TRAIL/Apo2L-induced apoptosis. These studies therefore provide a framework for clinical trials examining the use of single-agent and combined TRAIL/Apo2L-based therapies in MM.
Supported by the Laurie Strauss Leukemia Foundation (S.P.T. and N.M.), the International Myeloma Foundation (S.P.T.), the American Society of Clinical Oncology Young Investigator Award (S.P.T.), the Multiple Myeloma Research Foundation (S.P.T.), and the Doris Duke Distinguished Clinical Research Scientist Award (K.C.A.).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Kenneth C. Anderson, Dept of Adult Oncology, Dana Farber Cancer Institute, 44 Binney St, Boston, MA 02115; e-mail:kenneth_anderson@dfci.harvard.edu.




This feature is available to Subscribers Only
Sign In or Create an Account Close Modal