Abstract
Human mesenchymal stem/progenitor cells (MSCs) have been identified in adult bone marrow, but little is known about their presence during fetal life. MSCs were isolated and characterized in first-trimester fetal blood, liver, and bone marrow. When 106 fetal blood nucleated cells (median gestational age, 10+2 weeks [10 weeks, 2 days]) were cultured in 10% fetal bovine serum, the mean number (± SEM) of adherent fibroblastlike colonies was 8.2 ± 0.6/106 nucleated cells (69.6 ± 10/μL fetal blood). Frequency declined with advancing gestation. Fetal blood MSCs could be expanded for at least 20 passages with a mean cumulative population doubling of 50.3 ± 4.5. In their undifferentiated state, fetal blood MSCs were CD29+, CD44+, SH2+, SH3+, and SH4+; produced prolyl-4-hydroxylase, α-smooth muscle actin, fibronectin, laminin, and vimentin; and were CD45−, CD34−, CD14−, CD68−, vWF−, and HLA-DR−. Fetal blood MSCs cultured in adipogenic, osteogenic, or chondrogenic media differentiated, respectively, into adipocytes, osteocytes, and chondrocytes. Fetal blood MSCs supported the proliferation and differentiation of cord blood CD34+cells in long-term culture. MSCs were also detected in first-trimester fetal liver (11.3 ± 2.0/106 nucleated cells) and bone marrow (12.6 ± 3.6/106 nucleated cells). Their morphology, growth kinetics, and immunophenotype were comparable to those of fetal blood-derived MSCs and similarly differentiated along adipogenic, osteogenic, and chondrogenic lineages, even after sorting and expansion of a single mesenchymal cell. MSCs similar to those derived from adult bone marrow, fetal liver, and fetal bone marrow circulate in first-trimester human blood and may provide novel targets for in utero cellular and gene therapy.
Introduction
In addition to hematopoietic stem cells, it is now clear that adult human bone marrow contains a rare population of mesenchymal stem/progenitor cells (MSCs) (0.01% to 0.001%). Morphologically, MSCs in their undifferentiated state are spindle shaped and resemble fibroblasts. They can be extensively expanded in vitro and, when cultured under specific permissive conditions, retain their ability to differentiate into multiple lineages including bone, cartilage, tendon, muscle, nerve, and stromal cells.1-7
MSCs are of great therapeutic potential because of their ability to self-renew and differentiate into multiple tissues.8 Adult bone marrow-derived MSCs engraft in numerous organs and differentiate along tissue-specific lineages when transplanted into fetal sheep.9 They enhance engraftment of donor hematopoietic cells after cotransplantation in animal models,10-12 and they migrate into areas of muscle degeneration to undergo myogenic differentiation in immunodeficient mice.13 In humans, MSCs have been used to regenerate the marrow microenvironment after myeloablative therapy.14 Furthermore, Horwitz et al15 have shown that allogeneic bone marrow transplantation in children with osteogenesis imperfecta allowed engraftment of functional donor MSCs, resulting in increased bone marrow density.
Recent work has shown that mesenchymal progenitors are also present at low frequencies in adult peripheral blood16 and in term cord blood.17 To date little is known about their presence in early fetal life. MSCs are closely associated with hematopoietic stem cells in adult bone marrow, while first-trimester fetal blood contains significant numbers of hematopoietic progenitors18and SCID-repopulating cells,19 and fetal liver and bone marrow are well-known sites of active hematopoiesis during ontogeny.20 Our aim was to isolate and characterize MSCs early in gestation, which would promote understanding of the ontogeny of these cells and possibly open new avenues for in utero cellular and gene therapy. In this study we show that MSCs can be isolated from human first-trimester fetal blood, liver, and bone marrow, readily expanded, and induced to differentiate in vitro.
Materials and methods
Samples
Blood and fetal tissue collection for research purposes was approved by the Research Ethics Committees of Hammersmith Hospital and Queen Charlotte's Hospital. National guidelines (Polkinghorne) were complied with in relation to the use of fetal tissues for research. Pregnant women gave written consent for the clinical procedure and for the use of fetal blood or tissue for research purposes.
First-trimester blood samples (median gestational age, 10+2 weeks [10 weeks, 2 days]; range, 7+6 to 14+0 weeks; n = 34) were collected by cardiocentesis under ultrasound guidance under general anesthesia before clinically indicated termination of pregnancy using a siliconized 20-gauge, 15-cm needle (Cook, Herts, United Kingdom). Cytospun cells from blood samples of less than 11 weeks' gestation and blood films from samples of more than 11 weeks' gestation were stained with Leishman stain, and differential cell counts were performed. Second-trimester blood samples (median gestational age, 17+5; range, 14+5 to 25+4; n = 7) were collected by ultrasound-guided fetal blood sampling during clinically indicated termination of pregnancy from the cord or during clinically indicated fetal blood sampling from the umbilical vein for rapid karyotyping (results all euploid). Third-trimester blood samples (median gestational age, 39+1; range, 38+0 to 40+2; n = 5) were obtained from the umbilical cord at delivery from uncomplicated pregnancies.
Bone marrow samples were obtained from 4 fetuses (median gestational age, 13+5 weeks; range, 11+2 to 14+3). Single-cell suspensions of fetal bone marrow were prepared by flushing the bone marrow cells out of the humeri and femurs using a syringe and 22-gauge needle into Dulbecco modified Eagle medium (DMEM; Sigma-Aldrich, United Kingdom) supplemented with 10% fetal bovine serum (FBS) (Stem Cells Technology, Vancouver BC, Canada), 2 mM L-glutamine, 50 U/mL penicillin, and 50 mg/mL streptomycin (Gibco BRL, Life Technologies, Paisley, United Kingdom). Fetal liver samples were taken from 4 fetuses (median gestational age, 11+6 weeks; range, 10+0 to 14+3weeks). Single-cell suspensions were prepared by mincing the organ through a 70-μm nylon filter (Becton Dickinson, United Kingdom), and cells were resuspended as for the bone marrow samples.
Isolation and culture of fetal blood, liver, and bone marrow mesenchymal stem/progenitor cells
Unselected nucleated cells from fetal blood, liver, and bone marrow samples were diluted with 10% FBS in DMEM with 50 U/mL penicillin, 50 μg/mL streptomycin, and 2 mM L-glutamine and were plated into a well of a 6-well plate at a density of 100 000 cells/cm2 and incubated at 37°C in 5% CO2. After 72 hours, nonadherent cells were removed, and the medium was replaced. At 80% confluence, cells were harvested with 0.25% trypsin and 1 mM EDTA (Stem Cells Technology) for 5 minutes at 37°C and were replated in 75-cm2 flasks.
To expand the cells through successive passages, they were plated at 104 cells/cm2, grown to near confluence, and harvested with the same protocol. Growth curves were assessed by counting the number of adherent cells daily for 16 days, and the number of population doublings was determined by counting the number of adherent cells at the start and end of each passage. To isolate individual colonies, nucleated cells were plated in a 100-mm dish at a density of 12 000/cm2 and were collected by cloning cylinders (Sigma-Aldrich) and expanded. Cultured fetal MSCs were recloned by single-cell sorting using FACS Vantage (Becton Dickinson).
Immunocytochemistry of cultured fetal mesenchymal stem/progenitor cells
Monolayer and single colony-derived adherent cells (at the second and tenth passages in culture) from first-trimester fetal blood (n = 10), liver (n = 8), and bone marrow (n = 8) were analyzed by immunocytochemistry. Cytospin preparations and growing cells in double-chamber slides (Nunc) were fixed in equal volumes of methanol and acetone for 1 minute at room temperature, washed in TBST (Tris-buffered saline containing Tween; Dako, Bucks, United Kingdom), incubated with 3% hydrogen-peroxide (H2O2; Sigma-Aldrich), and blocked with 10% normal goat or rabbit serum at room temperature. Washed slides were incubated with the following primary antibodies: mouse anti–human macrophage, CD68 mAb (clone PG-M1; Dako), peroxidase-conjugated rabbit anti–human von Willebrand factor polyclonal Ab (Dako), mouse anti–human prolyl-4-hydroxylase mAb (clone 5B5; Dako), rabbit anti–human myoglobin mAb (clone A0324; Dako), mouse anti–α-smooth muscle actin mAb (clone 1A4; Sigma-Aldrich), mouse anti–human VCAM-1/vascular cell adhesion molecule-1 mAb (CD106; clone BB1G-V1; R&D Systems Europe), mouse anti–human fibronectin mAb (clone IST-4; Sigma-Aldrich), mouse anti–collagen type 1 mAb (clone COL-1; Sigma-Aldrich), mouse antivimentin mAb (clone V9; Sigma-Aldrich), and mouse antilaminin (clone LAM-89; Sigma-Aldrich) at 1: 50 dilution with Dako antibody diluent (Dako) for 30 minutes at room temperature. Antimouse or antirabbit peroxidase–conjugated immunoglobulin G antibodies (Sigma-Aldrich) were used as secondary antibodies at 1:100 dilution, and 3,3′-diaminobenzidine in chromogen solution (Dako) was applied to the slides, which were counterstained with 0.1% Mayer hematoxylin solution (Sigma-Aldrich).
FACS analysis of cultured fetal mesenchymal stem/progenitor cells
Monolayer and single colony-derived adherent cells (at the second and tenth passages in culture) from first-trimester fetal blood (n = 10), liver (n = 8), and bone marrow (n = 8) were trypsinized and stained with anti-CD34–fluorescein isothiocyanate (FITC), CD45-FITC, HLA-DR–phycoerythrin (PE; Becton Dickinson), CD14-FITC, CD105 (endoglin)-PE, CD44 (H-CAM)–FITC CD29 (integrin β1 chain)–PE, CD31 (PECAM-1)–FITC (Serotec, Oxford, United Kingdom), SH2, SH3, and SH4 mAbs (Osiris Therapeutics, Baltimore, MD) and were analyzed by FACScalibur flow cytometry (Becton Dickinson).
Coculture of fetal blood mesenchymal stem/progenitor cells and hematopoietic cells
After irradiation (8000 cGy), 2.0 × 105monolayer-derived adherent cells from first-trimester fetal blood (n = 3) were seeded in 12-well plates (Nunc). After 24 hours, 5 × 104 cord blood CD34+ cells, isolated with anti-CD34 antibodies (QBEND/10 mouse immunoglobulin G; Miltenyi Biotec) conjugated with microbeads and eluted through MiniMACS columns, were resuspended in long-term culture medium (Myelocult; Stem Cell Technologies), including 10−6 M hydrocortisone (Stem Cell Technologies), and were seeded over the adherent cells in the absence of exogenous growth factors. The fetal stroma–CD34+ cell cocultures were cultured at 37°C with 5% CO2 for 6 and 8 weeks. At weekly intervals, nonadherent cells in the collected half-volume of the culture medium were assayed for colony-forming cells by colony assays in standard methylcellulose culture (Methocult; Stem Cell Technologies). Control experiments were also performed by culturing cord blood CD34+ cells either in the absence of a stromal layer and growth factors or over a murine stromal cell line (M210-B421; kindly donated by Dr C. Eaves, Terry Fox Laboratories, Vancouver, BC, Canada).
Adipogenic, osteogenic, and chondrogenic differentiation
The differentiation ability of MSCs was assessed in single colonies (at the second and tenth passages) collected by cloning cylinders from primary cultures of first-trimester fetal blood (n = 6), liver (n = 4), and bone marrow (n = 4) and in colonies derived from single cells sorted from expanded MSCs at the 2nd passage from first-trimester fetal blood (n = 4), liver (n = 4), and bone marrow (n = 4).
Adipogenic differentiation was assessed by incubation with DMEM with 10% FBS supplemented with 0.5 μM hydrocortisone, 0.5 μM isobutyl methylxanthine, and 60 μM indomethacin (Sigma-Aldrich) for 2 weeks as previously described.22 Cells were stained with fresh Oil-red-O solution (Sigma-Aldrich). The percentage of adipocytes was assayed by counting 50 to 100 cells in multiple fields.
Osteogenic differentiation was assessed by incubating the cells with DMEM with 10% FBS supplemented with 10−8 M dexamethasone, 0.2 mM ascorbic acid, and 10 mM β-glycerol phosphate (Sigma-Aldrich) for 2 weeks as previously described.22 To assess mineralization, cultures were stained with silver nitrate (Sigma-Aldrich) and scored for the area of mineralization as a percentage of the total area of the confluent cultures.
Serum-free chondrogenic medium containing DMEM supplemented with 10 ng/mL transforming growth factor-β3 (R&D Systems), 100 nM dexamethasone, 50 μg/mL ascorbic acid, 100 μg/mL sodium pyruvate, 40 μg/mL proline (Sigma-Aldrich), and ITS-plus at the final concentrations (6.25 μg/mL bovine insulin, 6.25 μg/mL transferrin, 6.25 μg/mL selenious acid, 5.33 μg/mL linoleic acid, and 1.25 μg/mL bovine serum albumin; Collaborative Biomedical Products) was used for chondrogenic differentiation as previously described.23 Antibodies specific for extracellular matrix were used to assess chondrogenic differentiation, including collagen types 1 and 2 (clone COL-1 and clone COL-2; Sigma-Aldrich). Anionic sulfated proteoglycans were detected by Safranin O staining and toluidine blue (Sigma-Aldrich) metachromasia.
Human foreskin fibroblasts (kindly provided by Dr F. Hills, Imperial College School of Medicine, London, United Kingdom) were cultured in DMEM containing 2 mM L-glutamine, 50 μg/mL streptomycin, 50 U/mL penicillin, and 10% FBS and were used as controls for all the differentiation experiments.
Statistics
Results are expressed as mean ± SEM, and statistical comparisons were performed using the Student ttest.
Results
Adherent, fibroblastlike cells in first-trimester fetal blood, liver, and bone marrow
The mean nucleated cell concentration was significantly higher in the first trimester (74.3 ± 9.6 × 109/L) than in the second (21.2 ± 4.5 × 109/L;P = .006) and third (19.2 ± 3.2 × 109/L;P = .0007) trimesters. In first trimester, fetal blood erythroblasts were the predominant cells, accounting for 96.3% ± 2.6% of the nucleated cells, whereas blasts and neutrophils accounted for 2.6% ± 1.4% and 0.7% ± 0.03%, respectively. We also consistently noted a small population of cells with large cytoplasm, pseudopodia, and nucleoli that were present in all the first-trimester fetal samples (0.4% ± 0.04%) (Figure1A). These cells, which produced prolyl-4-hydroxylase and fibronectin as detected by immunocytochemistry, were not seen in any of the second-trimester or term cord blood samples.
MSCs isolated and cultured in the first trimester.
A-D, fetal blood (9+2 weeks); E-H, fetal liver (10+2 weeks); and I-L, fetal bone marrow (11+2weeks. Cytospins of uncultured fetal blood (A), fetal liver (E), and fetal bone marrow (I) were stained with Leishman stain (× 1000 magnification). Three- and 8-day culture of a mesenchymal colony from fetal blood (B-C), fetal liver (F-G), and bone marrow (J-K) were stained with crystal violet (× 400 and × 100 magnification, respectively). Cytospins of a trypsinized MSC colony from fetal blood (D), fetal liver (H), and fetal bone marrow (L) were stained with Leishman stain (× 1000 magnification).
MSCs isolated and cultured in the first trimester.
A-D, fetal blood (9+2 weeks); E-H, fetal liver (10+2 weeks); and I-L, fetal bone marrow (11+2weeks. Cytospins of uncultured fetal blood (A), fetal liver (E), and fetal bone marrow (I) were stained with Leishman stain (× 1000 magnification). Three- and 8-day culture of a mesenchymal colony from fetal blood (B-C), fetal liver (F-G), and bone marrow (J-K) were stained with crystal violet (× 400 and × 100 magnification, respectively). Cytospins of a trypsinized MSC colony from fetal blood (D), fetal liver (H), and fetal bone marrow (L) were stained with Leishman stain (× 1000 magnification).
When fetal blood nucleated cells were cultured at a density of 105 cells/cm2 in simple medium containing only 10% FBS with no additional growth factors, all first-trimester samples rapidly formed a monolayer of adherent cells that covered the well surface and, when trypsinized (Figure 1D), appeared identical to those in Figure 1A. Nucleated cells plated at a lower density (12 000/cm2) formed individual colonies consisting of several dozen to a few hundred spindle-shaped fibroblastic cells by day 3. After 8 to 10 days of culture, large colonies (more than 1000 cells) and smaller colonies (fewer than 300 cells) were seen. Figure 1B-C shows the development of a first-trimester fetal blood adherent cell colony from the initial stage of proliferation on day 3 through consecutive stages of cell proliferation; more than 1000 cells became confluent after 8 days. The frequency of adherent colonies in first-trimester blood was 8.2 ± 0.6/106 nucleated cells (equivalent to 69.6 ± 10 colonies/100 μL fetal blood). Adherent fibroblastlike colonies could not be isolated from second- and third-trimester fetal blood samples cultured under identical conditions. However, when mononuclear cells from second- and third-trimester samples were enriched by single-density centrifugation and plated at a 25-fold higher concentration (2.5 × 106cells/mL) than were used for first-trimester blood, small numbers of colonies of adherent cells did develop. Colonies were smaller than those derived from first-trimester blood (fewer than 100 cells/colony) and were present at lower frequencies: 1.3/106 cells plated (second trimester, n = 1) and 0.35/106 cells (term cord blood, n = 4) versus first-trimester fetal blood (8.2/106cells).
We also investigated whether similar cells were present in fetal liver and bone marrow during the first trimester. When cell suspensions from first-trimester fetal liver and bone marrow were prepared and cultured under conditions identical to those for first-trimester fetal blood (10% FBS with no additional growth factors), adherent cells were seen whose morphologic appearance was identical to that of fetal blood (Figure 1E-L). Frequencies of adherent, fibroblastlike colonies in first-trimester liver and bone marrow were 11.3 ± 2.0/106 nucleated cells and 12.6 ± 3.6/106 nucleated cells, respectively.
Growth characteristics of first-trimester fetal blood, liver, and bone marrow mesenchymal stem/progenitor cells
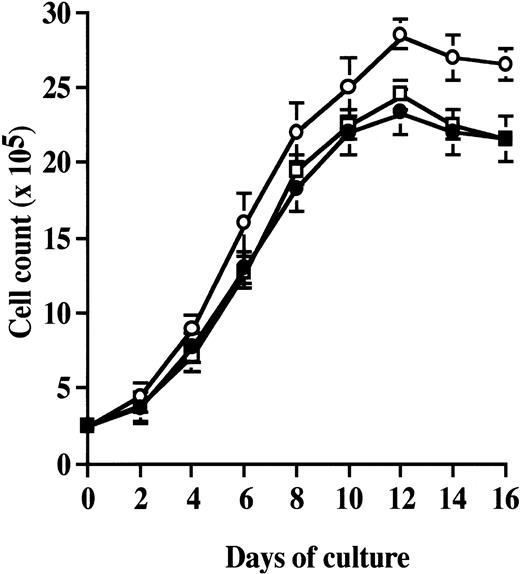
The growth kinetics of single colony-derived fetal blood adherent cells (n = 3) was measured at passage 2 (Figure2). Cells were allowed to divide for 16 days, duplicate cultures were harvested daily, and cell counts were taken. Growth curves depicted an initial lag phase of 2 days, followed by a log phase in which cells divided at exponential rates for 3 to 6 days. The log phase was followed by a plateau phase. Fetal blood adherent cells could be readily expanded in vitro by successive cycles of trypsinization, seeding, and culture every 5 days for 20 passages. The mean cumulative number of population doublings for fetal blood-derived colonies was 50.3 ± 4.5. Cells that had undergone up to 20 passages displayed no visible changes either in terms of their morphology by light microscopy, their forward and side scatter properties on flow cytometry, or their growth patterns. Similar growth patterns were observed with single colonies derived from first-trimester fetal liver and fetal bone marrow adherent cells (Figure 2). The mean cumulative number of population doublings of fetal liver and bone marrow adherent colonies was 52.2 ± 5.3 and 49.5 ± 3.5, respectively.
Growth curves of first-trimester MSCs from fetal blood, fetal liver, and fetal bone marrow.
Fetal MSCs were plated at a density of 10 000 cells/cm2, duplicate cultures were harvested each day for 16 days, and the number of adherent cells was determined. Results are expressed as mean ± SEM. Fetal blood, ●, n = 3; fetal liver, ○, n = 3; and fetal bone marrow, ■, n = 3.
Growth curves of first-trimester MSCs from fetal blood, fetal liver, and fetal bone marrow.
Fetal MSCs were plated at a density of 10 000 cells/cm2, duplicate cultures were harvested each day for 16 days, and the number of adherent cells was determined. Results are expressed as mean ± SEM. Fetal blood, ●, n = 3; fetal liver, ○, n = 3; and fetal bone marrow, ■, n = 3.
Immunophenotype of first-trimester fetal blood, liver, and bone marrow mesenchymal stem/progenitor cells
The immunophenotype of monolayer and single colony-derived adherent cells from first-trimester fetal blood, liver, and bone marrow was determined by flow cytometry and in situ immunocytochemistry using the antibodies listed in Table 1. The staining pattern of the monolayer-derived cells was identical to that seen for the single colony-derived cells. As shown in Table 1, fetal blood adherent cells stained positively for prolyl-4-hydroxylase; α-smooth muscle actin; the hyaluronate receptor, CD44; VCAM-1, a member of the immunoglobulin superfamily; endoglin (CD105); β1 integrin (CD29); SH2; SH3; SH4; laminin; fibronectin; and vimentin. Significantly, fetal blood adherent cells were all CD45− (Figure 3A), consistent with a nonhematopoietic origin and confirming that hematopoietic cells had been depleted from the cultures. In line with this finding, no macrophages (CD14+ cells; Figure 3A) could be detected in the cultures. Finally, fetal blood adherent cells were all CD34− and CD31(PECAM-1)− (Figure 3A). Cytoplasmic von Willebrand factor (vWF) expression was not detected, indicating that they were not endothelial cells. Adherent cells isolated from first-trimester fetal liver and bone marrow showed a similar immunophenotype (Table 1, Figure 3B-C). The immunophenotypic profile of fetal blood, liver, and bone marrow adherent cells did not change after 10 passages in culture.
Immunophenotype of cultured first-trimester fetal mesenchymal stem/progenitor cells
| Antigen . | Fetal blood . | Reactivity . | |
|---|---|---|---|
| Fetal liver . | Fetal bone marrow . | ||
| CD45* | − | − | − |
| CD14* | − | − | − |
| CD68† | − | − | − |
| CD29* | + | + | + |
| CD44* | + | + | + |
| CD105* | ± | ± | ± |
| CD106† | + | + | + |
| CD31* | − | − | − |
| vWF† | − | − | − |
| CD34* | − | − | − |
| HLA-DR* | − | − | − |
| SH2* | + | + | + |
| SH3* | + | + | + |
| SH4* | + | + | + |
| Myoglobin† | − | − | − |
| α-smooth muscle actin† | ± | ± | ± |
| Prolyl-4-hydroxylase† | + | + | + |
| Collagen type 1† | − | − | − |
| Fibronectin† | + | + | + |
| Laminin† | + | + | + |
| Vimentin† | + | + | + |
| Antigen . | Fetal blood . | Reactivity . | |
|---|---|---|---|
| Fetal liver . | Fetal bone marrow . | ||
| CD45* | − | − | − |
| CD14* | − | − | − |
| CD68† | − | − | − |
| CD29* | + | + | + |
| CD44* | + | + | + |
| CD105* | ± | ± | ± |
| CD106† | + | + | + |
| CD31* | − | − | − |
| vWF† | − | − | − |
| CD34* | − | − | − |
| HLA-DR* | − | − | − |
| SH2* | + | + | + |
| SH3* | + | + | + |
| SH4* | + | + | + |
| Myoglobin† | − | − | − |
| α-smooth muscle actin† | ± | ± | ± |
| Prolyl-4-hydroxylase† | + | + | + |
| Collagen type 1† | − | − | − |
| Fibronectin† | + | + | + |
| Laminin† | + | + | + |
| Vimentin† | + | + | + |
Assessed by flow cytometry.
Assessed by in situ immunocytochemistry.
− indicates no cells stained positively; ±, 10% to 15% of cells stained positively; +, more than 99% of cells stained positively.
Immunophenotype of fetal MSCs by FACS analysis.
MSCs (at the second and tenth passages in culture) from fetal blood (A; n = 6), liver (B; n = 4), and bone marrow (C; n = 4) were stained with surface antibodies and analyzed by FACS.
Immunophenotype of fetal MSCs by FACS analysis.
MSCs (at the second and tenth passages in culture) from fetal blood (A; n = 6), liver (B; n = 4), and bone marrow (C; n = 4) were stained with surface antibodies and analyzed by FACS.
Immunophenotypic characterization of these cells allowed us to use fluorescence-activated cell sorting (FACS) analysis to determine the frequency of MSCs in first-trimester fetal blood by staining freshly collected blood samples (n = 3; median, GA 9+5 weeks; range, 9+3 to 10+2) with SH-3, an antibody that recognizes a cell surface epitope present on human mesenchymal progenitor cells.24 25 A frequency of 0.33% ± 0.05% SH-3+ cells was found (equivalent to 0.18 ± 0.02 × 106 SH-3+ cells/mL), almost exactly matching the percentage of MSCs identified on morphologic grounds after Leishman staining of the cytospins of first-trimester blood (0.4% ± 0.04%). Because the number of colony-forming cells in first-trimester blood was only 8.2 ± 0.6/106 cells (0.0008% of nucleated cells), this indicates that colony-forming mesenchymal cells represent 0.2% of circulating mesenchymal cells during the first trimester.
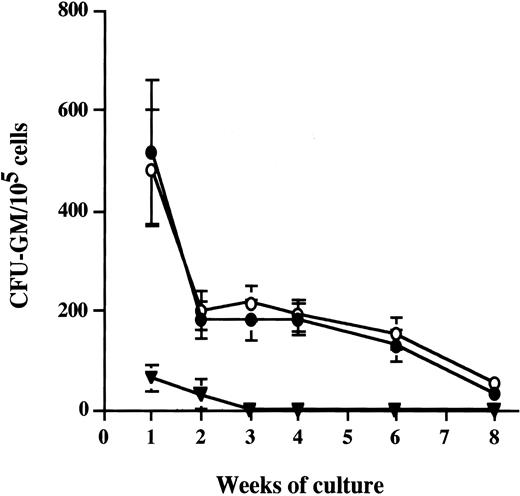
Ability of fetal blood mesenchymal stem/progenitor cells to support long-term hematopoiesis
To determine whether fetal blood MSCs were capable of supporting the proliferation and differentiation of hematopoietic stem–progenitor cells, second-passage MSCs (n = 3; median gestational age, 9+4 weeks) were irradiated and seeded in 12-well plates to form a semiconfluent monolayer. The next day, human CD34+cord blood cells (5 × 104 CD34+ cells/well) were overlaid and maintained in culture for up to 8 weeks in long-term culture (LTC) medium. As controls, umbilical cord blood CD34+ cells were overlaid on wells with a murine stromal cell line layer (M210B4) or were cultured in the absence of a stromal layer. Similar numbers of typical cobblestone areas, representing foci of hematopoiesis, were observed after 3 weeks culture on both fetal MSCs and M210B4 cultures, whereas no sign of hematopoiesis was observed when CD34+ cells were cultured in the absence of any stromal feeder. Granulocyte macrophage–colony-forming unit (CFU-GM) assays were carried out on the cells contained in the nonadherent fraction of the cultures at weekly intervals and at the time of termination of the cultures. No difference was detected in the number of CFU-GM progenitors generated from CD34+ cells cocultured with the fetal MSC or the M210B4 cell line at any time point (Figure4). By contrast, CD34+ cord blood cells grown in LTC medium in the absence of stromal cells and growth factors produced no clonogenic progenitors after 2 weeks of culture (Figure 4).
Coculture of fetal MSCs with umbilical cord blood CD34+ hematopoietic stem–progenitor cells.
Umbilical cord blood CD34+ cells were cocultured with fetal blood MSCs for 6 weeks (n = 2) and for 8 weeks (n = 1) (●). Control data include cord blood CD34+ cells grown either on murine stromal cells (○) or without stromal cells (▾).
Coculture of fetal MSCs with umbilical cord blood CD34+ hematopoietic stem–progenitor cells.
Umbilical cord blood CD34+ cells were cocultured with fetal blood MSCs for 6 weeks (n = 2) and for 8 weeks (n = 1) (●). Control data include cord blood CD34+ cells grown either on murine stromal cells (○) or without stromal cells (▾).
Differentiation of fetal blood, liver and bone marrow mesenchymal stem/progenitor cells into adipocytes, osteocytes, and chondrocytes
The differentiation potential of MSCs from first-trimester fetal blood, liver, and bone marrow was tested by culturing cells under conditions that favored adipogenic, osteogenic, and chondrogenic differentiation of adult MSCs.22 23 The first of two approaches we used was to use cloning cylinders to isolate individual colonies from second-passage MSCs. With this approach, adipogenic differentiation from single adherent colonies from first-trimester fetal blood samples (n = 6) was apparent after 2 weeks of incubation with hydrocortisone, indomethacin, and hydroxybutylmethylxanthine by the accumulation of Oil-red-O staining lipid-rich vacuoles: 77.3% ± 2.9% of cells from fetal blood MSCs differentiated into adipocytes (Figure 5A). A similar proportion of cells from fetal liver MSCs (75.2% ± 6.5%; n = 4) and fetal bone marrow MSC (85.2% ± 4.3%; n = 4) differentiated into adipocytes (Figure 5D,G). By contrast, when MSCs from the same fetal blood colonies that differentiated into adipocytes in adipogenic medium were cultured for 2 weeks with dexamethasone, β-glycerophosphate, and ascorbic acid to induce osteogenic differentiation, they formed aggregates and calcium deposits consistent with bone formation (n = 6 experiments; Figure 5B). MSCs from first-trimester fetal liver and bone marrow colonies also underwent progressive osteogenic differentiation when cultured under identical conditions (Figure 5E,H). MSCs from the same fetal blood colonies that differentiated into adipocytes and osteocytes also underwent chondrogenic differentiation, forming chondrocytelike lacunae visualized in histologic sections after 3 weeks of culture in serum-free chondrogenic medium and an extracellular matrix rich in types 1 and 2 collagens, together with the accumulation of anionic (toluidine blue) and sulfated (Sufranin O) proteoglycans (n = 6 experiments; Figure 5C). First-trimester fetal liver and bone marrow single colony-derived MSCs also underwent chondrogenic differentiation (Figure 5F,I) when cultured under identical conditions. Finally, we found that even late-passage (eighth passage) fetal MSCs from first-trimester fetal blood, liver, or bone marrow retained the ability to differentiate into all 3 lineages.
Differentiation of fetal MSCs from into adipocytes, osteocytes, and chondrocytes.
First-trimester fetal blood (9+2 weeks; A-C), fetal liver (14+0 weeks; D-F), and fetal bone marrow (11+2weeks; G-I) into adipocytes, osteocytes, and chondrocytes. Adipogenic differentiation was indicated by accumulation of neutral lipid vacuoles that stained with Oil-red-O (A, D, and G, × 400 magnification), and such changes were not evident with human foreskin fibroblasts (J). Osteogenic differentiation was indicated by calcium deposition (B, E, and H, × 400 magnification), which stained with silver nitrate; this was not seen in foreskin fibroblasts (K). Chondrogenic differentiation was shown by staining with a monoclonal antibody to type 2 collagen and by the formation of lacunae (C, F, and I, × 400 magnification), not seen by similarly culturing human foreskin fibroblasts (L), which also produce collagen type 2.
Differentiation of fetal MSCs from into adipocytes, osteocytes, and chondrocytes.
First-trimester fetal blood (9+2 weeks; A-C), fetal liver (14+0 weeks; D-F), and fetal bone marrow (11+2weeks; G-I) into adipocytes, osteocytes, and chondrocytes. Adipogenic differentiation was indicated by accumulation of neutral lipid vacuoles that stained with Oil-red-O (A, D, and G, × 400 magnification), and such changes were not evident with human foreskin fibroblasts (J). Osteogenic differentiation was indicated by calcium deposition (B, E, and H, × 400 magnification), which stained with silver nitrate; this was not seen in foreskin fibroblasts (K). Chondrogenic differentiation was shown by staining with a monoclonal antibody to type 2 collagen and by the formation of lacunae (C, F, and I, × 400 magnification), not seen by similarly culturing human foreskin fibroblasts (L), which also produce collagen type 2.
To investigate this further, we used a second approach to assess the differentiation potential of individual MSCs from first-trimester fetal blood, liver, and bone marrow. Using single cell sorting of second-passage MSCs by flow cytometry, individual colonies derived from single FACS-sorted cells were grown in 96-well plates; cells derived from these clones were then subcultured in adipogenic, osteogenic, or chondrogenic media. Cloning efficiency varied from 10% to 17% (n = 3 experiments), and 25% to 30% of the colonies expanded fairly rapidly to more than 1000 cells over a 2-week period; these rapidly growing colonies were used for subsequent differentiation experiments. Such cells (derived from first-trimester blood, marrow, and liver) all retained the ability to differentiate into multiple lineages. Interestingly, however, we found that though single colonies derived from first-trimester fetal blood or liver underwent osteogenic and chondrogenic differentiation, they appeared to lose their capacity for adipogenic differentiation (0 of 4 colonies). By contrast, 50% of the colonies derived from single cells from first-trimester fetal bone marrow retained the capacity for differentiation in all the lineages (adipogenic, osteogenic and chondrogenic).
Discussion
Although it is known that adult bone marrow–derived MSCs can be rapidly expanded in vitro, migrate, and differentiate into multiple tissues in vivo, there is little information about the characteristics and functional properties of MSCs in the fetus. We report the isolation and characterization of MSCs from first-trimester human fetal blood, liver, and bone marrow.
These 3 anatomic sites are likely sources of fetal MSCs for several reasons. First, it is clear that in adult bone marrow, mesenchymal cells provide signals for differentiation and proliferation of hematopoietic stem cells and their progeny through direct cell-cell interactions26 and secretion of hematopoietic growth factors and cytokines.27-29 Second, during human ontogeny, it has been demonstrated that proliferation and differentiation of hematopoietic stem–progenitor cells occurs in a number of histologically distinct microenvironments (yolk sac,30ventral aorta,31 fetal liver, thymus, spleen, and bone marrow20) and that stem cells migrate from one anatomic site to another through the circulation.32-34 Finally, mesenchymal cells have been shown to colocalize with foci of hematopoiesis early in ontogeny.36
Studies of fixed preparations of human fetal long bones before and immediately after the onset of hematopoiesis show that early in gestation (6-8.5 weeks), long bone rudiments contain mainly chondrocytes, osteoblasts, osteoclast precursors, and CD68+monocyte–macrophages.35 After this, at 8 to 10 weeks' gestation, at or just before hematopoietic colonization of the bone marrow, vascular cells, including CD34+ endothelial cells and α-smooth muscle actin–positive myoid cells, can be found in close contact with hematopoietic cells within the “primary logettes” of the marrow. Tavian et al36 showed, on fixed sections of human embryos, that (1) at day 26 to 27 after conception, CD45− α-smooth muscle actin–positive cells appeared in the mesenchyme underlying the endothelium of the ventral surface of the dorsal aorta; (2) these α-smooth muscle actin–positive cells were strictly confined to those areas containing clusters of CD34+ hematopoietic cells; and (3) by day 35, the 2 cell populations appeared to be in direct contact. Van den Heuvel et al37 showed that the number of fibroblast colony-forming units in murine fetal liver, spleen, and bone marrow becomes maximal at the time hematopoiesis begins at each site and that active hematopoiesis is preceded by the development of the stromal cell compartment. Similarly, Klein et al38 found high numbers of fibroblast colony-forming units in canine bone marrow before the appearance of hematopoietic stem cells.
When fetal samples older than 13 weeks of gestation were cultured at a plating density of 106 nucleated cells, we could identify MSCs in fetal liver and bone marrow but not in fetal blood samples. However, small numbers of MSCs could be cultured from second- and third-trimester blood samples when the mononuclear cells were plated at a 25-fold higher density. Their frequencies were 1.3/106mononuclear cells in the second trimester and 0.35/106mononuclear cells in term cord blood, thereby confirming the work of others17 showing that it is possible to demonstrate such cells at term but that they are present at an extremely low frequency. These data indicate that the frequency of circulating MSCs decreases substantially with gestational age; we speculate that this might be related to their migration from one hematopoietic site to another during ontogeny, ultimately to colonize bone marrow.
Lines of evidence indicate that the fetal MSCs we have identified in first-trimester fetal blood, liver, and bone marrow are similar to those present in adult bone marrow. First, their morphology and immunophenotype are similar to those of adult marrow MSCs, and they are clearly nonhematopoietic and nonendothelial—consistently CD45−, CD34−, CD14−, CD31−, and vWF-negative, as reported for adult MSCs.4,39 Like adult MSCs, first-trimester fetal MSCs also express a large number of adhesion molecules, including H-CAM (CD44), VCAM-1 (CD106), and CD29 and, in their undifferentiated state, are uniformly positive for intracellular markers such as fibronectin, vimentin, laminin, and prolyl-4-hydroxylase and for some mesenchymal markers, such as SH-2, SH-3, and SH-4. In addition, like adult MSCs,39 fetal MSCs isolated from first-trimester fetal blood are able to support proliferation and differentiation of hematopoietic stem/progenitor cells in vitro. Finally, like their adult counterparts,5 fetal MSCs have the ability to differentiate into at least 3 different tissues: fat, bone, and cartilage. We assessed this by seeding first-trimester blood, liver, and bone marrow nucleated cells at low density and plucking discrete colonies using cloning cylinders5 and by single-cell sorting. In the former method, all isolated colonies showed signs of differentiation into all 3 lineages when incubated in permissive media, even after 8 passages in culture. With the latter method, which can be considered a more appropriate method to prove clonality because it excludes the collection of “contaminating” cells migrating from neighboring colonies, single colonies from fetal bone marrow retained the capacity for adipogenic, osteogenic, and chondrogenic differentiation, whereas the colonies derived from fetal blood or fetal liver appeared to lose their capacity for adipogenic differentiation.
There are several explanations for the discrepant results obtained using cloning cylinders compared to single-cell sorting. One is that although cultures of fetal MSCs are morphologically and phenotypically homogenous, they might contain cell populations with distinct differentiation potential, as has been observed in adult MSCs.5,40 Alternatively, if the proportion of stem cells with multilineage differentiation potential is very low, then a large number of single cell-derived colonies would have to be isolated and investigated to identify those with stem cell properties. In addition, our results are likely to reflect different methods of MSC colony growth and expansion; in particular, cell-cell contact may play a role in the expansion and multilineage differentiation of fetal MSCs. It is interesting that adult MSCs, which have been extensively cultured (passages 8 to 14), have also been reported to lose their capacity for adipogenic differentiation while osteogenic differentiation is preserved.40 Finally, it is possible that in the intense replicative stress of single sorted cells, culture conditions for adipogenic differentiation might have been suboptimal.
The function of fetal MSCs in the human fetus remains to be determined, though they are highly likely to play a role in the establishment and maintenance of hematopoietic stem and progenitor cells. Cotransplantation of adult MSCs has been shown to enhance engraftment of hematopoietic stem cells in a fetal sheep model,10-12suggesting that in utero cotransplantation of fetal MSCs may also result in accelerated hematopoietic cell engraftment. First-trimester fetal blood represents a potentially harvestable source of autologous MSCs amenable to genetic manipulation and reinfusion in ongoing pregnancies. Indeed, fetal blood has been sampled in ongoing pregnancies from as early as 12 weeks,41 and, with advances in embryofetoscopic cannulation techniques,42 may become obtainable even earlier. We are currently assessing the possible use of fetal blood MSCs for in utero gene therapy for genetic disorders.
In conclusion, a population of MSCs was isolated from fetal blood, liver, and bone marrow in the first-trimester of pregnancy. These cells possess morphologic, immunophenotypic, and functional characteristics similar to those of adult-derived MSCs. Fetal MSCs might provide useful models for investigation of mesenchymal cell differentiation and regulation of hematopoiesis during ontogeny.
Supported in part by project grants from Wellbeing.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Cesare Campagnoli, Department of Maternal and Fetal Medicine, Institute of Reproductive and Developmental Biology, Imperial College School of Medicine, Hammersmith Campus, Du Cane Road, London W12 0NN, United Kingdom; e-mail: c.campagnoli@ic.ac.uk.




This feature is available to Subscribers Only
Sign In or Create an Account Close Modal