Key Points
Novel RARG-CPSF6 fusion in an AML case with promyelocytic features and no evidence of PML-RARA or X-RARA fusion.
Gene fusions involving RARG can initiate AML with promyelocytic morphological features.
Introduction
Although almost all cases of acute promyelocytic leukemia (APL) are associated with the t(15;17)(q24;q21) translocation that creates the chimeric promyelocytic leukemia (PML)–RARA oncogene (present in ∼98%-99% of cases), alternative X-RARA fusions can initiate acute myeloid leukemia (AML) with promyelocytic features.1 In both APL driven by PML-RARA and the AMLs driven by variant RARA translocations, the DNA-binding, retinoid X receptor (RXR)-binding, and ligand-binding domains of retinoic acid receptor (RAR) α (RARA) are preserved in the fusion proteins.2 RAR β (RARB) and RAR γ (RARG) are the 2 other RARs. The 3 RARs are highly homologous: they have highly conserved DNA-binding and ligand-binding domains.3 Although uncommon, gene fusions involving RARB (TBL1XR1-RARB) and RARG (PML-RARG and NUP98-RARG) have been reported in cases of AML with promyelocytic features.4-6 As in the PML-RARA and X-RARA fusions, the RARB and RARG fusions preserve the DNA-binding and ligand-binding domains of the RARs. We now report a third gene fusion involving RARG, a RARG-CPSF6 fusion, in a patient with AML that appeared to be typical APL by standard histopathology and immunophenotyping.
Case description
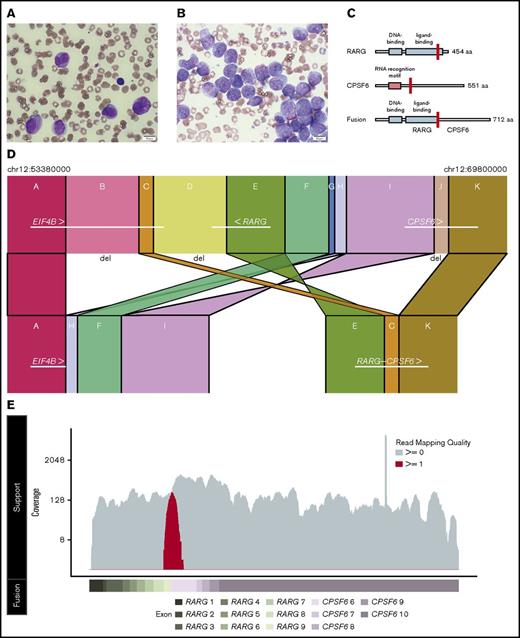
We report a patient presenting with AML with promyelocytic features without a detectable PML-RARA fusion by routine cytogenetics, standard fluorescence in situ hybridization (FISH), or reverse transcription–polymerase chain reaction (RT-PCR). The patient was a 26-year-old white man with no significant past medical history who presented with a 2-week history of epistaxis, gingival bleeding, and petechiae. His complete blood count showed a white blood cell (WBC) count of 16.4 × 109/L, hemoglobin of 10.5 g/dL, and platelet count of 52 × 109/L. Review of the peripheral blood smear revealed numerous circulating promyelocytes (81% of WBCs) and 3% circulating blasts, including many with Auer rods. The patient had a consumptive coagulopathy. The diagnostic bone marrow biopsy aspirate had a differential of 60% blasts, 15% promyelocytes, 6% myelocytes, and 1% metamyelocytes (the core biopsy showed overall cellularity of >90%). By morphology, review of the peripheral blood and bone marrow was consistent with the diagnosis of hypergranular (or “typical”) APL (Figure 1A-B). The promyelocytes had enlarged, convoluted, oval to irregularly shaped (including some bilobed or kidney-shaped) nuclei, dispersed chromatin, inconspicuous nucleoli, and abundant dust-like azurophilic granules. These cells demonstrated strong and diffuse reactivity to myeloperoxidase cytochemical staining, which often masked the nucleus and is characteristic of APL. Flow cytometry performed on the bone marrow aspirate showed blasts comprising 53% of marrow cellularity. The blasts were positive for CD33, CD13, CD64, CD117 (partial), and HLA-DR (weak). The blasts were negative for CD34, CD56, CD19, CD2, CD5, CD123, CD14, CD11b, and terminal deoxynucleotidyl transferase (TdT). Cytogenetic studies revealed an intermediate-risk karyotype of: 45, X, −Y [10]/45, idem, add(6)(q?13) [2]/46, XY[8]. Given the concern for APL, the patient was immediately treated with all-trans retinoic acid (ATRA); 7+3 chemotherapy (idarubicin and cytarabine) was started in addition to ATRA on day 2.
Histopathologic and genomic characterization of a case of AML with promyelocytic features. (A) Wright-Giemsa staining of the peripheral blood smear highlighting promyelocytes (original magnification ×100). (B) Wright-Giemsa staining of the aspirate from the diagnostic bone marrow biopsy highlighting numerous blasts and promyelocytes (original magnification ×100). The images were captured by an Olympus BX53 microscope with an Olympus UPlanSApo 100×/1.4 oil objective and an Olympus DP26 digital camera with Olympus cellSens standard software (version 1.16; Tokyo, Japan). (C) Representative schematic of the main protein domains of RARG isoform 1 (top), CSPF6 isoform 2 (middle), and the predicted RARG-CPSF6 fusion (bottom) with the fusion breakpoints highlighted in red (for RARG at amino acid 392 and for CPSF6 at amino acid 231). Isoform choice was based on read support from the RNA-Seq data. (D) Schematic of the highly rearranged region on chromosome 12 where the reciprocal inversion occurred. In panel D, regions A and K bookend regions B-J that were involved in distinct deletions or rearrangement events. The segments are not to scale. (E) RNA-Seq reads based on a pseudo-alignment to the RARG-CPSF6 predicted fusion transcript. The coverage of reads uniquely aligned to the predicted fusion (spanning the fusion breakpoint) is displayed in red on the top track in relation to the exons for the predicted fusion (bottom track). We observed only three reads supporting wild-type RARG expression, which are likely indicative of a small number of contaminating benign cells.
Histopathologic and genomic characterization of a case of AML with promyelocytic features. (A) Wright-Giemsa staining of the peripheral blood smear highlighting promyelocytes (original magnification ×100). (B) Wright-Giemsa staining of the aspirate from the diagnostic bone marrow biopsy highlighting numerous blasts and promyelocytes (original magnification ×100). The images were captured by an Olympus BX53 microscope with an Olympus UPlanSApo 100×/1.4 oil objective and an Olympus DP26 digital camera with Olympus cellSens standard software (version 1.16; Tokyo, Japan). (C) Representative schematic of the main protein domains of RARG isoform 1 (top), CSPF6 isoform 2 (middle), and the predicted RARG-CPSF6 fusion (bottom) with the fusion breakpoints highlighted in red (for RARG at amino acid 392 and for CPSF6 at amino acid 231). Isoform choice was based on read support from the RNA-Seq data. (D) Schematic of the highly rearranged region on chromosome 12 where the reciprocal inversion occurred. In panel D, regions A and K bookend regions B-J that were involved in distinct deletions or rearrangement events. The segments are not to scale. (E) RNA-Seq reads based on a pseudo-alignment to the RARG-CPSF6 predicted fusion transcript. The coverage of reads uniquely aligned to the predicted fusion (spanning the fusion breakpoint) is displayed in red on the top track in relation to the exons for the predicted fusion (bottom track). We observed only three reads supporting wild-type RARG expression, which are likely indicative of a small number of contaminating benign cells.
Standard AML molecular diagnostics were performed, and no other prognostically significant mutations were identified. We performed FISH with a RARA break-apart probe to detect X-RARA fusions, which was negative. In an effort to identify a cryptic PML-RARA fusion, we performed anti-PML immunostaining, which was normal.7 Given the absence of evidence of a RARA rearrangement, we hypothesized that an alternative genetic mechanism was driving this AML with promyelocytic features.
Methods
All sequencing runs were completed according the manufacturer’s recommendations (Illumina Inc, San Diego, CA). We used the latest version of our genome modeling system to complete the analysis (supplemental Methods; supplemental Data Files 1-5).8
The UAS-GFP and Gal4 construct cotransduction experiments were done as previously described. We created a truncated RARG*395 based on whether the RARG transcript did not splice into CPSF6 and translation read through into the intron (the next codons are: g/gt gag tca tga, and tga stops) (see supplemental Methods for the detailed methodology for western blotting, RT-PCR validation, and cotransduction experiments).9
Results and discussion
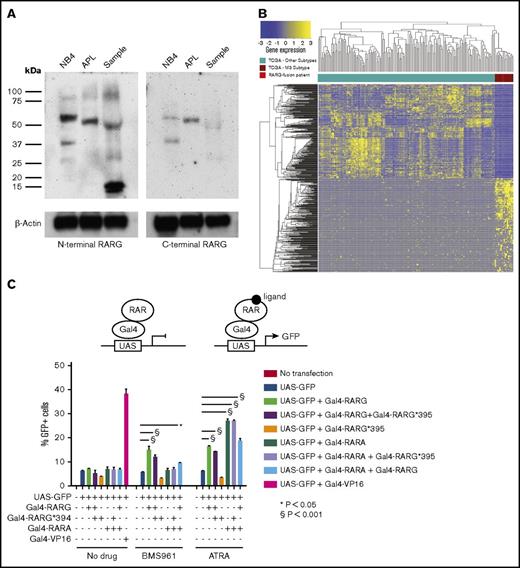
We performed whole-genome sequencing (WGS) and RNA sequencing (RNA-Seq) on DNA and RNA isolated from bulk, cryopreserved cells from the diagnostic bone marrow aspirate. We used DNA isolated from a skin biopsy as the “normal/germ line” comparator for WGS. We identified 9 total nonsilent coding somatic mutations (see supplemental Table 1 and supplemental Figure 1 for copy number events). Mutations in 3 of these genes (BMPR1A, NEAT1, and WT1) are thought to have a role in leukemogenesis.10-12 Notably, 2 truncating mutations were observed in WT1 (E340* and S1381*). WT1 has a complex pathogenic role in AML but is recurrently mutated in 5.5% of AML cases overall and is more common in APL (11%).10 We did not detect a PML-RARA or X-RARA fusion. We did identify a highly rearranged region (including multiple deletions, inversions, and intrachromosomal translocations) on chromosome 12 with break points in the EIF4B, RARG, and CPSF6 genes. The rearrangement resulted in a fusion of RARG (in intron 9) to EIF4B (in intron 8) and a deletion after intron 8 of EIF4B that then fused into the intron leading into exon 6 of CPSF6 (Figure 1C-D). This created a novel RARG-CPSF6 in-frame fusion transcript, which was validated by RNA-Seq read support as well as by RT-PCR followed by Sanger sequencing (Figure 1E; supplemental Figure 2). The RARG-EIF4B genomic rearrangement was also confirmed by PCR followed by Sanger sequencing (supplemental Figure 3; supplemental Data File 6). Immunoblotting with an N-terminal anti-RARG antibody or an anti-CPSF6 antibody did not show clear evidence of an expressed RARG-CPSF6 fusion protein (predicted at 78 kDa) (Figure 2A; supplemental Figure 4). If the RARG-CPSF6 fusion protein was expressed, it would have a C-terminal breakpoint disrupting the ligand-binding domain of RARG rather than the N-terminal breakpoints that occur in the other X-RAR fusions that preserve both the DNA- and ligand-binding domains (Figure 1C).3-6
Protein analysis and functional characterization of the RARG-CPSF6 gene fusion. (A) N-terminal and C-terminal anti-RARG antibodies were used to probe immunoblots prepared from NB4 cells (an APL cell line), a t(15;17) APL sample, and a sample from our patient. Both experiments were repeated independently with similar results. (B) Supervised hierarchical clustering of the top 500 dysregulated genes in t(15;17) APL (compared to all of the other non-t(15;17) AML cases included in the TCGA AML analysis) clusters the case (bright red) with other APLs (dark red). (C) A schematic of the experimental platform (top). The Gal4-RARG*395 truncation did not activate the UAS-GFP reporter when treated with either ATRA or BMS961 (a RARG agonist). Gal4-RARG and Gal4-RARA both activated the UAS-GFP reporter in response to ATRA, and this was not inhibited by coexpression of Gal4-RARG*395, indicating that the truncated RARG did not act as a dominant-negative against RARA or RARG in this assay (* and § P values calculated by ANOVA with Bonferroni correction for multiple comparisons). This experiment was repeated independently with similar results.
Protein analysis and functional characterization of the RARG-CPSF6 gene fusion. (A) N-terminal and C-terminal anti-RARG antibodies were used to probe immunoblots prepared from NB4 cells (an APL cell line), a t(15;17) APL sample, and a sample from our patient. Both experiments were repeated independently with similar results. (B) Supervised hierarchical clustering of the top 500 dysregulated genes in t(15;17) APL (compared to all of the other non-t(15;17) AML cases included in the TCGA AML analysis) clusters the case (bright red) with other APLs (dark red). (C) A schematic of the experimental platform (top). The Gal4-RARG*395 truncation did not activate the UAS-GFP reporter when treated with either ATRA or BMS961 (a RARG agonist). Gal4-RARG and Gal4-RARA both activated the UAS-GFP reporter in response to ATRA, and this was not inhibited by coexpression of Gal4-RARG*395, indicating that the truncated RARG did not act as a dominant-negative against RARA or RARG in this assay (* and § P values calculated by ANOVA with Bonferroni correction for multiple comparisons). This experiment was repeated independently with similar results.
Using 178 samples from the TCGA AML cohort, we used a Student t test to identify genes with significantly different expression in the 16 APL samples, which all harbored t(15;17), compared with the other AML subtypes.13 The top 250 up- and downregulated genes were selected to define a 500 gene APL signature. Hierarchical clustering based on this signature grouped this case with the t(15;17) APLs (Figure 2B; supplemental Data File 7). Next, we performed in vitro cotransduction/transfection experiments using a Gal4-RARG*395 truncation construct (the fragment of RARG predicted to be expressed in the fusion) and a UAS-GFP reporter plasmid (Figure 2C). The Gal4-RARG*395 truncation did not activate the UAS-GFP reporter when cells were treated with either ATRA or BMS961 (a RARG agonist), suggesting that our case is ATRA-resistant. To determine whether the RARG*395 truncation could act as a dominant-negative, we performed a cotransduction/transfection experiment with truncated RARG and PPAR response element (PPRE)-luciferase or ApoA1-luciferase reporters in 293T cells. The expression of truncated RARG*395 neither augmented nor inhibited the response to ATRA or to the RARG-specific ligand BMS961, suggesting a null phenotype rather than a dominant-negative phenotype (data not shown).
RARG has leukemogenic potential when fused to PML both in vitro14 and in vivo.5,15 In addition to PML-RARG, a NUP98-RARG gene fusion has been reported in AML with APL-like morphologic and immunophenotypic features.6,16,17 This is the first report of a case of AML with promyelocytic features characterized by the expression of a RARG-CPSF6 fusion. CPSF6 is a subunit of the cleavage and polyadenylation specificity factor (CPSF) protein complex that is involved in the processing of the 3′ end of messenger RNA (mRNA) precursors.18 mRNA processing may be important mechanistically in AML with variant RAR translocations as FIP1L1-RARA fusions have been reported, and FIP1L1 is also a subunit of the CPSF complex.3 CPSF6 has been found to be a recurrent fusion partner in myeloid/lymphoid neoplasms associated with eosinophilia.19,20 In our case, the disruption of neighboring genes around the area of the complex rearrangement event on chromosome 12 and the other somatic mutations present could have contributed to the promyelocytic phenotype. Moreover, we did not detect the presence of an expressed RARG-CPSF6 fusion protein by immunoblotting. If the RARG-CPSF6 fusion protein was expressed, the fragment of RARG that is part of the fusion may not bind ligand given the truncation of the ligand-binding domain and the results of our cotransduction/transfection experiments. Future studies are needed to define the mechanisms by which the RARG-CPSF6 gene fusion and/or the loss of endogenous RARG expression (we did not detect significant WT RARG expression by RNA-Seq or immunoblotting) contribute to leukemogenesis.
Note added in proof
During the revision of this manuscript, 2 studies were published that identified cases of AML with promyelocytic features with CPSF6-RARG fusions [Liu T, Wen L, Yuan H, et al. Blood. 2018;131(16):1870-1873 and Qin YZ, Huang XJ, Zhu HH. Leukemia. doi:10.1038/s41375-018-0095-z].
The full-text version of this article contains a data supplement.
Acknowledgments
The authors thank Gayla Hadwigger for technical assistance and L. Jeffrey Medeiros from the Anderson Cancer Center for performing anti-PML immunostaining.
This work was supported by private research support from the Division of Oncology and the McDonnell Genome Institute. This work was also supported by the following National Institutes of Health grants: National Heart, Lung, and Blood Institute R01 HL128447 (J.S.W.); National Human Genome Research Institute K99 HG007940 (M.G.); and National Cancer Institute K22 CA188163 (O.L.G.), K08 CA166229 (L.D.W.), and R50 CA211782 (C.A.M.). Flow cytometry was performed in the Siteman Cancer Center Flow Cytometry Core, which is supported in part by National Institutes of Health, National Cancer Institute Cancer Center support grant P30 CA91842.
This work was performed as part of the Washington University School of Medicine Genomics Tumor Board.
Authorship
Contribution: C.A.M. conceived parts of the study, analyzed data, and wrote the manuscript; C.T. analyzed data and wrote the manuscript; Z.L.S., Y.-S.L., and A.H. analyzed data and produced figures; G.L.U. conceived parts of the study, acquired data, and edited the manuscript; M.D.O., H.S., and L.T. performed experiments, acquired data, and interpreted results; J.S.W. performed experiments, acquired data, interpreted results, and edited the manuscript; E.J.D., M.G., and O.L.G. interpreted results and provided critical review of the manuscript; and L.D.W. conceived and designed the work, analyzed the data, and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Lukas D. Wartman, Division of Oncology, Washington University School of Medicine, 660 South Euclid Ave, Campus Box 8007, St. Louis, MO 63110; e-mail: lwartman@wustl.edu.