Key Points
RIC is a reasonable alternative to MAC for CML patients in the TKI era.
In CML patients, RIC results in similar survival as MAC, albeit at the expense of increased early posttransplant relapse.
Abstract
Allogeneic hematopoietic cell transplantation (allo-HCT) is a potentially curative treatment of chronic myeloid leukemia (CML). Optimal conditioning intensity for allo-HCT for CML in the era of tyrosine kinase inhibitors (TKIs) is unknown. Using the Center for International Blood and Marrow Transplant Research database, we sought to determine whether reduced-intensity/nonmyeloablative conditioning (RIC) allo-HCT and myeloablative conditioning (MAC) result in similar outcomes in CML patients. We evaluated 1395 CML allo-HCT recipients between the ages of 18 and 60 years. The disease status at transplant was divided into the following categories: chronic phase 1, chronic phase 2 or greater, and accelerated phase. Patients in blast phase at transplant and alternative donor transplants were excluded. The primary outcome was overall survival (OS) after allo-HCT. MAC (n = 1204) and RIC allo-HCT recipients (n = 191) from 2007 to 2014 were included. Patient, disease, and transplantation characteristics were similar, with a few exceptions. Multivariable analysis showed no significant difference in OS between MAC and RIC groups. In addition, leukemia-free survival and nonrelapse mortality did not differ significantly between the 2 groups. Compared with MAC, the RIC group had a higher risk of early relapse after allo-HCT (hazard ratio [HR], 1.85; P = .001). The cumulative incidence of chronic graft-versus-host disease (cGVHD) was lower with RIC than with MAC (HR, 0.77; P = .02). RIC provides similar survival and lower cGVHD compared with MAC and therefore may be a reasonable alternative to MAC for CML patients in the TKI era.
Introduction
With the remarkable success of tyrosine kinase inhibitors (TKIs) for the treatment of patients with chronic myeloid leukemia (CML), the use of allogeneic hematopoietic cell transplantation (allo-HCT) since the turn of the century has dramatically decreased.1-4 Nonetheless, allo-HCT is a useful and potentially curative treatment option for a subset of CML patients who are refractory to or intolerant of TKIs and those who present in accelerated phase (AP) or blast phase (BP).5-8 Traditionally, myeloablative conditioning (MAC) is the standard intensity for CML patients in need of allo-HCT.8-10 MAC is, however, characterized by a high risk of toxicity and nonrelapse mortality (NRM), especially among patients with comorbid conditions and advanced age. This prompted exploration of reduced-intensity/nonmyeloablative conditioning (RIC) regimens.11,12
Retrospective studies comparing MAC with RIC in patients with acute myeloid leukemia (AML) or myelodysplastic syndromes suggested that RIC was associated with increased relapse but reduced NRM, resulting in similar overall survival (OS), even though patients receiving RIC were older and/or less fit.13-21 In contrast, a randomized phase 3 study (BMT CTN protocol 0901) demonstrated that in fit (hematopoietic cell transplant-comorbidity index [HCT-CI] ≤4) patients with AML or myelodysplastic syndromes in remission between the ages of 18 and 65 years receiving allo-HCT from HLA-identical sibling or unrelated donors, RIC resulted in lower NRM but a significant disadvantage in leukemia-free survival (LFS) compared with MAC.13 It is remarkable that in the era of TKIs, there is a dearth of evidence pertaining to the role of conditioning intensity on outcomes after allo-HCT for CML that may guide practice patterns. To date, no prospective or large observational study has evaluated outcomes after MAC and RIC allo-HCT for CML. We conducted a registry analysis from the observational database of the Center for International Blood and Marrow Transplant Research (CIBMTR) comparing outcomes after RIC and MAC for allo-HCT in the era of TKIs. We hypothesized that RIC allo-HCT is as efficacious as MAC allo-HCT in CML patients for survival outcomes, considering the evidence for the graft-versus-leukemia effect of allo-HCT.22
Patients and methods
Data sources
The CIBMTR is a combined research program of the Medical College of Wisconsin and the National Marrow Donor Program, which consists of a voluntary network of more than 450 transplantation centers worldwide that contribute detailed data on consecutive allogeneic and autologous transplantations to a centralized statistical center. Observational studies conducted by the CIBMTR are performed in compliance with all applicable federal regulations pertaining to the protection of human research participants. Protected health information issued in the performance of such research is collected and maintained in the CIBMTR’s capacity as a Public Health Authority under the Health Insurance Portability and Accountability Act Privacy Rule.
Patients
Patients with CML between 18 and 60 years of age who underwent allo-HCT using a sibling or unrelated donor23 between 2007 and 2014 were included in the study. Donors were matched to the recipients at the allele level at HLA-A, HLA-B, HLA-C, and HLA-DRB1 loci or mismatched at a single HLA locus. An upper age limit of 60 years was introduced as an inclusion criterion to restrict the patient population to a cohort where by age criteria both MAC and RIC would be feasible. Patients in the chronic phase (CP) or AP24 were included. Those in BP at allo-HCT were excluded to reduce bias, because inferior survival outcomes would be expected with an RIC (vs MAC) regimen in BP patients, as suggested by the results of the prospective CTN 0901 study.13 Patients with haploidentical or cord blood transplant were excluded not only to limit the heterogeneity of the study population but also because of the small number of patients. Conditioning intensity was determined per Consensus CIBMTR criteria: MAC regimens were defined by total body irradiation (TBI) ≥5 Gy single dose or ≥8 Gy fractionated or busulfan (Bu) dose >8 mg/kg oral or >6.4 mg/kg IV, whereas RIC regimens were defined by Bu dose ≤8 mg/kg oral or IV equivalent, melphalan (Mel) ≤150 mg/m2 or TBI ≤2 Gy.25
Study end points
The primary end point of the study was OS. OS was defined as the time from transplantation to death from any cause or last follow-up. Death from any cause was considered an event. Surviving patients were censored at last follow-up. Secondary end points included LFS, NRM, and cumulative incidence of relapse and chronic graft-versus-host disease (cGVHD). LFS was defined as time from transplantation to either relapse or death from any cause, and alive patients were censored at the time of relapse or last follow-up. NRM was defined as death from any cause in continuous remission and was summarized by cumulative incidence estimate with relapse as competing risk. Relapse was summarized by cumulative incidence estimate with NRM as the competing risk. For relapse and NRM, patients in continuous complete remission were censored at last follow-up. cGVHD was graded per Consensus criteria.26 For cGVHD, death without the event was considered a competing event.
Statistical analysis
This is a retrospective comparative cohort study comparing outcomes after RIC vs MAC allo-HCT using related and unrelated donors for patients with CML in CP or AP. Eligible patients were stratified according to RIC vs MAC. The objective of this analysis was to compare these 2 types of conditioning regimens and their effect on outcomes after allo-HCT. The outcomes studied were OS, LFS, relapse rate, and incidence of cGVHD and NRM. Probabilities of NRM, relapse, and cGVHD were calculated by cumulative incidence function accounting for competing risks. Comparisons of cumulative incidence across time cohorts were performed via Gray’s test. Multivariable analyses were performed to evaluate associations among patient-related (age, Karnofsky Performance Score [KPS], HCT-CI, and Sorror comorbidity index27 ), disease-related (time from diagnosis to transplant and disease status at transplant), donor-related (donor type, cytomegalovirus [CMV] match, and sex match) and transplantation-related (year of transplant, GVHD prophylaxis, graft source, and in vivo T-cell depletion) variables and outcomes of interest (OS, LFS, NRM, GVHD, and relapse) using a Cox proportional hazards regression model. Forward stepwise selection was used to identify significant covariates that influenced outcomes. Disease status at transplant was categorized into chronic phase 1 (CP1), CP2 and beyond (CP2+), and AP. Covariates with P < .05 were considered significant. The proportional hazards assumption for Cox regression was tested by adding a time-dependent covariate for each risk factor and each outcome. Covariates violating the proportional hazards assumption were added as time-dependent covariates in the Cox regression model. Adjusted probabilities for OS, LFS, NRM, cGVHD, and relapse were calculated based on the final Cox models.28,29 The findings of multivariate analysis of cGVHD, NRM, and relapse by the Cox regression model were confirmed using the Fine-Gray model of competing risks. Interactions between the main effect (conditioning regimen) and significant covariates were examined. Power analysis was conducted; it was assumed that OS at 5 years for RIC was 60%. The median censoring time was assumed to be 7 years. Assuming OS of 45% at 5 years for MAC (relative risk, 1.56), the study had 92% statistical power. All analyses were performed using SAS 9.4.
Results
Patient, disease, and transplantation characteristics
Using the eligibility criteria, a total of 1395 patients were included in the study population, of which 1204 received MAC and 191 received RIC. Patient, disease, and transplantation characteristics were similar, with a few exceptions (Table 1). The median ages in MAC and RIC groups were 43 (range, 18-60) and 51 (range, 19-60) years, respectively. There were more males in the MAC group (60%) than the RIC group (47%). A greater proportion of MAC patients (70%) had KPS ≥90 compared with RIC (58%), and 20% and 30% of MAC and RIC recipients, respectively, had HCT-CI ≥3. As might be expected, the RIC cohort was enriched for older patients with lower KPS and higher HCT-CI. Median time from diagnosis to transplant was 23 months in the MAC cohort and 27 months in the RIC cohort. In both the cohorts, three-fourths of the patients received a peripheral blood graft. CP1 was the most common status prior to allo-HCT in both the MAC (42%) and RIC (48%) cohorts (P = .34). TKI was used for treatment before allo-HCT in 93% of MAC patients and 94% of RIC patients. In the MAC cohort, Bu/Cy was the most common regimen employed (40%), followed by Flu/Bu4 (24%) and Cy/TBI (24%). In the RIC cohort, Flu/Bu2 was the most common regimen (51%) followed by Flu/Mel (27%). In vivo T-cell depletion using ATG or alemtuzumab was used less commonly in the MAC cohort (22%) than the RIC cohort (47%). The majority of patients in both cohorts (88% in MAC and 90% in RIC) were from the North America or South America. Approximately 5% of patients were from Europe. Eastern Mediterranean, Southeastern Asian, and Western Pacific countries made up ∼5% of both cohorts. The median follow-up of survivors was 52 and 60 months in the MAC and RIC cohorts, respectively.
Characteristics of patients aged 18 to 60 years undergoing allo-HCT using MAC vs RIC for CML, 2007-2014
| Variable . | MAC (n = 1204) . | RIC (n = 191) . | P . |
|---|---|---|---|
| Follow-up of survivors, median (range), mo | 52 (4-102) | 60 (7-101) | |
| Number of centers | 163 | 76 | |
| Patient related | |||
| Age at transplant, median (range), y | 43 (18-60) | 51 (19-60) | <.001 |
| Age at transplant, y | <.001 | ||
| 18-29 | 212 (18) | 17 (9) | |
| 30-39 | 276 (23) | 21 (11) | |
| 40-49 | 404 (34) | 47 (25) | |
| 50-59 | 312 (26) | 106 (55) | |
| Sex | <.001 | ||
| Male | 722 (60) | 90 (47) | |
| Female | 482 (40) | 101 (53) | |
| KPS, % | <.001 | ||
| 90-100 | 845 (70) | 110 (58) | |
| <90 | 267 (22) | 72 (38) | |
| Missing | 92 (8) | 9 (5) | |
| WHO region | .60 | ||
| Africa | 1 (<1) | 0 | |
| Americas | 1054 (88) | 172 (90) | |
| Eastern Mediterranean | 22 (2) | 0 | |
| Europe | 78 (6) | 10 (5) | |
| Southeastern Asian | 21 (2) | 4 (2) | |
| Western Pacific | 27 (2) | 5 (3) | |
| Missing | 1 (<1) | 0 | |
| Sorror comorbidity index (HCT-CI) | .003 | ||
| 0 | 525 (44) | 64 (34) | |
| 1 | 132 (11) | 27 (14) | |
| 2 | 125 (10) | 25 (13) | |
| 3+ | 246 (20) | 58 (30) | |
| Missing | 176 (15) | 17 (9) | |
| Disease related | |||
| Disease status prior to transplant | .20 | ||
| CP1 | 504 (42) | 92 (48) | |
| AP | 405 (34) | 60 (31) | |
| CP2+ | 278 (23) | 38 (20) | |
| CP, NOS | 17 (1) | 1 (<1) | |
| Prior treatment | .85 | ||
| No | 9 (<1) | 1 (<1) | |
| Yes | 1185 (98) | 189 (99) | |
| Missing | 10 (<1) | 1 (<1) | |
| Use of TKI prior to HCT | .89 | ||
| No | 73 (6) | 11 (6) | |
| Yes | 1121 (93) | 179 (94) | |
| Missing | 10 (<1) | 1 (<1) | |
| TKI used pre-HCT | .11 | ||
| No TKI used | 73 (6) | 11 (6) | |
| Imatinib + dasatinib + nilotinib | 250 (21) | 52 (27) | |
| Imatinib + dasatinib | 295 (25) | 55 (29) | |
| Imatinib + nilotinib | 73 (6) | 13 (7) | |
| Dasatinib + nilotinib | 35 (3) | 8 (4) | |
| Imatinib | 395 (33) | 43 (23) | |
| Dasatinib | 52 (4) | 7 (4) | |
| Nilotinib | 21 (2) | 1 (<1) | |
| Missing | 10 (<1) | 1 (<1) | |
| Time to HCT from diagnosis, mo | 23 (<1-608) | 27 (4-281) | .03 |
| Time to HCT from diagnosis, mo | .12 | ||
| 0-12 | 316 (26) | 41 (21) | |
| 12-36 | 496 (41) | 75 (39) | |
| ≥36 | 391 (32) | 74 (39) | |
| Missing | 1 (<1) | 1 (<1) | |
| Donor-related | |||
| Donor type | .29 | ||
| HLA-identical sibling | 539 (45) | 73 (38) | |
| Well-matched unrelated | 447 (37) | 85 (45) | |
| Partially matched unrelated | 125 (10) | 21 (11) | |
| Mismatched unrelated | 9 (<1) | 2 (1) | |
| Unrelated (matching indeterminable) | 84 (7) | 10 (5) | |
| URD-recipient HLA-matching | .10 | ||
| 3 | 0 | 1 (<1) | |
| 5 | 1 (<1) | 0 | |
| 6 | 5 (<1) | 0 | |
| 7 | 101 (15) | 19 (16) | |
| 8 | 407 (61) | 79 (67) | |
| Missing | 151 (23) | 19 (16) | |
| Donor-recipient sex match | .003 | ||
| M-M | 456 (38) | 63 (33) | |
| M-F | 271 (23) | 66 (35) | |
| F-M | 264 (22) | 27 (14) | |
| F-F | 209 (17) | 34 (18) | |
| Missing | 4 (<1) | 1 (<1) | |
| Donor-recipient CMV status | .36 | ||
| +/+ | 377 (31) | 67 (35) | |
| +/− | 99 (8) | 18 (9) | |
| −/+ | 272 (23) | 47 (25) | |
| −/− | 287 (24) | 41 (21) | |
| URD age, median (range), y | 30 (18-61) | 29 (20-59) | .22 |
| URD age, y | .15 | ||
| 18-29 | 271 (41) | 59 (50) | |
| 30-39 | 137 (21) | 27 (23) | |
| 40-49 | 103 (15) | 17 (14) | |
| 50-59 | 37 (6) | 2 (2) | |
| ≥60 | 2 (<1) | 0 | |
| Missing | 115 (17) | 13 (11) | |
| Transplant related | |||
| Year of transplant | .08 | ||
| 2007-2008 | 261 (22) | 30 (16) | |
| 2009-2010 | 311 (26) | 60 (31) | |
| 2011-2012 | 302 (25) | 56 (29) | |
| 2013-2014 | 330 (27) | 45 (24) | |
| Graft type | .58 | ||
| BM | 293 (24) | 43 (23) | |
| PB | 911 (76) | 148 (77) | |
| Conditioning regimen | |||
| TBI ± Cy ± others (376; 31%) | Bu2 + Flu ± others (97; 51%) | ||
| Bu + Cy ± others (492; 41%) | Flu + Mel ± other (53; 28%) | ||
| Bu4 + Flu ± others (302; 25%) | Cy ± Flu ± TBI ± others (18; 9%) | ||
| Others (34; 3%) | TBI ± Flu ± others (11; 6%) | ||
| Others (12; 6%) | |||
| ATG/alemtuzumab | <.001 | ||
| ATG alone | 258 (21) | 72 (38) | |
| Alemtuzumab alone | 15 (1) | 18 (9) | |
| No ATG or alemtuzumab | 929 (77) | 101 (53) | |
| Missing | 2 (<1) | 0 | |
| GVHD prophylaxis | .26 | ||
| Ex vivo T-cell depletion/CD34 selection | 20 (2) | 1 (<1) | |
| TAC based | 712 (59) | 124 (65) | |
| CSA based | 414 (34) | 55 (29) | |
| Other | 53 (4) | 11 (6) | |
| Missing | 5 (<1) | 0 |
| Variable . | MAC (n = 1204) . | RIC (n = 191) . | P . |
|---|---|---|---|
| Follow-up of survivors, median (range), mo | 52 (4-102) | 60 (7-101) | |
| Number of centers | 163 | 76 | |
| Patient related | |||
| Age at transplant, median (range), y | 43 (18-60) | 51 (19-60) | <.001 |
| Age at transplant, y | <.001 | ||
| 18-29 | 212 (18) | 17 (9) | |
| 30-39 | 276 (23) | 21 (11) | |
| 40-49 | 404 (34) | 47 (25) | |
| 50-59 | 312 (26) | 106 (55) | |
| Sex | <.001 | ||
| Male | 722 (60) | 90 (47) | |
| Female | 482 (40) | 101 (53) | |
| KPS, % | <.001 | ||
| 90-100 | 845 (70) | 110 (58) | |
| <90 | 267 (22) | 72 (38) | |
| Missing | 92 (8) | 9 (5) | |
| WHO region | .60 | ||
| Africa | 1 (<1) | 0 | |
| Americas | 1054 (88) | 172 (90) | |
| Eastern Mediterranean | 22 (2) | 0 | |
| Europe | 78 (6) | 10 (5) | |
| Southeastern Asian | 21 (2) | 4 (2) | |
| Western Pacific | 27 (2) | 5 (3) | |
| Missing | 1 (<1) | 0 | |
| Sorror comorbidity index (HCT-CI) | .003 | ||
| 0 | 525 (44) | 64 (34) | |
| 1 | 132 (11) | 27 (14) | |
| 2 | 125 (10) | 25 (13) | |
| 3+ | 246 (20) | 58 (30) | |
| Missing | 176 (15) | 17 (9) | |
| Disease related | |||
| Disease status prior to transplant | .20 | ||
| CP1 | 504 (42) | 92 (48) | |
| AP | 405 (34) | 60 (31) | |
| CP2+ | 278 (23) | 38 (20) | |
| CP, NOS | 17 (1) | 1 (<1) | |
| Prior treatment | .85 | ||
| No | 9 (<1) | 1 (<1) | |
| Yes | 1185 (98) | 189 (99) | |
| Missing | 10 (<1) | 1 (<1) | |
| Use of TKI prior to HCT | .89 | ||
| No | 73 (6) | 11 (6) | |
| Yes | 1121 (93) | 179 (94) | |
| Missing | 10 (<1) | 1 (<1) | |
| TKI used pre-HCT | .11 | ||
| No TKI used | 73 (6) | 11 (6) | |
| Imatinib + dasatinib + nilotinib | 250 (21) | 52 (27) | |
| Imatinib + dasatinib | 295 (25) | 55 (29) | |
| Imatinib + nilotinib | 73 (6) | 13 (7) | |
| Dasatinib + nilotinib | 35 (3) | 8 (4) | |
| Imatinib | 395 (33) | 43 (23) | |
| Dasatinib | 52 (4) | 7 (4) | |
| Nilotinib | 21 (2) | 1 (<1) | |
| Missing | 10 (<1) | 1 (<1) | |
| Time to HCT from diagnosis, mo | 23 (<1-608) | 27 (4-281) | .03 |
| Time to HCT from diagnosis, mo | .12 | ||
| 0-12 | 316 (26) | 41 (21) | |
| 12-36 | 496 (41) | 75 (39) | |
| ≥36 | 391 (32) | 74 (39) | |
| Missing | 1 (<1) | 1 (<1) | |
| Donor-related | |||
| Donor type | .29 | ||
| HLA-identical sibling | 539 (45) | 73 (38) | |
| Well-matched unrelated | 447 (37) | 85 (45) | |
| Partially matched unrelated | 125 (10) | 21 (11) | |
| Mismatched unrelated | 9 (<1) | 2 (1) | |
| Unrelated (matching indeterminable) | 84 (7) | 10 (5) | |
| URD-recipient HLA-matching | .10 | ||
| 3 | 0 | 1 (<1) | |
| 5 | 1 (<1) | 0 | |
| 6 | 5 (<1) | 0 | |
| 7 | 101 (15) | 19 (16) | |
| 8 | 407 (61) | 79 (67) | |
| Missing | 151 (23) | 19 (16) | |
| Donor-recipient sex match | .003 | ||
| M-M | 456 (38) | 63 (33) | |
| M-F | 271 (23) | 66 (35) | |
| F-M | 264 (22) | 27 (14) | |
| F-F | 209 (17) | 34 (18) | |
| Missing | 4 (<1) | 1 (<1) | |
| Donor-recipient CMV status | .36 | ||
| +/+ | 377 (31) | 67 (35) | |
| +/− | 99 (8) | 18 (9) | |
| −/+ | 272 (23) | 47 (25) | |
| −/− | 287 (24) | 41 (21) | |
| URD age, median (range), y | 30 (18-61) | 29 (20-59) | .22 |
| URD age, y | .15 | ||
| 18-29 | 271 (41) | 59 (50) | |
| 30-39 | 137 (21) | 27 (23) | |
| 40-49 | 103 (15) | 17 (14) | |
| 50-59 | 37 (6) | 2 (2) | |
| ≥60 | 2 (<1) | 0 | |
| Missing | 115 (17) | 13 (11) | |
| Transplant related | |||
| Year of transplant | .08 | ||
| 2007-2008 | 261 (22) | 30 (16) | |
| 2009-2010 | 311 (26) | 60 (31) | |
| 2011-2012 | 302 (25) | 56 (29) | |
| 2013-2014 | 330 (27) | 45 (24) | |
| Graft type | .58 | ||
| BM | 293 (24) | 43 (23) | |
| PB | 911 (76) | 148 (77) | |
| Conditioning regimen | |||
| TBI ± Cy ± others (376; 31%) | Bu2 + Flu ± others (97; 51%) | ||
| Bu + Cy ± others (492; 41%) | Flu + Mel ± other (53; 28%) | ||
| Bu4 + Flu ± others (302; 25%) | Cy ± Flu ± TBI ± others (18; 9%) | ||
| Others (34; 3%) | TBI ± Flu ± others (11; 6%) | ||
| Others (12; 6%) | |||
| ATG/alemtuzumab | <.001 | ||
| ATG alone | 258 (21) | 72 (38) | |
| Alemtuzumab alone | 15 (1) | 18 (9) | |
| No ATG or alemtuzumab | 929 (77) | 101 (53) | |
| Missing | 2 (<1) | 0 | |
| GVHD prophylaxis | .26 | ||
| Ex vivo T-cell depletion/CD34 selection | 20 (2) | 1 (<1) | |
| TAC based | 712 (59) | 124 (65) | |
| CSA based | 414 (34) | 55 (29) | |
| Other | 53 (4) | 11 (6) | |
| Missing | 5 (<1) | 0 |
Data are presented as n (%) of patients unless otherwise indicated.
ATG, anti-thymocyte globulin; BM, bone marrow; CP, chronic phase; CSA, cyclosporine; Cy; cyclophosphamide; F, female; Flu, fludarabine; M, male; NOS, not otherwise specified; PB, peripheral blood; TAC, tacrolimus; URD; unrelated donor; WHO, World Health Organization.
Of the 596 patients categorized as CP1 at the time of allo-HCT (504 in MAC and 92 in RIC cohort) (Table 1), the indication for allo-HCT in 78% (n = 467) was failure to achieve deeper (cytogenetic and/or molecular) remission with nontransplant therapies. The indication was not available for the other 22% and is presumed to be intolerance to TKIs. A total of 465 patients were in AP at the time of allo-HCT (405 in MAC [34%] and 60 in RIC [31%]) (Table 1). A total of 230 patients (57%) in the MAC cohort and 31 patients (52%) in the RIC cohort had presented with AP or BP and achieved at least a hematologic response prior to allo-HCT. The baseline cytogenetic information (pre-HCT) was not available in the 2 cohorts given the type of data forms used for this study (Transplant Essential Data).
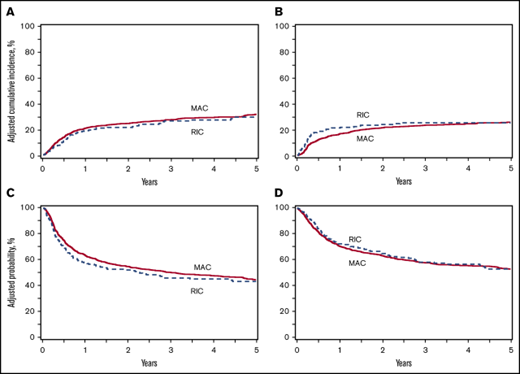
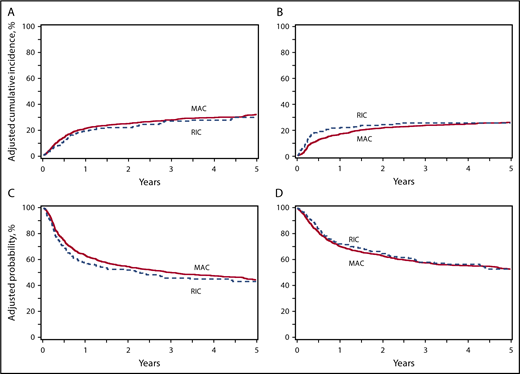
OS
On multivariable analysis, no significant difference in OS was seen between the MAC and RIC cohorts (HR, 0.99, P = .95) (Table 2; Figure 1D). The adjusted probabilities of 5-year OS were 53% (95% confidence interval [CI], 50%-56%) and 53% (95% CI, 45%-60%) for the MAC and RIC cohorts, respectively (P = .98) (Table 3). Variables associated with higher mortality included unrelated donor (matched or partially matched), CMV (donor seronegative/recipient seropositive and both donor and recipient seropositive), peripheral blood graft, and KPS <90% (Table 2). Additionally, compared with those in CP1, patients in AP (HR, 1.59; P = .0006) and CP2+ (HR, 1.18; P = .0008) had an increased risk of mortality after allo-HCT.
Multivariable analysis for patients aged 18 to 60 years undergoing allo-HCT using MAC vs RIC for CML, 2007-2014
| . | No. of patients (evaluable) . | HR . | 95% CI . | P . |
|---|---|---|---|---|
| OS | ||||
| MAC | 1204 | 1.0 | ||
| RIC | 191 | 0.99 | 0.79-1.25 | .95 |
| Disease status | .002 | |||
| CP1 | 596 | 1.0 | ||
| AP | 465 | 1.59 | 1.13-2.24 | .0006 |
| CP2+ | 316 | 1.18 | 0.85-1.63 | .0008 |
| CP, NOS | 11 | 1.96 | 0.71-5.36 | .28 |
| Missing | 7 | 0.87 | 0.63-1.20 | .17 |
| KPS | .0003 | |||
| ≥90% | 955 | 1.0 | ||
| <90% | 339 | 1.41 | 1.18-1.69 | .0002 |
| Missing | 101 | 1.08 | 0.76-1.54 | .66 |
| Graft type | .004 | |||
| BM | 336 | 1.0 | ||
| PB | 1059 | 1.36 | 1.10-1.66 | .004 |
| Donor type | .02 | |||
| HLA-identical sibling | 612 | 1.0 | ||
| Well-matched unrelated | 532 | 1.32 | 1.09-1.60 | .004 |
| Partially matched unrelated | 146 | 1.45 | 1.10-1.89 | .007 |
| Mismatched unrelated | 11 | 1.65 | 0.73-3.74 | .23 |
| URD matching TBD | 94 | 1.29 | 0.09-1.83 | .15 |
| CMV match | .03 | |||
| +/+ | 444 | 1.0 | ||
| +/− | 117 | 0.93 | 0.68-1.26 | .63 |
| −/+ | 319 | 1.11 | 0.90-1.37 | .33 |
| −/− | 328 | 0.76 | 0.60-0.95 | .02 |
| Missing | 187 | 1.04 | 0.76-1.42 | .79 |
| LFS | ||||
| MAC | 1190 | 1.0 | ||
| RIC | 191 | 1.13 | 0.92-1.39 | .29 |
| Disease status | <.0001 | |||
| CP1 | 593 | 1.0 | ||
| AP | 459 | 1.47 | 1.23-1.74 | <.0001 |
| CP2+ | 311 | 1.43 | 1.19-1.73 | .0002 |
| CP, NOS | 11 | 1.74 | 0.86-3.53 | .12 |
| Missing | 7 | 1.44 | 0.53-3.86 | .47 |
| KPS | <.0001 | |||
| ≥90% | 948 | 1.0 | ||
| <90% | 337 | 1.49 | 1.26-1.75 | <.0001 |
| Missing | 96 | 0.98 | 0.73-1.32 | .90 |
| Relapse ≤5 mo | ||||
| MAC | 1183 | 1.0 | ||
| RIC | 191 | 1.85 | 1.27-2.70 | .001 |
| Relapse >5 mo | ||||
| MAC | 922 | 1.0 | ||
| RIC | 137 | 0.64 | 0.37-1.08 | .097 |
| Disease status | <.0001 | |||
| CP1 | 593 | 1.0 | ||
| AP | 459 | 1.87 | 1.44-2.41 | <.0001 |
| CP2+ | 311 | 1.79 | 1.34-2.39 | <.0001 |
| CP, NOS | 11 | 1.58 | 0.50-5.02 | .43 |
| KPS | <.0001 | |||
| ≥90% | 944 | 1.0 | ||
| <90% | 334 | 1.81 | 1.42-2.29 | <.0001 |
| Missing | 96 | 1.06 | 0.69-1.62 | .80 |
| Donor type | .005 | |||
| HLA-identical sibling | 604 | 1.0 | ||
| Well-matched unrelated | 528 | 0.64 | 0.50-0.82 | .0004 |
| Partially matched unrelated | 143 | 0.64 | 0.43-0.95 | .03 |
| Mismatched unrelated | 10 | 0.82 | 0.20-3.33 | .78 |
| URD matching TBD | 89 | 0.75 | 0.45-1.23 | .25 |
| NRM | ||||
| MAC | 1190 | 1.0 | ||
| RIC | 191 | 1.01 | 0.76-1.34 | .97 |
| Age, y | .02 | |||
| 18-29 | 226 | 1.0 | ||
| 30-39 | 295 | 1.27 | 0.88-1.82 | .20 |
| 40-49 | 445 | 1.47 | 1.05-2.05 | .02 |
| 50-59 | 415 | 1.66 | 1.18-2.33 | .003 |
| Graft type | .02 | |||
| BM | 333 | 1.0 | ||
| PB | 1048 | 1.34 | 1.04-1.72 | .02 |
| Donor type | .0002 | |||
| HLA-identical sibling | 608 | 1.0 | ||
| Well-matched unrelated | 531 | 1.56 | 1.23-1.99 | .0003 |
| Partially matched unrelated | 143 | 1.89 | 1.28-2.53 | .0001 |
| Mismatched unrelated | 10 | 2.73 | 0.81-5.99 | .03 |
| URD matching TBD | 89 | 1.46 | 1.08-2.29 | .09 |
| CMV match | .02 | |||
| +/+ | 440 | 1.0 | ||
| +/− | 117 | 1.01 | 0.69-1.48 | .95 |
| −/+ | 316 | 1.22 | 0.94-1.58 | .13 |
| −/− | 326 | 0.74 | 0.55-0.97 | .04 |
| Missing | 182 | 0.97 | 0.67-1.39 | .85 |
| cGVHD | ||||
| MAC | 1177 | 1.0 | ||
| RIC | 187 | 0.77 | 0.61-0.97 | .02 |
| Graft type | <.0001 | |||
| BM | 327 | 1.0 | ||
| PB | 1037 | 1.75 | 1.46-2.10 | <.0001 |
| GVHD prophylaxis | .0005 | |||
| TAC | 821 | 1.0 | ||
| T-cell depletion/CD34 | 19 | 0.26 | 0.11-0.58 | .001 |
| CSA | 457 | 0.82 | 0.70-0.96 | .01 |
| Other | 64 | 0.67 | 0.46-0.99 | .04 |
| ATG/alemtuzumab | .004 | |||
| ATG alone | 319 | 1.0 | ||
| Alemtuzumab alone | 33 | 0.41 | 0.21-0.78 | .007 |
| No ATG/alemtuzumab | 1012 | 1.13 | 0.94-1.36 | .18 |
| Sex match | .007 | |||
| M-M | 508 | 1.0 | ||
| M-F | 331 | 0.91 | 0.75-1.10 | .33 |
| F-M | 284 | 1.30 | 1.08-1.58 | .006 |
| F-F | 241 | 1.06 | 0.87-1.30 | .57 |
| . | No. of patients (evaluable) . | HR . | 95% CI . | P . |
|---|---|---|---|---|
| OS | ||||
| MAC | 1204 | 1.0 | ||
| RIC | 191 | 0.99 | 0.79-1.25 | .95 |
| Disease status | .002 | |||
| CP1 | 596 | 1.0 | ||
| AP | 465 | 1.59 | 1.13-2.24 | .0006 |
| CP2+ | 316 | 1.18 | 0.85-1.63 | .0008 |
| CP, NOS | 11 | 1.96 | 0.71-5.36 | .28 |
| Missing | 7 | 0.87 | 0.63-1.20 | .17 |
| KPS | .0003 | |||
| ≥90% | 955 | 1.0 | ||
| <90% | 339 | 1.41 | 1.18-1.69 | .0002 |
| Missing | 101 | 1.08 | 0.76-1.54 | .66 |
| Graft type | .004 | |||
| BM | 336 | 1.0 | ||
| PB | 1059 | 1.36 | 1.10-1.66 | .004 |
| Donor type | .02 | |||
| HLA-identical sibling | 612 | 1.0 | ||
| Well-matched unrelated | 532 | 1.32 | 1.09-1.60 | .004 |
| Partially matched unrelated | 146 | 1.45 | 1.10-1.89 | .007 |
| Mismatched unrelated | 11 | 1.65 | 0.73-3.74 | .23 |
| URD matching TBD | 94 | 1.29 | 0.09-1.83 | .15 |
| CMV match | .03 | |||
| +/+ | 444 | 1.0 | ||
| +/− | 117 | 0.93 | 0.68-1.26 | .63 |
| −/+ | 319 | 1.11 | 0.90-1.37 | .33 |
| −/− | 328 | 0.76 | 0.60-0.95 | .02 |
| Missing | 187 | 1.04 | 0.76-1.42 | .79 |
| LFS | ||||
| MAC | 1190 | 1.0 | ||
| RIC | 191 | 1.13 | 0.92-1.39 | .29 |
| Disease status | <.0001 | |||
| CP1 | 593 | 1.0 | ||
| AP | 459 | 1.47 | 1.23-1.74 | <.0001 |
| CP2+ | 311 | 1.43 | 1.19-1.73 | .0002 |
| CP, NOS | 11 | 1.74 | 0.86-3.53 | .12 |
| Missing | 7 | 1.44 | 0.53-3.86 | .47 |
| KPS | <.0001 | |||
| ≥90% | 948 | 1.0 | ||
| <90% | 337 | 1.49 | 1.26-1.75 | <.0001 |
| Missing | 96 | 0.98 | 0.73-1.32 | .90 |
| Relapse ≤5 mo | ||||
| MAC | 1183 | 1.0 | ||
| RIC | 191 | 1.85 | 1.27-2.70 | .001 |
| Relapse >5 mo | ||||
| MAC | 922 | 1.0 | ||
| RIC | 137 | 0.64 | 0.37-1.08 | .097 |
| Disease status | <.0001 | |||
| CP1 | 593 | 1.0 | ||
| AP | 459 | 1.87 | 1.44-2.41 | <.0001 |
| CP2+ | 311 | 1.79 | 1.34-2.39 | <.0001 |
| CP, NOS | 11 | 1.58 | 0.50-5.02 | .43 |
| KPS | <.0001 | |||
| ≥90% | 944 | 1.0 | ||
| <90% | 334 | 1.81 | 1.42-2.29 | <.0001 |
| Missing | 96 | 1.06 | 0.69-1.62 | .80 |
| Donor type | .005 | |||
| HLA-identical sibling | 604 | 1.0 | ||
| Well-matched unrelated | 528 | 0.64 | 0.50-0.82 | .0004 |
| Partially matched unrelated | 143 | 0.64 | 0.43-0.95 | .03 |
| Mismatched unrelated | 10 | 0.82 | 0.20-3.33 | .78 |
| URD matching TBD | 89 | 0.75 | 0.45-1.23 | .25 |
| NRM | ||||
| MAC | 1190 | 1.0 | ||
| RIC | 191 | 1.01 | 0.76-1.34 | .97 |
| Age, y | .02 | |||
| 18-29 | 226 | 1.0 | ||
| 30-39 | 295 | 1.27 | 0.88-1.82 | .20 |
| 40-49 | 445 | 1.47 | 1.05-2.05 | .02 |
| 50-59 | 415 | 1.66 | 1.18-2.33 | .003 |
| Graft type | .02 | |||
| BM | 333 | 1.0 | ||
| PB | 1048 | 1.34 | 1.04-1.72 | .02 |
| Donor type | .0002 | |||
| HLA-identical sibling | 608 | 1.0 | ||
| Well-matched unrelated | 531 | 1.56 | 1.23-1.99 | .0003 |
| Partially matched unrelated | 143 | 1.89 | 1.28-2.53 | .0001 |
| Mismatched unrelated | 10 | 2.73 | 0.81-5.99 | .03 |
| URD matching TBD | 89 | 1.46 | 1.08-2.29 | .09 |
| CMV match | .02 | |||
| +/+ | 440 | 1.0 | ||
| +/− | 117 | 1.01 | 0.69-1.48 | .95 |
| −/+ | 316 | 1.22 | 0.94-1.58 | .13 |
| −/− | 326 | 0.74 | 0.55-0.97 | .04 |
| Missing | 182 | 0.97 | 0.67-1.39 | .85 |
| cGVHD | ||||
| MAC | 1177 | 1.0 | ||
| RIC | 187 | 0.77 | 0.61-0.97 | .02 |
| Graft type | <.0001 | |||
| BM | 327 | 1.0 | ||
| PB | 1037 | 1.75 | 1.46-2.10 | <.0001 |
| GVHD prophylaxis | .0005 | |||
| TAC | 821 | 1.0 | ||
| T-cell depletion/CD34 | 19 | 0.26 | 0.11-0.58 | .001 |
| CSA | 457 | 0.82 | 0.70-0.96 | .01 |
| Other | 64 | 0.67 | 0.46-0.99 | .04 |
| ATG/alemtuzumab | .004 | |||
| ATG alone | 319 | 1.0 | ||
| Alemtuzumab alone | 33 | 0.41 | 0.21-0.78 | .007 |
| No ATG/alemtuzumab | 1012 | 1.13 | 0.94-1.36 | .18 |
| Sex match | .007 | |||
| M-M | 508 | 1.0 | ||
| M-F | 331 | 0.91 | 0.75-1.10 | .33 |
| F-M | 284 | 1.30 | 1.08-1.58 | .006 |
| F-F | 241 | 1.06 | 0.87-1.30 | .57 |
TBD, to be determined.
Outcomes after MAC versus RIC alloHCT for CML. (A) Adjusted curves for NRM after allo-HCT for CML using MAC vs RIC. (B) Adjusted curves for disease relapse after allo-HCT for CML using MAC vs RIC. (C) Adjusted curves for LFS after allo-HCT for CML using MAC vs RIC. (D) Adjusted curves for OS after allo-HCT for CML using MAC vs RIC.
Outcomes after MAC versus RIC alloHCT for CML. (A) Adjusted curves for NRM after allo-HCT for CML using MAC vs RIC. (B) Adjusted curves for disease relapse after allo-HCT for CML using MAC vs RIC. (C) Adjusted curves for LFS after allo-HCT for CML using MAC vs RIC. (D) Adjusted curves for OS after allo-HCT for CML using MAC vs RIC.
Adjusted probabilities of outcomes in CML patients aged 18 to 60 years undergoing allo-HCT using MAC vs RIC, 2007-2014
| . | MAC (n = 1204) . | RIC (n = 191) . | . | ||
|---|---|---|---|---|---|
| Outcomes . | No. of patients (evaluable) . | Probability (95% CI), % . | No. of patients (evaluable) . | Probability (95% CI), % . | P . |
| OS, y | 1204 | 191 | |||
| 1 | 831 | 71 (68-73) | 133 | 72 (66-78) | .61 |
| 3 | 501 | 58 (55-60) | 86 | 58 (51-65) | .91 |
| 5 | 272 | 53 (50-56) | 49 | 53 (45-60) | .98 |
| LFS, y | 1190 | 191 | |||
| 1 | 731 | 63 (60-66) | 106 | 58 (51-65) | .15 |
| 3 | 423 | 50 (47-53) | 70 | 46 (39-53) | .31 |
| 5 | 222 | 44 (41-47) | 40 | 43 (36-51) | .81 |
| Relapse, y | 1190 | 191 | |||
| 1 | 731 | 16 (14-18) | 106 | 21 (16-27) | .10 |
| 3 | 423 | 23 (21-26) | 70 | 25 (19-31) | .49 |
| 5 | 222 | 26 (23-28) | 40 | 25 (19-31) | .96 |
| NRM, y | 1190 | 191 | |||
| 1 | 731 | 21 (18-23) | 106 | 19 (14-24) | .50 |
| 3 | 423 | 28 (25-30) | 70 | 26 (20-33) | .71 |
| 5 | 222 | 32 (29-35) | 40 | 29 (22-36) | .53 |
| cGVHD, y | 1182 | 188 | |||
| 1 | 316 | 50 (47-53) | 64 | 41 (33-48) | .02 |
| 3 | 122 | 58 (55-61) | 27 | 51 (43-58) | .08 |
| 5 | 57 | 59 (56-62) | 16 | 51 (44-59) | .07 |
| . | MAC (n = 1204) . | RIC (n = 191) . | . | ||
|---|---|---|---|---|---|
| Outcomes . | No. of patients (evaluable) . | Probability (95% CI), % . | No. of patients (evaluable) . | Probability (95% CI), % . | P . |
| OS, y | 1204 | 191 | |||
| 1 | 831 | 71 (68-73) | 133 | 72 (66-78) | .61 |
| 3 | 501 | 58 (55-60) | 86 | 58 (51-65) | .91 |
| 5 | 272 | 53 (50-56) | 49 | 53 (45-60) | .98 |
| LFS, y | 1190 | 191 | |||
| 1 | 731 | 63 (60-66) | 106 | 58 (51-65) | .15 |
| 3 | 423 | 50 (47-53) | 70 | 46 (39-53) | .31 |
| 5 | 222 | 44 (41-47) | 40 | 43 (36-51) | .81 |
| Relapse, y | 1190 | 191 | |||
| 1 | 731 | 16 (14-18) | 106 | 21 (16-27) | .10 |
| 3 | 423 | 23 (21-26) | 70 | 25 (19-31) | .49 |
| 5 | 222 | 26 (23-28) | 40 | 25 (19-31) | .96 |
| NRM, y | 1190 | 191 | |||
| 1 | 731 | 21 (18-23) | 106 | 19 (14-24) | .50 |
| 3 | 423 | 28 (25-30) | 70 | 26 (20-33) | .71 |
| 5 | 222 | 32 (29-35) | 40 | 29 (22-36) | .53 |
| cGVHD, y | 1182 | 188 | |||
| 1 | 316 | 50 (47-53) | 64 | 41 (33-48) | .02 |
| 3 | 122 | 58 (55-61) | 27 | 51 (43-58) | .08 |
| 5 | 57 | 59 (56-62) | 16 | 51 (44-59) | .07 |
LFS
On multivariable analysis, no significant difference was observed when comparing the MAC and RIC cohorts (HR, 1.13; P = .29) (Table 2; Figure 1C). The adjusted 5-year LFS rates for MAC and RIC were 44% (95% CI, 41%-47%) and 43% (95% CI 36%-51%), respectively (P = .81; Table 3). Variables associated with higher risk of treatment failure (inverse of LFS) included disease states of AP (HR, 1.47; P < .0001) and CP2+ (HR, 1.43; P = .0002) at allo-HCT (compared with CP1) and KPS <90% (HR, 1.49; P < .0001).
NRM and relapse
On multivariable analysis, there was no significant difference in NRM between the MAC and RIC groups (Cox regression model: HR, 1.01; P = .97; Fine-Gray model: HR, 0.92; P = .57) (Table 2; Figure 1A; supplemental Table 2). The adjusted 5-year NRM rates were 32% (95% CI, 29%-35%) and 29% (95% CI, 22%-36%) in the MAC and RIC cohorts, respectively (P = .53; Table 3). Independent of the conditioning intensity, recipient age (40-49 years: HR, 1.47; P = .02; 50-59 years: HR, 1.66; P = .003 [compared with 18-29 years age group]), donor type (matched unrelated and partially matched unrelated compared with matched sibling), CMV (donor and recipient seropositivity), and peripheral blood graft were associated with a significantly higher risk of NRM.
Multivariable analysis confirmed that the risk of relapse between the 2 cohorts was time dependent; RIC had a significantly increased risk of relapse early after allo-HCT (in the first 5 months) (HR, 1.85; P = .001), but no statistically significant difference was observed during the late (>5 months) allo-HCT course (Table 2; Figure 1B). Similar results were obtained with the Fine-Gray model (≤5 months: HR, 1.86; P = .001; >5 months: HR, 0.60; P = .06; supplemental Table 2). The adjusted cumulative incidence rates of relapse at 5 years were 26% (95% CI, 23%-28%) and 25% (95% CI, 19%-31%) for MAC and RIC, respectively (P = .96; Table 3). In addition to the conditioning intensity, disease status, KPS, and donor type affected the relapse risk. AP (HR 1.87, P < .0001) and CP2+ (HR, 1.79; P < .0001) carried an increased risk of relapse relative to CP1. Well-matched and partially matched unrelated donors and KPS ≥90% were associated with a lower relapse risk. An evaluation of the causes of death in the 2 cohorts (supplemental Table 1) did not reveal any significant differences between the cohorts; disease relapse (∼30% in both) and GVHD (29% in both) were the dominant causes of death in both cohorts.
cGVHD
Multivariable analysis showed a significantly reduced risk of cGVHD (Cox model: HR, 0.77; 95% CI, 0.61-0.97; P = .02; Fine-Gray model: HR, 0.78; P = .03) with RIC relative to MAC (Table 2; supplemental Table 2). The adjusted cumulative incidence rates of cGVHD at 1 and 5 years were 50% (95% CI, 47%-53%) and 59% (95% CI, 56%-62%) after MAC compared with 41% (95% CI, 33%-48%) and 51% (95% CI, 44%-59%) with RIC (P = .02 and .07, respectively) (Table 3). In patients without in vivo T-cell depletion, the incidence of cGVHD was not significantly different relative to those receiving ATG (HR, 1.13; P = .18) but was significantly higher compared with those receiving alemtuzumab (HR, 2.76; P = .002). Compared with ATG, alemtuzumab significantly decreased the risk of cGVHD (HR, 0.41; P = .007). In addition, female donor/male recipient had a 30% higher cGVHD risk than male donor and recipient (P = .006).
Subgroup analysis
CP2+ and AP
Multivariable analysis of a prespecified subgroup of CP2+ and AP at the time of allo-HCT was done to see if there were differences in outcomes in this group of patients with higher-risk disease (Table 4). The analysis showed that in the RIC cohort, OS (HR, 1.18; P = .26) and LFS (HR, 1.27; P = .08) were not significantly different when compared with MAC. NRM was also not affected by the conditioning intensity in this high-risk subgroup (HR, 1.32; P = .17). The risk of relapse, however, varied by the time from allo-HCT: RIC patients with CP2+/AP carried a higher risk of early relapse (HR, 2.06; P = .002) but had a relapse risk similar to MAC later (>5 months) in the course (HR, 0.46; P = .06). The cumulative incidence of cGVHD did not differ significantly between MAC and RIC (HR, 0.83; P = .26).
Multivariable analysis for patients aged 18 to 60 years in AP/CP2+ undergoing allo-HCT using MAC vs RIC for CML, 2007-2014
| . | n . | HR . | 95% CI . | P . |
|---|---|---|---|---|
| cGVHD | ||||
| MAC | 668 | 1 | ||
| RIC | 97 | 0.83 | 0.60-1.15 | .26 |
| Relapse ≤5 mo | ||||
| MAC | 672 | 1 | ||
| RIC | 98 | 2.06 | 1.31-3.23 | .002 |
| Relapse >5 mo | ||||
| MAC | 503 | 1 | ||
| RIC | 99 | 0.46 | 0.20-1.05 | .06 |
| NRM | ||||
| MAC | 672 | 1 | ||
| RIC | 98 | 1.32 | 0.89-1.94 | .17 |
| LFS | ||||
| MAC | 672 | 1 | ||
| RIC | 98 | 1.27 | 0.97-1.66 | .08 |
| OS | ||||
| MAC | 683 | 1 | ||
| RIC | 98 | 1.18 | 0.88-1.57 | .26 |
| . | n . | HR . | 95% CI . | P . |
|---|---|---|---|---|
| cGVHD | ||||
| MAC | 668 | 1 | ||
| RIC | 97 | 0.83 | 0.60-1.15 | .26 |
| Relapse ≤5 mo | ||||
| MAC | 672 | 1 | ||
| RIC | 98 | 2.06 | 1.31-3.23 | .002 |
| Relapse >5 mo | ||||
| MAC | 503 | 1 | ||
| RIC | 99 | 0.46 | 0.20-1.05 | .06 |
| NRM | ||||
| MAC | 672 | 1 | ||
| RIC | 98 | 1.32 | 0.89-1.94 | .17 |
| LFS | ||||
| MAC | 672 | 1 | ||
| RIC | 98 | 1.27 | 0.97-1.66 | .08 |
| OS | ||||
| MAC | 683 | 1 | ||
| RIC | 98 | 1.18 | 0.88-1.57 | .26 |
Discussion
Although allogeneic transplantation is no longer a first-line treatment of CML in CP1 in the United States, many patients who are resistant to or intolerant of TKIs continue to require it.2,30 The European Leukemia Network, in addition, recommends allo-HCT for all patients with AP or BP at diagnosis.2 Since the approval of the TKI imatinib mesylate in 2001 based on the phase 3 IRIS study,31,32 the great majority of CML patients undergo allo-HCT later in their course. Nonetheless, the question about the optimal allogeneic transplant conditioning regimen intensity for CML is relevant and has been addressed for the first time in this observational study. Our data illustrate that in the era of TKIs, RIC is an appropriate alternative to MAC for CML patients given the equivalent survival.
Studies have shown that RIC allo-HCT for CML patients can prolong survival with acceptable NRM. A retrospective study by Crawley et al reported the outcomes after RIC allo-HCT and demonstrated its feasibility in 186 CML patients.11 The median age of patients was 50 years; 64% patients were in CP1, 13% in CP2, 17% in AP, and 6% in BP. OS and progression-free survival at 3 years were 58% and 37%, respectively. Warlick et al described outcomes in 306 CML patients of age ≥40 years undergoing RIC allo-HCT and reported to CIBMTR.12 Of these, 38% patients were aged 40 to 49 years, 39% were 50 to 59 years, and 23% were ≥60 years. The 3-year OS (54%, 52%, and 41%) and 1-year NRM (18%, 20%, and 13%) were similar across age groups. LFS and relapse were similar across age groups in CP1 patients.
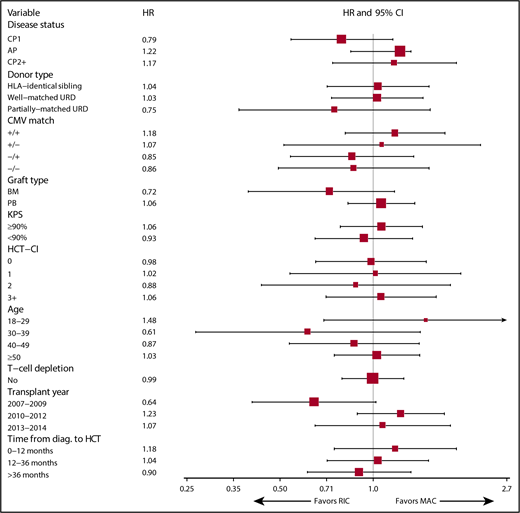
Our study makes several important observations. Patients with AP and CP2+ at allo-HCT had higher mortality compared with those in CP1, which could be explained by the advanced disease outstripping the ensuing graft-versus-leukemia effect early in the course. In addition, LFS did not differ significantly between the 2 conditioning intensities. The analysis also failed to show any difference in NRM between the 2 cohorts. RIC was associated with 85% greater risk of early after allo-HCT relapse but did not have a statistically significant difference beyond 5 months after allo-HCT. The higher early relapse risk with RIC allo-HCT could be explained by the modest cytoreduction engendered by the conditioning, enabling early relapse. However, the increased early relapse risk in the RIC cohort did not translate into worse OS due to potentially successful salvage treatment with TKIs and/or donor lymphocyte infusion (DLI) in those relapsing. Furthermore, in multivariable analysis, adjusting for many factors, including in vivo T-cell depletion, the cumulative incidence of cGVHD was notably lower in the RIC cohort than the MAC cohort in the first year after allo-HCT but lost statistical significance by 3 years. We can speculate that the use of nonmyeloablative (18%) and reduced-intensity conditioning (82%) may be associated with lower incidence of cGVHD, through potentially less tissue injury and cytokine release compared with MAC, as was also reported in BMT CTN 0901 study,13 although the strength of evidence in support of this argument would be considered weak based on other published studies.33-37 It is also possible that a higher frequency of TKI use after RIC allo-HCT for treatment or prevention of CML relapse may have curbed the cGVHD risk.38-40 In multivariable analysis, no significant interaction was found between conditioning intensity and disease status at the time of allo-HCT. The survival outcomes in patients who were in AP or CP2+ at allo-HCT were not significantly different between the conditioning cohorts. Furthermore, no significant interaction was detected between conditioning intensity and other covariates such as age, KPS, HCT-CI, donor type, donor–recipient CMV status, graft source, in vivo T-cell depletion, year of HCT, and time from diagnosis to HCT; this has been demonstrated in a forest plot (Figure 2).
Prespecified subgroup analysis according to baseline characteristics showing HRs and 95% CIs for OS after allo-HCT for CML patients using MAC vs RIC, 2007-2014.
Prespecified subgroup analysis according to baseline characteristics showing HRs and 95% CIs for OS after allo-HCT for CML patients using MAC vs RIC, 2007-2014.
This observational study has limitations. The major limitation of this analysis is that the information on CML therapies (including TKIs and DLI) used after HCT was not available. The use of TKIs as maintenance therapy or for treatment of relapse/progression of CML and of DLI preemptively or for salvage, thereby preventing relapse and/or improving OS in relapsed CML patients in the RIC cohort, is certainly within the realm of possibility. Having 5 Food and Drug Administration–approved TKIs in the United States by 2012 suggests that the great majority of study patients had a decent probability of access to effective TKIs after HCT, and not having that data is a serious limitation. Nonetheless, the study aimed at evaluating the impact of conditioning intensity on allo-HCT outcomes and did not intend to examine the role of prophylactic or maintenance after allo-HCT TKIs. Even though centers have been employing maintenance TKIs,41-44 a recent CIBMTR study demonstrated no significant impact of maintenance TKI therapy on risk of cGVHD, NRM, relapse, LFS, and OS following allo-HCT in CML patients.45 Patients who underwent MAC and RIC alloHCT between 2007 and 2014, and received TKI pre-HCT were included in that study. A landmark analysis was performed at day 100 after HCT. A total of 390 patients were included in the analysis (TKI maintenance, n = 89; no TKI maintenance, n = 301). A major proportion of both cohorts underwent MAC allo-HCT (85% in TKI cohort and 83% in no TKI cohort). With so few RIC patients, the study findings cannot be interpreted as lack of evidence in favor of maintenance TKIs after RIC allo-HCT as a relapse risk-reduction strategy.
An additional caveat of the study is that information on the depth of response prior to allo-HCT (ie, cytogenetic and/or molecular response to therapy) was not available. Having this useful data may further enable demonstration of the impact of the depth of response on outcomes and interaction with conditioning intensity and therefore, may theoretically play a role in the conditioning selection process. In addition, a potential demerit of the study is that the conditioning intensity (MAC vs RIC) selection criteria were not known; we can speculate that the treating physician made the decision to use a specific conditioning regimen based on certain clinical variables, the prevalent institutional guidelines, and the available clinical trials. The only way to prevent the selection bias would be to conduct a prospective randomized study. We tried to adjust for confounding caused by the different variables by taking them into account in the multivariable analysis, but the possibility of residual confounding remains. Finally, we analyzed the data in patients who underwent the allo-HCT but could not ascertain the justification for it in all patients. We can safely assume that the decision to proceed to allo-HCT was appropriate in those who were diagnosed with CML in AP or BP, but the reason for allo-HCT in others is not apparent in the data forms.
In summary, the current study represents the comparison of CML patients undergoing MAC and RIC allo-HCT in the era of TKIs and supports the notion that RIC allo-HCT is an appropriate alternative to MAC for CML. However, the lack of difference in OS between the MAC and RIC allo-HCT in the analysis is not to be construed as an argument in favor of selecting RIC over MAC for CML patients. On the contrary, the analysis revealed that compared with MAC, RIC allo-HCT afforded similar survival, albeit at the expense of increased early post–allo-HCT relapse risk. It is paramount to recognize that the intent of the study was not to identify a superior conditioning intensity between MAC and RIC but to demonstrate that OS and LFS in CML patients who are unable to proceed to MAC allo-HCT on clinical grounds are similar, should they receive RIC allo-HCT. Examining the interactions between conditioning intensity and several clinical variables did not suggest any advantage for RIC over MAC or vice versa to help make a recommendation on selection of conditioning intensity in CML patient subgroups based on these clinical variables. To conclude, this study is significant in light of the fact that a confirmation of the findings through a prospective randomized controlled trial is not likely to be attempted in the current times, where patients have access to an increasing number of potent TKIs and there is a possibility of long-term remission with treatment-free intervals and, consequently, fewer patients in need of allo-HCT.
Presented orally at the 59th annual meeting of the American Society of Hematology, Atlanta, GA, 11 December 2017.
The full-text version of this article contains a data supplement.
Acknowledgments
The CIBMTR is supported primarily by the National Institutes of Health (public health service grant/cooperative agreement 5U24CA076518 from the National Cancer Institute, National Heart, Lung, and Blood Institute, and National Institute of Allergy and Infectious Diseases and grant/cooperative agreement 4U10HL069294 from the National Heart, Lung, and Blood Institute and National Cancer Institute), the Health Resources and Services Administration/Department of Health and Human Services (contract HHSH250201200016C), and the Office of Naval Research (grants N00014-17-1-2388 and N0014-17-1-2850). The CIBMTR is also supported by Actinium Pharmaceuticals, Amgen, Amneal Biosciences, Angiocrine Bioscience, and anonymous donation to the Medical College of Wisconsin, Astellas Pharma US, Atara Biotherapeutics, Be the Match Foundation; bluebird bio, Bristol Myers Squibb Oncology, Celgene Corporation, Cerus Corporation; Chimerix, the Fred Hutchinson Cancer Research Center, Gamida Cell, Gilead Sciences, HistoGenetics, Immucor, Incyte Corporation, Janssen Scientific Affairs, Jazz Pharmaceuticals, Juno Therapeutics, Karyopharm Therapeutics, Kite Pharma, Medac, MedImmune, The Medical College of Wisconsin, Mediware, Merck & Co, Mesoblast, MesoScale Diagnostics, Millennium, Miltenyi Biotec, the National Marrow Donor Program, Neovii Biotech NA, Novartis Pharmaceuticals Corporation, Otsuka Pharmaceutical (Japan), Patient-Centered Outcomes Research Institute, Pfizer, Pharmacyclics, PIRCHE, Sanofi Genzyme, Seattle Genetics, Shire, Spectrum Pharmaceuticals, St. Baldrick’s Foundation, Sunesis Pharmaceuticals, Swedish Orphan Biovitrum, Takeda Oncology, Telomere Diagnostics, and the University of Minnesota.
The views expressed in this article do not reflect the official policy or position of the National Institutes of Health, Department of the Navy, Department of Defense, Health Resources and Services Administration, or any other agency of the US Government.
Authorship
Contribution: S.C., K.W.A., Z.-H.H., S.J., and W.S. designed research; K.W.A. and Z.-H.H. collected data and performed statistical analysis; S.C., K.W.A., Z.H.H., S.J., and W.S. interpreted data; S.C. drafted the manuscript; and K.W.A., Z.-H.H., S.J., A.A., J.C., E.A.C., A.D., Z.D., S.M.G., R.P.G., S.G., B.K.H., G.C.H., J.W.H., Y.I., A.S.K., H.J.K., H.M.L., M.R.L., S.N., R.F.O., A.P., O.R., J.M.R., A.S., B.N.S., H.C.S., S.S., N.N.S., M.S., R.K.S., C.U., A.E.W., J.A.Y., E.P.A., M.E.K., U.P., R.M.S., and W.S. critically reviewed and revised the manuscript.
Conflict-of-interest disclosure: A.A. has advisory board engagements with Boston Biomedical and Incyte Corporation. The remaining authors declare no competing financial interests.
Correspondence: Saurabh Chhabra, Division of Hematology/Oncology, Department of Medicine, Medical College of Wisconsin, 9200 W Wisconsin Ave, Milwaukee, WI 53226; e-mail: schhabra@mcw.edu.