Key Points
Ide-cel CAR-T for RRMM is associated with a cardiac event profile similar to that of anti-CD19 CAR-T.
Worse baseline functional status and higher-grade CRS and neurotoxicity are associated with cardiac events after ide-cel CAR-T.
Abstract
Idecabtagene vicleucel (ide-cel) is a type of B-cell maturation antigen (BCMA)–targeting chimeric antigen receptor T-cell (CAR-T) approved for the treatment of relapsed and refractory multiple myeloma (RRMM). Currently, the incidence of cardiac events associated with ide-cel remains unclear. This was a retrospective single-center observational study of patients treated with ide-cel for RRMM. We included all consecutive patients who received standard-of-care ide-cel treatment at least 1-month follow-up. Baseline clinical risk factors, safety profile, and responses were examined based on the development of a cardiac event. A total of 78 patients were treated with ide-cel, and 11 patients (14.1%) developed cardiac events: heart failure (5.1%), atrial fibrillation (10.3%), nonsustained ventricular tachycardia (3.8%), and cardiovascular death (1.3%). Only 11 of the 78 patients had repeat echocardiogram. Baseline risk factors associated with the development of cardiac events included being female sex and having poor performance status, λ light-chain disease, and advanced Revised International Staging System stage. Baseline cardiac characteristics were not associated with cardiac events. During index hospitalization after CAR-T, higher-grade (≥grade 2) cytokine release syndrome (CRS) and immune cell–associated neurologic syndrome were associated with cardiac events. In multivariable analyses, the hazard ratio for the association of the presence of cardiac events with overall survival (OS) was 2.66 and progression-free survival (PFS) was 1.98. Ide-cel CAR-T for RRMM was associated with similar cardiac events as other types of CAR-T. Worse baseline performance status and higher-grade CRS and neurotoxicity were associated with cardiac events after BCMA-directed CAR-T-cell therapy. Our results suggest that the presence of cardiac events may confer worse PFS or OS; although because of the small sample size, the power to detect an association was limited.
Introduction
Chimeric antigen receptor T-cell (CAR-T) is a cell-based treatment approved for various malignancies, including lymphoma and relapsed/refractory multiple myeloma (RRMM).1-5 Cardiac events have been common (5%-20%) after anti-CD 19 CAR-T,6-8 and risk factors include baseline cardiac disease, baseline creatinine, type of CAR-T, and high-grade cytokine release syndrome (CRS).6-11 Surprisingly, prior anthracycline use or chest radiation therapy exposure have not been associated with increased risk for cardiac events after anti-CD19 CAR-T.12
Idecabtagene vicleucel (ide-cel) is an autologous B-cell maturation antigen (BCMA)–directed CAR-T.2,13 Based on the results of the pivotal phase 2 KarMMa trial, ide-cel was approved by the FDA in March 2021 for the treatment of RRMM after at least 4 prior lines of therapy.2,13 MM treatment includes various potential cardiotoxic agents, most commonly carfilzomib, a proteasome inhibitor.14 It is possible that patients with prior multiple lines of potentially cardiotoxic treatment are at a higher risk for cardiac events after anti-BCMA CAR-T. There is a paucity of data regarding cardiac events after anti-BCMA CAR-T. The purpose of this study was to assess the incidence and risk factors for cardiac events among patients with RRMM after standard of care (SOC) ide-cel administration.
Methods
Study population
This was a retrospective, single-center, observational study of patients with RRMM treated with ide-cel at a National Cancer Institute-Designated Comprehensive Cancer Center (H. Lee Moffitt Cancer Center & Research Institute). All consecutive patients with RRMM who underwent SOC anti-BCMA CAR-T therapy with ide-cel from May 2021 to October 2022 were included. This study was approved by the institutional review board of University of South Florida (Pro00029257) and Moffitt Cancer Center (Advarra Pro00046602). The study was conducted in accordance with the Declaration of Helsinki.
Clinical assessment
After leukapheresis, lymphodepletion chemotherapy was administered on days −5, −4, and −3 before CAR-T infusion. Routine baseline cardiac workup before CAR-T was performed on all patients, and it included an electrocardiogram, transthoracic echocardiogram, troponin-I (reference <0.03 ng/mL), and B-type natriuretic peptide (BNP; reference <100 pg/mL). CRS and immune cell–associated neurologic syndrome (ICANS) grading were based on published guidelines by the American Society for Transplantation and Cellular Therapy criteria, whereas hematologic toxicity was based on the Common Terminology Criteria for Adverse Events version 5.0.15,16 Responses were assessed based on the International Myeloma Working Group criteria.17 Repeat echocardiograms were performed when clinical suspicion for cardiac events occurred, based on the clinicians’ discretion as suggested by ESC guideline on Cardio-Oncology.18 Arrhythmia was detected through abnormality of heart rate upon routine vital sign checks or when a patient was symptomatic.
Data collection
We retrospectively reviewed patients’ electronic medical records for baseline RRMM-related and cardiovascular system–related characteristics and index hospitalization, laboratory, and diagnostic data. Standardized clinical echocardiography reports were extracted. Left ventricle (LV) ejection fraction (LVEF) was calculated through the method-of-disk. Left atrial (LA) volume was also calculated through the method-of-disk and indexed to the body surface area. Cancer therapy–related cardiac dysfunction (CTRCD) was categorized as a new LVEF decrease to <40% (severe asymptomatic), a new LVEF decrease from >10% to an LVEF of <50% (moderate asymptomatic), or LVEF ≥50% and an increase in cardiac biomarker (mild asymptomatic) or symptomatic CTRCD, as suggested by 2022 European Society of Cardiology (ESC) Guideline on Cardio-Oncology.18 The primary outcome of the study was the incidence of cardiac events, defined as CTRCD, tachyarrhythmia (atrial fibrillation/flutter, ventricular tachycardia), bradyarrhythmia (second degree or higher atrio-ventricular block), acute coronary syndrome, or cardiovascular death. Cardiac events were captured from ide-cel infusion until the present, including follow-up outpatient visits. All cardiac imaging modalities and clinical events were reviewed and confirmed by Cardio-oncologists.
Statistical analysis
Data were managed using Research Electronic Data Capture hosted at Moffitt Cancer Center.19 Continuous variables were presented as mean ± standard deviation (SD) or median with interquartile range, depending on the Shapiro-Wilk normality test. The distribution of baseline patient characteristics and safety profiles were examined based on the presence of cardiac events using parametric Student t test, analysis of variance, or nonparametric comparisons for continuous variables and χ2 tests for categorical variables. Overall survival (OS) was calculated as the time between the date of infusion of CAR-T and the date of death from any cause or the date of last contact. Progression-free survival (PFS) was calculated as the time between the date of CAR-T infusion and the date of progression, death, or last contact. Kaplan-Meier survival analysis and log-rank tests were performed to compare OS and PFS based on cardiotoxicity. Cox proportional hazard regression models were used to estimate hazard ratios and 95% confidence intervals (95% CIs) for the association between cardiac events and OS and PFS while adjusting for covariates previously identified as associated with CAR-T outcomes in RRMM.20 Two-tailed P ≤ .05 was considered statistically significant. Statistical analysis was performed using R Software version 4.1.2.21
Results
Baseline patient demographics
A total of 78 patients were included in the analysis. Baseline demographics are summarized in Table 1. The mean age of all cohort was 64 years (SD, 8.7). The percentage of male patients was 59%. White was the predominant race (74.4%), followed by Black race (15.4%) and others (10.3%). Most patients had a good baseline functional status, as assessed by Eastern Cooperative Oncology Group performance status (ECOG) of 0 or 1 (85.9%).
Overall baseline patient characteristics and based on cardiac events
| . | Total cohort (N = 78) . | No cardiac events (N = 67) . | Cardiac events (N = 11) . | P value . |
|---|---|---|---|---|
| Age at CAR-T | 64.1 ± 8.7 | 63.7 ± 8.5 | 67.0 ± 9.7 | .243 |
| Sex | .048 | |||
| Male | 46 (59.0%) | 43 (64.2%) | 3 (27.3%) | |
| Female | 32 (41.0%) | 24 (35.8%) | 8 (72.7%) | |
| Ethnicity | .053 | |||
| White | 58 (74.4%) | 53 (79.1%) | 5 (45.5%) | |
| Black | 12 (15.4%) | 8 (11.9%) | 4 (36.4%) | |
| Other | 8 (10.3%) | 6 (9.0%) | 2 (18.2%) | |
| Baseline ECOG | < .001 | |||
| 0 | 26 (33.3%) | 24 (35.8%) | 2 (18.2%) | |
| 1 | 41 (52.6%) | 38 (56.7%) | 3 (27.3%) | |
| 2 | 7 (9.0%) | 3 (4.5%) | 4 (36.4%) | |
| 3 | 3 (3.8%) | 1 (1.5%) | 2 (18.2%) | |
| 4 | 1 (1.3%) | 1 (1.5%) | 0 (0.0%) | |
| Body surface area (m2) | 2.0 (1.7-2.1) | 1.9 ± 0.2 | 1.8 ± 0.4 | .415 |
| Heart rate (bpm) | 85.0 (75.0-96.0) | 84.0 (74.5-94.5) | 95.0 (80.5-100.0) | .153 |
| Systolic BP (mmHg) | 122.0 ± 17.4 | 122.3 ± 17.1 | 120.7 ± 19.5 | .789 |
| Diastolic BP (mmHg) | 75.2 ± 9.5 | 75.7 ± 9.1 | 71.9 ± 11.2 | .221 |
| White blood cell (×1000/μL) | 3.9 (2.9-5.2) | 4.0 (3.1-5.2) | 3.5 (2.8-4.7) | .409 |
| Hemoglobin (g/dL) | 10.1 (9.2-11.2) | 10.0 (9.1-11.2) | 10.2 (9.5-10.8) | .954 |
| Platelet (×1000/μL) | 137.0 (90.0-189.0) | 147.8 ± 73.9 | 112.0 ± 66.5 | .136 |
| Creatinine (mg/dL) | 0.9 (0.7-1.1) | 0.9 (0.7-1.1) | 0.9 (0.6-1.4) | .789 |
| . | Total cohort (N = 78) . | No cardiac events (N = 67) . | Cardiac events (N = 11) . | P value . |
|---|---|---|---|---|
| Age at CAR-T | 64.1 ± 8.7 | 63.7 ± 8.5 | 67.0 ± 9.7 | .243 |
| Sex | .048 | |||
| Male | 46 (59.0%) | 43 (64.2%) | 3 (27.3%) | |
| Female | 32 (41.0%) | 24 (35.8%) | 8 (72.7%) | |
| Ethnicity | .053 | |||
| White | 58 (74.4%) | 53 (79.1%) | 5 (45.5%) | |
| Black | 12 (15.4%) | 8 (11.9%) | 4 (36.4%) | |
| Other | 8 (10.3%) | 6 (9.0%) | 2 (18.2%) | |
| Baseline ECOG | < .001 | |||
| 0 | 26 (33.3%) | 24 (35.8%) | 2 (18.2%) | |
| 1 | 41 (52.6%) | 38 (56.7%) | 3 (27.3%) | |
| 2 | 7 (9.0%) | 3 (4.5%) | 4 (36.4%) | |
| 3 | 3 (3.8%) | 1 (1.5%) | 2 (18.2%) | |
| 4 | 1 (1.3%) | 1 (1.5%) | 0 (0.0%) | |
| Body surface area (m2) | 2.0 (1.7-2.1) | 1.9 ± 0.2 | 1.8 ± 0.4 | .415 |
| Heart rate (bpm) | 85.0 (75.0-96.0) | 84.0 (74.5-94.5) | 95.0 (80.5-100.0) | .153 |
| Systolic BP (mmHg) | 122.0 ± 17.4 | 122.3 ± 17.1 | 120.7 ± 19.5 | .789 |
| Diastolic BP (mmHg) | 75.2 ± 9.5 | 75.7 ± 9.1 | 71.9 ± 11.2 | .221 |
| White blood cell (×1000/μL) | 3.9 (2.9-5.2) | 4.0 (3.1-5.2) | 3.5 (2.8-4.7) | .409 |
| Hemoglobin (g/dL) | 10.1 (9.2-11.2) | 10.0 (9.1-11.2) | 10.2 (9.5-10.8) | .954 |
| Platelet (×1000/μL) | 137.0 (90.0-189.0) | 147.8 ± 73.9 | 112.0 ± 66.5 | .136 |
| Creatinine (mg/dL) | 0.9 (0.7-1.1) | 0.9 (0.7-1.1) | 0.9 (0.6-1.4) | .789 |
All values are at the time of baseline lymphodepletion.
Data are presented as mean ± SD, median (interquartile range), or number (percentage), depending on the type of data.
P < .05 is bolded.
BP, blood pressure; bpm, beats per minute.
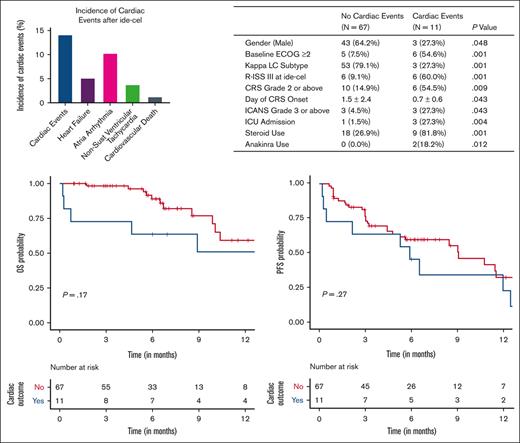
Incidence of cardiac events
There were 11 patients (14.1%) who developed cardiac events, including 4 patients with CTRCD (5.1%), 8 with atrial fibrillation/flutter (10.3%), 3 with nonsustained ventricular tachycardia (NSVT; 3.8%), and 1 cardiovascular death (1.3%). Some patients had >1 type of cardiac event. Two out of the 4 patients with CTRCD had atrial arrhythmia and/or NSVT. One patient developed symptomatic heart failure (follow-up LVEF of 45%) and later progressed to death from ICANS, pneumonia, and other multiorgan failure. Eleven patients underwent repeat transthoracic echocardiography after ide-cel (median 7 days after CAR-T infusion). Eight patients did not have a decrease in LVEF. Among the 3 who did develop a decrease in LVEF, the mean LVEF decrease was 17%. Two patients had severe CTRCD (LVEF decrease of 20% to LVEF of 30% and LVEF of 40%, each). One patient had moderate CTRCD (LVEF decrease of 12% to LVEF of 45%). One patient had mild asymptomatic CTRCD with a follow-up LVEF of 65% but with a troponin-I level of 2.1 ng/mL and cardiac magnetic resonance imaging (MRI) with mild myocardial edema in the LV. Of the 8 patients who developed atrial arrhythmia, 7 patients did not have a history of atrial arrhythmia. One patient with a history of preexisting atrial arrhythmia developed NSVT and heart failure. There were no patients with acute coronary syndrome. All events occurred ranging from 0 to 13 days after CAR-T infusion, with a median of 2 days after maximum grade CRS. Patients who had atrial fibrillation were not treated with anticoagulation because of either low CHA2DS2-VASc score or contraindication to anticoagulation (thrombocytopenia, clinically significant bleeding, or multiorgan failure). The median day of follow-up echocardiogram was 7 days after ide-cel infusion (range, 2-83 days).
Baseline patient demographic differences in cardiac events
The mean age was 64 years (range, 41-83 years; SD, 7). Age was not associated with the development of cardiac events. Female sex (72.7% vs 35.8%; P = .048) and poor baseline performance status (ECOG > 1; 54.6% vs 7.5%; P < .001) were more common in patients who developed cardiac events than those who did not develop cardiac events. In addition, people of Black race, compared with White race, had an increased incidence of cardiac events, although not statistically significant (36.4% vs 11.9%, respectively; P = .053). Age, baseline blood counts, renal function, and vital signs were similar between those who did and did not develop cardiac events.
Baseline RRMM characteristic differences in cardiac events
The baseline characteristics of RRMM are summarized in Table 2. Light-chain disease had a higher incidence of cardiac events than intact immunoglobulin disease, although not statistically significant (45.5% vs 19.4%; P = .13). More specifically, λ light-chain subtype disease was more common in patients who developed cardiac events than κ light-chain disease (72.7% vs 20.9%; P = .001). Furthermore, patients with higher Revised International Staging System stages of RRMM were more likely to develop cardiac events than those who did not develop cardiac events (60.0% vs 9.1%; P = .001). The presence of amyloid light-chain (AL) cardiac amyloidosis was uncommon (n = 1), and this patient did not develop any cardiac toxicity. In addition, t(11;14) in bone marrow fluorescence in situ hybridization, the most common cytogenetic abnormality in AL amyloidosis and a standard risk cytogenetic feature, was not associated with an increased risk of cardiac events. The heterogeneity of t(11;14) expressed in bone marrow biopsy specimen, as assessed based on the percentage of cells expressing immunoglobulin heavy chain/CCDN1, was similar between those who did and those who did not develop cardiac events (median for both, 0%; range, 0%-90% in cardiac event group; range, 0%-99% in no cardiac event group). There were no patients with features of AL amyloidosis, including significant albuminuria (+3 grams per day) or liver dysfunction. With the exception of 1 patient, all were previously exposed to carfilzomib (98.7%), which has known cardiotoxicity. There was no difference between the number of lines of therapy before ide-cel between those who did and those who did not develop cardiac events (median, 6.0 vs 6.0, respectively; P = .715). Baseline ferritin levels were higher in patients who developed cardiac events than those who did not develop cardiac events (median, 730 vs 327 ng/mL; P = .028).
Multiple myeloma baseline characteristics based on cardiac events
| . | No cardiac events (N = 67) . | Cardiac events (N = 11) . | P value . |
|---|---|---|---|
| Multiple myeloma subtype | .13 | ||
| Intact immunoglobulin disease | 54 (80.6%) | 6 (54.5%) | |
| Light-chain disease | 13 (19.4%) | 5 (45.5%) | |
| All multiple myeloma LC subtype | .001 | ||
| κ | 53 (79.1%) | 3 (27.3%) | |
| λ | 14 (20.9%) | 8 (72.7%) | |
| Light-chain disease LC subtype | .769 | ||
| κ | 8 (61.5%) | 2 (40.0%) | |
| λ | 5 (38.5%) | 3 (60.0%) | |
| Concomitant amyloidosis | 1 (1.5%) | 0 (0.0%) | 1 |
| High-risk cytogenetics | 17 (25.4%) | 5 (45.5%) | .312 |
| t(11,14) in BM FISH | 4 (6.0%) | 1 (9.1%) | 1 |
| IgH/CCDN1 percentage (t(11;14)) | 0.0 (0.0-0.0) | 0.0 (0.0-34.0) | .141 |
| High BM burden | 20 (29.9%) | 6 (54.5%) | .206 |
| R-ISS stage at CAR-T infusion | < .001 | ||
| I | 16 (24.2%) | 2 (20.0%) | |
| II | 44 (66.7%) | 2 (20.0%) | |
| III | 6 (9.1%) | 6 (60.0%) | |
| Extramedullary disease | 29 (43.3%) | 8 (72.7%) | .137 |
| Prior line of therapy | 6.2±2.4 | 6.0±1.4 | .795 |
| Last dose of carfilzomib (d) | 561.0 ± 566.4 | 401.9 ± 444.9 | .379 |
| Prior autologous HSCT | 53 (79.1%) | 9 (81.8%) | 1 |
| Bridging therapy | 37 (55.2%) | 8 (80.0%) | .255 |
| Prior anti BCMA exposure | 10 (15.4%) | 0 (0.0%) | .361 |
| Refractory status | .021 | ||
| Double refractory | 2 (3.0%) | 3 (27.3%) | |
| Triple refractory | 36 (53.7%) | 4 (36.4%) | |
| Penta refractory | 26 (38.8%) | 4 (36.4%) | |
| Κ LC value (mg/dL) | 76.0 (10.7-446.3) | 1.8 (1.4-12.1) | .013 |
| Λ LC value (mg/dL) | 2.9 (1.6-12.5) | 1048.4 (2.3-1553.2) | .023 |
| Serum M spike value (g/dL) | 0.6 (0.2-1.6) | 0.4 (0.0-2.8) | .657 |
| Baseline ferritin (ng/mL) | 327.0 (90.0-830.5) | 730.0 (502.0-3575.0) | .028 |
| Baseline CRP (μg/mL) | 0.8 (0.2-3.3) | 0.9 (0.7-3.9) | .455 |
| Fluid overload post lymphodepletion | 6 (9.0%) | 2 (18.2%) | .690 |
| . | No cardiac events (N = 67) . | Cardiac events (N = 11) . | P value . |
|---|---|---|---|
| Multiple myeloma subtype | .13 | ||
| Intact immunoglobulin disease | 54 (80.6%) | 6 (54.5%) | |
| Light-chain disease | 13 (19.4%) | 5 (45.5%) | |
| All multiple myeloma LC subtype | .001 | ||
| κ | 53 (79.1%) | 3 (27.3%) | |
| λ | 14 (20.9%) | 8 (72.7%) | |
| Light-chain disease LC subtype | .769 | ||
| κ | 8 (61.5%) | 2 (40.0%) | |
| λ | 5 (38.5%) | 3 (60.0%) | |
| Concomitant amyloidosis | 1 (1.5%) | 0 (0.0%) | 1 |
| High-risk cytogenetics | 17 (25.4%) | 5 (45.5%) | .312 |
| t(11,14) in BM FISH | 4 (6.0%) | 1 (9.1%) | 1 |
| IgH/CCDN1 percentage (t(11;14)) | 0.0 (0.0-0.0) | 0.0 (0.0-34.0) | .141 |
| High BM burden | 20 (29.9%) | 6 (54.5%) | .206 |
| R-ISS stage at CAR-T infusion | < .001 | ||
| I | 16 (24.2%) | 2 (20.0%) | |
| II | 44 (66.7%) | 2 (20.0%) | |
| III | 6 (9.1%) | 6 (60.0%) | |
| Extramedullary disease | 29 (43.3%) | 8 (72.7%) | .137 |
| Prior line of therapy | 6.2±2.4 | 6.0±1.4 | .795 |
| Last dose of carfilzomib (d) | 561.0 ± 566.4 | 401.9 ± 444.9 | .379 |
| Prior autologous HSCT | 53 (79.1%) | 9 (81.8%) | 1 |
| Bridging therapy | 37 (55.2%) | 8 (80.0%) | .255 |
| Prior anti BCMA exposure | 10 (15.4%) | 0 (0.0%) | .361 |
| Refractory status | .021 | ||
| Double refractory | 2 (3.0%) | 3 (27.3%) | |
| Triple refractory | 36 (53.7%) | 4 (36.4%) | |
| Penta refractory | 26 (38.8%) | 4 (36.4%) | |
| Κ LC value (mg/dL) | 76.0 (10.7-446.3) | 1.8 (1.4-12.1) | .013 |
| Λ LC value (mg/dL) | 2.9 (1.6-12.5) | 1048.4 (2.3-1553.2) | .023 |
| Serum M spike value (g/dL) | 0.6 (0.2-1.6) | 0.4 (0.0-2.8) | .657 |
| Baseline ferritin (ng/mL) | 327.0 (90.0-830.5) | 730.0 (502.0-3575.0) | .028 |
| Baseline CRP (μg/mL) | 0.8 (0.2-3.3) | 0.9 (0.7-3.9) | .455 |
| Fluid overload post lymphodepletion | 6 (9.0%) | 2 (18.2%) | .690 |
Data are presented as mean ± SD, median (interquartile range), or number (percentage), depending on the type of data.
P < .05 is bolded.
High-risk cytogenetics when any of following cytogenetics are present: del(17p), t(4;14) or t(14;16).
High BM burden was defined as ≥ 50% CD138-positive plasma cells in baseline ide-cel bone marrow core biopsy specimen.
Double-refractory disease: refractory to an immunomodulatory agent (IMiD) and proteasome inhibitor (PI).
Triple-refractory disease: refractory to an IMiD, PI, and an anti-CD38 monoclonal antibody.
Penta-refractory disease: refractory to lenalidomide, pomalidomide, bortezomib, carfilzomib, and daratumumab or isatuximab.
All multiple myeloma LC subtype means light-chain subtype for all patients with multiple myeloma (n = 78). Light-chain disease LC subtype means light-chain subtype for only light-chain subtype of multiple myeloma (n = 18 total).
IgH/CCND1 gene rearrangement, which is also called t(11;14). t(11;14) percentage mosaicism means the percentage of cells with loss of one IgH signal and gain of one CCND1 signal.
BM, bone marrow; CRP, C-reactive protein; FISH, fluorescent in situ hybridization; HSCT, hematopoietic stem cell transplant; IgH, immunoglobulin heavy chain; LC, light-chain; R-ISS, Revised International Staging System.
Baseline cardiac characteristic differences in cardiac events
Traditional cardiac risk factors, including prior cardiac comorbidities (Table 3), and electrocardiography, echocardiographic characteristics, and cardiac biomarkers (Table 4), were similar between patients with and without cardiac events. However, baseline BNP levels were higher in those who developed cardiac events than in those who did not develop cardiac events, but this did not reach statistical significance (131.9 vs 288.7 ng/mL; P = .123).
Baseline cardiac comorbidities based on cardiac events
| . | No cardiac events (N = 67) . | Cardiac events (N = 11) . | P value . |
|---|---|---|---|
| Hypertension | 34 (50.7%) | 6 (54.5%) | 1 |
| Hyperlipidemia | 12 (17.9%) | 3 (27.3%) | .751 |
| Diabetes mellitus | 6 (9.0%) | 1 (9.1%) | 1 |
| CAD (PCI/CABG) | 4 (6.0%) | 1 (9.1%) | 1 |
| CHF/cardiomyopathy | 2 (3.0%) | 1 (9.1%) | .896 |
| Stroke or TIA | 0 (0.0%) | 0 (0.0%) | 1 |
| COPD | 2 (3.0%) | 0 (0.0%) | 1 |
| OSA | 4 (6.0%) | 0 (0.0%) | .925 |
| Liver dysfunction | 0 (0.0%) | 0 (0.0%) | 1 |
| CKD stage I-III | 3 (4.5%) | 1 (9.1%) | 1 |
| CKD stage IV-V | 2 (3.0%) | 2 (18.2%) | .167 |
| Atrial arrhythmia | 8 (11.9%) | 2 (18.2%) | .93 |
| Ventricular arrhythmia | 1 (1.5%) | 0 (0.0%) | 1 |
| Smoking history | .642 | ||
| Past | 23 (34.3%) | 5 (45.5%) | |
| Never | 41 (61.2%) | 6 (54.5%) | |
| Current | 3 (4.5%) | 0 (0.0%) | |
| Rheumatologic disorder | 3 (4.5%) | 0 (0.0%) | 1 |
| . | No cardiac events (N = 67) . | Cardiac events (N = 11) . | P value . |
|---|---|---|---|
| Hypertension | 34 (50.7%) | 6 (54.5%) | 1 |
| Hyperlipidemia | 12 (17.9%) | 3 (27.3%) | .751 |
| Diabetes mellitus | 6 (9.0%) | 1 (9.1%) | 1 |
| CAD (PCI/CABG) | 4 (6.0%) | 1 (9.1%) | 1 |
| CHF/cardiomyopathy | 2 (3.0%) | 1 (9.1%) | .896 |
| Stroke or TIA | 0 (0.0%) | 0 (0.0%) | 1 |
| COPD | 2 (3.0%) | 0 (0.0%) | 1 |
| OSA | 4 (6.0%) | 0 (0.0%) | .925 |
| Liver dysfunction | 0 (0.0%) | 0 (0.0%) | 1 |
| CKD stage I-III | 3 (4.5%) | 1 (9.1%) | 1 |
| CKD stage IV-V | 2 (3.0%) | 2 (18.2%) | .167 |
| Atrial arrhythmia | 8 (11.9%) | 2 (18.2%) | .93 |
| Ventricular arrhythmia | 1 (1.5%) | 0 (0.0%) | 1 |
| Smoking history | .642 | ||
| Past | 23 (34.3%) | 5 (45.5%) | |
| Never | 41 (61.2%) | 6 (54.5%) | |
| Current | 3 (4.5%) | 0 (0.0%) | |
| Rheumatologic disorder | 3 (4.5%) | 0 (0.0%) | 1 |
Data are presented as a number (percentage).
Liver dysfunction defined as aspartate aminotransferaseor alanine aminotransferaselevels above twice the upper limit of normal.
CABG, coronary artery bypass graft; CAD, coronary artery disease; CHF, congestive heart failure; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; OSA, obstructive sleep apnea; PCI, percutaneous coronary intervention; TIA, transient ischemic attack.
Baseline cardiac diagnostic workup based on cardiac events
| . | No cardiac events (N = 67) . | Cardiac events (N = 11) . | P . |
|---|---|---|---|
| LVEF (%) | 59.0 ± 4.7 | 58.8 ± 3.9 | .928 |
| MV E velocity (cm/s) | 71.2 ± 18.8 | 82.3 ± 33.7 | .33 |
| MV A velocity (cm/s) | 80.8 ± 20.2 | 82.6 ± 17.2 | .784 |
| MV E/A ratio | 0.9 ± 0.2 | 1.0 ± 0.5 | .388 |
| MV E/e' average | 10.7 ± 4.2 | 12.6 ± 5.8 | .196 |
| LV diameter in diastole (cm) | 4.6 ± 0.5 | 5.0 ± 0.8 | .138 |
| LV diameter in systole (cm) | 3.1 ± 0.4 | 3.2 ± 0.6 | .562 |
| Interventricular septum thickness (cm) | 0.9 ± 0.2 | 0.9 ± 0.1 | .353 |
| Posterior wall thickness (cm) | 1.0 ± 0.2 | 0.9 ± 0.1 | .197 |
| Aortic root diameter (cm) | 3.0 ± 0.5 | 2.9 ± 0.5 | .592 |
| LA volume indexed (mL/m2) | 21.1 ± 7.5 | 22.9 ± 11.2 | .616 |
| Global longitudinal strain (%) | −18.4 ± 2.3 | −18.8 ± 3.9 | .705 |
| Baseline troponin level (ng/mL) | 0.010 (0.010-0.010) | 0.010 (0.010-0.015) | .419 |
| Baseline BNP level (pg/mL) | 131.9 ± 301.8 | 288.7 ± 340.3 | .123 |
| . | No cardiac events (N = 67) . | Cardiac events (N = 11) . | P . |
|---|---|---|---|
| LVEF (%) | 59.0 ± 4.7 | 58.8 ± 3.9 | .928 |
| MV E velocity (cm/s) | 71.2 ± 18.8 | 82.3 ± 33.7 | .33 |
| MV A velocity (cm/s) | 80.8 ± 20.2 | 82.6 ± 17.2 | .784 |
| MV E/A ratio | 0.9 ± 0.2 | 1.0 ± 0.5 | .388 |
| MV E/e' average | 10.7 ± 4.2 | 12.6 ± 5.8 | .196 |
| LV diameter in diastole (cm) | 4.6 ± 0.5 | 5.0 ± 0.8 | .138 |
| LV diameter in systole (cm) | 3.1 ± 0.4 | 3.2 ± 0.6 | .562 |
| Interventricular septum thickness (cm) | 0.9 ± 0.2 | 0.9 ± 0.1 | .353 |
| Posterior wall thickness (cm) | 1.0 ± 0.2 | 0.9 ± 0.1 | .197 |
| Aortic root diameter (cm) | 3.0 ± 0.5 | 2.9 ± 0.5 | .592 |
| LA volume indexed (mL/m2) | 21.1 ± 7.5 | 22.9 ± 11.2 | .616 |
| Global longitudinal strain (%) | −18.4 ± 2.3 | −18.8 ± 3.9 | .705 |
| Baseline troponin level (ng/mL) | 0.010 (0.010-0.010) | 0.010 (0.010-0.015) | .419 |
| Baseline BNP level (pg/mL) | 131.9 ± 301.8 | 288.7 ± 340.3 | .123 |
Data are presented as mean ± SD or median (interquartile range) depending on the normality of data.
All echocardiogram data are from baseline transthoracic echocardiogram; data are presented as mean ± SD or median (25%-75% range), depending on the normality of the data.
MV, mitral valve.
Ide-cel index hospitalization characteristic differences in cardiac events
The clinical events that occurred during CAR-T index hospitalization are summarized in Table 5. During index CAR-T hospitalization, there were 16 patients (20.5%) who developed CRS grade 2 or above. CRS grade 2 or above (54.5% vs 14.9%; P = .009) and ICANS grade 3 or above (27.3% vs 4.5%; P = .043) were more common in those who developed cardiac events than in those who did not develop cardiac events. Patients who developed cardiac events had earlier-onset CRS than those who did not develop cardiac events (0.7 vs 1.5 days; P = .043), but no difference was observed in the duration of CRS between the 2 groups. The duration of hospitalization for those who developed cardiac events was longer than for those who did not develop cardiac events, although not statistically significant (22 vs 9.4 days; P = .104). There were more patients who developed cardiac events who required intensive care unit admission than those who did not develop cardiac events (27.3% vs 1.5%; P = .004). All patients who developed cardiac events received tocilizumab (100%) compared with only 71.6% of the patients who did not develop cardiac events (P = .099). Most patients were treated with tocilizumab within 1 day after CRS onset in the whole cohort (96.2%). There was no difference in the time between CRS onset and tocilizumab administration in those who developed vs in those who did not develop cardiac events. Patients who developed cardiac events required increased use of steroids (P = .001) and anakinra (P = .012) compared with patients who did not develop cardiac events. There was no difference between the level of maximum ferritin levels between the groups (10 154 vs 3410 ng/mL; P = .129). There was no difference in scheduled day 5 troponin-I, but day 5 BNP was higher in patients who developed than in those who did not develop cardiac events, although not statistically significant (1105 vs 100 ng/mL; P = .059).
CAR-T hospitalization characteristics by cardiac events
| . | No cardiac events (N = 67) . | Cardiac events (N = 11) . | P . |
|---|---|---|---|
| Maximum CRS gr 2 or above | 10 (14.9%) | 6 (54.5%) | .009 |
| Maximum CRS grade | |||
| 0 | 15 (22.4%) | 0 (0.0%) | |
| 1 | 42 (62.7%) | 5 (45.5%) | |
| 2 | 10 (14.9%) | 4 (36.4%) | |
| 3 | 0 (0.0%) | 0 (0.0%) | |
| 4 | 0 (0.0%) | 1 (9.1%) | |
| 5 | 0 (0.0%) | 1 (9.1%) | |
| Day of CRS onset after CAR-T | 1.5 ± 2.4 | 0.7 ± 0.6 | .043 |
| Day of maximum CRS after CAR-T | 1.8 ± 2.6 | 1.3 ± 1.4 | .383 |
| Duration of CRS in days | 2.5 ± 1.8 | 2.5 ± 1.6 | .978 |
| Maximum ICANS gr 3 or above | 3 (4.5%) | 3 (27.3%) | .043 |
| Maximum ICANS | .005 | ||
| 0 | 59 (88.1%) | 7 (63.6%) | |
| 1 | 3 (4.5%) | 0 (0.0%) | |
| 2 | 2 (3.0%) | 1 (9.1%) | |
| 3 | 3 (4.5%) | 1 (9.1%) | |
| 4 | 0 (0.0%) | 2 (18.2%) | |
| CAR-T dose | 1 | ||
| Less than 400 million | 22 (33.8%) | 4 (36.4%) | |
| More than 400 million | 43 (66.2%) | 7 (63.6%) | |
| Length of stay in days | 9.4 ± 3.9 | 22.0 ± 23.3 | .104 |
| ICU admission | 1 (1.5%) | 3 (27.3%) | .004 |
| Tocilizumab use | 48 (71.6%) | 11 (100.0%) | .099 |
| Steroid use | 18 (26.9%) | 9 (81.8%) | .001 |
| Anakinra use | 0 (0.0%) | 2 (18.2%) | .012 |
| Tocilizumab day after CRS onset | .720 | ||
| 0 d | 33 (70.2%) | 7 (62.6%) | |
| 1 d | 11 (23.4%) | 4 (36.4%) | |
| 2-3 d | 3 (6.4%) | 0 (0%) | |
| Maximum CRP (μg/mL) | 9.3 ± 8.0 | 10.2 ± 8.4 | .728 |
| Maximum ferritin (ng/mL) | 3 410.3 ± 5 441.9 | 10 165.5 ± 13 431.3 | .129 |
| Troponin level, day 5 (ng/mL) | 0.0 ± 0.0 | 0.2 ± 0.5 | .277 |
| BNP level, day 5 (pg/mL) | 100.8 ± 171.6 | 1 105.9 ± 1 370.5 | .059 |
| . | No cardiac events (N = 67) . | Cardiac events (N = 11) . | P . |
|---|---|---|---|
| Maximum CRS gr 2 or above | 10 (14.9%) | 6 (54.5%) | .009 |
| Maximum CRS grade | |||
| 0 | 15 (22.4%) | 0 (0.0%) | |
| 1 | 42 (62.7%) | 5 (45.5%) | |
| 2 | 10 (14.9%) | 4 (36.4%) | |
| 3 | 0 (0.0%) | 0 (0.0%) | |
| 4 | 0 (0.0%) | 1 (9.1%) | |
| 5 | 0 (0.0%) | 1 (9.1%) | |
| Day of CRS onset after CAR-T | 1.5 ± 2.4 | 0.7 ± 0.6 | .043 |
| Day of maximum CRS after CAR-T | 1.8 ± 2.6 | 1.3 ± 1.4 | .383 |
| Duration of CRS in days | 2.5 ± 1.8 | 2.5 ± 1.6 | .978 |
| Maximum ICANS gr 3 or above | 3 (4.5%) | 3 (27.3%) | .043 |
| Maximum ICANS | .005 | ||
| 0 | 59 (88.1%) | 7 (63.6%) | |
| 1 | 3 (4.5%) | 0 (0.0%) | |
| 2 | 2 (3.0%) | 1 (9.1%) | |
| 3 | 3 (4.5%) | 1 (9.1%) | |
| 4 | 0 (0.0%) | 2 (18.2%) | |
| CAR-T dose | 1 | ||
| Less than 400 million | 22 (33.8%) | 4 (36.4%) | |
| More than 400 million | 43 (66.2%) | 7 (63.6%) | |
| Length of stay in days | 9.4 ± 3.9 | 22.0 ± 23.3 | .104 |
| ICU admission | 1 (1.5%) | 3 (27.3%) | .004 |
| Tocilizumab use | 48 (71.6%) | 11 (100.0%) | .099 |
| Steroid use | 18 (26.9%) | 9 (81.8%) | .001 |
| Anakinra use | 0 (0.0%) | 2 (18.2%) | .012 |
| Tocilizumab day after CRS onset | .720 | ||
| 0 d | 33 (70.2%) | 7 (62.6%) | |
| 1 d | 11 (23.4%) | 4 (36.4%) | |
| 2-3 d | 3 (6.4%) | 0 (0%) | |
| Maximum CRP (μg/mL) | 9.3 ± 8.0 | 10.2 ± 8.4 | .728 |
| Maximum ferritin (ng/mL) | 3 410.3 ± 5 441.9 | 10 165.5 ± 13 431.3 | .129 |
| Troponin level, day 5 (ng/mL) | 0.0 ± 0.0 | 0.2 ± 0.5 | .277 |
| BNP level, day 5 (pg/mL) | 100.8 ± 171.6 | 1 105.9 ± 1 370.5 | .059 |
Data are presented as mean ± SD, median (interquartile range), or number (percentage), depending on type of data.
P < .05 is bolded.
gr, grade; ICU, intensive care unit.
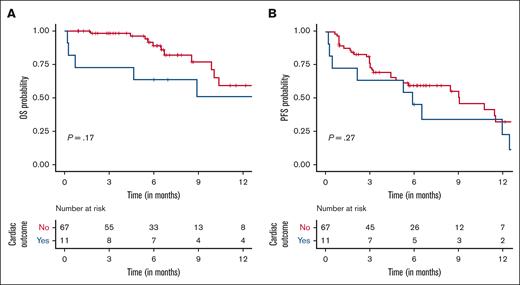
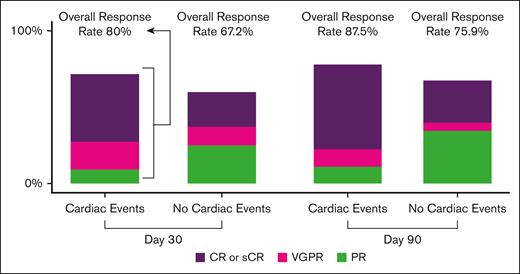
Clinical outcome after ide-cel differences in cardiac events
There were no cardiac events observed after index hospitalization after ide-cel. The overall response to ide-cel and survival data with OS and PFS are summarized in Table 6 and Figures 1 and 2. There was no difference in day 30 or day 90 overall response rate in those with cardiac events compared with those who did not develop cardiac events (P = .175 for day 30 and P = .362 for day 90 response). The overall median follow-up time was 6.09 months (Table 7). The median OS time was not reached. The overall median PFS was 9.03 months (95% CI, 5.62-12.5 months). The median PFS was 5.91 months (95% CI, 2.71 to not reached) for those who developed cardiac events and 9.10 months (95% CI, 5.62 to not reached) for those who did not develop cardiac events. In multivariable analyses, the hazard ratio for the association of the presence of cardiac events with OS was 2.66 (95% CI, 0.85-8.26) and with PFS was 1.98 (95% CI, 0.90-4.37). In those who developed cardiac events, the causes of death were attributed to MM progression (n = 3) and cardiac-related death (n = 1).
Relapsed/refractory multiple myeloma–related outcome based on cardiotoxicity
| . | No cardiac events (N = 67) . | Cardiac events (N = 11) . | P . |
|---|---|---|---|
| Day 30 response | .175 | ||
| sCR | 13 (19.4%) | 5 (50.0%) | |
| CR | 4 (6.0%) | 0 (0.0%) | |
| VGPR | 9 (13.4%) | 2 (20.0%) | |
| PR | 19 (28.4%) | 1 (10.0%) | |
| SD | 13 (19.4%) | 0 (0.0%) | |
| PD | 9 (13.4%) | 2 (20.0%) | |
| Day 90 response | .362 | ||
| sCR | 10 (18.5%) | 4 (50.0%) | |
| CR | 7 (13.0%) | 1 (12.5%) | |
| VGPR | 3 (5.6%) | 1 (12.5%) | |
| PR | 21 (38.9%) | 1 (12.5%) | |
| SD | 2 (3.7%) | 0 (0.0%) | |
| PD | 11 (20.4%) | 1 (12.5%) | |
| Overall response rate at day 30 | 45 (67.2%) | 8 (80.0%) | .652 |
| Overall response rate at day 90 | 41 (75.9%) | 7 (87.5%) | .781 |
| No progression of disease at end of follow-up | 46 (68.7%) | 6 (54.5%) | .565 |
| Alive at end of follow-up | 58 (86.6%) | 7 (63.6%) | .146 |
| . | No cardiac events (N = 67) . | Cardiac events (N = 11) . | P . |
|---|---|---|---|
| Day 30 response | .175 | ||
| sCR | 13 (19.4%) | 5 (50.0%) | |
| CR | 4 (6.0%) | 0 (0.0%) | |
| VGPR | 9 (13.4%) | 2 (20.0%) | |
| PR | 19 (28.4%) | 1 (10.0%) | |
| SD | 13 (19.4%) | 0 (0.0%) | |
| PD | 9 (13.4%) | 2 (20.0%) | |
| Day 90 response | .362 | ||
| sCR | 10 (18.5%) | 4 (50.0%) | |
| CR | 7 (13.0%) | 1 (12.5%) | |
| VGPR | 3 (5.6%) | 1 (12.5%) | |
| PR | 21 (38.9%) | 1 (12.5%) | |
| SD | 2 (3.7%) | 0 (0.0%) | |
| PD | 11 (20.4%) | 1 (12.5%) | |
| Overall response rate at day 30 | 45 (67.2%) | 8 (80.0%) | .652 |
| Overall response rate at day 90 | 41 (75.9%) | 7 (87.5%) | .781 |
| No progression of disease at end of follow-up | 46 (68.7%) | 6 (54.5%) | .565 |
| Alive at end of follow-up | 58 (86.6%) | 7 (63.6%) | .146 |
Overall response rate was designated when there was partial response or better (sCR, CR, VGPR, or PR).
PFS rate was designated when there was no progression of disease (sCR, CR, VGPR, PR, or SD).
OS was calculated as the time between the date of infusion and date of death from any cause or last contact, and PFS was calculated as the time between the date of infusion and date of progression, death, or last contact.
CR, complete response; PD, progression of disease; PR, partial response; sCR, stringent complete response; SD, stable disease; VGPR, very good partial response.
Survival after ide-cel. OS (A) and PFS (B) based on the presence of cardiac events after ide-cel CAR-T. Kaplan-Meier survival curve of OS (A) and PFS (B) estimates by presence of cardiac events after ide-cel CAR-T. The lines depict survival curve of patients who did not develop cardiac events (red line) or patients who did develop cardiac events (blue line). The y-axis indicates the probability of survival. The x-axis indicates survival time in months. Median OS was not reached. Median PFS was 9.03 months.
Survival after ide-cel. OS (A) and PFS (B) based on the presence of cardiac events after ide-cel CAR-T. Kaplan-Meier survival curve of OS (A) and PFS (B) estimates by presence of cardiac events after ide-cel CAR-T. The lines depict survival curve of patients who did not develop cardiac events (red line) or patients who did develop cardiac events (blue line). The y-axis indicates the probability of survival. The x-axis indicates survival time in months. Median OS was not reached. Median PFS was 9.03 months.
Tumor responses based on the presence of cardiac events. Bar graph of tumor responses based on the presence or absence of cardiac events on day 30 and day 90. Overall response rate, defined as CR, sCR, VGPR, or PR are noted at the top of each bar graph. CR, complete response; PR, partial response; sCR, stringent complete response; VGPR, very good partial response.
Tumor responses based on the presence of cardiac events. Bar graph of tumor responses based on the presence or absence of cardiac events on day 30 and day 90. Overall response rate, defined as CR, sCR, VGPR, or PR are noted at the top of each bar graph. CR, complete response; PR, partial response; sCR, stringent complete response; VGPR, very good partial response.
Multivariable analysis of the association of cardiac events with OS and PFS
| . | Model 1 . | Model 2 . | ||||
|---|---|---|---|---|---|---|
| N (event N) . | HR (95% CI) . | P value . | N (event N) . | HR (95% CI) . | P value . | |
| OS | ||||||
| Cardiac event | ||||||
| No | 67 (11) | 1.00 (referent) | .20 | 65 (11) | 1.00 (referent) | .09 |
| Yes | 11 (5) | 2.07 (0.71-6.06) | 11 (5) | 2.66 (0.85-8.26) | ||
| PFS | ||||||
| Cardiac event | ||||||
| No | 67 (31) | 1.00 (referent) | .30 | 65 (30) | 1.00 (referent) | .09 |
| Yes | 11 (9) | 1.52 (0.71-3.22) | 11 (9) | 1.98 (0.90-4.37) | ||
| . | Model 1 . | Model 2 . | ||||
|---|---|---|---|---|---|---|
| N (event N) . | HR (95% CI) . | P value . | N (event N) . | HR (95% CI) . | P value . | |
| OS | ||||||
| Cardiac event | ||||||
| No | 67 (11) | 1.00 (referent) | .20 | 65 (11) | 1.00 (referent) | .09 |
| Yes | 11 (5) | 2.07 (0.71-6.06) | 11 (5) | 2.66 (0.85-8.26) | ||
| PFS | ||||||
| Cardiac event | ||||||
| No | 67 (31) | 1.00 (referent) | .30 | 65 (30) | 1.00 (referent) | .09 |
| Yes | 11 (9) | 1.52 (0.71-3.22) | 11 (9) | 1.98 (0.90-4.37) | ||
Model 1 is unadjusted.
Model 2 is adjusted for age at CAR-T infusion, prior BCMA therapy, and high-risk cytogenetics.
HR, hazard ratio.
Discussion
To our knowledge, this is the first and largest report of cardiac outcomes in patients with RRMM who received ide-cel CAR-T as the SOC. Overall, we observed a similar incidence of cardiac events (14.1%) in ide-cel CAR-T compared with what has been reported for anti-CD19 CAR-T therapy.6-10 The most common cardiac event was atrial arrhythmias followed by CTRCD in our cohort. These were comparable with prior studies investigating cardiotoxicity after anti-CD19 CAR-T therapy.6-8,10
The risk factors associated with cardiac events in our study were female sex, Black race, light-chain subtype of myeloma with strikingly higher incidence with λ subtype of the disease, worse baseline performance status (ECOG > 1), elevated baseline BNP, and ferritin above the upper limit of normal.
One of our hypotheses was that prior exposure to cardiotoxic agents such as carfilzomib would increase the risk of cardiac events after ide-cel. However, this was difficult to assess because there was only 1 patient in our cohort who was not exposed to carfilzomib before ide-cel. None of the 3 patients who had a history of preexisting congestive heart failure/cardiomyopathy experienced cardiotoxicity. In a prospective study investigating the incidence of cardiac events after carfilzomib, >50% experienced grade 3 or higher cardiovascular adverse events, mostly comprising heart failure (20%) and hypertension (23%).22 Of note, there were 41% of all grade heart failure (21% grade 1-2 and 20% grade 3-4 heart failures). In a large meta-analysis of the risk of carfilzomib on cardiac events, the pooling of multiple clinical trial data shows that cardiac failure incidence was 4.4%.23 However, the risk of discontinuation of carfilzomib or death because of cardiac events was low. Also, carfilzomib-associated cardiotoxicity appears to be reversible, with nearly complete recovery of cardiac function with appropriate medical therapy.24 Therefore, we do not believe that prior use of carfilzomib in ide-cel increases the risk of cardiac event development, when compared with those who receive anti-CD19 CAR-T.
Surprisingly, baseline cardiac comorbidities were not associated with cardiac events in our cohort, although this should be interpreted with caution because of the low number of events in this study. Indeed, other studies did find a correlation between baseline cardiac comorbidities and cardiac events after CAR-T.6-8,12,25 In addition, baseline transthoracic echocardiogram quantitative measures were not associated with cardiac events. However, our cohort has similar baseline cardiac comorbidities compared with that of patients with MM who have been treated with at least 3 agents (proteasome inhibitor, immunomodulatory agent, and either alkylating agent or anthracycline).26 In most studies, baseline LVEF was similar between those who did and those who did not develop cardiac events after anti-CD19 CAR-T.7,12,27 For instance, in a study in which comprehensive serial echocardiograms were performed before and after anti-CD19 CAR-T, baseline LV dimensions and LVEF were not different between those who did and those who did not develop cardiac events.12 However, in a recent cohort of patients who underwent anti-CD19 CAR-T, our team found that larger LV and LA dimensions were associated with cardiac events after anti-CD19 CAR-T.11 This is likely due to most cardiac events occurring after anti-CD19 CAR-T being atrial arrhythmias. This was not surprising because preexisting cardiac remodeling, such as LA enlargement, predisposes the patient to atrial arrhythmias.28 However, in our study of ide-cel, baseline LA volume index was not higher in those who developed atrial arrhythmias than in those who did not develop atrial arrhythmias (23.9 vs 21.1 mL/m2; P = .566). Patients who developed CRS grade 2 or above were more likely to develop cardiac events. This is in line with prior studies6-8,12 and likely because of the same phenomenon of cytokine storm leading to proinflammatory status in the heart, which leads to cardiac events. Patients with cardiotoxicity were more likely to have ICANS grade 3 or above, longer intensive care unit stay, and higher post–CAR-T day 5 BNP levels compared with those who did not develop cardiac events. There was no difference in tocilizumab use patterns (the majority of patients were treated with tocilizumab), but more patients with cardiotoxicity were treated with steroids and anakinra.
We and others have previously shown that cardiac events in the setting of CAR-T are inflammatory in nature.6,7,11,29,30 Based on this report, the subtype of the disease may play a role in the development of cardiac events. Specifically, our cohort showed a predisposition for cardiac events in patients with λ light-chain RRMM and in patients with intact immunoglobulin disease with λ light-chain subtype. The reason for this finding remains unclear, but 1 hypothesis is that subclinical light-chain amyloidosis is associated with an increased risk of cardiac events in these patients. There was only 1 patient with cardiac AL amyloidosis on cardiac MRI in our study, and this patient did not develop any cardiac events. In addition, t(11;14) is one of the most common chromosomal abnormalities in the setting of AL amyloidosis. However, patients with concurrent cardiac AL amyloidosis and RRMM had a lower incidence of t(11;14) than those with cardiac AL amyloidosis alone (17.6% vs 56.5%).31 In a retrospective study of AL amyloidosis, ∼40% to 60% of patients had t(11;14), which was associated with poor outcome.32 In our cohort, the overall incidence of t(11;14) was 6.4% and did not have an impact on the likelihood of cardiac events. Furthermore, the chromosomal mosaicism of t(11;14) was not higher in patients who developed cardiac events. Other suggestive clinical indicators of AL amyloidosis, such as significant proteinuria and liver dysfunction, were not present in our cohort. Although there are no published data on the significance of chromosomal mosaicism of t(11;14) in MM or AL amyloidosis, this is a relationship that can be investigated in the future. Therefore, the evidence for subclinical light-chain amyloidosis leading to increased cardiac events is lacking, although the overall incidence of these clinical characteristics associated with AL amyloidosis is too low in our cohort to allow definitive conclusions.
Our results on survival data are in line with the first SOC experience on ide-cel CAR-T.20 Part of our data in this study was included in the multicenter data on SOC ide-cel. Our results suggest that the presence of cardiac events may confer poor PFS or OS; however, because of the small sample size, the power to detect an association was limited. The effect of cardiac events on cancer-related outcomes cannot be fully explained but is in line with other CAR-T studies.7,11
Limitations of this study include its retrospective design and limited follow-up. Repeat echocardiograms were only performed when a clinical suspicion for cardiac events occurred. Therefore, a systematic surveillance approach for a more accurate incidence of cardiomyopathy could not be performed. Another limitation of this study is the small number of cardiotoxicity events in these patients, preventing a multivariable regression analysis to investigate factors associated with cardiotoxicity because of inadequate power. There is a possibility of selection bias, whereby patients with severe heart failure may not have been treated with ide-cel. In addition, the true incidence of CTCRD may be underestimated, given the limited number of patients (11 of 78) who underwent surveillance echocardiogram based on clinical suspicion; hence, asymptomatic cardiomyopathy might have been overlooked. Despite these limitations, to our knowledge, our study is the first and the largest single-center study investigating cardiac events in anti-BCMA CAR-T therapy for RRMM as the SOC. Of note, our prior paper on cardiac events after CAR-T in 2019 included investigational CAR-T bb2121 for RRMM.6 Our results are novel, with hypothesis-generating risk factors, such as λ light-chain predisposition as well as higher rates in women and Black patients that warrant future studies. Surprisingly, comprehensive baseline cardiac workup, including baseline cardiac biomarkers, ECG, and echocardiogram, was not different in patients who developed cardiac events after ide-cel. Future prospective studies investigating the concurrent presence of subclinical cardiac amyloidosis with cardiac MRI are warranted.
In conclusion, ide-cel CAR-T is associated with similar cardiac events as other types of CAR-T. Patients with inferior performance status, higher-grade CRS and ICANS, and λ light-chain RRMM appear to be at an increased risk of developing cardiac events. The presence of cardiac events imply a poor cancer-related prognosis or OS.
Acknowledgments
This project was supported by a grant through the USF GME Research Grant Program (D.H.L., 2022-2023). R.C.B., K.H.S., M. Alsina, D.K.H., L.C.P., L.B.O., and C.F. are funded by Pentecost Myeloma Research Center.
Authorship
Contribution: D.H.L., T.M., M. Alsina, B.J.B., M.J., R.C.B., F.L.L., G.H.O., M. Alomar, and D.K.H. designed the research; D.H.L., A.K., T.M., D.K.H., and M. Alomar performed the research; D.H.L., A.K., T.M., C.B., S.C., A.G.C., G.D.A., M. Alomar, and D.K.H. collected data; D.H.L., L.C.P., L.B.O., and D.K.H. analyzed the data; and D.H.L., A.K., T.M., M. Alsina, B.J.B., J.B., H.E., R.F., C.F., M.J., S.K., F.K., H.L., T.N., O.A.C.P., K.H.S., E.S., R.C.B., F.L.L., G.H.O., M. Alomar, and D.K.H. wrote the paper.
Conflict-of-interest disclosure: A.L. consults and is on the advisory board for Kadmon/Sanofi, Humanigen, and Avrobio. F.L.L. has a scientific advisory role for A2, Allogene, Amgen, bluebird bio, Bristol Myers Squibb (BMS)/Celgene, Calibr, Caribou, Cellular Biomedicine Group, Daiichi Sankyo, GammaDelta Therapeutics, Iovance, Kite Pharma, Janssen, Legend Biotech, Novartis, Sana, Takeda, Wugen, and Umoja; has received research funding from Kite Pharma (institutional), Allogene (institutional), CERo Therapeutics (institutional), Novartis (institutional), bluebird bio (institutional), BMS (institutional), National Cancer Institute, and Leukemia and Lymphoma Society; and has a consulting role at Cowen, EcoR1, Emerging Therapy Solutions, and Gerson Lehrman Group. M.J. is a consulting adviser for Kite/Gilead, Novartis, BMS, and Myeloid Tx, and received research funding from Incyte and Kite/Gilead. K.H.S. consults and is on the advisory board for Sanofi, BMS, Janssen, Amgen, Karyopharm, Adaptive, GlaxoSmithKline (GSK), and Takeda, and received research support from Karyopharm and AbbVie. M.L.D. receives consulting fees from Adicet, Bellicum, Capsta, Syncopation, and Synthekine; has stock or stock options with Adaptive Biotechnologies, Adicet, Bellicum Precision Biosciences, and Prescient; and receives licensing fees from Atara and CRISPR. R.F. receives research support from Novartis and Kite/Gilead. L.C.P. receives research support from BMS. A.G.C. is on the advisory board and speaking bureau of Sanofi. R.C.B. receives research support from BMS, Karyopharm, AbbVie, and Janssen, and is an advisory board member with Janssen, Pfizer, GSK, BMS, AbbVie, Takeda, and Sanofi. D.K.H. received honoraria from OncLive; has a consulting or advisory role and received research funding from BMS; received research funding from Adaptive Biotech; and is supported by the Pentecost Family Myeloma Research Center and the International Myeloma Society Young Investigator Award. The remaining authors declare no competing financial interests.
Correspondence: Doris K. Hansen, Department of Blood and Marrow Transplant and Cellular Immunotherapy, H. Lee Moffitt Cancer Center and Research Institute, 12902 USF Magnolia Dr, CSB-7 BMT, Tampa, FL 33612; e-mail: doris.hansen@moffitt.org; and Mohammed Alomar, Division of Cardio-Oncology, H. Lee Moffitt Cancer Center, 12902 USF Magnolia Dr, CSB 3130, Tampa, FL 33612; e-mail: mealomar@usf.edu.
References
Author notes
∗D.H.L., A.K., and T.M. contributed equally to this study.
†D.K.H. and M. Alomar are joint senior authors and contributed equally to this study.
Data are available on request from the corresponding author, Doris K. Hansen (doris.hansen@moffitt.org).