Abstract
Clinical data indicate that after allogeneic hematopoietic stem cell transplantation (HSCT) for hematological malignancies, the graft-versus-leukemia (GVL) effect is in large part mediated by the graft-versus-host reaction (GVHR), which also often leads to graft-versus-host disease (GVHD). Controlling alloreactivity to prevent GVHD while retaining GVL poses a true dilemma for the successful treatment of such malignancies. We reasoned that suicide gene therapy, which kills dividing cells expressing the thymidine kinase (TK) “suicide” gene using time-controlled administration of ganciclovir (GCV), might solve this dilemma. We have previously shown that after infusion of allogeneic TK T cells along with HSCT to an irradiated recipient, an early and short GCV treatment efficiently prevents GVHD by selectively eliminating alloreactive T cells while sparing nonalloreactive T cells, which can then contribute to immune reconstitution. Nevertheless, it remained to be established that this therapeutic strategy retained the desired GVL effect. Hypothesizing that a contained GVHR would be essential, we evaluated the GVL effect using different protocols of GCV administration. We were able to show that when the GCV treatment is initiated at, or close to, the time of grafting, GVHD is controlled but GVL is lost. In contrast, when the onset of GCV administration is delayed until day 6, a potent GVL effect is retained while GVHD is still controlled. These data emphasize that, by a time-optimized scheduling of the administration of GCV, this TK/GCV strategy can be tuned to efficiently treat malignant hemopathies.
Introduction
Allogeneic hematopoietic stem cell transplantation (HSCT) is the treatment of choice for many hematological malignancies. Following the intensive conditioning of the recipient before transplantation aimed at eliminating malignant cells, donor T cells present in the graft contribute to the graft-versus-leukemia (GVL) effect1 by eliminating residual leukemic cells expressing disparate major histocompatibility complex (MHC) antigens and/or tumor-associated antigens. Donor T cells also improve engraftment2 and provide a graft-versus-infection (GVI) effect for patients who are severely immunodeficient owing to the conditioning.3,4 Unfortunately, in addition to their ability to provide such beneficial effects, donor T cells are also responsible for the life-threatening graft-versus-host disease (GVHD) that is initiated by mature T cells that recognize MHC alloantigens presented by recipient cells.5 6 This complication can be circumvented by the removal of mature T cells from the graft, but only to the detriment of engraftment, as well as of the GVI and GVL effects. Thus, the GVHD and GVL effects are closely linked, and controlling alloreactivity to prevent GVHD while retaining the GVL effect represents the challenge for successful HSCT.
We and others have developed a strategy for controlling GVHD that relies on ex vivo transduction of donor T cells carrying a suicide gene encoding Herpes simplex type 1 thymidine kinase (TK). The expression of the TK transgene allows the metabolism of the nucleoside analog ganciclovir (GCV) into triphosphated-GCV (the active form of GCV), which blocks DNA elongation and thereby causes cell death.7-9 When donor TK T cells divide after recognizing recipient alloantigens, they become sensitive to, and can be killed by, GCV administration.10,11 Suicide gene therapy permits the selective elimination of those T cells that recognize recipient alloantigens, while preserving the T cells that did not divide during the treatment with GCV.12 In preclinical experiments using TK T cells from transgenic mice, we and others have previously demonstrated that this therapeutic approach (1) efficiently prevents GVHD,13,14 (2) does not impair engraftment after either myeloablative13,15,16 or nonmyeloablative17 conditioning, and (3) spares a pool of nondividing donor TK T cells that further contributes to the recipient immune system reconstitution.12
To date, all preclinical data using the TK/GCV system in the field of allogeneic HSCT were obtained under conditions where a GVL effect was not required. The clinical relevance of this therapeutic strategy for the treatment of hematological malignancies thus remained to be established by a demonstration that it permits the simultaneous control of GVHD while retaining the desired GVL effect. In this work, using a murine model of leukemia, we show that when the GCV treatment is initiated at, or close to, the time of grafting, GVHD is indeed controlled, but the GVL effect is lost. In contrast, when the onset of GCV administration is delayed until day 6, a potent GVL effect is retained while GVHD is still controlled.
Materials and methods
Mice
C57BL/6 (B6, H-2b), DBA/2 (D2, H-2d), and B6 × D2 F1 (H-2bxd) mice were obtained from Iffa Credo (L'Arbresle, France). The ΔTK line 6 (referred to as TK in this report) mice, expressing the ΔTK transgene18 in virtually all CD4 and CD8 T cells, were described previously.15 Human CD4 (hCD4) transgenic mice, line 10, express the hCD4 protein at the cell surface of mouse CD4 (mCD4) and mCD8 cells (referred to in the text as CD4 or CD4+ and CD8 or CD8+ cells, whereas the transgene is referred to as hCD4).19 Double-transgenic (hCD4 × TK) mice were obtained by breeding the line 6 ΔTK and the line 10 hCD4 transgenic mice. All transgenic mice were bred in the animal facility of the Faculté de Médecine PitiéSalpêtrière (Paris, France). Mice were manipulated according to European union guidelines.
Experimental GVHD and drug administration
Experiments were performed as described,12 except where otherwise stated. Briefly, hybrid B6 × D2 F1females (8 to 12 weeks of age) were lethally irradiated (11Gy). The day after irradiation, 5 × 106 T-cell–depleted (TCD)–BM cells from B6 mice plus 8.4 × 106 to 9.2 × 106 T cells collected from spleen and lymph nodes of TK or hCD4 × TK transgenic B6 mice were injected intravenously. GCV (Roche, Neuilly-sur-Seine, France) was administered intraperitoneally at a dosage of 50 mg/kg twice daily. Different schemes of GCV administration were used: a total of 5 injections administered twice daily beginning at day 1, day 3½, or day 6 after grafting. The control group received a 7-day GCV treatment with miniosmotic pumps implanted subcutaneously at the time of bone marrow transplantation (BMT) under tri-bromo-ethanol anesthesia and delivering 1 ± 0.02 μL/h. This last group provides an experimental model of lethal GVHD that is efficiently controlled by early GCV administration as initially described.13 Cyclosporin A (CsA) (Sandimmun; Novartis, Bâle, Swiss) was administered intraperitoneally daily from day −2 before BMT to day 10 at a dose of 50 mg/kg/d, as previously described.20
Analysis of in vivo T-cell proliferation
T cells from double-transgenic (hCD4 × TK) mice were stained with the 5- and 6- carboxyfluorescein diacetate succinimidyl ester (CFSE): 1 × 107 cells per milliliter were incubated for 10 minutes at 37°C, 5% CO2 in a medium (RPMI 1640) containing CFSE at a concentration of 1.5 μM. Staining was stopped by addition of fetal calf serum to reach a concentration of 20% of the final volume. Labeled cells were washed twice in phosphate buffer saline, numbered, and injected intravenously with BM cells in lethally irradiated mice. Splenocytes from grafted animals were collected at day 2½, day 3½, or day 6½ after transplantation. Cell proliferation was studied by flow cytometry as the sequential loss of CFSE fluorescence upon cell division after gating on donor (hCD4+) CD4 and CD8 populations.
Flow cytometrical analysis
Spleens from grafted animals were digested with collagenase and DNAse, and splenocytes were incubated with 2.4.G2 anti-Fc receptor monoclonal antibody (mAb). Transplanted mature donor T cells and their progeny were identified by their expression of the hCD4 transgene. For analysis of chimerism, cells were stained with combinations of the following mAbs: phycoerythrin (PE)–labeled anti-CD3 (clone 145-2c11; Pharmingen, San Diego, CA); fluorescein isothiocyanate–labeled anti-B220 (clone RA3-6B2; Caltag Laboratories, San Francisco, CA); biotinylated anti–H-2Kd(clone SF1-1.1; Pharmingen) revealed with tricolor-labeled streptavidin (Caltag); and PE-labeled anti–H-2Kb (clone CTKb; Caltag). For CFSE experiments, splenocytes were stained with the following mAbs: allophycocyanin-labeled anti-hCD4 (clone S3.5; Caltag); PE-labeled anti-CD4 (clone RMH-5; Pharmingen); and tricolor-labeled anti-CD8 (clone CT-CD8a; Caltag). Events were acquired on a FACSCalibur (Becton Dickinson, San Jose, CA) and analyzed by means of CellQuest software (Becton Dickinson).
Leukemia model
P815 mastocytoma cells that are of DBA/2 mouse origin express H-2d MHC molecules. First, 2 × 103P815 cells were injected intravenously in the retro-orbital sinus to recipients at the time of BMT. Clinical signs of leukemia were macroscopic tumor at the site of leukemic cell injection followed in most cases by lower-limb paralysis. Leukemic cells were also identified in peripheral blood by the surface expression of H-2d(recipient-type) but not H-2b (donor-type) histocompatibility antigens.
Histopathological examination
Liver samples were prepared in Bouin fixative and embedded in paraffin, and sections were stained with hematoxylin and eosin. A pathologist unaware of treatment evaluated slides. GVHD lesions were scored as described previously.21
Statistical analysis
Statview software (Abacus Concepts, Berkeley, CA) was used for statistical analysis. Kaplan-Meier survival curves were established for each group. Mice suffering from advanced-stage GVHD were killed for histopathological examination and considered dead in the Kaplan-Meier analysis. Survival differences between the 2 groups were determined by means of the log-rank test. Analysis of variance (ANOVA) was used to compare GVHD scores. Pis indicated only when differences between the 2 groups were statistically significant.
Results
Optimizing the GCV treatment protocol according to the kinetics of T-cell proliferation following allogeneic transfer
We have previously shown that a 7-day GCV treatment initiated immediately after grafting provides a good prophylaxis against GVHD.13 On the basis of experimental as well as clinical data, we hypothesized that preserving the GVL effect would require letting the graft-versus-host reaction (GVHR) proceed for a limited period of time, and then stopping it before GVHD appears and becomes uncontrollable. Since the TK/GCV approach is based on the selective killing of dividing cells, we reasoned that a careful examination of T-cell division would help define the optimal GCV protocol for achieving this goal.
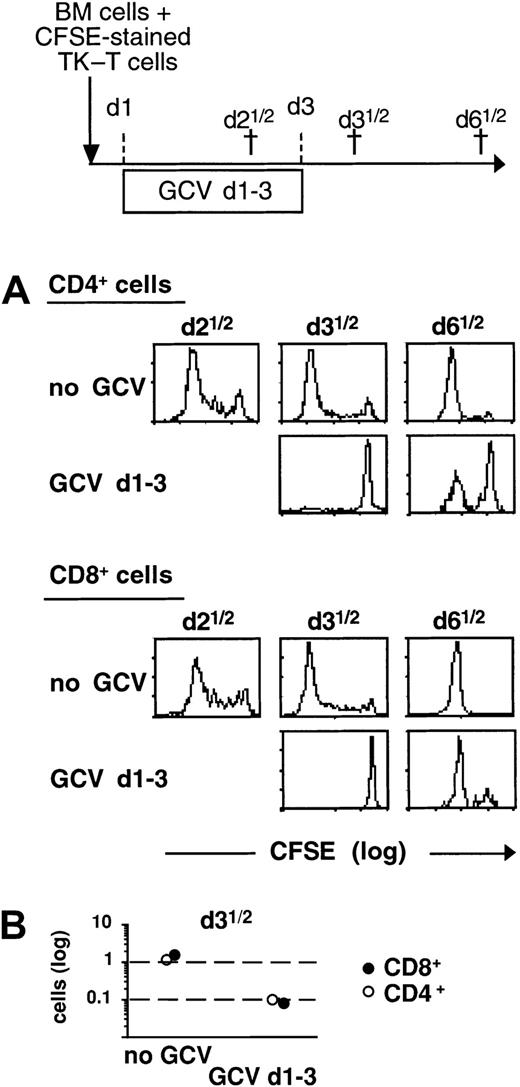
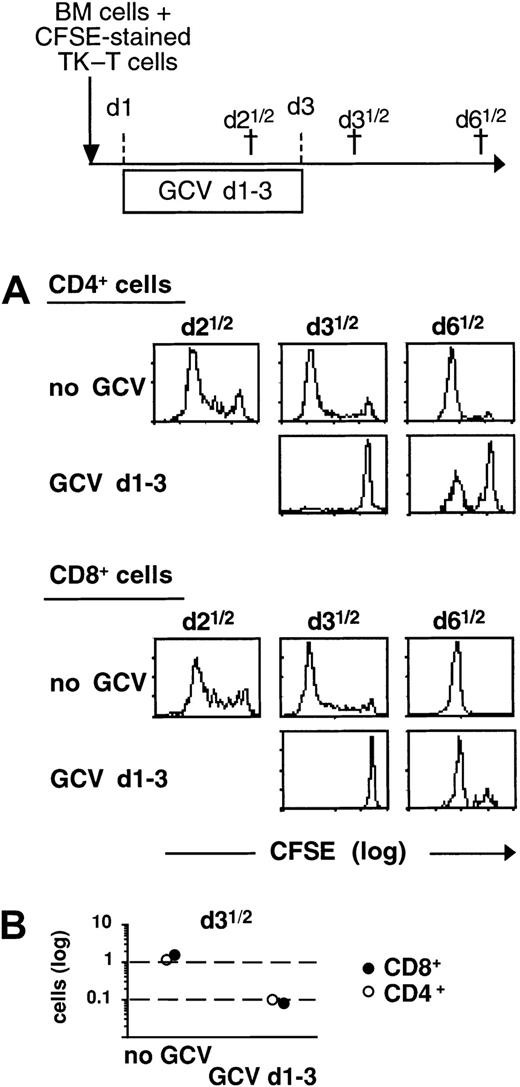
Using CFSE-cell staining, we analyzed T-cell division kinetics after allogeneic BMT, as well as after GCV administration. CFSE-stained TK T cells were infused together with BM cells from wild-type B6 mice into lethally irradiated semiallogeneic B6 × D2 F1 recipients. To unambiguously identify transplanted donor T cells, we used T cells obtained from double-transgenic mice expressing, in addition to the TK transgene, the hCD4 marker molecule on both CD4+ and CD8+ T cells.15,19 Spleen cells from mice that received transplants were collected at different time points after BMT, and donor T-cell division was assessed by the sequential loss of CFSE fluorescence intensity after gating on hCD4+CD4+ and hCD4+CD8+double-positive populations. Using a similar approach, we recently demonstrated that after injection of allogeneic donor T cells (without BM cells) into lethally irradiated mice, alloreactive and nonalloreactive T cells can be distinguished on the basis of their division rate and phenotypic differences.22 In the current experiments, we observed that CD4+ and CD8+donor T cells present in the spleen of grafted animals had already started to divide by day 2½, and that at day 3½, the vast majority of donor T cells had divided several times (Figure1A). We thus reasoned that a short GCV treatment administered from day 1 to day 3 after BMT should be sufficient to eliminate most alloreactive T cells and, therefore, to control GVHD. Additionally, shortening the duration of the GCV treatment from 7 days (as initially described13) to 2 days should affect fewer nonalloreactive T cells,12 including those that recognize tumor-associated antigens and might participate in the nonallogeneic part of the GVL effect. When GCV treatment was administered from day 1 to day 3 after BMT, we did not observe any cell division in CD4+ and CD8+ donor T cells during the period of GCV administration (Figure 1A). At day 3½, we observed an approximately 10-fold decrease of hCD4+CD4+ and hCD4+CD8+T-cell counts as compared with untreated animals, illustrating the cytolytic effect of GCV on dividing TK T cells (Figure 1B). At day 6½ (3½ days after discontinuation of GCV), numerous cell divisions had occurred in both CD4+ and CD8+ donor T cells. Thus, these data suggest that a short GCV administration should suffice to eliminate alloreactive T cells while sparing at least a portion of the nonalloreactive donor TK T cells.
Kinetics of cell division after TK T cell infusion in lethally irradiated hosts.
(A) B6 × D2 F1 irradiated mice received B6 BM cells supplemented with 1 × 107 CFSE-labeled mature T cells from hCD4 × TK double-transgenic B6 mice. Control groups received no GCV treatment (no GCV). In treated groups, GCV treatment consisted of 5 injections that began 24 hours after grafting and were administered every 12 hours (GCV d1-3). †Time mice were killed on the experimental scheme. CFSE intensity of hCD4+ in CD4+ and CD8+ T cells was analyzed at different time points after grafting. Each histogram is representative of 2 mice. The peak of highest intensity on the log scale identifies the parent generation of infused donor T cells. Peaks with decreased CFSE intensity represent daughter generations that have undergone cell division. (B) The number of CD4+ and CD8+ donor T cells in spleens of grafted animals (n = 2 for each group) was evaluated at day 3½ by their expression of the hCD4 marker. The coefficient of variation of duplicates was less than 10%.
Kinetics of cell division after TK T cell infusion in lethally irradiated hosts.
(A) B6 × D2 F1 irradiated mice received B6 BM cells supplemented with 1 × 107 CFSE-labeled mature T cells from hCD4 × TK double-transgenic B6 mice. Control groups received no GCV treatment (no GCV). In treated groups, GCV treatment consisted of 5 injections that began 24 hours after grafting and were administered every 12 hours (GCV d1-3). †Time mice were killed on the experimental scheme. CFSE intensity of hCD4+ in CD4+ and CD8+ T cells was analyzed at different time points after grafting. Each histogram is representative of 2 mice. The peak of highest intensity on the log scale identifies the parent generation of infused donor T cells. Peaks with decreased CFSE intensity represent daughter generations that have undergone cell division. (B) The number of CD4+ and CD8+ donor T cells in spleens of grafted animals (n = 2 for each group) was evaluated at day 3½ by their expression of the hCD4 marker. The coefficient of variation of duplicates was less than 10%.
Short and early GCV treatment protects against GVHD but also prevents the GVL effect
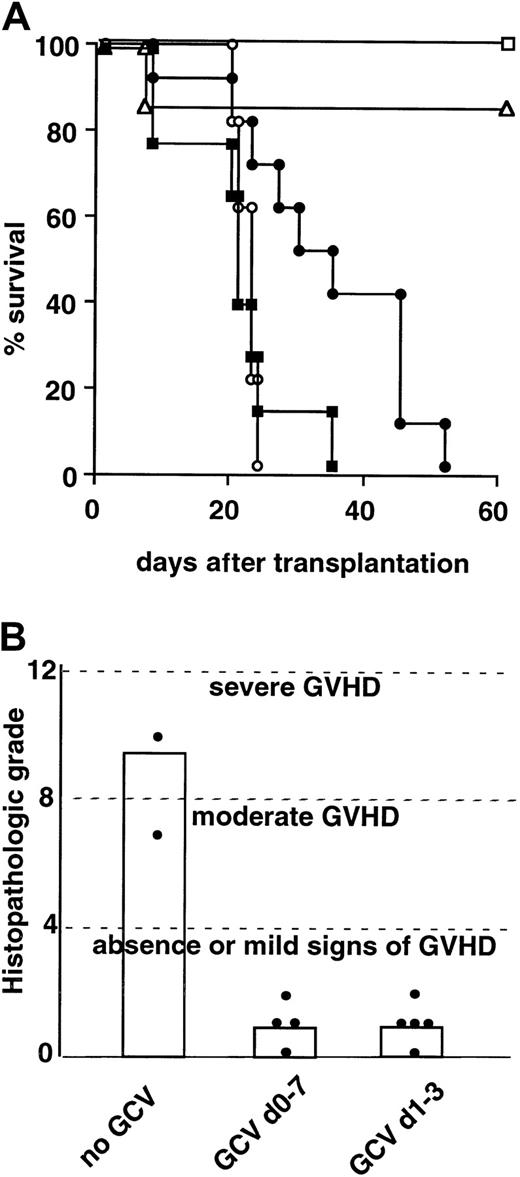
We next evaluated the efficacy of GVHD control in allografted mice receiving a day 1–to–day 3 GCV treatment. This short treatment prevented GVHD as efficiently as the day 0–to–day 7 GCV treatment.13,15 16 At day 60, 85% of the treated mice were still alive (Figure 2A) with a histopathological score (Figure 2B) comparable to that observed with the 7-day GCV treatment. In contrast, all untreated mice died (Figure2A) with characteristic clinical signs (weight loss, skin lesions, and hunching), and histological signs (lymphocyte infiltration and parenchymal injury of liver) of GVHD (Figure 2B). More than 95% of the splenocytes from GCV-treated animals were of donor H-2b and not of recipient H-2d origin in both the B- and T-cell compartments, attesting to a good engraftment (not shown). Thus, a 2-day GCV treatment started at day 1 after grafting is efficient in preventing GVHD.
Absence of GVL effect after early GCV treatment.
(A) Experimental GVHD was induced by B6 TK T cells injected together with B6 TCD-BM cells in lethally irradiated B6 × D2 F1 recipient mice. Leukemic challenge was performed by intravenous injection of 2 × 103 P815 (H-2d) mastocytoma cells at the time of grafting. In the absence of treatment (black circle; n = 10) GVHD is lethal. GCV is administered by continuous subcutaneous infusion from day 0 until day 7 after graft (white square; n = 4) or by 5 intraperitoneal injections every 12 hours beginning 24 hours after BMT (white triangle; n = 6). For the leukemia control group, B6 × D2 F1mice were grafted with B6 TCD-BM plus P815 cells (white circle; n = 5). The experimental group is represented by B6 × D2 F1 mice grafted with B6 TCD BM plus B6 TK T cells plus P815 cells and treated by GCV from day 1 to day 3 after graft (black square; n = 8). Results are presented as Kaplan-Meier survival. (B) Histopathologic liver score after semiallogeneic BMT. Histopathologic examination and grading of GVHD of liver from mice were performed 65 to 75 days after transplantation. GVHD control mice did not receive GCV treatment (no GCV; n = 2) and were killed at day 19 with clinical signs of GVHD (body weight below 13 g, hunching). GCV treatment consisted of continuous subcutaneous administration from day 0 to day 7 after graft (GCV d0-7; n = 4) or of 5 intraperitoneal injections every 12 hours beginning 24 hours after graft (GCV d1-3; n = 5). Histograms indicate the mean histopatological score for each group. The Fisher test was used for the ANOVA;P < .05 for GVHD group versus all other groups.
Absence of GVL effect after early GCV treatment.
(A) Experimental GVHD was induced by B6 TK T cells injected together with B6 TCD-BM cells in lethally irradiated B6 × D2 F1 recipient mice. Leukemic challenge was performed by intravenous injection of 2 × 103 P815 (H-2d) mastocytoma cells at the time of grafting. In the absence of treatment (black circle; n = 10) GVHD is lethal. GCV is administered by continuous subcutaneous infusion from day 0 until day 7 after graft (white square; n = 4) or by 5 intraperitoneal injections every 12 hours beginning 24 hours after BMT (white triangle; n = 6). For the leukemia control group, B6 × D2 F1mice were grafted with B6 TCD-BM plus P815 cells (white circle; n = 5). The experimental group is represented by B6 × D2 F1 mice grafted with B6 TCD BM plus B6 TK T cells plus P815 cells and treated by GCV from day 1 to day 3 after graft (black square; n = 8). Results are presented as Kaplan-Meier survival. (B) Histopathologic liver score after semiallogeneic BMT. Histopathologic examination and grading of GVHD of liver from mice were performed 65 to 75 days after transplantation. GVHD control mice did not receive GCV treatment (no GCV; n = 2) and were killed at day 19 with clinical signs of GVHD (body weight below 13 g, hunching). GCV treatment consisted of continuous subcutaneous administration from day 0 to day 7 after graft (GCV d0-7; n = 4) or of 5 intraperitoneal injections every 12 hours beginning 24 hours after graft (GCV d1-3; n = 5). Histograms indicate the mean histopatological score for each group. The Fisher test was used for the ANOVA;P < .05 for GVHD group versus all other groups.
We next investigated whether a GVL effect could be observed with the use of such GCV treatment. Leukemia was induced in lethally irradiated mice by injecting 2 × 103 P815 cells intravenously at day 0. This led to 100% mortality in mice grafted with TCD-BM (Figure2A), with death being preceded by the appearance of leukemic cells in peripheral blood, a retro-orbital tumor at the site of injection, and, in most cases, a hind-limb paralysis. Similar mortality was observed in TCD-BM–grafted mice treated with GCV, indicating that GCV was not toxic for the leukemic cells (not shown). We then assessed whether the addition of TK T cells to the TCD-BM and the P815 cells, under our GCV treatment scheme, provided a GVL effect. In this experiment, all mice died with characteristic biological and clinical signs of leukemia, with the same kinetics as those observed for control mice not receiving the TK T cells (Figure 2A).
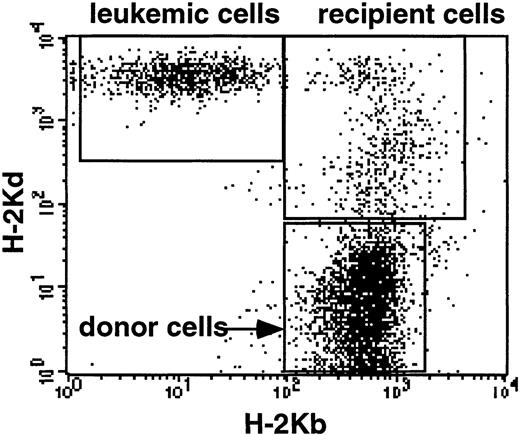
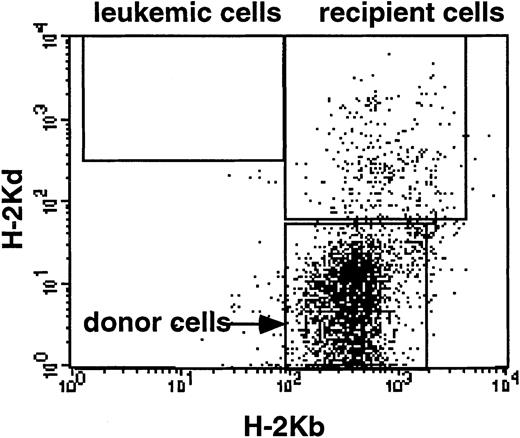
The presence of leukemic cells in the peripheral blood of mice was unequivocally confirmed by their expression of recipient-type H-2Kd, and not donor-type H-2Kb, MHC class I molecules (Figure 3). Thus, when alloreactive T cells are eliminated by GCV treatment early after BMT, GVHD is controlled, but there is no GVL effect.
Detection of P815 leukemic cells in the peripheral blood of mice.
P815 mastocytoma cells were identified by flow cytometry by the expression of recipient type (H-2d), but not donor type, (H-2b) MHC class I molecules. P815 cells were identified on 3 of 3 mice having clinical leukemic signs after BM grafting plus TK T cell infusion and GCV treatment from day 1 to day 3, as illustrated here.
Detection of P815 leukemic cells in the peripheral blood of mice.
P815 mastocytoma cells were identified by flow cytometry by the expression of recipient type (H-2d), but not donor type, (H-2b) MHC class I molecules. P815 cells were identified on 3 of 3 mice having clinical leukemic signs after BM grafting plus TK T cell infusion and GCV treatment from day 1 to day 3, as illustrated here.
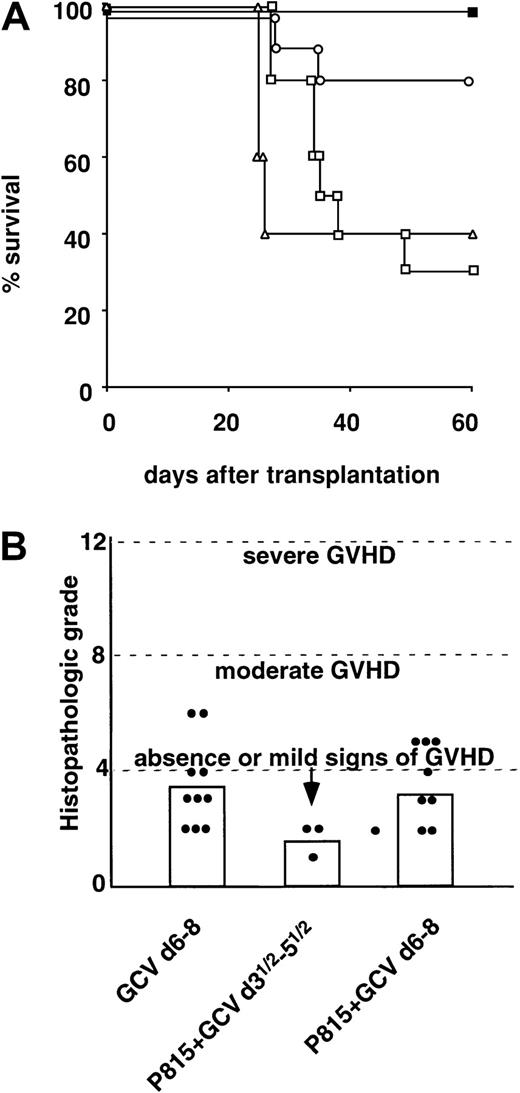
Delayed GCV treatment permits GVL effect without altering protection against GVHD
We reasoned that if GCV administration was delayed, alloreactive donor T cells might be maintained for a longer time after BMT, thus allowing a time-limited GVHR that might favor the GVL effect. When mice received the same 2-day GCV treatment from day 3½ or day 6 rather than from day 1, they all survived without any clinical signs of GVHD (Figure 4A). Compared with mice receiving a GCV treatment starting at day 0 or day 1, histological signs of GVHD were either absent when the treatment was delayed to day 3½ or slightly increased when the treatment started at day 6 (Figure 4B). Splenocytes of GCV-treated animals were of donor H-2b, and not of recipient H-2, origin (greater than 97%), in the B- and T-cell compartments, attesting to satisfactory engraftment (not shown). This indicates that GCV administration can be delayed without losing therapeutic efficacy.
GVL effect obtained by delayed GCV administration.
(A) Experimental GVHD was induced by B6 TK T cells injected together with B6 TCD-BM cells in lethally irradiated B6 × D2 F1 recipient mice. Leukemic challenge was performed by intravenous injection of 2 × 103 P815 cells at the time of grafting. GCV was administered from day 6 to day 8 after graft (black square; n = 10); GVL effect was induced in GVHD mice receiving P815 cells and treated with GCV from day 3½ after graft (white square; n = 10) or from day 6 after graft (white circle; n = 10). One group of mice also received CsA treatment from day −2 until day 10 after the graft and GCV treatment from day 6 to day 8 (white triangle; n = 5). Results are presented as Kaplan-Meier survival curves of cumulative data of 2 independent experiments. (B) Histopathologic liver score after semiallogeneic BMT. Histopathologic examination and grading of GVHD of liver from mice were performed 65 to 75 days after transplantation. GCV was administered at day 6 (GCV d6-8; n = 10). Two groups of mice received P815 leukemia cells at the time of transplantation and were treated by GCV starting on day 3½ (P815 + GCV d3½-d5 1/2; n = 3) or day 6 (P815 + GCV d6-8; n = 8) after the graft, respectively. Histograms indicate the mean histopathological score for each group. The Fisher test was used for ANOVA; P < .05 for P815 + GCV d3½-5½ versus P815 + GCV d6-8.
GVL effect obtained by delayed GCV administration.
(A) Experimental GVHD was induced by B6 TK T cells injected together with B6 TCD-BM cells in lethally irradiated B6 × D2 F1 recipient mice. Leukemic challenge was performed by intravenous injection of 2 × 103 P815 cells at the time of grafting. GCV was administered from day 6 to day 8 after graft (black square; n = 10); GVL effect was induced in GVHD mice receiving P815 cells and treated with GCV from day 3½ after graft (white square; n = 10) or from day 6 after graft (white circle; n = 10). One group of mice also received CsA treatment from day −2 until day 10 after the graft and GCV treatment from day 6 to day 8 (white triangle; n = 5). Results are presented as Kaplan-Meier survival curves of cumulative data of 2 independent experiments. (B) Histopathologic liver score after semiallogeneic BMT. Histopathologic examination and grading of GVHD of liver from mice were performed 65 to 75 days after transplantation. GCV was administered at day 6 (GCV d6-8; n = 10). Two groups of mice received P815 leukemia cells at the time of transplantation and were treated by GCV starting on day 3½ (P815 + GCV d3½-d5 1/2; n = 3) or day 6 (P815 + GCV d6-8; n = 8) after the graft, respectively. Histograms indicate the mean histopathological score for each group. The Fisher test was used for ANOVA; P < .05 for P815 + GCV d3½-5½ versus P815 + GCV d6-8.
When GCV was administered at day 3½ to mice challenged with P815 leukemic cells, leukemia-associated mortality was significantly delayed compared with mice treated at day 1 (P < .05), although 7 of 10 mice still died of leukemia (Figure 4A). The 3 surviving mice had neither clinical signs of leukemia nor clinical or histopathological signs of GVHD (Figure 4B). When we further delayed GCV administration to day 6, only 2 of 10 mice died of leukemia. The 8 mice that survived until day 60 (P < .001 compared with mice treated by GCV at day 1) had no detectable leukemic cells in the peripheral blood at the end of the experiments (Figure5).
Detection of P815 leukemic cells in the peripheral blood of mice.
In mice that were protected from GVHD and that did not develop clinical signs of leukemia, peripheral blood cells were systematically collected and tested for the presence of P815 cells. On 3 of 3 and 8 of 8 protected mice treated at day 3½ or day 6, respectively, P815 cells were never detected more than 2 months after P815 cell injection, as illustrated here in a mouse treated at day 6.
Detection of P815 leukemic cells in the peripheral blood of mice.
In mice that were protected from GVHD and that did not develop clinical signs of leukemia, peripheral blood cells were systematically collected and tested for the presence of P815 cells. On 3 of 3 and 8 of 8 protected mice treated at day 3½ or day 6, respectively, P815 cells were never detected more than 2 months after P815 cell injection, as illustrated here in a mouse treated at day 6.
Taken together, these results indicate that by adjusting the modalities of GCV administration, one can obtain a potent GVL effect without compromising the protection against GVHD.
We also tested whether donor T cells with antileukemeic activity persisted after GCV treatment administered at day 6. Mice protected from GVHD and leukemia by the GCV-controlled GVHR were rechallenged with P815 cells at day 15. Four of 4 such mice developed and eventually died of leukemia.
Cyclosporin A impairs the GVL effect mediated by TK T cells after allogeneic BMT
CsA administered alone or in combination with methotrexate is the standard preventive treatment of GVHD.23 This immunosuppressive agent may, however, interfere with the antileukemic effect of donor TK T cells by inhibiting T-cell proliferation.24,25 We thus evaluated whether the presence of CsA before and during GCV administration had an impact on the GVL effect. To answer this question, CsA was administered from day 2 before transplantation until day 10 after BMT to mice receiving a 2-day GCV administration schedule starting at day 6 after BMT. Under these experimental conditions, we have recently demonstrated that CsA does not alter the capacity of GCV to control GVHD.26 In the present experiment, the GVL effect was dramatically altered in mice challenged with P815 cells, when compared with mice not receiving CsA. Indeed, 60% of mice treated with GCV and CsA developed typical signs of leukemia and died between day 23 and day 26 (Figure 4A). These results indicate that combining a CsA prophylactic treatment with the TK/GCV approach might result in the loss of the GVL effect.
Discussion
The GVL effect is one of the main benefits brought by donor T cells after allogeneic HSCT. The antileukemic activity of allogeneic donor T cells has been directly evidenced by remissions observed after donor lymphocyte infusions into patients experiencing relapse of hematological malignancies following allogeneic BMT.27-29 More recently, such a role for alloreactive T cells has also been shown in solid tumors after partial or complete regression of metastatic renal cell carcinoma was obtained in patients receiving allogeneic HSCT.30 These alloreactivity-based approaches have proven to be promising for the treatment of leukemia as well as solid tumors, although their usefulness remains limited by life-threatening GVHD. Here, we tested the efficacy of the TK/GCV strategy in preclinical conditions where a GVL effect is required. One of the main advantages of this TK/GCV strategy is its versatility and, in particular, the time-controlled delivery of the ablative signal, that is, GCV. Although few experimental data suggest that some GVL effect can be obtained independently of alloreactivity,31it is clear from numerous studies that, in most cases, the GVHR is likely to be the main driving force behind the GVL effect.1 We thus anticipated that an optimal GVL effect would be achieved only by allowing a limited GVHR to proceed. However, we have previously shown that delaying GCV administration beyond a certain time point can result in the appearance of an uncontrollable GVHD.21 We thus assessed the consequences of delaying and reducing GCV administration on both the GVHD and the GVL effect. We first observed that a 2-day GCV treatment administered at day 1 after transplantation was as efficient in eliminating alloreactive donor T cells and controling GVHD as our previous 7-day–long treatment. Starting this 2-day–long treatment at day 3½ or even at day 6, had no, or minimal, effect on its ability to control GVHD. Interestingly, when GCV was started at day 1, no GVL effect was observed. In contrast, when GCV was administered at day 3½, a significant GVL effect was observed, which was increased if the GCV administration was further delayed to day 6. These data indicate that in this model, the GVL effect is due mainly to donor T cells dividing within the first 6 days following transplantation, and is thus most probably mediated by alloreactive T cells. This is further demonstrated by the inability of remaining donor T cells to control leukemia relapse after a second challenge with P815 cells. It is thus possible that, after the GCV treatment, the immune repertoire contains reduced numbers of alloantigen-specific or leukemic antigen–specific GVL-mediating T cells capable of preventing late leukemia relapse. In this case, it will still be possible to perform delayed donor TK T cell infusion to mediate a GVL effect while controlling GVHD, as already evaluated in a clinical trial.32
The final question we studied in this work was whether the TK/GCV strategy should be associated with the standard prophylactic treatment of GVHD based on CsA. Indeed, there is theoretically a putative antagonism between the cytostatic effect exerted by CsA24,25 and the cell division–dependent destruction of alloreactive T cells mediated by the TK/GCV system. We recently observed that the efficacy of GCV in controlling GVHD was not affected by CsA administration, which could inhibit T-cell division for only 2 days. Thereafter, grafted T cells proliferated despite CsA and could be eliminated by GCV.26 The consequence of CsA administration on GVL when GVHD is controlled by the TK/GCV system remained to be determined. Here, we demonstrate that if CsA is administered during the first 6 days after HSCT before GCV is started, GVL is dramatically reduced. This indicates that the CsA-mediated inhibition of alloreactive T-cell activation during the first 2 days significantly reduced the potency of GVHR and thus GVL. Likewise, CsA administration, although not interfering with GCV-mediated control of GVHD, should preferably be delayed until the end of GCV administration.
Our data emphasize that, by a time-optimized scheduling, this therapeutic approach can be tuned to efficiently treat malignant hemopathies. The TK/GCV strategy for the control of GVHD has already been evaluated in clinical trials.33 One study concerned patients who received ex vivo–transduced donor TK T cell infusion for the treatment of relapse or Epstein-Barr virus (EBV)–induced lymphoproliferation occurring after TCD-allogeneic BMT.32 In another study, transduced T cells were administered with a TCD-allogeneic BMT.34 In both cases, GCV was administered to patients after they had developed GVHD. All together, in 6 of 7 patients, GCV administration was associated with complete or partial remission of GVHD. We have previously observed in mice that a course of GCV treatment sufficient to prevent GVHD was not able to completely reverse an advanced GVHD.21 We demonstrate here that an intermediate strategy can be proposed for the treatment of leukemia involving no GCV administration at the time of grafting to improve the GVL effect, followed by a systematic GCV treatment before the occurrence of clinical signs of GVHD. These data obtained in our experimental mouse model should now be translated to the clinical setting of allo-HSCT. Here, GVHR and GVL effects occurred in an MHC mismatch setting. Alloreactivity is therefore robust and probably has a more rapid onset than in HLA-matched situations. Given the variability of major and minor antigen discrepancies encountered in human HLA-matched or HLA-mismatched transplantation, it is presumable that a unique time frame for GCV administration may not apply to all donor-recipient pairs. Also, in our experiments, we used unmanipulated TK T cells from transgenic mice that presumably retain better immune function than T cells transduced ex vivo with a retroviral vector. All together, we have proved the concept that with the TK/GCV system, a time-controlled GVHR permits one to solve the dilemma of allo-HSCT: retaining GVL while controlling GVHD. The definition of appropriate therapeutic scheme(s) for human allo-HSCT can now be investigated only in clinical trials. We indeed are about to test different therapeutic schemes in HLA-matched or haplo-mismatched human HSCT, for the treatment of leukemia or severe autoimmune diseases.
We acknowledge Guillaume Gavori for technical assistance.
Prepublished online as Blood First Edition Paper, May 17, 2002; DOI 10.1182/blood-2002-01-0161.
Supported in part by Association Française contre les Myopathies, the University Pierre and Marie Curie (Paris V) Fondation de France “Leucémie,” and the Contre National de la Recherche Scientifique. E.L. is supported by l'Association pour la Recherche sur le Cancer.
E.L. and S.M. contributed equally to this work.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
David Klatzmann, CNRS/UPMC UMR 7087, Hôpital Pitié- Salpêtrière, 83, bd de l'Hôpital, F-75651 Paris Cedex 13, France; e-mail:david.klatzmann@chups.jussieu.fr.