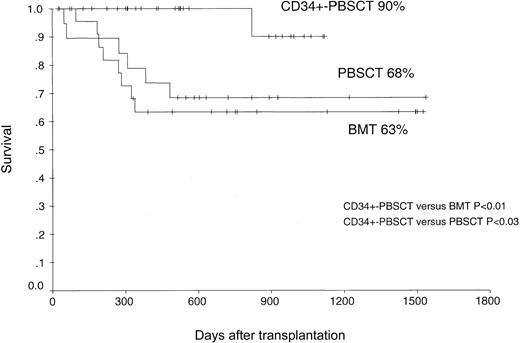
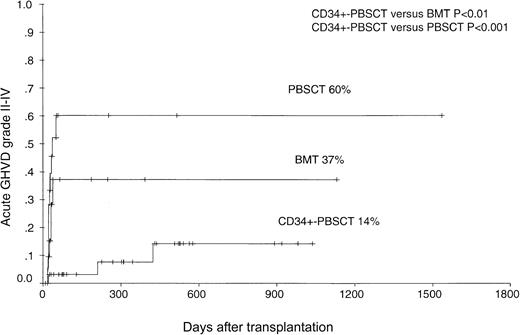
Outcomes of highly purified CD34+ peripheral blood stem cell transplantation (PBSCT) for chronic phase chronic myeloid leukemia (CML) (n = 32) were compared with those of PBSCT (n = 19) and of bone marrow transplantation (BMT) (n = 22) in the HLA-compatible sibling donor setting. Median follow-up was 18 months after CD34+-PBSCT and unmanipulated PBSCT and 20 months after BMT. CD34+-PBSCT was associated with delayed T-cell immune reconstitution at 3 months and 12 months after transplantation compared with PBSCT (P < .001) or BMT (not significant [NS]). The estimated probability of grades II to IV acute graft-versus-host disease (GVHD) was 60% ± 13% for the PBSCT group, 37% ± 13% for the BMT group, and only 14% ± 8% for the CD34+-PBSCT group (CD34-PBSCT versus BMT,P < .01; and CD34-PBSCT versus PBSCT,P < .001). The probabilities for molecular relapse were 88% for CD34+-PBSCT, 55% after BMT, and 37% after PBSCT (CD34+-PBSCT versus PBSCT,P < .03). Cytogenetic relapse probability was 58% after CD34+-PBSCT, 42% after BMT, and 28% after PBSCT (NS). After CD34+-PBSCT, 26 of 32 patients received a T-cell add-back. Hematologic relapse occurred in 4 of 22 patients after BMT, in 3 of 19 patients after PBSCT, and in only 1 of 32 patients after CD34+-PBSCT. The occurrence of a hematologic relapse in patients receiving CD34+-PBSC transplants was prevented by donor leukocyte infusions, which were applied at a median of 4 times (range, 1-7 times) with a median T-cell dose of 3.3 × 106 × kg/body weight [at a median] beginning at day 120 (range, 60-690 days). The estimated probability of 3-year survival after transplantation was 90% in the CD34+-PBSCT group, 68% in the PBSCT group, and 63% in the BMT group (CD34-PBSCT versus BMT, P < .01; and CD34-PBSCT versus PBSCT, P < .03). Transplantation of CD34+-PBSCs with T-cell add-back for patients with CML in first chronic phase seems to be safe and is an encouraging alternative transplant procedure to BMT or PBSCT.
Introduction
Acute graft-versus-host-disease (GVHD) is one of the major complications that affects the outcome of allogeneic transplantation. Mature alloreactive donor T cells cause acute GVHD reactions. T-cell depletion of the graft can reduce this complication effectively, but it is associated with an increased risk of leukemic relapse and graft failure, so that the outcome is very similar to that of unmanipulated allogeneic transplantation when bone marrow is used as the graft source.1-8
The use of granulocyte colony-stimulating factor (G-CSF)–mobilized peripheral blood stem cells and CD34+ selection as T-cell–depletion method offer the possibility to transfuse higher numbers of CD34+ cells and may thereby diminish the risk of graft failure. Moreover, the positive selection technique leads concomitantly to an effective depletion of T lymphocytes by 4 to 5 log10, which allows for omission of prophylactic posttransplantation immunosuppression.9 Additionally, a delayed donor lymphocyte add-back transfusion may reduce the risk of leukemic relapse.6 10 Thus, this transplantation method seems to be very promising in respect to reducing transplantation-related mortality. Nevertheless, the value of a new transplantation method may be determined only by comparing it to the standard transplantation methods of unmanipulated bone marrow transplantation (BMT) or unmanipulated peripheral blood stem cell transplantation (PBSCT).
In the present retrospective single-center study, we compare the clinical outcome of the CD34+-enriched PBSCT with delayed T-cell add-back with the outcome of unmanipulated BMT and PBSCT in patients with first chronic phase chronic myeloid leukemia (CML).
Patients and methods
Patients
All patients (n = 73) undergoing BMT (n = 22), PBSCT (n = 19), or CD34+ highly purified PBSCT (n = 32) in the first chronic phase of CML from genotypically HLA-identical sibling donors at the University Hospital of Essen, Germany, between September 1997 and December 2001 were consecutively included in the present study. All aspects of this study were approved by the Institutional Review Board on Medical Ethics at the University Hospital Essen.
Assignment to the transplantation procedures
All patients were informed in detail about the 3 different transplantation procedures (BMT, unselected PBSCT, and CD34+-PBSCT) before transplantation. Patients who intended to undergo CD34+-PBSCT were informed of the need to participate in a phase 2 study investigating the feasibility of highly purified CD34+ cell transplantation. Including criteria for this study were to have documented CML in chronic phase, to have an HLA-identical sibling donor, and to be older than 18 years of age for patients and donors. These patients were asked for a written informed consent before participating in the study. Patients were offered preferentially blood stem cell transplants (CD34+-PBSCT or unselected PBSCT) when a history of documented serious infectious complications in the 6 months before the transplantation was found or organ functional impairment of the donor precluded anesthesia or marrow harvest. These criteria were fulfilled by only 3 patients. Three patients with a history of renal insufficiency were offered a CD34+-PBSCT without prophylactic posttransplantation immunosuppression in order to avoid a long-term cyclosporine A application. All other patients and donors could freely choose the transplantation procedures or the way of donation of stem cell source. There were no other criteria for assignment of the patients to the study groups. The analyses of the study were done retrospectively.
All transplantations were performed in reverse isolation rooms equipped with high-efficiency particle air filtration systems (HEPA), and all patients received prophylactic metronidazole, ciprofloxacin, and fluconazole. Patients who were discharged after transplantation were enrolled in our long-term follow-up program. Outpatient visits were performed at least monthly during the first 6 months and at 3-month intervals thereafter during the first 2 years after transplantation. After 2 years, patients usually were seen at yearly intervals.
Conditioning regimen
The conditioning regimen consisted of intravenous cyclophosphamide (60 mg/kg of body weight [BW] per day × 2) in combination with fractioned total body irradiation (TBI) delivered by a 60cobalt source in 4 daily fractions of 2.5 Gy (n = 40), or oral busulfan (BU) (1 mg/kg of BW every 6 hours over 4 days) in combination with intravenous cyclophosphamide (60 mg/kg of BW per day × 2) (n = 2). Patients who were scheduled for CD34+-PBSCT received a conditioning regimen with fractioned TBI, cyclophosphamide (60 mg/kg of BW per day × 2), and thiotepa (5 mg/kg of BW per day × 2) with (n = 26) or without (rabbit) anti–T-lymphocyte globuline (ATG) (10 mg/kg of BW for 4 days) (n = 5). ATG was purchased from Fresenius (ATG-S, Fresenius, Bad Homburg, Germany).
All blood products were irradiated (30 Gy) and leukocyte-depleted throughout the posttransplantation course. GVHD prophylaxis consisted of intravenous methotrexate (15 mg/m2, day 1; 10 mg/m2, days 3, 6, and 11) in combination with continuous intravenous cyclosporine in patients who received an unmanipulated graft (n = 41). In the patients who underwent a CD34+-PBSCT, no further GVHD prophylaxis was given.
Patient demographics are summarized in Table1.
Donors
All donors were HLA-identical at the A, B, DRB1, and DQB1 loci with their respective recipients. All PBSC donors received a G-CSF at a dose of 16 μg/kg/d, administered subcutaneously daily for 5 to 6 consecutive days. If the first apheresis procedure resulted in the collection of fewer than 5.0 × 106 CD34+cells per kilogram of the recipient's body weight, a second apheresis procedure was performed the following day.
Magnetic-activated cell separation (MACS)
CD34+ cells were positive-selected with anti-CD34 antibody conjugated to iron-dextran microbeads using the CliniMACS device (Miltenyi Biotech, Bergisch Gladbach, Germany), as earlier described.9
Quantitation of CD34+ cells and peripheral blood cell subsets
CD34+ cell determinations were performed on bone marrow and leukapheresis products. Peripheral blood cell subsets were determined by flow cytometry, as previously described.11
Clinical evaluation
Neutrophil engraftment was defined as the first of 3 consecutive days with an absolute neutrophil count (ANC) greater than 0.5 × 109/L. Platelet engraftment was defined as the first day of a platelet count greater than 20 × 109/L or 50 × 109/L without platelet transfusions. Acute GVHD was graded according to standard criteria.12 Chronic GVHD was assessed in patients alive after day 90. Cytomegalovirus (CMV) reactivation was determined weekly by pp65 antigenemia in blood leukocytes. Transplantation-related mortality (TRM) was defined as death with no relapse. Disease-free survival (DFS) was defined as survival without hematologic relapse.
Minimal residual disease (MRD) detection by quantitative real-time RT-PCR and chimerism analysis
Isolation of mRNA and real-time reverse transcriptase–polymerase chain reaction (RT-PCR) for the bcr-abl transcript were performed on peripheral blood cells and bone marrow buffy coat cells, as described earlier.13 The real-time RT-PCR assay has a sensitivity of 0.0001%.13 A molecular relapse was defined as the detection of 2 consecutive positive PCR assays within a 4-week interval, without regard to the level of measured quantitative bcr-abl/gapdh quotient.
Blood samples were evaluated monthly in the first 6 months and at 3-month intervals thereafter during the first 2 years after transplantation. After 2 years, patients without evidence of molecular or cytogenetic relapse were evaluated once per year. A total of 560 samples (blood or bone marrow) were evaluable.
Chimerism analysis
Chimerism analyses were performed on patients with sex-mismatched donors by interphase fluorescent in-situ hybridization (FISH) with X and Y probes (Vysis, Downers Grove, IL), according to the manufacturer's instructions. Chimerism of patients with sex-matched donors were analyzed by variable number of tandem repeats (VNTR)–PCR as published earlier.14Chimerism analyses were performed at 6-week intervals on CD34+-PBSCT patients only, except in the case of relapse, when they were also performed on BMT or PBSCT patients.
Definition of relapse
Hematologic relapse was diagnosed on the basis of standard hematologic criteria. An isolated cytogenetic relapse was assumed if after a period of negativity, Ph1-positive metaphases were detected in a cytogenetic analysis without evidence of hematologic disease. For the diagnosis of molecular relapse or persistence, only those bcr-abl–positive real-time RT-PCR results that were confirmed on a consecutive real-time RT-PCR assay within a 4-week interval were considered positive.
Statistics
Cumulative estimates (± standard error) were calculated with the use of the Kaplan-Meier method.15 Differences between time-to-event distribution functions were compared by a log-rank test (Mantel-Haenszel).16 A stepwise proportional hazards general linear model (PHGLM) analysis was used to evaluate interactions of different covariates on the analytic end point of TRM. Covariates in PHGLM analysis were stratified according to time between diagnosis and transplantation (≤ 12 months or > 12 months), patient age (≤ 40 or > 40 years), sex constellation (male recipient with female donor or other), and occurrence of acute (grades I-IV) and chronic GVHD. Conditional risk ratios (RR) and their 95% confidence intervals (95% CI) were derived from PHGLM analysis after adjustment for significant covariates in the model. Differences between the groups concerning the number of cells administered, time to engraftment, number of transfusions, and number of peripheral blood mononuclear cell subsets were evaluated with the use of a 2-samplet test and the Mann-Whitney U test.
Only patients surviving more than 30 days were included in the analysis of acute GVHD. A minimum of 90 days of follow-up was the criterion for chronic GVHD.
Results
Performance of the CD34+ stem cell transplants
After MACS, CD34+ cells were recovered at a median of 59.7% (range, 46.4%-72.1%). A purity of 97.2% (median) of CD34+ cells in the graft were achieved (range, 94.5%-98.3%). The T cells were depleted after MACS separation at a median of 4.6 × 10log times (range, 3.8-5.0 × 10log). Mononuclear cells (MNCs) and CD34+ cells were significantly higher in the PBSC leukapheresis products than in the bone marrow products (P < .001, Table 1).
Time to engraftment and transfusion requirements
Absolute neutrophil counts exceeded 500/μL 5 days earlier in the CD34+-PBSC recipients than in the PBSC recipients, and 10 days earlier than in the BM recipients (CD34-PBSCT versus BMT,P < .001; and CD34-PBSCT versus PBSCT,P < .01, Table 2). Similarly, platelet counts exceeded 50 000/μL, without need for transfusions, 3 days earlier in the CD34+-PBSC recipients than in the PBSC recipients, and 9 days earlier than in the BM recipients (CD34-PBSCT versus BMT, P < .02). The first 24 patients of the 32 who underwent CD34+-PBSCT received G-CSF after transplantation, whereas only 2 patients after PBSCT and only 4 patients after BMT received G-CSF.
The number of transfused units of platelets and of red cells did not differ significantly in all groups.
Immune reconstitution 3 and 12 months after transplantation
Peripheral blood CD3+CD4+ T cells were significantly lower 3 and 12 months after CD34+-PBSCT compared with PBSCT (P < .001 [3 months] andP < .06 [12 months]) and lower compared with BMT (NS) (Table 3). These differences were also seen for CD3+CD4+ subsets (naive T helper cells and memory T helper cells) 3 months after transplantation (Table 3). In contrast, the level of CD19+ B cells was more than 10 times higher in patients receiving CD34+-PBSCs than in patients receiving PBSCs (P < .001) or BMT (P < .001) 3 months after transplantation and remained higher 12 months after transplantation (CD34-PBSCT versus BMT and CD34-PBSCT versus PBSCT, P < .01). Further, patients receiving CD34+-PBSCs had a higher level of natural killer (NK) cells 3 months after transplantation compared with patients receiving PBSCs or BM. The level of monocytes, CD8+, and CD19+ cells did not differ significantly after CD34+-PBSCT, PBSCT, and BMT (Table 3). Although the CD4/CD8 ratio was lower after CD34+-PBSCT (mean 0.45 after CD34+-PBSCT versus 0.6 and 0.66 after BMT and PBSCT, respectively) 3 months after transplantation, the differences were not significant.
Acute and chronic GVHD
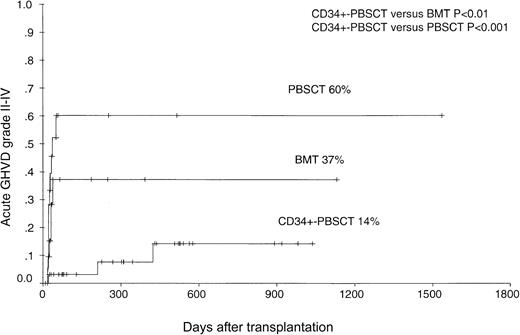
The cumulative incidence of grade I-IV acute GVHD was lowest at 39% after CD34+-PBSCT compared with 89% after PBSCT (P < .001) and 88% after BMT (P < .001). The estimated probability of grade II-IV acute GVHD was 60% ± 13% for the PBSCT group, 37% ± 13% for the BMT group, and only 14% ± 8% for the CD34+-PBSCT group (CD34-PBSCT versus PBSCT,P < .001 and CD34-PBSCT versus BMT,P < .01, Figure1).
The probability of the occurrence of grade II-IV acute GVHD in patients after PBSCT, BMT, or CD34+-PBSCT from sibling donors.
The probability of the occurrence of grade II-IV acute GVHD in patients after PBSCT, BMT, or CD34+-PBSCT from sibling donors.
Chronic GVHD occurred in 11 of 22 patients assigned to receive BM and 10 of 19 patients assigned to receive PBSCs, compared with 6 of 29 evaluable patients of those assigned to receive CD34+-PBSCs (Table 2). The estimated probability of (limited and extensive) chronic GVHD 3 years after transplantation was 56% in the PBSC group, 50% in the BMT group, and 36% in the CD34+-PBSCT (CD34-PBSCT versus BMT, P < .03 and CD34-PBSCT versus PBSCT, P < .01).
Molecular, cytogenetic, and hematologic relapse
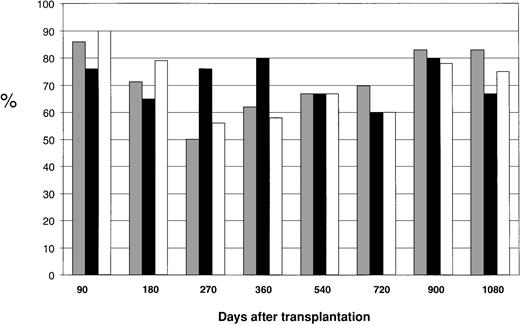
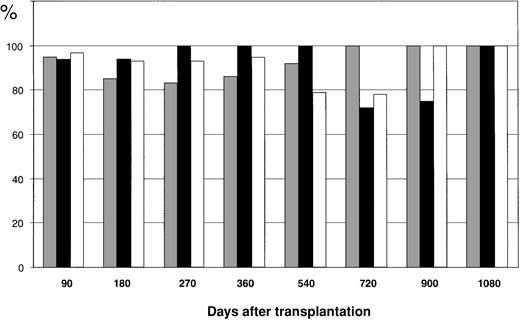
According to the applied definition of molecular relapse, a repeatedly positive bcr-abl–PCR assay within a 4-week interval was detectable in 11 of 22 patients (50%) after BMT, in 6 of 19 (32%) after PBSCT, and in 25 of 32 patients (78%) after CD34+-PBSCT (NS). The 18-month estimated probability of molecular relapse was 55% ± 11% after BMT, 37% ± 12% after PBSCT, and 88% after CD34+-PBSCT (CD34-PBSCT versus PBSCT,P < .03). Because T-cell add-back or withdrawal of immunosuppression or interferon-alfa therapies could induce molecular remissions in patients with a molecular relapse of CML again, we evaluated the proportion of patients in molecular remission at different time periods after transplantation. Figure2 shows the proportion of patients in molecular remission at several time periods from 90 days to 1080 days after transplantation considering the influence of antileukemic therapies. There were no significant differences between the 3 transplantation procedures at different time periods after transplantation.
The proportion of patients in molecular remission at different time periods (90, 180, 270, 360, 540, 720, 900, and 1080 days) after PBSCT, BMT, or CD34+-PBSCT from sibling donors.
░ represents BMT patients; ▪, PBSCT patients; and ■, CD34+-PBSCT patients. The number of evaluated patients was 71 at day 90 and 15 at day 1080.
The proportion of patients in molecular remission at different time periods (90, 180, 270, 360, 540, 720, 900, and 1080 days) after PBSCT, BMT, or CD34+-PBSCT from sibling donors.
░ represents BMT patients; ▪, PBSCT patients; and ■, CD34+-PBSCT patients. The number of evaluated patients was 71 at day 90 and 15 at day 1080.
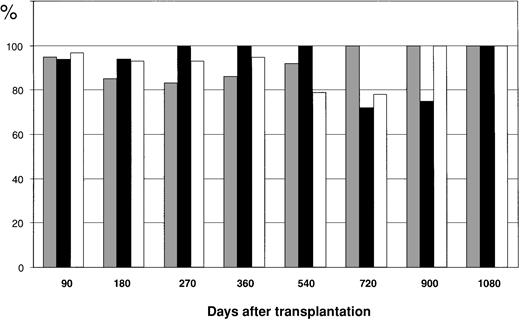
Cytogenetic relapse occurred in 6 of 22 patients after BMT (27%), in 3 of 19 patients after PBSCT (16%), and in 6 of 32 patients after CD34+-PBSCT (19%). Similarly, the 3-year estimated probability of cytogenetic relapse was 42% ± 13% after BMT, 28% ± 15% after PBSCT, and 58% ± 17% after CD34+-PBSCT (NS). Figure 3 shows the proportion of patients in cytogenetic remission at different time periods between 90 days and 1080 days after transplantation considering the influence of antileukemic procedures such as T-cell add-back, which shows no significant differences between the 3 transplant groups.
The proportion of patients in cytogenetic remission at different time periods (90, 180, 270, 360, 540, 720, 900, and 1080 days) after PBSCT, BMT, or CD34+-PBSCT from sibling donors.
░ represents BMT patients; ▪, PBSCT patients; and ■, CD34+-PBSCT patients. The number of evaluated patients was 71 at day 90 and 15 at day 1080.
The proportion of patients in cytogenetic remission at different time periods (90, 180, 270, 360, 540, 720, 900, and 1080 days) after PBSCT, BMT, or CD34+-PBSCT from sibling donors.
░ represents BMT patients; ▪, PBSCT patients; and ■, CD34+-PBSCT patients. The number of evaluated patients was 71 at day 90 and 15 at day 1080.
Hematologic relapse was found in 4 of 22 patients after BMT (18%), in 3 of 19 patients after PBSCT (16%), and in 1 of 32 patients after CD34+-PBSCT (3%). The 3-year estimated probability of hematologic relapse was 24% ± 11% after BMT, 29% ± 15% after PBSCT, and 6% ± 4% after CD34+-PBSCT.
Chimerism analysis 3 months after transplantation in patients receiving CD34+-PBSCs
Chimerism analyses were performed in 28 of the 32 patients undergoing CD34+-PBSCT. Of these, 13 patients were analyzed by XY-FISH and 11 patients by VNTR-PCR. Only 5 of 28 evaluated patients receiving CD34+-PBSCs (18%) had a complete chimerism. The proportion of autologous hematopoiesis detected by XY-FISH in patients 3 months after transplantation was 17% (median, range, 0%-100%).
Four patients had decreasing proportions of donor hematopoiesis (minimum at median, 28.2%) without increasing bcr-abl titer in the real-time RT PCR assay (data not shown). After application of donor leukocyte infusions (DLIs) to 3 patients, the proportion of donor hematopoiesis increased again at a median of 99%.
T-cell add-back to treat relapse and prevent graft rejection in patients after CD34+-PBSCT
DLIs were given to 26 of 32 patients who underwent CD34+-PBSCT at a median of 120 days after transplantation (range, 60-690 days). DLIs were given at a median of 4 times (range, 1-7 times) in increasing T-cell doses starting at 1 × 105 T cells/kg/BW of recipients with a median of 3 × 106 T cells/kg/BW (range, 3 × 104 to 3 × 107 T cells/kg/BW). DLIs were applied to the first 12 patients initially only in case of the occurrence of a molecular or cytogenetic relapse. Thereafter, DLIs were given systematically to prevent relapse in the following patients regardless of their MRD status at day 90 with a starting T-cell dose of 3 × 105T cells/kg/BW, followed by a second application of 1 × 106 T cells/kg/BW at day 135 after transplantation. Thereafter, further DLIs were given only in case of persisting or new occurrence of a positive PCR test for bcr-abl.
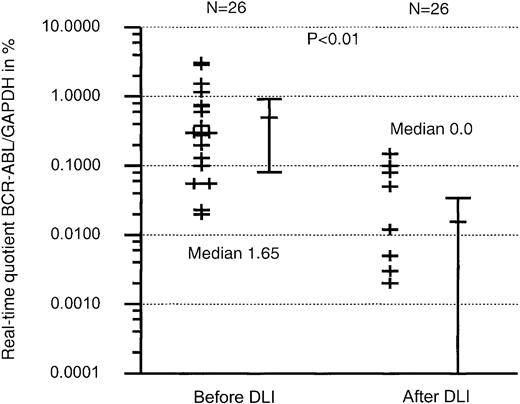
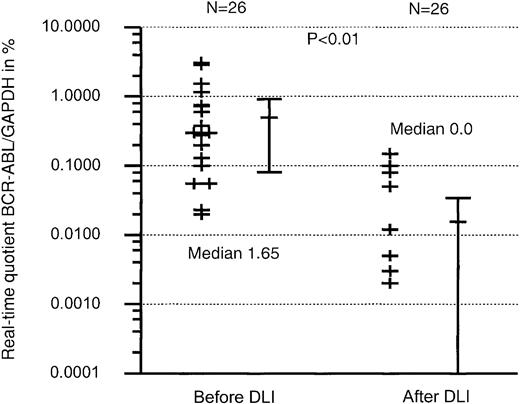
After DLIs were applied, 14 of the 22 patients with a molecular relapse and 5 of 6 patients with a cytogenetic relapse achieved a molecular or cytogenetic remission again. The quantitative bcr-abl amount, defined as the quotient of bcr-abl/glyceraldehyde phosphate dehydrogenase (GAPDH), decreased from 1.65 (range, 0%-3.1%) to under detectable levels of real time RT-PCR (0%, range, 0%-0.15%) as shown in Figure 4. In 3 cases DLIs were given to patients who had a decreasing proportion of donor chimerism in the unfractioned leukocyte analysis (n = 2) and in the T-cell chimerism analysis (n = 3) to prevent graft rejection. Only one patient who did not receive DLIs developed a secondary graft rejection. This patient received another transplant successfully from the same donor.
The real-time quotient (BCR-ABL/GAPDH) in percentage before and after DLIs were applied in patients receiving CD34+-PBSCs.
The real-time quotient (BCR-ABL/GAPDH) in percentage before and after DLIs were applied in patients receiving CD34+-PBSCs.
Withdrawal of immunosuppression, DLIs, and interferon-alfa therapy in patients with molecular or cytogenetic relapse after BMT or PBSCT
Eight patients in molecular relapse of CML after PBSCT (n = 3) or BMT (n = 5) were treated by withdrawal of immunosuppression (n = 7) or interferon-alfa (n = 1). All patients achieved a molecular remission of CML. But only 5 of these 8 patients achieved a sustained molecular remission, whereas 3 other patients again developed a molecular relapse after a median of 6 months. These patients were further treated with interferon-alfa. All 3 patients in cytogenetic relapse of CML after BMT (n = 2) or PBSCT (n = 1) achieved a cytogenetic remission after the immunosuppression was tapered or withdrawn (n = 2) or interferon-alfa (n = 1) was applied.
Of 6 patients in hematologic relapse, 5 achieved a cytogenetic remission again after treatment with DLIs and interferon (n = 4) or imatinib mesylate (n = 2). One patient who relapsed in blast crises of CML did not respond to any of these treatment modalities. This patient died from her CML in blast crises.
The quantitative bcr-abl amount of all patients after PBSCT or BMT decreased from 2.8% at median (range, 0.05%-153%) to 0.002% of real time RT-PCR (median, range, 0%-50%).
Rates of death and survival, long-term immunosuppression
Of the 22 patients assigned to receive bone marrow (BM), 8 (36%) died, and of the 19 patients assigned to receive unmanipulated PBSCs, 6 (32%) died, compared with 1 of 32 patients in the CD34+-PBSCT group (3%). In the CD34+-PBSCT group, one patient died from a metastasic prostate cancer at day 822 after transplantation. The predominant causes of death in the BM and PBSC groups were infections and severe acute GVHD (Table4). The estimated probability of transplantation-related death at 3 years after transplantation was 32% ± 10% (± standard error) in the BMT group and 32% ± 9% in the PBSCT group, compared with 10% ± 9% in the CD34+-PBSCT group (P < .03). This resulted in an estimated probability of a 3-year-survival of 63% for patients in the BMT group, of 68% in the PBSCT group, and 90% in the CD34+-PBSCT group (CD34-PBSCT versus BMT,P < .01; and CD34-PBSCT versus PBSCT,P < .03) (Figure 5). The estimated probability of DFS as defined to remain in continuous hematologic remission was 70% in the CD34+-PBSCT group, 52% in the PBSCT group, and 53% in the BMT group (CD34-PBSCT versus BMT or versus PBSCT, P < .03).
Overall survival of patients after PBSCT, BMT, or CD34+-PBSCT from sibling donors.
Overall survival of patients after PBSCT, BMT, or CD34+-PBSCT from sibling donors.
After PBSCT, 7 of 13 patients received a long-term immunosuppression at time of analysis; after BMT, only 1 of 14; and after CD34+-PBSCT, 1 of 31.
Multivariate analysis for TRM
For TRM, the time from diagnosis to transplantation (≤ 12 months or > 12 months), age (≤ 40 or > 40 years), sex constellation (male recipient with female donor or other), and acute and chronic GVHD were analyzed. Only acute GVHD influenced TRM significantly (P < .001).
Discussion
As expected and in concordance with studies about other T-cell–depleted transplant procedures, the rates of acute and chronic GVHD were significantly lower in the group that received CD34+-PBSCs than in the BM group or PBSC group.6-8,17 Acute and chronic GVHD occurred mostly after DLIs were applied to patients receiving highly purified CD34+ cell transplants. The estimated probability of acute grades II-IV GVHD was only 14% after CD34+-PBSCT compared with 60% after PBSCT (P < .001) and 37% after BMT (P < .01). The incidence of acute GVHD in patients after CD34+-PBSCT in our study was in the range of that for T-cell–depleted BMT reported by others in CML patients in chronic phase.7,8 17
Patients receiving transplants of highly purified CD34+cells had a faster neutrophil and platelet recovery than patients receiving bone marrow or PBSC transplants, which might be associated with the omission of posttransplantation prophylactic immunosuppression and the application of G-CSF after transplantation to most of the patients in this study group. The administration of G-CSF after transplantation was given only in the first 24 of 32 patients receiving CD34-PBSCs, and thereafter not continued due to a study by Volpi and coworker reporting that postgrafting administration of G-CSF impairs functional immune recovery in patients receiving HLA haplotype mismatched grafts.18
However, the number of platelets and red blood cells did not differ significantly after CD34+-PBSCT compared to the BM group or the PBSC group.
In agreement with earlier published studies about T-cell–depleted BMT, we found a documented slower numeric T-cell reconstitution in patients who received a CD34+-PBSC transplant than in patients receiving BM or PBSCs.19,20 Compared with patients who received BM or PBSC transplants, CD34+-PBSC recipients had peripheral blood naive (CD4+CD45RA+) and memory (CD4+CD45RO+) T helper cells that were significantly lower at 3 and 12 months after transplantation. But surprisingly, the number of B cells was about 10 times higher at 3 months after transplantation than it was in patients after BMT or PBSCT and remained significantly higher at 12 months after transplantation. This might be caused by the fact that in contrast to patients after CD34+-PBSCT, patients after BMT or PBSCT receive posttransplantation immunosuppression with cyclosporine. Rapid B-cell recovery after T-cell–depleted BMT using Campath-1 was described already earlier by Parreira and coworkers.20
The delayed T-cell immune reconstitution after CD34+-PBSCT was not associated with an increased risk for infectious complications. So far, none of the 32 patients receiving CD34+-PBSCs died from opportunistic infections after transplantation, which resulted in an overall low transplantation-related mortality and a probability of survival of 90% at 3 years, whereas the transplantation-related mortality in patients after BMT and PBSCT were in the expected field of 30%, resulting in a probability of 3-year survival of 68% after PBSCT and of 63% after BMT (CD34-PBSCT versus BMT, P < .01 and CD34-PBSCT versus PBSCT,P < .03). A multivariate analysis for TRM identified the occurrence of acute GVHD as the only independent predictor for TRM.
Other study groups did not confirm that T-cell–depleted transplant procedures result in an improved survival when compared to non–T-cell transplant procedures.6-8 In most studies, patients died from graft rejections, relapse, or opportunistic infections.6-8 Only Drobyski and coworkers have described similar results of about 80% 5-year survival after T-cell–depleted BMT for patients with CML in chronic phase.21 Although the T-cell depletion procedures varied between the studies, which makes comparisons difficult, there are a few major differences between the published studies and the present one. First, we intensified the conditioning therapy consisting of TBI and cyclophosphamide by adding thiotepa in patients who received CD34+-PBSCs in order to increase the antileukemic effect. Second, we transfused a higher number of CD34+ stem cells than described in most other T-cell–depleted BMT procedures in order to reduce the risk of graft failures. This did not negatively effect the outcome of patients in our study, in contrast to a study published recently.22 Third, we omitted posttransplantation prophylactic immunosuppression, which probably resulted in an improved immune reconstitution compared with other T-cell–depleted transplant procedures. Further, we have performed a T-cell add-back in most of the patients receiving a highly purified CD34+ cell transplant to reduce the risk of relapse.
T-cell–depleted stem cell transplantations are associated with an increased risk of graft failures.4,5 The risk for graft failures correlates with the number of donor T cells in the transplant. Urbano-Ispizua and coworkers found that the probability of graft failures increased up to 18% when the number of T cells declined to 2 × 105/kg of the recipient's body weight.23 Although the number of donor T cells in the transplants of CD34+-PBSCT in our study was lower than 2 × 105/kg, we did not experience that high number of patients with graft failures after CD34+-PSBCT. However, we observed a decreasing donor chimerism in 4 patients without increasing bcr-abl titer in the real-time RT-PCR within the first 3 months after transplantation. One of these patients consecutively suffered from a second transplantation failure and had to receive another transplant with unmanipulated stem cells from the origin donor, whereas in the remaining 3 patients a secondary graft failure might have been prevented by the application of DLI with increasing T-cell doses.
Many study groups reported that there is an increased risk for leukemic relapse in patients who underwent T-cell–depleted bone marrow or blood stem cell transplantation.5 10 In concordance with these observations, we also found here an increased risk for a molecular or cytogenetic relapse in patients who underwent CD34+-PBSCT compared with patients who underwent BMT or unselected PBSCT. But the progression of molecular or cytogenetic relapse to hematologic relapse might be prevented due to the T-cell add-back policy here, in all cases except one. In the first 4 of 26 patients receiving DLIs, T cells were given at a starting dose of 1 × 107/kg/BW, which resulted in the occurrence of a GVHD grade III in one case with a need for immunosuppressive therapy with prednisolone and cyclosporine. But when reducing the starting T-cell dose to 3.3 × 105/kg/BW, GVHD no longer occurred. At the beginning, only patients (n = 15) with a molecular or cytogenetic relapse or increasing mixed chimerism proportions were treated with DLIs. Thereafter, DLIs were given to 10 patients at day 90 after transplantation regardless of the minimal residual disease and chimerism status.
The response to DLI is pronounced in patients in the early stages of CML relapse, for example, molecular or cytogenetic relapse, compared to patients with more advanced disease stages. The use of a quantitative real-time PCR assay, which has been shown to correlate bcr-abl titers to disease stages,13 enabled us to diagnose relapses of CML early and apply DLIs very soon. However, the antileukemic effect of DLIs may also be more intensive in patients receiving T-cell–depleted transplants, who did not experience the allogeneic T-cell reactions within the transplantation procedure compared with patients receiving a non–T-cell–depleted transplant as described earlier.24 This point, together with the early diagnosis of relapse, might be the reason that up to the date of analysis, hematologic relapse has been prevented in all but one study patient.
The application of DLI with increasing T-cell doses was first described by Mackinnon and coworkers as a safe way to induce an antileukemic immune reaction without inducing severe GVHD.10 A low initial DLI dose recently has been shown to be similarly effective as higher DLI doses without causing acute GVHD.
Almost all of the patients with molecular or cytogenetic relapse after unselected PBSCT or BMT were successfully treated by withdrawal of immunosuppression, interferon-alfa therapy, or DLI. Withdrawal of immunosuppression was applied first in patients who received an immunosuppressive therapy to treat or prevent GVHD. Patients who did not receive any immunosuppression or did not respond to the withdrawal of immunosuppression by achieving a remission were treated by interferon-alfa or DLIs. Treatment criteria for patients in molecular relapse was an increasing quantitative bcr-abl titer measured by real-time PCR.
Despite the positive results of therapy with the tyrosine kinase inhibitor imatinib mesylate in patients with CML,25,26allogeneic CD34+-PBSCT from HLA-identical sibling donors might offer a therapeutic option with a durable antileukemic effect, which may also result in improved DFS. As shown recently, patients with CML who receive transplants from an HLA-identical unrelated donor have a low transplantation-related mortality.27 Thus, allogeneic transplantations remain the option with the best antileukemic effect for CML patients with a compatible related or unrelated donor. Our data support the notion that CML patients with a compatible donor for whom cure is the chief objective should undergo allogeneic stem cell transplantation as stated earlier by us and others.27 28Prospective randomized trials comparing CD34+-PBSCT and PBSCT or BMT in patients with first chronic phase CML are required to further substantiate the differences in the evaluation of survival and TRM.
The authors thank Katja Ahrens, Melanie Kroll, and Ines Riepenhoff for their excellent technical performance of the PCR analyses, and Martina Franke, Ramona Dittloff, and Ines Krimphoff for their flow cytometric studies.
Prepublished online as Blood First Edition Paper, September 12, 2002; DOI 10.1182/blood-2002-05-1615.
Ulrich W. Schaefer died on August 18, 2002.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
A. H. Elmaagacli, Department of Bone Marrow Transplantation, University Hospital Essen, Hufelandstr 55, 45122 Essen, Germany; e-mail:ahmet.elmaagacli@uni-essen.de.