Abstract
The steps to leukemia following an in utero fusion ofMLL (HRX, ALL-1) to a partner gene in humans are not known. Introduction of the Mll-AF9 fusion gene into embryonic stem cells results in leukemia in mice with cell-type specificity similar to humans. In this study we used myeloid colony assays, immunophenotyping, and transplantation to evaluate myelopoiesis in Mll-AF9 mice. Colony assays demonstrated that both prenatal and postnatal Mll-AF9 tissues have significantly increased numbers of CD11b+/CD117+/Gr-1+/− myeloid cells, often in compact clusters. The self-renewal capacity of prenatal myeloid progenitors was found to decrease following serial replating of colony-forming cells. In contrast, early postnatal myeloid progenitors increased following replating; however, the enhanced self-renewal of early postnatal myeloid progenitor cells was limited and did not result in long-term cell lines or leukemia in vivo. Unlimited replating, long-term CD11b/Gr-1+ myeloid cell lines, and the ability to produce early leukemia in vivo in transplantation experiments, were found only in mice with overt leukemia. Prenatal Mll-AF9tissues had reduced total (mature and progenitor) CD11b/Gr-1+ cells compared with wild-type tissues. Colony replating, immunophenotyping, and cytochemistry suggest that any perturbation of cellular differentiation from the prenatal stage onward is partial and largely reversible. We describe a novel informative in vitro and in vivo model system that permits study of the stages in the pathogenesis of Mll fusion gene leukemia, beginning in prenatal myeloid cells, progressing to a second stage in the postnatal period and, finally, resulting in overt leukemia in adult animals.
Introduction
Leukemia associated with the fusion of a portion of the MLL (HRX, ALL-1) gene to a portion of a partner gene is the most frequent leukemia in human infants and is found in adults also.1,2 The amino-terminal portion ofMLL can partner with more than 30 different genes to form various fusion genes.3 Evidence that MLL fusion genes often form in utero in humans is derived from studies of identical twins and studies of DNA collected at birth.4,5The Mll-AF9 fusion gene introduced into embryonic stem (ES) cells by homologous recombination results in leukemia in adult mice with cell-type specificity similar to that seen in humans.6 7 Leukemia develops in Mll-AF9 mice with a 5- to 6-month delay. However, the prenatal and postnatal steps in the pathogenesis of MLL fusion gene leukemia are not defined. In this study we initiated studies to evaluate the possibility of a sequential multistep pathogenesis.
Both human MLL-AF9 and murine Mll-AF9 leukemias are most frequently myeloid in phenotype.1,7 Here we studied fetal and postnatal myeloid cells to evaluate the early stages of Mll-AF9 fusion gene–induced cellular abnormalities. Myelopoiesis is active in mammalian fetal tissues.8-10 In the present study, fetal liver and bone marrow were compared with bone marrow early after birth and later in adult mice with overt leukemia. Our results are the first to report a model system to characterize prenatal and postnatal abnormalities that result from early introduction of an Mll fusion gene.
Materials and methods
Mice
Heterozygous Mll-AF9+/− mice were produced by targeting the human AF9 short form into exon 8 of the mouse Mll gene. Strain CCB ES cells were transfected with the Mll-AF9 targeting vector. Homologous recombination and confirmation of the presence of a single insertion site were as previously described.6 Heterozygous mice were obtained by crossing chimeric males with wild-type females. Mice designatedMll-AF9 in this study were allMll-AF9+/−. Genomic DNA was extracted from murine tissue. Polymerase chain reaction (PCR) was used to distinguishMll-AF+/− fromMll-AF9−/− mice by a 247–base pair (bp) product of the Mll-AF9 fusion gene. The sense primer sequence is 5′-GTGGGAGATGGGAGGCTT-3′; the antisense primer sequence is 5′-TTGTCCAGCGAGCAAAGA-3′. PCR was carried out in a 50 μL volume with 20 pmol of each primer, 25 nmol of each of the deoxyribonucleoside triphosphates (dNTPs), 1 μL titanium Taq DNA polymerase (Clontech, Palo Alto, CA), and 20 to 80 ng of extracted genomic DNA.
Preparation and fluorescence-activated cell-sorting (FACS) immunophenotyping of fetal liver and bone marrow
Fetal liver was obtained from embryonic day (E) 13.5 mice. Single-cell suspensions were obtained using a 21-gauge needle and syringe; red blood cells were hypotonically lysed with water and cells passed through a 70-μm cell strainer to remove debris. Bone marrow was obtained from day-6 mice by grinding the femur and tibia in media using a mortar and pestle. Cells in suspension were prepared for flow cytometric analysis. Fetal liver cells or 6-day bone marrow cells were incubated at 4°C for at least 5 minutes with CD16/CD32 Fc block (BD PharMingen, San Diego, CA) and subsequently stained with specific antibody or matching isotype control antibody for at least 30 minutes on ice. Cells were washed twice with fluorescence-activated cell sorter (FACS) buffer containing 10% fetal bovine serum and 0.2% sodium azide and fixed in 1% paraformaldehyde. Fluorescence was detected using a FACSCalibur, and the phenotype of gated hematopoietic cells was analyzed using CellQuest-Pro software (BD Pharmingen). The following conjugated antibodies were used: CD11b (Mac-1α), Ly-6G (Gr-1), and CD45 (Ly-5) (BD Pharmingen).
Immunohistochemistry
Studies were performed on fetal tissues and 6-day postnatal marrow. E13.5-day fetal livers, E17.5-day whole fetuses, and femurs and tibias from 6-day-old mice were removed and frozen in optimal cutting temperature (OCT) compound. Five-micron sections were cut on a cryostat and fixed in acetone. Sections were stained using the following technique (Vector Laboratory, Burlingame, CA): Nonspecific binding was blocked using normal goat serum and avidin/biotin. CD11b (Mac-1α) rat antibody, or the isotype control was used followed by biotinylated antirat immunoglobulin G2β (IgG2β) antibody. CD45 (Ly5) antibody was directly conjugated with biotin. All antibodies were from BD Pharmingen. Color development used an avidin–horseradish peroxidase complex with 3,3′-diaminobenzene (DAB) as color substrate. Slides were counterstained with methyl green, cleared, and mounted.
Cells from type A, B, and C colonies grown in methylcellulose were evaluated for phenotype using the antibodies described above with the addition of CD117 (c-kit) (BD Pharmingen) and F4/80 (Serotec, Oxford, United Kingdom) antibodies. For phenotyping cells from different colonies, cytospins were prepared as described above, fixed in 4% paraformaldehyde for 30 minutes, and stored at 4°C. Random microscopic fields were selected for analysis, and 200 cells were counted in multiple experiments. Representative experiments are shown in Figure 3.
Culture of fetal liver and bone marrow
To detect murine granulocytic/monocytic progenitors, fetal liver cells (E13.5), or day-6 or bone marrow cells were cultured in triplicate in methylcellulose enriched with Iscove modified Dulbecco medium (IMDM), including 10 ng/mL interleukin-6 (IL-6), 10 ng/mL IL-3, 50 ng/mL stem cell factor (SCF), and 10% fetal bovine serum (FBS) (Methocult GF, Stem Cell Technologies, Vancouver, BC, Canada) and further supplemented with 10 ng/mL granulocyte-macrophage colony-stimulating factor (GM-CSF) (R&D Systems, Minneapolis, MN). Cells were plated in 3.5-cm dishes using 103 fetal liver or 5 × 103 bone marrow cells per 3.5-cm dish. Colonies of more than 50 cells were counted and classified 7 to 8 days after plating. Colony classification was similar to that described earlier by Lavau et al.11 Type A colonies were most easily distinguished at day 7 in blind experiments. Replating of second and third generations was carried out with pooled colonies using the same conditions. Following the third generation, cultures were carried out in a Dulbecco modified Eagle medium (DMEM)–based enriched liquid medium that included 15% FBS, IL-3, IL-6, GM-CSF, and SCF. Cytospins were prepared from cells isolated from type A, B, and C colonies. Air-dried glass slides were stained using May-Grünwald Giemsa or α-naphthyl butyrate esterase. Cellular esterase results in release of naphthyl groups, and subsequent azo-dye coupling reaction forms a brownish precipitate in cells of monocytic lineage.
To study the differentiation potential of cells from type A, B, and C, colonies, cells from each colony type were replated in methylcellulose medium. Colony number and colony type distribution were evaluated 7 days later.
Cell transplantation into secondary recipients
Bone marrow cells from mice displaying overt leukemia were cleared of erythrocytes and injected intravenously at a dose of 1.5 × 107 cells per recipient into wild-type siblings that lacked the Mll-AF9 gene and had been prepared with 300 cGy whole-body cesium irradiation. In the same manner, marrow cells from 6-day-old mice both with and without Mll-AF9 were given to wild-type recipients at a dose of 1.5 × 106 cells each. Fetal liver cells were harvested from myeloid colonies grown in methylcellulose and injected into either radiated or nonirradiated recipients at a dose of 1 × 106 each. Recipients were monitored over time, and any displaying signs of leukemia had tissues harvested and tested for the presence of the Mll-AF9 gene and immunophenotype using FACS analysis.
Results
Colony assays demonstrate an Mll-AF9–induced expansion of myeloid progenitor cells as early as day 13.5 in fetal development
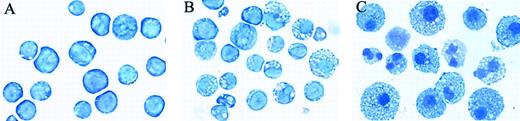
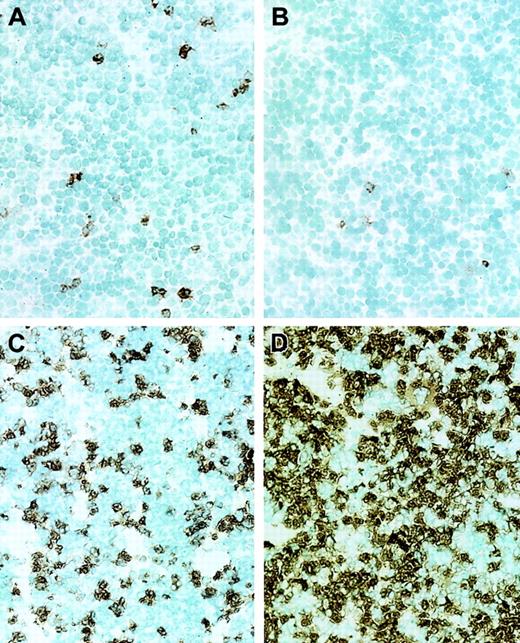
We used colony-forming unit assays to compare myeloid clonogenic cells from the fetal livers at day-13.5 gestation with postnatal preleukemia marrow in Mll-AF9 and wild-type mice. E13.5 fetal liver myeloid cells were cultured in methylcellulose medium supplemented with IL-3, IL-6, GM-CSF, and SCF. Myeloid colonies were visualized and counted after 7 to 8 days of culture. All colony assays were evaluated without knowledge of the genotype of the mice. Three types of colonies were observed in fetal liver and bone marrow as shown in Figure 1. Type A colonies were found frequently in Mll-AF9 mice but rarely in wild-type mice, while type B and type C colonies were found in both wild-type andMll-AF9 mice. Type A colonies are very compact without a halo of migrating cells. Type B colonies have a compact center and a halo of single cells. Type C colonies have no center and only single cells. The classification of colonies is identical to that used previously following retroviral transduction of Hrx (Mll)-ENL into primary marrow cultures.11 In the current studies type A, B, and C colony morphologies were identical in fetal liver and bone marrow.
Myeloid colonies from fetal liver or bone marrow grown in methylcellulose medium containing IL-3, IL-6, GM-CSF, and SCF.
Colonies of types A, B, and C are as described in “Results.” Type A colonies are rarely found in wild-type mice. Original magnification, × 10.
Myeloid colonies from fetal liver or bone marrow grown in methylcellulose medium containing IL-3, IL-6, GM-CSF, and SCF.
Colonies of types A, B, and C are as described in “Results.” Type A colonies are rarely found in wild-type mice. Original magnification, × 10.
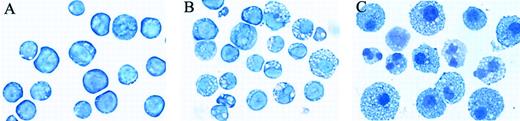
As shown in Figure 2, cells from type A colonies generally have an undifferentiated appearance with large nuclei and minimal cytoplasm. Rare cells from type A colonies showed myelomonocytic differentiation based on cellular morphology and α-napthyl butyrate esterase staining in the cytoplasm. Cells in type B and type C colonies are more differentiated myelomonocytic cells as shown in Figure 2. Cell morphology in type A, B, and C colonies did not differ when Mll-AF9 fetal liver and bone marrow were compared. As quantified in the next section, type A colonies were only rarely found in wild-type mice and were insufficient to conduct further in-depth studies.
Cytospins of cells from type A, B, and C colonies with May-Grünwald Giemsa stain.
Cells in type A colonies are largely undifferentiated with a high nuclear/cytoplasmic ratio, while cells from type C colonies generally demonstrate evidence of monocytic or granulocytic lineage differentiation. Type B colonies are a mixture of undifferentiated and more mature cells. Original magnification, × 40.
Cytospins of cells from type A, B, and C colonies with May-Grünwald Giemsa stain.
Cells in type A colonies are largely undifferentiated with a high nuclear/cytoplasmic ratio, while cells from type C colonies generally demonstrate evidence of monocytic or granulocytic lineage differentiation. Type B colonies are a mixture of undifferentiated and more mature cells. Original magnification, × 40.
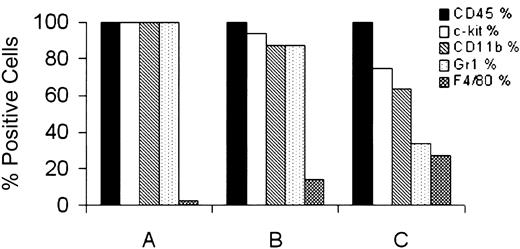
In addition to the morphology and histochemistry of cells in type A, B, and C myeloid colonies described in the previous paragraph, we evaluated colonies by immunophenotyping of cells from cytospins. Results are shown in Figure 3.
Immunophenotype of cells from cytospins of type A, B, and C colonies from fetal liver of
Mll-AF9 mice. Colonies show progression in myeloid maturation from A to B to C colonies, manifest as a progressive loss of the early marker, CD117 (c-kit), and gain of the mature myeloid marker, F4/80.
Immunophenotype of cells from cytospins of type A, B, and C colonies from fetal liver of
Mll-AF9 mice. Colonies show progression in myeloid maturation from A to B to C colonies, manifest as a progressive loss of the early marker, CD117 (c-kit), and gain of the mature myeloid marker, F4/80.
The results from Mll-AF9 fetal liver shown in Figure 3demonstrate that the cells in type A colonies are 100% positive for CD117 (c-kit), CD11b, Gr-1, and CD45, characteristic of myeloid progenitor cells. Cells from type A colonies were only rarely positive for F4/80, a marker of mature monocyte/macrophage cells. As expected, more cells from type B and C colonies are more often F4/80+and c-kit− than type A colonies. Colonies from day-6 marrow were also studied and found to be similar to those of fetal liver, with the exception of a lower percentage of Gr-1+cells. The combined results of morphology and immunophenotyping shown in Figure 2 and Figure 3 suggest that most cells from type A colonies are myeloid progenitor cells, with an immunophenotype similar to that seen in leukemia cells. Insufficient wild-type A colonies were available for analysis.
The presence of B and C colonies in wild-type and Mll-AF9mice permitted a comparison using immunophenotyping and cytochemistry for evidence of a block in differentiation as a result of the fusion gene. Repeated experiments, with a representative experiment in Figure3, demonstrated no differences between wild-type and Mll-AF9type B and C colonies with immunophenotyping (including c-kit) cytomorphology or cytochemistry. These results suggest that a block in differentiation, as suggested by the predominance of type A colonies inMll-AF9 mice, is only partial and likely reversible. To further evaluate the potential of cells for further differentiation, we conducted replating experiments. Replating of type A, B, and C colonies from 6-day postnatal marrow was carried out. The replating efficiency was highest for type A, intermediate for type B, and lowest for type C colonies. (In one representative experiment, 1200 type A colonies, 275 type B colonies, and rare type C colonies were cultured per 10 000 cells plated.) Importantly, replating of type A cells resulted in type A, B, and C with a predominance of type B colonies. Type B cells resulted mostly in B and C colonies. Replating of type C cells resulted only in type C colonies. These results demonstrate that cells from type A colonies are capable of producing mature cells, consistent with a partial and reversible maturation block, but not with a complete differentiation block resulting fromMll-AF9. These results are concordant with the immunophenotyping and cytochemistry results described above. Our results are quite similar to those reported previously from colonies obtained in the Mll-ENL retroviral transduction system.11
Serial replating demonstrates differences in replating efficiency between prenatal and postnatal Mll-AF9 cells
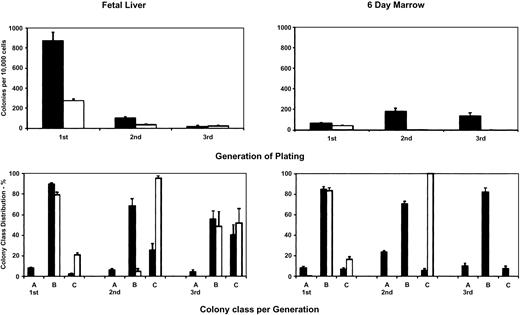
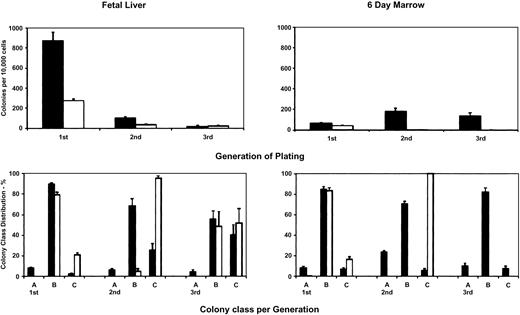
We next compared the myeloid colonies from fetal liver and 6-day postnatal marrow in a quantitative manner. Results from a representative of 6 replicate experiments are shown in Figure4.
Myeloid colonies from
Mll-AF9 (▪) and wild-type mice (■).Fetal liver (E13.5) results in left upper and lower panels and bone marrow from 6-day-old mice in right upper and lower panels. ▪ represents Mll-AF9 mice; ■, wild-type mice. Upper panels: total colonies from first, second, and third generations of plating. Lower panels: colonies by type A, B, or C class. Means and standard errors are shown.
Myeloid colonies from
Mll-AF9 (▪) and wild-type mice (■).Fetal liver (E13.5) results in left upper and lower panels and bone marrow from 6-day-old mice in right upper and lower panels. ▪ represents Mll-AF9 mice; ■, wild-type mice. Upper panels: total colonies from first, second, and third generations of plating. Lower panels: colonies by type A, B, or C class. Means and standard errors are shown.
Results in Figure 4 show fetal liver on the left and postnatal bone marrow on the right. Black bars show results from Mll-AF9and open bars from wild-type mice. Results are from the first through the third generations of plating. As shown in the upper panels, the total number of Mll-AF9 myeloid colonies was always greater than that of wild-type mice in both prenatal fetal liver and postnatal marrow. From wild-type mice, significant numbers of prenatal myeloid colonies were cultured from fetal liver for 3 generations, although with decreasing frequency in each subsequent plating. In contrast, there was little or no colony growth in wild-type postnatal marrow by the second or third generation.
Importantly, in Mll-AF9 mice as shown in Figure 4, postnatal marrow myeloid colonies of types A, B, and C were increased after replating in the second and third generations, in contrast to fetal liver where the number of colonies decreased from the first through the third generation. Type A colonies were cultured from prenatal fetal liver and postnatal bone marrow from Mll-AF9 mice but rarely from wild-type mice (Figure 2, lower left and right panels, respectively). Type A colonies persisted from Mll-AF9 mice after replating to the second and third generations in both prenatal fetal liver and postnatal bone marrow. However, the number of type A colonies continued to increase with plating to second and third generations in postnatal marrow while the number in prenatal fetal liver was lower than that seen in the first generation.
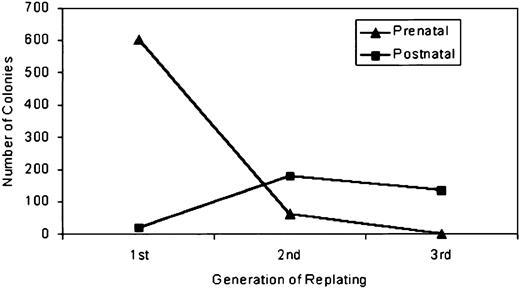
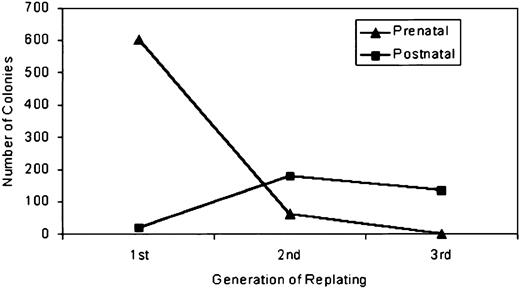
When cells from all colony types from wild-type and Mll-AF9were compared at each generation, a significant increase in colony number was seen in postnatal but not prenatal Mll-AF9cells. A summary comparison of the number of the replating efficiency of prenatal and postnatal myeloid colonies from Mll-AF9 mice is shown in Figure 5. These results are summarized from the data from Figure 4 with the data representing the number of wild-type colonies subtracted from the Mll-AF9colonies.
Comparison of the replating efficiency of prenatal and postnatal myeloid colonies from
Mll-AF9 mice from the first to the third generations. Results are shown as number of colonies per 10 000 plated. Prenatal cells have lost self-renewal capacity by the third passage while postnatal cells continue to self-renew.
Comparison of the replating efficiency of prenatal and postnatal myeloid colonies from
Mll-AF9 mice from the first to the third generations. Results are shown as number of colonies per 10 000 plated. Prenatal cells have lost self-renewal capacity by the third passage while postnatal cells continue to self-renew.
Overall, the results in Figure 5 demonstrate significant differences in the self-renewal capacity of prenatal and postnatal myeloid cells inMll-AF9 mice. These differences, which have been reproduced in 12 experiments to date, demonstrate a limited capacity for self-renewal in prenatal myeloid cells in the second and third generations of replating, unlike the postnatal cells that continue to self-renew at least to the third generation. We interpret this increased self-renewal in postnatal bone marrow to most likely indicate progression of Mll-AF9 myeloid progenitors to a second stage of leukemogenesis.
Expansion of myeloid progenitor cells in vivo is not observed until the postnatal period
If progression of leukemogenesis occurs between prenatal and postnatal life, we would expect that this progression will be reflected in vivo based on the in vitro studies shown earlier in “Results.” Therefore, we next evaluated the effects of the Mll-AF9fusion gene on myeloid cell development in vivo. Immunohistochemistry was used to evaluate the number of CD11b+ cells from murine fetal liver and postnatal marrow. Results from prenatal fetal liver at day-13.5 gestation and postnatal bone marrow at day-6 after birth are shown in Figure6.
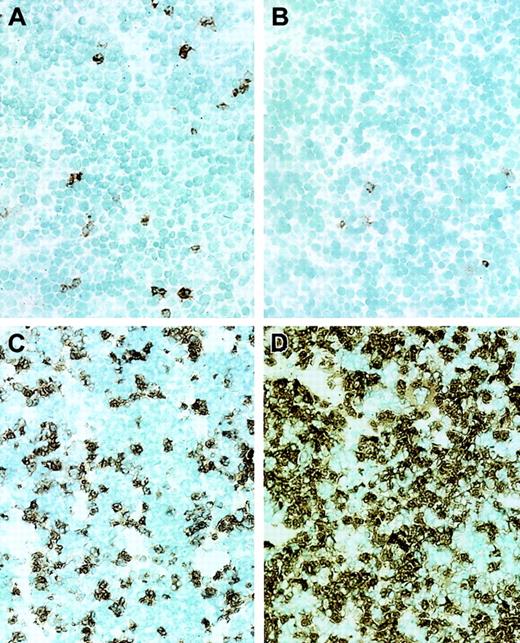
Sections of murine fetal liver (day E13.5) and bone marrow (6-day postnatal) were stained with CD11b (Mac-1α) antibody–horseradish peroxidase (HRP) (brown) and counterstained with methyl green.
(A) Wild-type fetal liver. (B) Mll-AF9 fetal liver. (C) Wild-type 6-day postnatal bone marrow. (D) Mll-AF9 6-day postnatal bone marrow. Original magnification, × 20.
Sections of murine fetal liver (day E13.5) and bone marrow (6-day postnatal) were stained with CD11b (Mac-1α) antibody–horseradish peroxidase (HRP) (brown) and counterstained with methyl green.
(A) Wild-type fetal liver. (B) Mll-AF9 fetal liver. (C) Wild-type 6-day postnatal bone marrow. (D) Mll-AF9 6-day postnatal bone marrow. Original magnification, × 20.
A total of 43 fetal livers and seven 6-day marrows fromMll-AF9+/− mice were compared with 50 fetal livers and 11 6-day marrows from siblingMll-AF9−/− mice. Significant differences were found between Mll-AF9 fetal liver and postnatal marrow when compared with normal mice. In the fetal liver there was a reduction in CD11b+ cells in Mll-AF9 (Figure 6B) compared with wild-type mice (Figure 6A). By contrast, the postnatalMll-AF9 bone marrow had a significant increase in the number of CD11b+ cells (Figure 6D) compared with wild-type marrow (Figure 6C). The number of CD45+ cells paralleled those found with CD11b in both fetal liver and bone marrow (data not shown).
Using flow cytometric analysis, we compared suspensions of fetal liver and bone marrow cells. In fetal livers, consisting of 43Mll-AF9 and 50 wild-type mice, we found a significant decrease of CD11b/Gr-1+ cells in Mll-AF9 mice compared with wild-type ones (an average of 2.7% CD11b/Gr-1+ in Mll-AF9 fetal livers compared with 5.0% in wild-type fetal livers, P < .001).Mll-AF9 mice had fewer total CD11b+ cells and fewer total Gr-1+ cells than wild-type mice (a total average of 38.0% CD11b+ cells and 4.7% Gr-1+cells in Mll-AF9 mice compared with 53.8% and 7.7%, respectively, in wild-type mice; P < .005 andP < .001). The paradox between the increase in CD11b/Gr-1+ myeloid progenitors in the Mll-AF9fetal tissue as detected in the colony assay and the decrease in CD11b/Gr-1+ cells in vivo in fetal liver is best explained by a reduction in mature CD11b/Gr-1+ cells. It is likely that expansion of clonogenic progenitors is occurring at the expense of the development of mature myeloid cells inMll- AF9 mice.
Results from postnatal bone marrow were different from that seen in fetal liver: As previously reported, CD11b/Gr-1+ cells are increased in 6-day postnatal marrow using flow cytometric analysis.7 These results are extended in this study in Figure 6C-D using immunohistochemistry.
One possible explanation for the reduction in total CD11b+cells in Mll-AF9 fetal liver is that abnormal myeloid cells do not grow well in the fetal liver environment when compared with that of the bone marrow. To evaluate this possibility, we studied day- 17.5 fetuses, at which time both fetal liver and marrow myelopoiesis is active. Importantly, the same reduction in total CD11b+cells was observed in the fetal marrow as was found in the fetal liver (data not shown). These results suggest that the fetal liver is not deficient in the ability to support the proliferation of abnormal myeloid progenitors compared with the marrow compartment.
Long-term cultures of CD11b/Gr-1+ cells are successful from mice with leukemia but not from fetal liver or 6-day marrow of Mll-AF9 mice
We next compared the long-term growth potential and cytokine requirements of myeloid cells from prenatal fetal liver, early postnatal marrow and, finally, marrow from young adult mice with leukemia. These cells were cultured in liquid media beyond the third generation in the presence of IL-3, IL-6, GM-CSF, and SCF. Cells from mice with leukemia were readily cultured for at least 3 months in liquid media, and 3 independent long-term lines have been developed. These cells had a CD11b/Gr-1+ myeloid phenotype but, interestingly, remained dependent on the growth factor, IL-3 (data not shown). Our attempts to establish long-term CD11b/Gr-1+cell lines from fetal liver and 6-day marrow have been entirely unsuccessful (0 of 18 attempts). The inability to successfully culture CD11b/Gr-1+ cells long-term from fetal liver or 6-day postnatal marrow is contrasted with the relative ease of establishing long-term growth of CD11b/Gr-1+ cells from leukemia mice. These data provide additional evidence that sequential events are required for the development of leukemia in the Mll-AF9murine model system.
Cells from adult mice with leukemia but not prenatal or postnatal cells produce early leukemias in transplantation experiments
As discussed in the previous section, we found that prenatal and early postnatal cells were incapable of producing long-term myeloid cell lines in contrast to cells from leukemic animals. We next compared these same cells populations in vivo to determine the ability to produce leukemia in animals. Pooled cells from prenatal myeloid cultures were used. In one type of transplantation, experiment cells were injected intravenously into sublethally irradiated (n = 13) and nonirradiated (n = 13) recipients. Mice were observed for 7 months without signs of leukemia. The number of CD11b+ cells was not increased in these mice. Similarly, no leukemia has developed in recipients of fresh bone marrow from 6-day postnatal Mll-AF9mice at 3.5 months of follow-up. In control experiments, cells from both leukemia-bearing Mll-AF9 mice and from a cell line that had been established from a mouse with Mll-AF9 leukemia resulted in frank leukemia no later than 2 months in transplant recipients. Long-term follow-up of the mice that received prenatal or early postnatal myeloid cells is under way to evaluate the possibility that, as in primary mice, progression through the stages of leukemia will occur given sufficient time and accumulated genetic and cellular abnormalities.
Summary of in vitro and in vivo results
The results presented in the previous sections demonstrate evidence of progression of Mll-AF9 fusion gene leukemia when the in vitro and in vivo results are combined. These results are summarized in Table 1. Results shown in Table 1 demonstrate several stages in the pathogenesis ofMll-AF9 leukemia in the murine model. The prenatal stage is characterized by expansion of myeloid progenitors in fetal liver and marrow but with a very limited ability of cells to persist in replating experiments. The second stage in the early postnatal period is characterized by an enhanced progenitor replating (enhanced self-renewal) beyond that seen in the prenatal period. The third and frank leukemia stage is characterized by unlimited in vitro replating potential, ability to produce long-term cell lines, and early leukemia in recipient mice in transplantation experiments.
Discussion
Animal models are potentially very useful in the understanding of the steps in the pathogenesis of human leukemias. Mll fusion gene leukemias have been produced using homologous recombination withMll-AF9 into embryonic stem cells or retroviral transduction with Mll-ENL. Previous studies withMll-ENL and Mll-ELL have demonstrated that the fusion gene will result in the immortalizing of retrovirally transduced young adult bone marrow cells.11 12 In both previously reported models there is a somewhat long incubation period, suggesting that several steps, possibly including additional cooperating genetic mutations, are necessary to produce leukemia. In the experiments reported here we chose the introduction of Mll-AF9 by homologous recombination to evaluate steps in the pathogenesis ofMll fusion gene leukemia. Homologous recombination has the advantage over other methods to experimentally introduce fusion oncogenes in that human chromosomal translocations can be reproduced. This results in (1) a single copy of the fusion oncogene under the control of the endogenous Mll promoter with expression of the oncogene at levels similar to those in naturally occurring leukemias and (2) haploinsufficiency in the normal allele.
In our experiments we directly demonstrate that theMll-AF9 fusion oncogene when introduced into embryonic stem cells results in myeloid abnormalities at least as early as day 13.5 in fetal development. Our results demonstrate a dramatic expansion in fetal myeloid progenitor cells in myeloid colony assays. The results of fetal liver colony-forming cell assay in Mll-AF9 are clearly different from fetal liver from Mll mutant mice where reduced numbers of colony-forming cells were observed.13The differences between the mice with the Mll fusion gene and mice that lack Mll strongly support “gain of function” abnormalities resulting from Mll-AF9.
Our results from knock-in Mll-AF9 mice provide the first evidence that Mll translocations, if they occur prior to or at day 13 of hematopoiesis, can result in prenatal abnormalities of myeloid cell proliferation and differentiation. Comparisons between murine and human MLL fusion gene leukemias are of obvious interest. Further studies will be necessary to directly demonstrate the presence of naturally occurring translocations at or before fetal myelopoiesis in humans. Our results demonstrate a dramatic increase in the number of myeloid colony-forming cells in Mll-AF9 mice beginning as early as the fetal liver stage of hematopoiesis. The data show that Mll-AF9 fetal liver has an increase in clonogenic myeloid cells with progeny that are largely CD11b/Gr-1+. However, the increase in clonogenic myeloid cells in Mll-AF9 mice is not associated with an increase in the total number of CD11b+ cells in fetal liver as detected in tissues by immunohistochemistry and flow cytometry. In fact, there is a decrease in the number of myeloid cells in vivo in fetal livers from Mll-AF9 mice. Possible explanations are that this early stage represents either an Mll-AF9–induced block in cell differentiation and/or a commitment to self-renewal of myeloid progenitors at the expense of differentiation. Previous results from in vitro analyses have suggested a reversible differentiation block resulting from either Mll-AF9 or Mll-ENLfusion gene in bone marrow–derived cells.14,15 Previous studies with human MLL leukemia have demonstrated a reversible block in differentiation in leukemia cells.16Our results demonstrated that at the prenatal stage cells have a limited ability to self-renew in replating experiments. Also, mice that received cells from the prenatal stage did not develop leukemia when followed for 7 months after transplantation.
In our experiments, early postnatal marrow demonstrated both an increase in self-renewal of colony-forming cells in replating experiments and a corresponding accumulation of CD11b/Gr-1 myeloid cells in the marrow. We postulate that early postnatalMll-AF9 marrow represents a stage or period characterized by enhanced cell survival with slow accumulation. However, mice are not frankly leukemic and do not die for an additional 5 to 6 months. This second or survival/accumulation phase could result either from a decrease in apoptotic cell death or an increase in proliferative rate compared with normal myeloid progenitor cells. The increase in replating efficiency of postnatal when compared with prenatal cells suggests that increased cell survival is the most likely explanation for this second phase. While we do not know the molecular events responsible for the transition from the prenatal to the postnatal phase, our murine model will permit cellular and molecular studies of the mechanisms of this important transition. Interestingly, our previous studies in human MLL-AF4 leukemia have suggested that MLL fusion gene leukemias do not have increased proliferative rates but rather develop apoptotic resistance and survive despite removal of survival factors.17Apoptotic resistance in MLL leukemias may be due to interference with the GADD34-mediated apoptotic pathway.18
Comparison of our Mll-AF9 results with those obtained by others utilizing retrovirally mediated gene transfer ofMll-ELL and Mll-ENL into postnatal marrow demonstrates several features: Progenitor expansion in the methylcellulose assay varies, possibly dependent on the Mllfusion partner; Mll-ENL transduced cells11 have the most significant increase in serial replating with lesser increase noted for Mll-ELL12 orMll-AF9 (current results). The replating efficiency may predict the time to develop leukemia with “early” leukemia noted with Mll-ENL11 and late development of leukemia for Mll-ELL (100 to 200 days) andMll-AF9 (5 to 6 months). The delay in development ofMll leukemia in mice is somewhat different from the early onset seen in many human cases of MLL leukemia, which sometimes develop early in infancy. The reasons for these differences are not clear but could result from differences in time-sensitive susceptibility of critical genes to secondary mutations in mice and human beings. Studies of these similarities and differences between mice and human beings are the subject of ongoing research in the laboratory.
Our studies suggest that the postnatal cell survival/accumulation stage is distinct from the overt leukemic stage. The final stage of overt leukemia occurs later, because animals do not die until 5 to 6 months of age. Of interest, it is only at this later stage that we are able to establish long-term cultures of the appropriate phenotype and to promptly produce leukemia in recipient mice. Our working model for this third step in pathogenesis of MLL fusion gene leukemias suggests that distinct genetic events occur at each stage of leukemia development. Our murine model will permit analysis of prenatal, postnatal, and leukemia phases as a means to further define the critical steps in pathogenesis of MLL fusion gene leukemia.
In summary, this study demonstrates significant abnormalities inMll-AF9 cells in prenatal myeloid cells when studied in vitro and in vivo. We have further demonstrated significant differences between prenatal and postnatal myeloid cells, all preceding the development of frank leukemia in the adult mouse. These abnormalities suggest that there are several steps in the pathogenesis of leukemias that are initiated beginning with formation of theMll fusion gene. The further understanding of these steps in the process of leukemogenesis should assist in the development of improved in utero prevention or early treatment strategies in humanMLL leukemia.
Prepublished online as Blood First Edition Paper, December 19, 2002; DOI 10.1182/blood-2002-05-1515.
Supported in part by grants (Outstanding Investigator grant CA49721 and CA87053) from the National Cancer Institute and from the Children's Cancer Research Fund (J.H.K).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
John Kersey, 754 Cancer Center Research Bldg, 425 East River Rd, Minneapolis, MN 55455; e-mail:kerse001@umn.edu.