Abstract
The development of extranodal lymphomas is thought to be initiated by the transformation event in peripheral organs. Lymphomatoid papulosis (LyP) is a low-grade cutaneous lymphoma and may progress into the cutaneous anaplastic lymphoma. We identified 2 patients who 3 and 4 years before the development of LyP were treated for an unrelated malignancy (Burkitt lymphoma and small-cell B-cell lymphoma). We analyzed the T-cell receptor (TCR) gene rearrangement pattern in their skin, blood, and bone marrow, including the archival bone marrow sampled years before the development of clinically evident LyP. In all samples we detected the unique monoclonal TCR rearrangements. This observation suggests that the initial malignant transformation in LyP occurred in bone marrow and not, as could be supposed, in the skin. (Blood. 2003;102:3797-3799)
Introduction
The development of most leukemias is initiated by a malignant transformation at the level of the early hematopoietic precursor in the bone marrow1-4 that finally differentiates into the malignant phenotype.
The ontogeny of malignant lymphomas is less elucidated, but the initial malignant transformation is supposed to occur at any stage of lymphocyte development. The resulting malignant cell clone remains “arrested” at a particular developmental stage with little subsequent differentiation.5
Lymphomatoid papulosis (LyP) is a low-malignant cutaneous CD30+ T-cell lymphoma that sometimes clonally evolves into a more aggressive anaplastic large-cell lymphoma (ALCL).6-8 In this paper we describe data on 2 patients in whom characteristic T-cell receptor (TCR) gene rearrangement has been identified in bone marrow years before the emergence of cutaneous lesions of LyP or ALCL. This observation suggests that the initial malignant transformation in these extranodal T-cell lymphomas occurred in bone marrow rather than, as could be assumed, in the skin.
Study design
Case 1
A 36-year-old woman presented in 1996 with Burkitt lymphoma. She had a complete remission after treatment with cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP). In 1999, she developed LyP (Figure 1A-B) and during the following 4 months erythematous, ulcerated tumors of ALCL developed on the trunk and lower limbs (Figure 1C). During the following 2 months new ALCL lesions appeared, despite local radiotherapy. In 2001, the patient died from the systemic dissemination of ALCL.
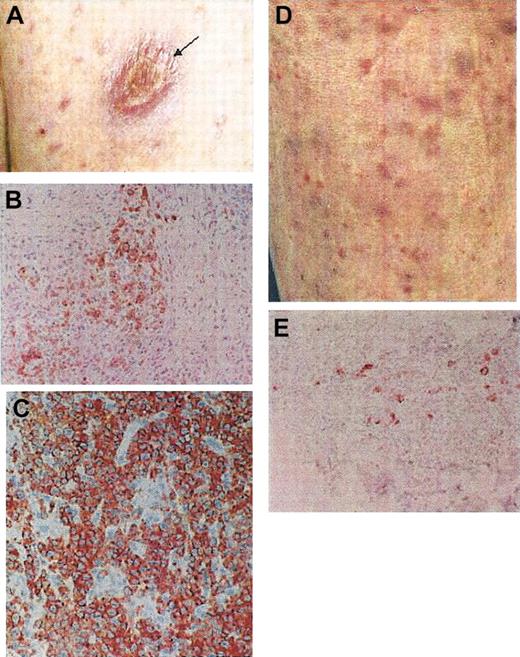
Clinical and histopathologic features of the 2 patients with LyP. Case 1 (A-C) and case 2 (D-E). Arrow in panel A shows the tumor of ALCL; the papular lesions in panels A and D represent LyP. Panels B and E show positive CD30 staining of atypical lymphoid cells in LyP. Panel C shows a more massive infiltration and pronounced atypia of CD30+ cells in ALCL. Original magnification, × 200 (B,C,E).
Clinical and histopathologic features of the 2 patients with LyP. Case 1 (A-C) and case 2 (D-E). Arrow in panel A shows the tumor of ALCL; the papular lesions in panels A and D represent LyP. Panels B and E show positive CD30 staining of atypical lymphoid cells in LyP. Panel C shows a more massive infiltration and pronounced atypia of CD30+ cells in ALCL. Original magnification, × 200 (B,C,E).
Case 2
A 63-year-old man presented in 1996 with small-cell lymphocytic B-cell lymphoma CD5-23-IgM+ involving the spleen, lymph nodes, and bone marrow. He was treated with chlorambucil (1997-1998) with a partial response. In 1999, he had a relapse and received 6 series of CHOP, which gave full remission during the observation period (up to May 2003). In 1999, while he was receiving CHOP treatment, he developed widespread, papular skin lesions with clinical and histopathologic features of LyP (Figure 1D-E). Partial remission has been achieved during the treatment with methotrexate (15 mg weekly) and PUVA (psoralen and UVA radiation), but LyP recurred after the cessation of the treatment. The disease is actually controlled with maintenance PUVA treatments.
Gene rearrangement studies
Nuclei were released by mechanic disintegration of the formaldehyde-fixed, paraffin-embedded skin biopsies and bone marrow specimens9 and analyzed by polymerase chain reaction (PCR) with fluorescence fragment product analysis on an automated capillary electrophoresis DNA sequencer (GeneScan; Applied Biosystems, Weiterstadt, Germany)10,11 in the German laboratory by A.L. The PCR products were purified and sequenced on the 310 ABI PRISM (Applied Biosystems).11 To eliminate the possibility of false-positive results (contamination from other samples), the sequences were routinely compared with all other TCR-γ sequences ever found in this laboratory and were confirmed to be unique. Moreover, DNA obtained from freshly sampled bone marrow and blood specimens12 was independently analyzed for the presence of clonal immunoglobulin heavy chain (IgH) VDJ gene rearrangements and TCR-γ and -δ gene rearrangements by manual sequencing detection13 in the Danish center by H.O.M. (case 1). Pooled lymphocytes from healthy donors were used as negative control. Moreover, the minimal residual disease (MRD) analysis was performed14,15 using the clone-specific PCR with TCR-γ and IgH sequences detected in the gene rearrangement analysis as clone-specific probes for the T-cell lymphoma and Burkitt lymphoma, respectively.
Results and discussion
In case 1 identical biallelic clonal gene TCR rearrangements were found in the samples of bone marrow, peripheral blood, and skin lesions of LyP and ALCL (Table 1). The most important finding was the presence of the clone-specific TCR-γ rearrangement in bone marrow found 4 years later also in skin lesions of LyP and ALCL (Table 1). The frequency of clonally rearranged cells in bone marrow was only 8% in comparison with peripheral blood (Table 1). In case 2 the bone marrow biopsy was obtained in 1997 as a routine diagnostic procedure for non-Hodgkin lymphoma. PCR fluorescence fragment analysis of paraffin-embedded bone marrow samples revealed amplicons corresponding to rearrangement comprising TCR-γ V9-J1/2 (Table 2). An identical PCR pattern was found 2 years later in the cutaneous lesions of LyP (Table 2). The above results indicate that a clinically silent and histopathologically undistinguishable cell clone bearing the molecular lymphoma fingerprint had already been present in bone marrow years before the development of the cutaneous T-cell lymphoma.
In case of extranodal lymphomas the malignant transformation is thought to take place directly within mature T cells infiltrating or recycling through the target organ.16-20 Many researchers were unsuccessful in their attempts to detect clonal rearrangements in bone marrow of patients with LyP and mycosis fungoides (MF),21 which further supported the concept of the skin origin of cutaneous lymphomas. Our observations suggest another scenario in case of LyP, a low-grade cutaneous T-cell lymphoma. We speculate that the precursor malignant clone develops primarily in bone marrow and disseminates to the skin via circulation. Local cutaneous microenvironment permits further differentiation into a mature LyP phenotype, and in some patients even further to ALCL (case 1, Davis et al6 and Steinhoff et al7 ). There is probably recirculation of malignant cells between the cutaneous and blood compartments, which explains an over 10-fold higher frequency of clonally rearranged cells in blood than in bone marrow. Our success with the search for bone marrow clone in the 2 described patients was probably due to a higher than usual frequency of bone marrow lymphoma precursors. It is likely that in many patients the proportion of precursor cells is below the resolution power of routine PCR techniques (< 2%-5%). Use of more sensitive detection techniques, such as the clone-specific PCR, could help to identify more patients with bone marrow involvement.
The hypothesis of the existence of bone marrow precursors of LyP explains several biologic properties of this lymphoma that are otherwise difficult to account for by the traditional model assuming malignant transformation in the skin. First, even at the very early stages multiple skin lesions develop in LyP patients suggesting hematogenous dissemination from extracutaneous compartment. Second, even a complete eradication of cutaneous lesions by local radiation therapy or phototherapy cannot prevent the relapse of the disease, suggesting again that the precursor lymphoma cells are not affected by these local modalities. Third, cure cannot be usually obtained even with aggressive, high-dose chemotherapy, but a symptomatic relief on skin lesions can usually be achieved even with low doses of cytostatics. In our case 1, intensive chemotherapy eradicated the malignant B-cell clone but the bone marrow cells harboring the signature TCR rearrangement remained unaffected. It can be speculated that similar to the situation seen in chronic leukemias, the malignant precursor cells in bone marrow are slowly cycling and are thus not affected by the cytostatics. Fourth, patients with LyP have for unknown reasons a highly (10-fold) increased risk for the development of lymphoid (and to a lesser extent myeloid) malignancies.22,23 A concept suggesting a genetic defect at an early stage of multipotent hematopoietic progenitor could provide a plausible mechanistic explanation of this phenomenon, as that suggested for multiple cell-lineage leukemias24 and lymphomas (notably LyP and cutaneous anaplastic lymphoma).7 Fifth, a clinically silent malignant clone in patients with peripheral T-cell lymphoma can be transmitted by allogeneic bone marrow transplantation.25
In summary, our observations are compatible with the view that CD30+ cutaneous lymphomas are differentiating systems comprising bone marrow-derived progenitor cells giving rise to the malignant cells in the skin. Further studies are needed to determine the phenotypic characteristics of these progenitor cells. Our concept may provide a framework for the understanding of the biologic properties of LyP and can possibly be extended to other types of peripheral T-cell lymphoma.
Prepublished online as Blood First Edition Paper, July 3, 2003; DOI 10.1182/blood-2003-03-0899.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.