Abstract
Interleukin 15 (IL-15) and the IL-15 receptor α (IL-15Rα) chain are both required for the basal proliferation of memory CD8 T cells, but which cell types are required to express IL-15 or IL-15Rα to mediate this proliferation is not known. Using bone marrow (BM) chimeras, we showed that virus-specific CD8 memory T-cell proliferation was driven by IL-15 produced by either BM-derived or parenchymal cells. Experiments using mixed BM chimeras showed that IL-15Rα expression by memory CD8 T cells was not required for their division. In addition, wild-type memory CD8 T cells did not divide after transfer into IL-15Rα-/- mice. Further analyses demonstrated that IL-15Rα+ BM-derived cells were crucial in driving memory CD8 T-cell division in the spleen while both parenchymal and BM-derived cells promoted memory cell division in the lung. Proliferation in response to soluble IL-15 in vivo required expression of IL-15Rα by opposing cells and IL-15Rβ by CD8 memory cells, indicating that IL-15 interacted directly with the T cells. These results indicate that transpresentation of IL-15 by IL-15Rα on BM-derived cells mediates the basal proliferation of memory CD8 T cells. (Blood. 2004;103:988-994)
Introduction
Memory T cells are a product of a primary immune response that drives differentiation of naive T cells into effectors and subsequently into memory T cells. Whether an intermediate effector stage is required during the naive to memory cell transition is controversial, although available evidence strongly supports this scenario for CD8 T cells.1-6 The generation of memory T cells is crucial as this population is responsible for a rapid and more efficient response to pathogens upon a secondary encounter. Once memory T cells are generated, homeostatic mechanisms are in place to maintain the memory pool. Thus, the homeostasis of antigen-specific memory T cells is a requirement for long-term sustenance of immunologic memory and continual protection.
Memory T-cell homeostasis is maintained by continual low level of proliferation and long-term survival.7-9 Interleukin 7 (IL-7) and IL-15 are the 2 mediators shown to be important for memory CD8 T-cell survival and proliferation, respectively.10-13 Although both IL-7 and IL-15 have the ability to induce T-cell proliferation and increase CD8 T-cell survival in vitro, in vivo studies indicate that IL-7 acts more as a survival factor for memory CD8 T cells,10,13 whereas IL-15 maintains memory CD8 T-cell division.10-12 Specifically, it has been demonstrated that proliferation of antigen-specific memory CD8 T cells is greatly diminished in the absence of either IL-15 or IL-15 receptor α (IL-15Rα).11,12 However, the exact mechanism by which IL-15 operates is not clear and which cell types need to produce and respond to IL-15 to drive memory cell proliferation needs to be addressed.
IL-15-mediated signals are a result of IL-15 binding to either an intermediate-affinity heterodimeric receptor complex or a high-affinity heterotrimeric receptor complex. The intermediate-affinity receptor complex is composed of the shared cytokine receptor chains, the IL-2/15Rβ and the common γ chain (γC).15 The IL-15Rα has a high affinity for IL-15 (Kd = 10-11) compared with the IL-2/15Rβ chain (Kd = 10-9).15-17 When complexed with the IL-2Rβ and γC, the IL-15Rα chain helps form a high-affinity receptor complex for IL-15 but is not required for inducing a proliferation signal.16,17 In vitro studies demonstrate that IL-15 can act directly on T cells to induce proliferation.18,19 CD8 T cells are known to express the IL-2/15Rβ, γC, and IL-15Rα proteins.11,18 Elevated levels of IL-15Rα expression by memory CD8 T cells were demonstrated using an IL-15-Fc fusion protein whose binding is dependent on the presence of IL-15Rα.11 This result agrees well with the heightened sensitivity of memory CD8 T cells to IL-15 action in vitro and in vivo compared with either naive CD4 and CD8 T cells or memory CD4 T cells. Overall, the evidence suggests that CD8 T cells are direct targets of IL-15, however, the role of the IL-15Rα expression by CD8 T cells is not clear.
IL-15Rα mRNA is expressed by T cells as well as other types of bone marrow (BM)-derived cells and non-BM-derived parenchymal cells.16,17 Recent data suggest that IL-15Rα not only acts as a component of the high-affinity IL-15R signaling complex but also can act to present IL-15 to opposing cells in vitro.20,21 One goal of this study was to elucidate the role of the IL-15Rα chain in the basal proliferation of antigen-specific memory T cells in vivo. Like IL-15Rα expression, many cell types express IL-15 mRNA.19 Although anti-IL-15 antibodies do exist, IL-15 protein is rarely detected in culture supernatants or in tissues.22 The inability to detect IL-15 protein is due in part to the poor translation and short half life of IL-15.19,22-24 With the recent study suggesting IL-15 can be presented by IL-15Rα, it is also possible that IL-15 protein may be difficult to detect as it is usually bound to IL-15Rα. Another goal of this study was to determine the cell source of IL-15 that is used by memory CD8 T cells to maintain proliferation. Thus, we used various mouse models with restricted expression of IL-15 or IL-15Rα to identify the cell types that mediate the proliferation of memory CD8 T cells.
Materials and methods
Mice
C57Bl/6J (Ly5.1) and C57Bl/6 (Ly5.2) mice were purchased from The Jackson Laboratories (Bar Harbor, ME) and Charles River (Wilmington, MA) through the National Cancer Institute (NCI) program, respectively. C57Bl/6-IL-15-/- mice25 and IL-15Rα-/- mice26 were generously provided by Jacques Peschon, Immunex (Seattle, WA) and by Averil Ma (University of Chicago), respectively. IL-15Rα-/- mice were backcrossed to C57Bl/6 mice 8 generations. IL-2/15Rβ+/- mice were obtained from The Jackson Laboratories and were bred to generate IL-2/15Rβ-/- offspring. All mice were maintained under specific pathogen-free conditions at University of Connecticut Health Center (UCHC).
Generation of VSV-specific memory CD8 T cells and detection with MHC tetramers
Mice were infected intravenously with 1 × 106 plaque-forming units (PFUs) of vesicular stomatitis virus (VSV; Indiana or New Jersey serotype). In some cases, memory cell levels were increased by secondary infection with the alternate serotype. CD8 T cells specific for the VSV nucleoprotein (N) were detected using H-2Kb tetramers containing the N protein-derived peptide RGYVYQGL. Major histocompatibility complex (MHC) tetramers were generated as previously described.27 To identify VSV-N-specific CD8 T cells, cells were incubated with 100 μL of a properly diluted mixture of N-tetramer-allophycocyanin (APC) and anti-CD8 peridinin chlorophyll A protein (PerCP) monoclonal antibody (mAb) at 25°C for 1 hour. The cells were then washed and incubated with additional antibodies at 4°C for 20 minutes. Anti-CD44-phycoerythrin (PE)/APC and anti-Ly5.2-PE were purchased from BD Biosciences Pharmingen (San Diego, CA).
Generation of bone marrow chimeras
BM cells were obtained from femurs and tibias of IL-15-/-, IL-15Rα-/-, and control mice. To remove T cells present in the BM suspension, BM cells were treated with anti-Thy1 mAb (T24)28 followed by incubation with low-ToxM Rabbit Complement (Cedarlane, Hornby, ON, Canada) for 1 hour at 37°C. Recipients were irradiated with 10 Gy (1000 rad) from a 137Cs source and injected intravenously with 5 × 106 BM cells. Chimeras were used 8 to 10 weeks later for VSV infections or cell transfers.
Analysis of proliferation in vivo
For bromodeoxyuridine (BrdU) incorporation studies, VSV-infected mice were given water daily containing BrdU (0.8 mg/mL; Sigma, St Louis, MO) for 4 weeks. BrdU staining was performed after cell surface staining using BrdU Flow kit according to manufacturer's instructions (BD Biosciences Pharmingen). For transfer studies, spleen cells from mice infected with VSV more than 50 days prior were depleted of CD4 T cells and B cells using Dynabeads (Dynal, Oslo, Norway). Spleen cells were incubated with rat anti-CD4 mAb (GK1.5), washed, and incubated with goat antirat Dynabeads to bind CD4 T cells and goat antimouse Dynabeads to bind B cells. Magnetic-coated cells were then removed with a Dynal magnet. The enrichment procedure resulted in a population that contained approximately 60% CD8 T cells and 30% B cells and less than 1% CD4 T cells. Cells were resuspended in HBSS/HEPES (Hanks balanced salt solution/N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid), l-glutamine, Pen/Strep, gentamicin sulfate (HGPG) at a concentration of 10 × 106 cells/mL and warmed to 37°C. CFSE (5-(and 6) carboxyfluorescein diacetate succinimidyl ester); Molecular Probes, Eugene, OR) was added to the cell suspension at a final concentration of 0.01 mM and incubated for 10 minutes at 37°C.29 Cells were washed with HBSS/10% fetal calf serum (FCS) then resuspended in phosphate-buffered saline (PBS) prior to intravenous injection. Between 8 × 106 and 12 × 106 CD8 T cells containing approximately 0.5 × 106 tetramer-positive cells were transferred into each mouse. For IL-15 treatment in vivo, CD8 T cells were enriched from either VSV-infected mice, uninfected wild-type, or IL-2/15Rβ-/- mice as previously described, labeled with CFSE, and transferred intravenously into either control or IL-15Rα-/- mice. Mice were then injected intravenously with 2.5 μg of recombinant murine IL-15 (rmIL-15; R&D Systems, Minneapolis, MN). Three days after IL-15 treatment, lymphocytes from spleen and lung were analyzed for CFSE intensity on memory CD8 T cells. The percentage of cells of the original population that had divided (the “responding” population, R) was calculated as described.30
Isolation of lymphocyte populations
Spleens were homogenized in HBSS-HGPG, filtered through Nitex nylon mesh, and treated with tris-ammonium chloride to lyse red blood cells. To obtain lymphocytes from lung, anesthetized mice were perfused with PBS containing 75 U/mL of heparin until the tissues were cleared of blood. Lungs were minced and incubated with stirring at 37°C for 30 minutes in HBSS containing 1.3 mM ethylenediaminetetraacetic acid (EDTA), followed by treatment at 37°C for 1 hour with collagenase (150 U/mL; Gibco-BRL, Grand Island, NY) in RPMI with 5% FCS/1 mM MgCl2/1 mM CaCl2. The resulting suspension was pelleted by centrifugation, resuspended in 44% Percoll (Pharmacia, Uppsala, Sweden) layered on 67.5% Percoll, and centrifuged at 600g. Cells at the gradient interface were harvested and washed extensively before use.
Results
BM-derived or non-BM-derived cells can provide IL-15 for memory CD8 T-cell proliferation
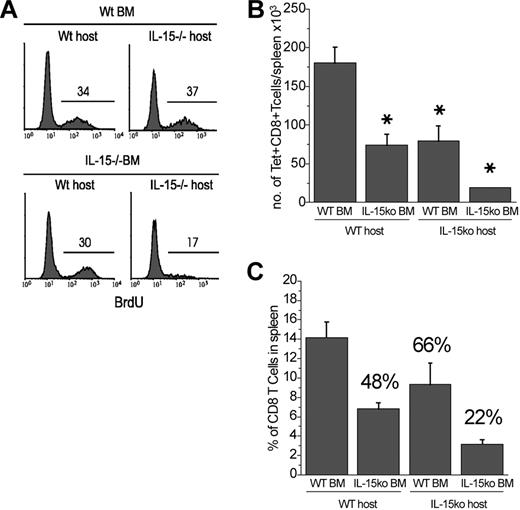
To define which cell types can provide IL-15 for IL-15-mediated memory CD8 T-cell proliferation, BM chimeras were generated in which IL-15 was expressed by either radiation-sensitive BM-derived cells or by radiation-resistant parenchymal cells. Ten weeks after reconstitution, the chimeras were infected with VSV to generate VSV-specific memory CD8 T cells. To examine the basal division of the memory CD8 T cells, chimeras were given BrdU in the drinking water during the memory phase (day 40-70 after infection) and BrdU incorporation by the memory CD8 T cells was measured. In Wt → Wt chimeras, 34% of tetramer-positive memory CD8 T cells incorporated BrdU during the previous 30 days (Figure 1A). In Wt → IL-15-/- or IL-15-/- → Wt chimeras, tetramer-positive memory CD8 T cells incorporated similar levels of BrdU as those in control chimeras (Figure 1A). However, tetramer-positive memory CD8 T cells in the IL-15-/- → IL-15-/- chimeras had little BrdU incorporation (Figure 1A).
IL-15 produced by BM-derived or non-BM-derived cells can mediate memory CD8 T-cell proliferation. Combinations of BM chimeras were generated using IL-15-/- and B6 mice as a source of BM or as hosts. Ten weeks after reconstitution, mice were infected with VSV. Forty days after infection, mice were given BrdU in their drinking water for 4 weeks. Mice were killed and spleen cells were stained with anti-BrdU, N-tetramer, and anti-CD8. Panel A shows the BrdU intensity of N-tetramer-positive, CD8+ gated cells (*P < .05). (B) The total number of N-tetramer-positive cells recovered from spleens 10 weeks after VSV infection. (C) The percentage of CD8 T cells present in the spleen of each type of BM chimera. The values above each bar represent the percentage of control (Wt → Wt). Error bars indicate standard deviation.
IL-15 produced by BM-derived or non-BM-derived cells can mediate memory CD8 T-cell proliferation. Combinations of BM chimeras were generated using IL-15-/- and B6 mice as a source of BM or as hosts. Ten weeks after reconstitution, mice were infected with VSV. Forty days after infection, mice were given BrdU in their drinking water for 4 weeks. Mice were killed and spleen cells were stained with anti-BrdU, N-tetramer, and anti-CD8. Panel A shows the BrdU intensity of N-tetramer-positive, CD8+ gated cells (*P < .05). (B) The total number of N-tetramer-positive cells recovered from spleens 10 weeks after VSV infection. (C) The percentage of CD8 T cells present in the spleen of each type of BM chimera. The values above each bar represent the percentage of control (Wt → Wt). Error bars indicate standard deviation.
Quantitating the total number of tetramer-positive cells in each group revealed that fewer antigen-specific cells were present in the Wt → IL-15-/- and IL-15-/- → Wt chimeras compared with the control chimeras (Wt → Wt; Figure 1B). In addition, the memory cells in chimeras completely lacking IL-15 were further decreased compared with the mixed chimeras and the control chimeras (P < .05). The decrease in the number of tetramer-positive cells present in each group was primarily reflective of a decrease in total CD8 T-cell numbers. The chimeras that lack IL-15 expression in either the parenchymal or BM-derived cells had a decreased ability to develop normal percentages of CD8 T cells (approximately 50%-60% of control) and chimeras devoid of IL-15 had a further decrease in the percent of CD8 T-cell numbers (approximately 25% of control; Figure 1C). Therefore, IL-15 from both the parenchymal and BM-derived cells was essential for normal CD8 T-cell development. In contrast, once memory CD8 T cells had developed, IL-15 from either cell type was sufficient to sustain memory CD8 T-cell proliferation.
IL-15Rα expression by memory CD8 T cells is not required for their maintenance
Our previous studies suggest that IL-15Rα is expressed by memory CD8 T cells.11 Therefore, we tested whether expression of IL-15Rα by memory CD8 T cells was required for their proliferation. To do so, we used mixed BM chimeras that allow IL-15Rα+/+ and IL-15Rα-/- CD8 T cells to be compared within the same host. Thus, BM from IL-15Rα-/- mice (Ly5.1) and wild-type mice (Ly5.1/Ly5.2) were mixed and injected into irradiated wild-type hosts (Ly5.2). Because of the differential expression of Ly5 isoforms, cells from each source can be distinguished. After the hematopoietic compartment was regenerated, mice were infected with VSV and the CD8 T-cell response was analyzed.
Our previous data demonstrated that the expansion phase of the immune response was normal in IL-15Rα-/- mice. However, during the contraction phase, tetramer-positive cells began to decrease compared with controls.11 Furthermore, during the memory phase, the number of IL-15Rα-/- VSV-specific memory CD8 T cells declined faster than in the controls due to the inability to maintain proliferation.11 If IL-15-mediated proliferation requires IL-15Rα expression by the memory CD8 T cells then we would predict that in the mixed BM chimeras IL-15Rα-/- CD8 memory T cells would decline more rapidly than their normal counterparts. On the contrary, the percentage of tetramer-positive CD8 T cells among IL-15Rα-/- and IL-15Rα+/+ cells remained similar throughout the contraction and memory phases in the mixed BM chimeras (Figure 2A).
IL-15Rα expression by memory CD8 T cells is not required for their proliferation. A mixture of BM from IL-15Rα-/- (Ly5.1) and wild-type mice (Ly5.1/5.2) was injected into lethally irradiated wild-type mice (Ly5.2). After reconstitution, chimeras were infected with VSV to analyze a viral CD8 T-cell response. (A) The percentage of N-tetramer-positive cells present in the peripheral blood was measured at various times after VSV infection. Wild-type and IL-15Rα-/- cells were distinguished by the gating on Ly5.1/5.2+ and Ly5.1+ cells, respectively. Error bars indicate SD. (B) Sixty days after VSV infection, BrdU was added to drinking water for 4 weeks. Lymphocytes from spleens and lungs were isolated and stained with anti-BrdU, N-tetramer, anti-CD8, and anti-Ly5.2. Histograms show BrdU incorporation of N-tetramer-positive CD8+ T cells from either Ly5.2+ (wild-type) or Ly5.2- (IL-15Rα-/-) cells. Horizontal lines demarcate BrdU-positive cells and the numbers indicate the percentage of BrdU-positive cells.
IL-15Rα expression by memory CD8 T cells is not required for their proliferation. A mixture of BM from IL-15Rα-/- (Ly5.1) and wild-type mice (Ly5.1/5.2) was injected into lethally irradiated wild-type mice (Ly5.2). After reconstitution, chimeras were infected with VSV to analyze a viral CD8 T-cell response. (A) The percentage of N-tetramer-positive cells present in the peripheral blood was measured at various times after VSV infection. Wild-type and IL-15Rα-/- cells were distinguished by the gating on Ly5.1/5.2+ and Ly5.1+ cells, respectively. Error bars indicate SD. (B) Sixty days after VSV infection, BrdU was added to drinking water for 4 weeks. Lymphocytes from spleens and lungs were isolated and stained with anti-BrdU, N-tetramer, anti-CD8, and anti-Ly5.2. Histograms show BrdU incorporation of N-tetramer-positive CD8+ T cells from either Ly5.2+ (wild-type) or Ly5.2- (IL-15Rα-/-) cells. Horizontal lines demarcate BrdU-positive cells and the numbers indicate the percentage of BrdU-positive cells.
To determine if the IL-15Rα-/- memory CD8 T cells underwent a normal level of cell division, the chimeras were treated with BrdU for 4 weeks. A similar level of BrdU incorporation was observed in both IL-15Rα-/- and wild-type tetramer-positive memory CD8 T cells from the spleen. As a substantial population of virus-specific memory CD8 T cells is also found in nonlymphoid tissues,31 the lymphocytes of the lung were analyzed as a representative nonlymphoid population. It is thought that memory T cells residing in nonlymphoid tissues may have different attributes than lymphoid-resident memory T cells.31,32 Whereas there was consistently less BrdU incorporation by lung IL-15Rα-/- memory CD8 T cells compared with controls, this effect was not statistically significant. These data suggested that IL-15Rα expression by memory CD8 T cells was not required for the proliferation that maintains the memory CD8 T-cell pool.
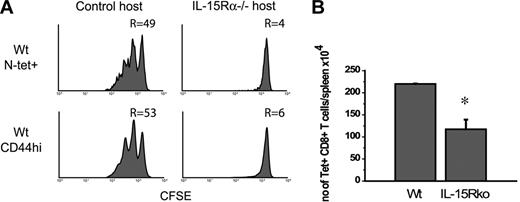
Host cell IL-15Rα expression is crucial for memory CD8 T-cell proliferation
The finding that IL-15Rα-/- memory CD8 T cells present in a normal environment divided at a normal rate posed the question of whether normal memory CD8 T cells proliferate in an environment lacking IL-15Rα. CD8 T cells from VSV-infected wild-type mice were labeled with CFSE and transferred into either wild-type or IL-15Rα-/- hosts. Over the next 4 weeks, both tetramer-positive memory CD8 T cells and CD44hi memory phenotype CD8 T cells divided at a similar rate with approximately 50% of the CD8 T cells responding (Figure 3A). However, the same populations of memory CD8 T cells failed to divide in IL-15Rα-/- hosts (Figure 3A). This lack of basal proliferation of memory CD8 T cells in IL-15Rα-/- hosts resulted in a decrease in the number of N-tetramer-positive CD8 T cells recovered from the spleen (Figure 3B).
IL-15Rα expression by host cells is crucial for memory CD8 T-cell proliferation. Spleen cells from VSV-infected B6 mice were enriched for CD8 T cells, labeled with CFSE, and transferred to either normal or IL-15Rα-/- hosts. Approximately 10 × 106 CD8 T cells containing 0.5 × 106 tetramer-positive cells were transferred into each mouse. Mice were killed 4 weeks later. (A) Lymphocytes from spleen were analyzed for CFSE intensity after gating on either N-tetramer-positive CD8+ T cells or CD44hiCD8+ T cells. R indicates the percent of cells that responded. Panel B shows the number of tetramer-positive cells recovered from the spleens of each group of mice. Error bars indicate SD (P < .05).
IL-15Rα expression by host cells is crucial for memory CD8 T-cell proliferation. Spleen cells from VSV-infected B6 mice were enriched for CD8 T cells, labeled with CFSE, and transferred to either normal or IL-15Rα-/- hosts. Approximately 10 × 106 CD8 T cells containing 0.5 × 106 tetramer-positive cells were transferred into each mouse. Mice were killed 4 weeks later. (A) Lymphocytes from spleen were analyzed for CFSE intensity after gating on either N-tetramer-positive CD8+ T cells or CD44hiCD8+ T cells. R indicates the percent of cells that responded. Panel B shows the number of tetramer-positive cells recovered from the spleens of each group of mice. Error bars indicate SD (P < .05).
IL-15Rα expression on BM-derived cells is critical to memory CD8 T-cell proliferation
Since host IL-15Rα expression was important for memory CD8 T-cell proliferation, we examined which cell types were involved in this process. BM chimeras were generated with differential expression of IL-15Rα on either BM-derived or non-BM-derived cells and were used as recipients of CFSE-labeled memory CD8 T cells. In this situation, the memory CD8 T cells are potentially IL-15Rα+ but the hosts have a mixed IL-15Rα expression pattern. Lymphocytes from the lung were also examined to determine whether differential expression of IL-15Rα within the tissues mediates memory CD8 T-cell proliferation.
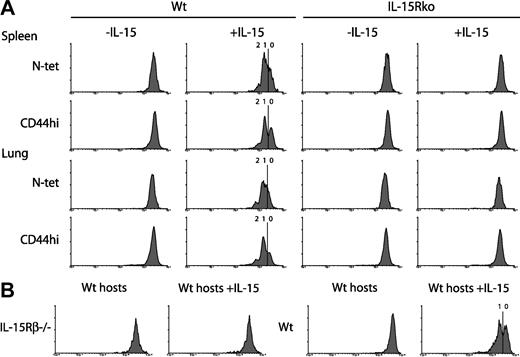
Normal memory CD8 T cells proliferated in chimeras that expressed IL-15Rα in all cell types (Figure 4A). Forty percent of the VSV-specific memory CD8 T cells responded, whereas 65% of the CD44hi memory CD8 T cells responded (Figure 4A). Tetramer-positive and CD44hi memory CD8 T cells also divided in chimeras expressing IL-15Rα only on BM-derived cells, suggesting that expression restricted to BM-derived cells was sufficient to maintain memory CD8 T-cell proliferation (Figure 4A). In contrast, memory CD8 T cells transferred into chimeras that expressed IL-15Rα only on parenchymal cells divided very little (Figure 4A). This amount of cell division was slightly higher than in chimeras lacking IL-15Rα expression indicating that IL-15Rα expression by non-BM-derived cells may play a minor role in driving memory cell proliferation. Alternatively, although perhaps unlikely, a small population of radiation-resistant cells could participate. Analysis of total cell numbers recovered from the spleens also demonstrated that tetramer-positive memory CD8 T cells were decreased by at least half in chimeras with parenchymal IL-15Rα expression compared with those with IL-15Rα expression by BM-derived cells (P < .05; Figure 4B). These data were evidence that IL-15Rα expression by BM-derived cells was crucial for mediating memory CD8 T-cell proliferation.
IL-15Rα expression by BM-derived cells mediates memory CD8 T-cell proliferation. Spleen cells from VSV-infected B6 mice were enriched for CD8 T cells, labeled with CFSE, and transferred to various BM chimeras (10 × 106 CD8 T cells/mouse). Forty days after transfer, lymphocytes from spleen (SP) and lung (LG) were analyzed for CFSE intensity, N-tetramer reactivity, and CD8 and CD44 expression. (A) Histograms showing intensity of CFSE on N-tetramer-positive CD8+ T cells and CD44hiCD8+ T cells. R indicates the percent of cells that responded. (B) Comparison of the amount of tetramer-positive CD8+ T cells recovered from the spleen and the lung from each group of BM chimeras. Control chimeras are represented by the Wt → Wt. Error bars indicate SD (P < .05).
IL-15Rα expression by BM-derived cells mediates memory CD8 T-cell proliferation. Spleen cells from VSV-infected B6 mice were enriched for CD8 T cells, labeled with CFSE, and transferred to various BM chimeras (10 × 106 CD8 T cells/mouse). Forty days after transfer, lymphocytes from spleen (SP) and lung (LG) were analyzed for CFSE intensity, N-tetramer reactivity, and CD8 and CD44 expression. (A) Histograms showing intensity of CFSE on N-tetramer-positive CD8+ T cells and CD44hiCD8+ T cells. R indicates the percent of cells that responded. (B) Comparison of the amount of tetramer-positive CD8+ T cells recovered from the spleen and the lung from each group of BM chimeras. Control chimeras are represented by the Wt → Wt. Error bars indicate SD (P < .05).
Analysis of lung lymphocytes showed that irrespective of the pattern of IL-15Rα expression, donor CD8 T cells migrated efficiently to the lung. Interestingly, in hosts expressing IL-15Rα in all tissues, VSV-specific memory CD8 T cells in the lung had undergone less cell divisions than their splenic counterparts (Figure 4A). Surprisingly, IL-15Rα expression in either BM-derived cells or the parenchyma could drive low levels of proliferation of tetramer-positive memory CD8 T cells in the lung (Figure 4A). This dependence for IL-15Rα on both BM-derived cells and parenchymal cells was also reflected in the total cell numbers recovered from the lung (Figure 4B). In contrast, the CD44hi memory-phenotype CD8 T cells in the lung were similar to the memory CD8 T cells in the spleen in that the IL-15Rα expression on BM-derived cells appeared to be more important for cell division (Figure 4A), although, as with tetramer-positive cells, fewer CD44hi cells divided in the lung. This data suggest that virus-specific memory CD8 T cells in the lung had a lower rate of division than the virus-specific memory CD8 T cells in the spleen and were less dependent on IL-15Rα expression by BM-derived cells.
Transregulation of IL-15-mediated proliferation
Recent reports have demonstrated that IL-15Rα can present IL-15 in an active form to opposing cells to induce IL-15-mediated effects in vitro.20,21 Whereas the presentation of IL-15 required expression of IL-15Rα on the opposing cell, the responding cell only needed to express the IL-2/15Rβ and γC complex.20 The hypothesis that IL-15Rα acts as a presentation molecule could explain how the expression of IL-15Rα on host cells was crucial for IL-15-mediated proliferation of memory CD8 T cells. Short-term in vivo treatment with rIL-15 induces a burst of proliferation in memory-phenotype CD8 T cells.18 Thus, this system was used to test the ability of memory CD8 T cells to respond to IL-15 in the presence or absence of IL-15Rα. CD8 T cells from VSV-infected mice were enriched, labeled with CFSE, and transferred into either control or IL-15Rα-/- mice. One day after transfer, mice were given rIL-15. Three days after IL-15 treatment, lymphocytes were isolated and memory CD8 T-cell populations were analyzed for cell division. In untreated control mice, tetramer-positive and memory-phenotype CD8 T cells did not divide over the 3-day period (Figure 5A). IL-15 treatment induced proliferation of memory CD8 T cells (tetramer-positive and CD44hi populations) in the spleen and lung of control mice with approximately 50% of the cells responding (Figure 5A). In contrast, memory CD8 T cells present in IL-15Rα-/- hosts failed to undergo division in either the spleen or the lung in the presence of IL-15 (Figure 5A). As memory CD8 T cells express IL-15Rα but were unable to respond to IL-15 in IL-15Rα-deficient hosts, this finding indicated that IL-15-mediated functions required transpresentation of IL-15 by IL-15Rα in vivo.
Memory CD8 T-cell responses to IL-15 require IL-15Rα expression by opposing cells and IL-15Rβ expression by memory CD8 T cells. (A) Spleen cells from VSV-infected B6 mice were enriched for CD8 T cells, labeled with CFSE, and transferred to either normal or IL-15Rα-/- hosts. Approximately 10 × 106 CD8 T cells containing 0.5 × 106 tetramer-positive cells were transferred into each mouse, followed by treatment with 2.5 μg of rIL-15 intravenously. Three days after IL-15 treatment, lymphocytes from spleen and lung were analyzed for CFSE intensity on N-tetramer-positive CD8+ T cells and CD44hiCD8+ T cells. In the second column, the division peaks are labeled with a demarcation between the zero and first divisions. (B) Spleen and lymph node (LN) cells from IL-2/15Rβ-/- mice or wild-type mice were enriched for CD8 T cells, labeled with CFSE, and transferred into normal Ly5.2 hosts, and treated with rIL-15 intravenously. Three days later, lymphocytes from spleen were analyzed for CFSE intensity on Ly5.1+CD44hiCD8+T cells.
Memory CD8 T-cell responses to IL-15 require IL-15Rα expression by opposing cells and IL-15Rβ expression by memory CD8 T cells. (A) Spleen cells from VSV-infected B6 mice were enriched for CD8 T cells, labeled with CFSE, and transferred to either normal or IL-15Rα-/- hosts. Approximately 10 × 106 CD8 T cells containing 0.5 × 106 tetramer-positive cells were transferred into each mouse, followed by treatment with 2.5 μg of rIL-15 intravenously. Three days after IL-15 treatment, lymphocytes from spleen and lung were analyzed for CFSE intensity on N-tetramer-positive CD8+ T cells and CD44hiCD8+ T cells. In the second column, the division peaks are labeled with a demarcation between the zero and first divisions. (B) Spleen and lymph node (LN) cells from IL-2/15Rβ-/- mice or wild-type mice were enriched for CD8 T cells, labeled with CFSE, and transferred into normal Ly5.2 hosts, and treated with rIL-15 intravenously. Three days later, lymphocytes from spleen were analyzed for CFSE intensity on Ly5.1+CD44hiCD8+T cells.
To demonstrate that IL-15-mediated signaling was directly responsible for CD8 memory T-cell proliferation, CD8 T cells from IL-2/15Rβ-/- mice were tested for the ability to respond to soluble IL-15 in vivo. CD8 T cells from IL-2/15Rβ-/- were labeled with CFSE and transferred to normal hosts, followed by an injection of rIL-15. After 3 days, CD44hiCD8 T cells from normal mice divided in response to rIL-15, whereas the CD44hiCD8 T cells from IL-2/15Rβ-/- mice failed to divide (Figure 5B). The lack of proliferation in IL-2/15Rβ-/- CD8 T cells indicated that the proliferation of memory CD8 T cells was the result of direct IL-15 action on the T cells. Together with the data that IL-15Rα expression was required by opposing cells to drive memory cell proliferation strongly supported the hypothesis that IL-15Rα presents IL-15 to T cells resulting in a signal mediated by the IL-2/15Rβ/γC receptor.
Discussion
This study examined the requirements for IL-15 and IL-15Rα expression for mediating proliferation of virus-specific memory CD8 T cells. As both IL-15 and IL-15Rα have a broad expression pattern, we asked how the IL-15-mediated proliferation of memory CD8 T cells was regulated. Based primarily on in vitro studies, it was thought that IL-15 was produced by non-T cells in a secreted form and bound the high-affinity receptor complex on T cells to induce IL-15-mediated events such as proliferation. Therefore, it was surprising that IL-15Rα expression by memory CD8 T cells was not required for IL-15-mediated proliferation. This result was also obtained in a system using T-cell receptor (TCR) transgenic memory cells induced by soluble antigen and adjuvant.21 One possibility was that IL-15 was acting indirectly on another non-CD8 T cell through the high-affinity IL-15R complex to induce a sequential signal that directly mediates memory CD8 T-cell proliferation. However, there has not yet been another factor identified, besides IL-15, that is required for cell division of memory CD8 T cells. Furthermore, we show in this paper that IL-15-mediated proliferation of CD8 T cells requires the CD8 T cells to express a major signaling component of the IL-15R complex (ie, the IL-15Rβ subunit). An alternative hypothesis was recently proposed by Dubois et al20 suggesting that IL-15Rα can present IL-15 to opposing cells. This hypothesis is attractive as it still allows IL-15 to act directly on T cells, which is consistent with past observations of IL-15 actions. Our current study provided 2 pieces of evidence that IL-15Rα presented IL-15 in trans to memory CD8 T cells in vivo. First, we demonstrated that IL-15Rα expression by opposing BM-derived cells was required for long-term basal proliferation of memory CD8 T cells. Second, proliferation of memory CD8 T cells in response to soluble IL-15 required IL-15Rα expression by the host cells and IL-15Rβ expression by the responding CD8 T cells.
Although our results and the results of others21 showed that memory CD8 T-cell IL-15Rα expression was not required for proliferation, it remains possible that IL-15Rα expression by CD8 T cells could be advantageous. Indeed, Berard et al33 demonstrate that survival of CD8 T cells in vitro does not require IL-15Rα but the presence of IL-15Rα enhanced the sensitivity of cells to low concentrations of IL-15. In the future, using a more sensitive analysis or analyzing longer time points, we may be able to observe that IL-15Rα-negative memory CD8 T cells undergo less division or have decreased survival. Alternatively, the expression of IL-15Rα on CD8 T cells may not be advantageous during the memory phase but rather prior to or during an immune response. Memory CD8 T cells respond to soluble IL-15 in vitro suggesting that under circumstances when high concentrations of IL-15 are present, memory CD8 T cells may not require transpresentation by IL-15Rα. We also wonder if either CD4 T cells or naive CD8 T cells are able to respond to the presentation of IL-15. Is the decreased responsiveness of CD4 T cells and naive CD8 T cells to IL-15 due to their decreased ability to respond to IL-15 in trans? If so, is this due to the lower expression of IL-2/15Rβ chain on these T-cell subsets or due to the absence of a coreceptor that has yet to be identified? Future studies will need to define which cell types respond to presentation of IL-15 by IL-15Rα and the molecular components required.
As many cell types express IL-15Rα mRNA,16 one can speculate that any cell that expresses IL-15Rα may be able to provide IL-15 to memory CD8 T cells. On the contrary, our study indicated that a specific BM-derived cell type presented IL-15 to memory CD8 T cells. This may indicate that other non-BM-derived cell types do not express IL-15Rα protein or that these BM-derived cells have additional attributes that enhance their competence to present IL-15. The cell types that are considered as potential candidates of IL-15 presentation are B cells, CD4 cells, natural killer (NK) cells, monocytes and macrophages, and dendritic cells. We do not believe that B cells are a major cell type presenting IL-15 to CD8 T cells, as B cells from IL-15Rα+ mice, which were present along with the transferred CD8 T cells, were not sufficient to allow memory CD8 T-cell proliferation. CD4 T cells are also not likely required for IL-15-mediating proliferation as CD4 T cells may have an inhibitory role on memory CD8 T-cell proliferation. Specifically, studies have shown that the presence of CD25+CD4 T cells correlates with a decrease in memory CD8 T-cell proliferation.34,35 This is one reason CD4 T cells were depleted from our transferred populations. We have also found that complete depletion of CD4 T cells from the host did not inhibit the basal proliferation of transferred memory CD8 T cells (K.S.S., L.L., unpublished observations, May 2003). Dendritic cells (DCs) are good candidates for being the crucial IL-15-presenting cell type as DCs are notorious for interacting intimately with T cells, produce IL-15, and require IL-15 signals for optimal antigen-presenting functions.36-39 More complicated experiments will need to be performed to further elucidate the specific cell type that presents IL-15 to memory CD8 T cells.
Whereas memory CD8 T-cell proliferation requires a BM-derived cell type to express IL-15Rα, memory CD8 T cells do not have a similar requirement for the cell type producing IL-15. This suggests that IL-15 is being produced by multiple cell types, acquired by the BM-derived cells, and then presented to the memory CD8 T cells. The requirement for memory CD8 T cells to proliferate in response to IL-15 only through transpresentation suggests that this response requires an adequate amount of both IL-15 and IL-15Rα. The expression levels of IL-15 and IL-15Rα may be quite different in various tissues. Theoretically, memory CD8 T cells residing in tissues with inadequate levels of IL-15Rα would undergo very little division, despite the amount of IL-15 protein produced in that site. Alternatively, a particular tissue may have adequate amounts of IL-15Rα but a lower level of IL-15 protein expression leading to a high portion of unoccupied IL-15Rα. As we often observed less cell division of memory CD8 T cells in the lung compared with the spleen, this may be an indication that the lung has a lower expression level of IL-15Rα than the spleen, contains less IL-15Rα+ BM-derived cells than the spleen, or has a lower expression of IL-15. All these situations would lead to fewer opportunities for memory CD8 T cells to encounter IL-15 in a presented form. Our experiments in which mice were treated with rIL-15 demonstrated that memory CD8 T cells in the lung and the spleen had a similar division pattern indicating that both memory CD8 T-cell populations were equally responsive to IL-15. This data suggested that an adequate number of IL-15Rα molecules were present in the lung but that the level of unoccupied IL-15Rα molecules may be higher than that found in the spleen.
Differences in memory CD8 T-cell proliferation in the lung and spleen could also be unrelated to IL-15 and IL-15Rα expression. Memory CD8 T cells that differentiated in the lung during an immune response may be quite different than the splenic memory CD8 T cells that migrate there during the memory phase. Memory T cells have been shown to be further divided into central and effector subsets with each subset having a differential tissue localization, migratory potential, and proliferation rate.31,32,40 Whether each subset has a similar dependence or responsiveness to IL-15 requires further analysis.
The survival of memory T cells is another crucial component of memory T-cell maintenance and IL-15 has been shown to increase T-cell survival.41 In the absence of IL-15-mediated proliferation, we do not observe any defects on memory CD8 T-cell survival as the memory cell numbers that remain are reduced to a level expected of a population that did not divide but was sustained. This is most likely because IL-7 is present and acting as the major survival factor for memory CD8 T cells.10,42 Homeostatic proliferation of naive CD8 T cells in response to a lymphopenic environment requires IL-7 expressed by non-BM-derived cells.42,43 Currently, it is not known whether memory CD8 T cells also receive IL-7 survival signals from non-BM-derived cell types. If that is the case, it would indicate that memory CD8 T cells need to encounter 2 different cell types to maintain homeostasis (ie, IL-15-mediated proliferation signals from BM-derived cells and IL-7-mediated survival signals from non-BM-derived cell types). Various tissues could have different combinations of IL-15- and IL-7-producing cell types that maintain memory CD8 T cells. It is possible that IL-15 only promotes survival when interactions with IL-7-producing stromal cells are limited.
This study provided in vivo evidence that presentation of IL-15 by IL-15Rα on opposing cells was integral to the proliferation of memory CD8 T cells. Novel results from our experiments involving soluble IL-15 treatment in vivo demonstrated that the presentation of IL-15 to memory CD8 T cells was direct and required IL-15Rβ expression by the T cells. Our work also proved that the proliferation of memory CD8 T cells did not require the expression of IL-15 to be restricted to BM-derived cells, in contrast to IL-15Rα expression. However, IL-15Rα expression requirements were distinct between the spleen and the lung. Future studies will focus on identifying the relevant cell type for IL-15 presentation in vivo and on defining the mechanisms of tissue-specific regulation of IL-15R-mediated signals.
Prepublished online as Blood First Edition Paper, September 25, 2003; DOI 10.1182/blood-2003-08-2814.
Supported by National Institutes of Health grants AI41576, AI051583, DK45260 (L.L.) and by National Institutes of Health Postdoctoral Fellowship AI053970 (K.D.K.).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.