Almost 10 years ago, Ryser et al1 reported that cleavage of 2 disulfide bonds in the gp120 surface component of the HIV-1 envelope is required for virion entry into CD4-bearing cells and that cell surface protein disulfide isomerase (PDI) is responsible for this effect. Since that initial report, there have been numerous structural and mechanistic studies of envelope binding, yet exceedingly few of these studies have incorporated any model of dynamic changes in gp120 disulfide bonding. The notable exceptions are papers from Fenouillet et al2 and Barbouche et al3 that have confirmed the original Ryser et al findings. Now, in this issue of Blood, Markovic and colleagues (page 1586) weigh in as the third group to confirm these findings, and they provide new information about the location of PDI in previously undescribed domains of the cell membrane.
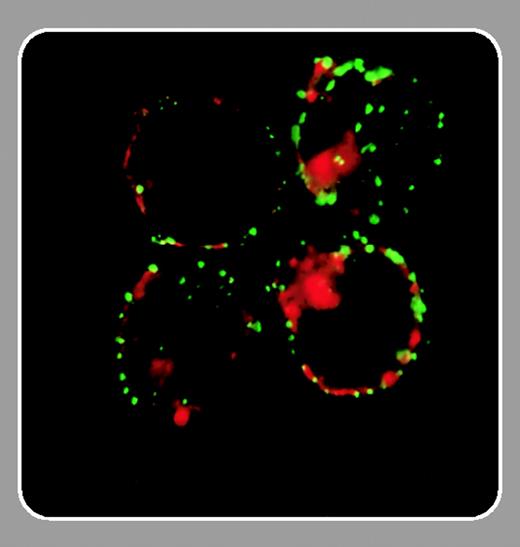
The basic information is as follows: HIV virions, which bear perhaps only a dozen or so envelope spikes, use gp120 to bind to CD4, but this alone serves only to attach the virion loosely to the cell surface. Biophysical evaluation indicates that gp120 has a relatively short off-rate from monomeric CD4, although binding by multiple spikes could increase the avidity of binding.4 An alternative explanation is that once gp120 detaches, it has a high probability of reattaching to an adjacent CD4 molecule on the cell surface, producing the appearance of a long off-rate through a newly recognized phenomenon termed “allovalency.”5 (This explains the long-puzzling finding that soluble CD4 or anti-CD4 antibodies can prevent HIV infection even if added a few minutes after virion adsorption.) Eventually, however, gp120 moves laterally along the membrane surface until it collides with a patch of PDI in a domain of the membrane that Markovic et al distinguish from a typical lipid raft. There, PDI reduces 2 disulfide bonds in gp120, producing conformation changes that likely stabilize the binding of gp120 to CD4 and expose the V3 loop for subsequent binding to the chemokine coreceptor. Following this, gp41 undergoes rearrangement into its fusigenic intermediates and entry occurs (Markovic and colleagues and Reyser et al,1 Fenouillet et al,2 Barbouche et al,3 and Gallina et al6 ).FIG1
Taken in aggregate, the reports from these 3 groups have profound implications for our understanding of the HIV virion surface. As shown by Kwong et al,4 the relatively invariant CD4 binding site in gp120 is kept recessed to prevent access by otherwise neutralizing antibodies. The initial CD4 binding event is but a prelude to PDI-mediated reduction that unfolds the envelope into a more open conformation that presumably binds more favorably to CD4 and to the chemokine coreceptor. If evasion of neutralizing antibodies is the likely evolutionary reason for this shuffling two-step at entry, then it would be interesting to know if a PDI-rearranged envelope is a better vaccine immunogen for raising neutralizing antibodies. PDI is too ubiquitous an enzyme to use as a drug target.6 However, just as drugs have been developed that block CD4 binding, chemokine coreceptor binding, and now, most successfully, gp41-mediated fusion, it will be interesting to learn if the PDI-rearrangement step in gp120 could provide a new therapeutic target.