Abstract
Combinations of hematopoietic cytokines and the ventral mesoderm inducer BMP-4 have recently been shown to augment hematopoietic cell fate of human embryonic stem cells (hESCs) during embryoid body (EB) development. However, factors capable of regulating lineage commitment of hESC-derived hematopoiesis have yet to be reported. Here we show that vascular endothelial growth factor (VEGF-A165) selectively promotes erythropoietic development from hESCs. Effects of VEGF-A165 were dependent on the presence of hematopoietic cytokines and BMP-4, and could be augmented by addition of erythropoietin (EPO). Treatment of human EBs with VEGF-A165 increased the frequency of cells coexpressing CD34 and the VEGF-A165 receptor KDR, as well as cells expressing erythroid markers. Although fetal/adult globins were unaffected, VEGF-A165 induced the expression of embryonic zeta (ζ) and epsilon (ϵ) globins, and was accompanied by expression of the hematopoietic transcription factor SCL/Tal-1. In addition to promoting erythropoietic differentiation from hESCs, the presence of VEGF-A165 enhanced the in vitro self-renewal potential of primitive hematopoietic cells capable of erythroid progenitor capacity. Our study demonstrates a role for VEGF-A165 during erythropoiesis of differentiating hESCs, thereby providing the first evidence for a factor capable of regulating hematopoietic lineage development of hESCs.
Introduction
Vascular endothelial growth factor (VEGF-A165) is a multifunctional cytokine that plays a prominent role in normal vascular biology by regulating numerous cellular responses of endothelial precursors including proliferation, differentiation, migration, and apoptosis.1-6 In addition, a role for VEGF-A165 in hematopoietic differentiation has been identified,7-10 and has been extended to primitive hematopoietic cells capable of repopulation from mouse embryonic stem cells (ESCs),11 and by targeted gene disruption of VEGF-A165 or its tyrosine kinase receptor VEGFR2/KDR/Flk-1 (hereafter KDR).12-14 Furthermore, a role for VEGF-A165 in early developmental events of primitive and definitive erythroid lineages from mouse ESCs has been established.15 This latter observation indicates a potential function of VEGF-A165 in cellular events leading to the emergence of mouse hematopoiesis that specifically affects erythroid differentiation.
During mammalian embryogenesis, erythropoiesis occurs in 2 waves: the primitive wave, which occurs and remains confined to the extra-embryonic yolk sac,16-18 is followed by the definitive wave, which originates in the yolk sac and/or within the embryo proper,19,20 which then sequentially migrates to the fetal liver and ultimately to the bone marrow.18 Definitive and primitive erythroid cells derived from mouse ESCs are morphologically distinct9,21 and can be molecularly distinguished by differences in globin expression, where primitive erythroid cells express the embryonic ζ and ϵ globins whereas definitive cells express the adult β globin.22-25 Mammalian erythropoiesis from uncommitted pluripotent stem cells is an early cellular differentiation event that can be characterized by sequential progress through stages of progenitor development that can be assayed from erythroid blast-forming units (BFU-Es) to erythroid colony-forming units (CFU-Es) and eventually maturation into erythroblasts, normoblasts, reticulocytes, and finally enucleated mature erythrocytes.26 This complex process is controlled by the combined effects of growth factors, including the erythroid-specific cytokine erythropoietin (EPO).27
Because human embryonic erythropoietic development is inaccessible for in vivo study, an in vitro model allowing the study of this process at both the cellular and molecular levels is necessary. Human embryonic stem cells (hESCs) provide a potential model of early developmental events of cell fate commitment which includes the study of embryonic hematopoiesis.28 Recently, hESCs have been shown to respond to a combination of hematopoietic cytokines and BMP-4 that promotes hESC differentiation toward hematopoietic cell fate.29 However, in vitro manipulation of hESCs to direct or regulate hematopoietic differentiation and blood lineage development have not been explored. Taking advantage of the ability to effectively differentiate hESCs into hematopoietic progenitors that represent primitive erythroid cells by CFU assays, the availability of surrogate markers for stages of erythroid maturation, and patterns of globin expression emerging from mouse ECSs, we examined embryonic erythropoiesis from hESCs. Our study demonstrates that VEGF-A165 acts to promote development of the erythroid lineage, thereby providing evidence for a factor capable of regulating hematopoietic lineage commitment derived from hESCs.
Materials and methods
Undifferentiated hESC cultures and EB formation
Human ESC lines H1 and H930 were maintained as undifferentiated cells by passage in feeder-free culture, as previously described.29 Briefly, hESCs were cultured on matrigel-coated (BD Biosciences, Bedford, MA) plates, with mouse embryonic fibroblast—conditioned medium supplemented with 8 ng/mL human recombinant basic fibroblast growth factor (bFGF) (Invitrogen, Burlington, ON, Canada). Cells were fed daily and passaged weekly to maintain undifferentiated growth, as described.29 On the day of passage, undifferentiated hESCs were treated with 200 U/mL collagenase IV (Invitrogen) and then transferred to low attachement plates to allow erythroid body (EB) formation by overnight incubation in differentiation medium consisting of knockout Dulbecco modified Eagle medium (DMEM) supplemented with 20% non—heat inactivated fetal bovine serum (FBS; Hyclone, Logan, UT), 1% nonessential amino acids, 1 mM l-glutamine, and 0.1 mM β-mercaptoethanol. The next day, cultured EBs were given fresh medium supplemented with the following treatments: human recombinant bone morphogenetic protein 4 (BMP-4; 50 ng/mL; R&D Systems, Minneapolis, MN); human recombinant VEGF-A165 (5 ng/mL unless otherwise stated; R&D Systems); a mixture of human recombinant cytokines (hereafter referred to as cytokines; 300 ng/mL stem cell factor [SCF]; Amgen, Thousand Oaks, CA), 300 ng/mL Flt-3 ligand (Flt-3L; R&D Systems), 10 ng/mL interleukin-3 (IL-3; R&D Systems), 10 ng/mL interleukin-6 (IL-6; R&D Systems), and 50 ng/mL granulocyte colony-stimulating factor (G-CSF; Amgen), or combinations of these treatments (hereafter referred to as BMP-4+VEGF-A165, cytokines+VEGF-A165, cytokines+BMP-4, cytokines+BMP-4+VEGF-A165). In some experiments, human recombinant EPO (3 U/mL; Amgen) was added at the initiation or at day 10 of EB differentiation, in the presence or absence of the indicated treatments. When stated, a neutralizing anti-human VEGF-A165 monoclonal antibody (mAb; R&D Systems) used at a concentration of 2.5 μg/mL was added simultaneously with the indicated treatments at the initiation of EB differentiation. EBs were cultured for 15 days at 37°C and 5% CO2 in a humidified atmosphere, with changes of media and the different treatments every 3 days. Because VEGF-A165 provided statistically similar effects on the development of the erythroid lineage from both H1 and H9 hESCs, all results from both cell lines were combined for this study.
Colony-forming unit (CFU) assays
EBs were dissociated into single-cell suspensions by incubation with 0.4 U/mL Collagenase B (Roche Diagnostics, Laval, QC, Canada) for 2 hours at 37°C, followed by incubation with cell dissociation buffer (Invitrogen) for 10 minutes in a 37°C water bath, gentle pipetting and passage through 40-μm mesh. Dissociated EBs were counted and plated at a density of 1 × 105 cells/mL in Iscove modified Dulbecco medium (IMDM) containing 0.9% methylcellulose H4230 (Stem Cell Technologies, Vancouver, BC, Canada) supplemented with the following recombinant human growth factors: 3 U/mL EPO, 50 ng/mL SCF, 10 ng/mL granulocyte monocyte—colony-stimulating growth factor (GM-CSF; Novartis, Dorval, QC, Canada), and 10 ng/mL IL-3. After 10 to 14 days of incubation at 37°C and 5% CO2 in a humidified atmosphere, clusters of more than 50 cells showing standard morphologic hematopoietic criteria31 were scored as colonies on an inverted microscope, except for the erythroid colonies. Those colonies were considered as positive when composed of 8 to 50 cells and were scored every 3 days between 7 and 28 days of incubation. Colonies composed of erythroid cells, granulocytes, macrophages, both granulocytes and macrophages, or a mixture of these cells were designated as erythroid, CFU-G, CFU-M, CFU-GM, and CFU-mixed, respectively. All CFU-mixed colonies comprised erythroid cells. For flow cytometry, colonies of similar morphology were individually isolated from methylcellulose, pooled, washed 3 times in phosphate-buffered saline (PBS)/3% FBS (Invitrogen) and filtered through 85-μm mesh.
Flow cytometric analyses
Single-cell suspensions of either EBs or colonies were resuspended at approximately 0.2 × 105 cells/mL to 5 × 105 cells/mL in PBS/3% FBS and stained for 30 minutes at 4°C with the following fluorochrome-conjugated mAbs: CD34—allophycocyanin (APC), CD45—fluorescein isothiocyanate (FITC), c-kit—phycoerythrin (PE) (Becton Dickinson Immunocytometry Systems [BDIS], San Jose, CA), c-kit-APC (Caltag Laboratories, Burlingame, CA), and glycophorinA-PE (Beckman Coulter, Marseille, France) or their isotype-matched control mAbs, at a concentration of 5 μg/mL. Cells were then washed twice in PBS/3% FBS and stained with the 7-AAD (7-amino-actinomycin D) viability dye (Beckman Coulter) at 15 μL/mL to 20 μL/mL for 15 minutes at room temperature (RT). For detection of Ep-CAM expression, cells were preincubated with the primary KS1/4 mAb32 (BD Biosciences) and then washed twice prior to addition of the secondary FITC-conjugated goat antimouse IgG antibody (Beckman Coulter). Expression of KDR (Research Diagnostics, Flanders, New Jersey) was analyzed according to the protocol described elsewhere.33 Intracellular expression of fetal (HbF) and adult (HbA) globins was analyzed according to the manufacturer's instructions, using mouse FITC-conjugated anti-HbF (Research Diagnostics) and anti-HbA (PerkinElmer Life Sciences, Norton, ON, Canada) mAbs, respectively. Briefly, 1 × 105 to 2 × 105 cells were resuspended in 1 mL cold 0.05% glutaraldehyde for 10 minutes at RT, washed in PBS/0.1% bovine serum albumin (BSA), then resuspended in 0.5 mL 0.1% Triton X-100 for 5 minutes at RT. After washing, 2.5 μg of antibody was added to the cells in a 100 μL volume for 15 minutes at RT, before washing and resuspension in 200 μL PBS/3% FBS for immediate analysis. Live cells identified by 7-AAD exclusion were analyzed for surface marker expression using a FACSCalibur cell analyzer (BDIS) and Cell Quest software (BDIS). The percentages of positive cells were determined as compared with isotypic controls establishing the background level of nonspecific staining.
Cytospin and Giemsa stainings
To analyze erythroid cell morphology, colonies were individually isolated from methylcellulose by aspiration, washed in PBS, and centrifuged onto slides (Cytospin3; Thermo Shandon, Pittsburgh, PA). After fixation in methanol:acetone (80:20 volume), the slides were stained with Giemsa (Sigma-Aldrich) as previously described.29
Reverse transcription—polymerase chain reaction (RT-PCR) analyses
mRNA was extracted from frozen cell pellets and reverse transcribed into cDNA using mRNA extraction and first strand cDNA synthesis kits (Amersham Biosciences, Baie d-Urfe, QC, Canada) according to the manufacturer's instructions. The specified genes were amplified on a Perkin-Elmer 9700 cycler for 40 cycles using the following primer sets and annealing conditions: globin ζ (400 base pair [bp]) forward primer 5′-CCA AGA CTG AGA GGA CCA TCA TTG and reverse primer 5′-AGG ACA GAG GAT ACG ACC GAT AGG at 64°C; globin ϵ (212 bp) forward primer 5′-AAG ATG AAT GTG GAA GAG GCT GG and reverse primer 5′-TTA GCA AAG GCG GGC TTG AG at 63°C; β globin (394 bp) forward primer 5′-GGG CAG GTT GGT ATC AAG GTT AC and reverse primer 5′-GGG GAA AGA AAA CAT CAA GCG at 62°C; GATA-1 (378 bp) forward primer 5′-TCA ATT CAG CAG CCT ATT CC and reverse primer 5′-TTC GAG TCT GAA TAC CAT CC at 57°C; PU-1 (600 bp) forward primer 5′-CGA CCA TTA CTG GGA CTT CC and reverse primer 5′-TTC TTC TTC ACC TTC TTG ACC at 58°C; SCL/TAL-1 (356 bp) forward primer 5′-ATG GTG CAG CTG AGT CCT CC and reverse primer 5′-ATA TAC TTC ATG GCC AGG CGG at 55°C; and β-actin (222 bp) forward primer 5′-GAT CCA CAT CTG CTG GAA GG and reverse primer 5′-AAG TGT GAC GTT GAC ATC CG at 60°C. For each PCR reaction, the β-actin PCR product, used as an internal invariant control, was simultaneously amplified. The amplified products were separated on 1.5% to 2% agarose gels with ethidium bromide. Intensities of the bands were scanned and normalized to intensities of the β-actin band.
Statistical analyses
Results were expressed as means ± SD. Statistical significance was determined using a 2-tailed Student t test. Results were considered significant when P values were less than .05.
Results
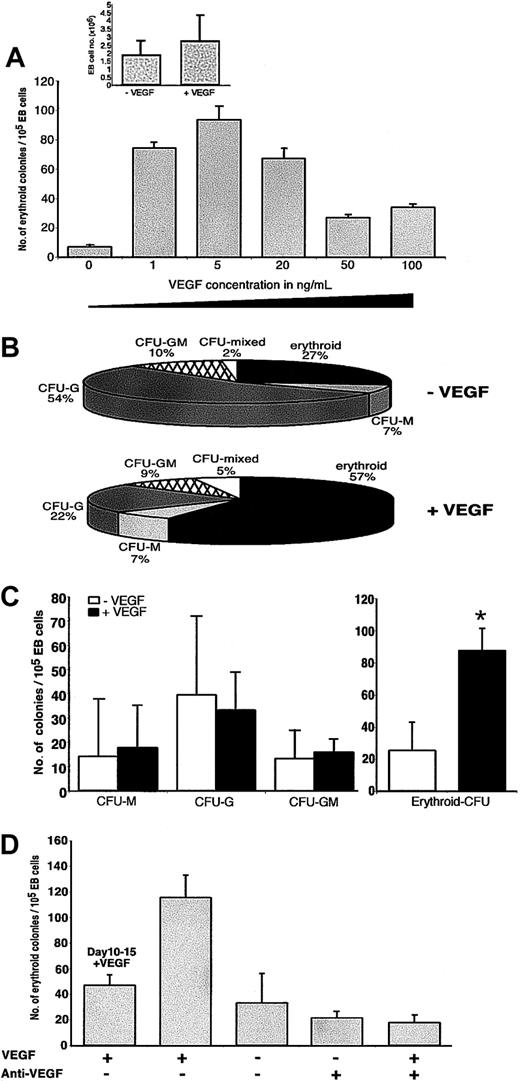
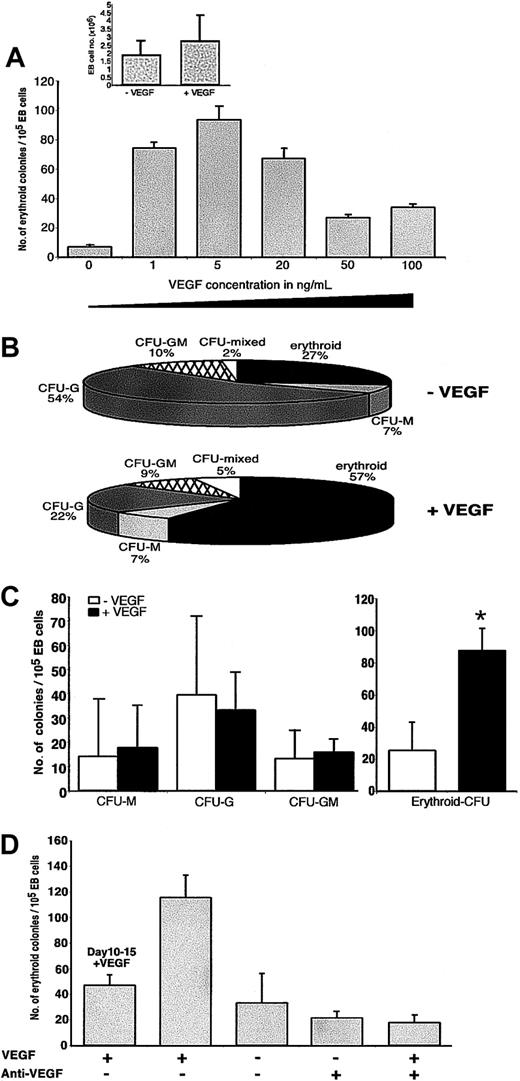
VEGF-A165 specifically promotes in vitro erythroid colony formation from hESCs
As shown previously, after 15 days of EB differentiation in the presence of a mixture of hematopoietic cytokines (SCF, Flt-3L, IL-3, IL-6, G-CSF) and BMP-4,29 hESC lines H1 and H930 could be differentiated into hematopoietic progenitors as detected by multilineage hematopoietic CFU potential. To determine the effects of VEGF-A165 on the differentiation of hESCs, we examined the CFU potential of 1 × 105 cells derived from dissociated EBs that were treated for 15 days with cytokines+BMP-4 alone (hereafter referred to as control EBs) or cytokines+BMP-4+VEGF-A165 (hereafter referred to as VEGF-A165—treated EBs). Addition of VEGF-A165 at a concentration ranging between 1 ng/mL and 20 ng/mL in the presence of cytokines+BMP-4 increased the total number of derived erythroid colonies by 10-fold as compared with control EBs (P = .005; Figure 1A). As such, we chose to use 5 ng/mL in all subsequent experiments. The increased number of erythroid colonies was not associated with an increased proliferation rate of EB cells since the total yield of cells was not statistically different between both types of EBs at day 15 of differentiation (P = .2; Figure 1A, inset). The frequency of the erythroid lineage was also strongly increased by the VEGF-A165 treatment of EBs, averaging 57% compared with only 27% without VEGF-A165 addition (P = .01; Figure 1B). In contrast, addition of VEGF-A165 did not significantly affect commitment of other hematopoietic progenitors, except for CFU-mixed colonies that also comprised erythroid lineages, for which the frequency was also significantly increased (P = .016; Figure 1B). Apparent reduction of the granulocytic lineage (54% of CFU-G colonies derived from control EBs versus 22% from VEGF-A165—treated EBs) only reflected the amplification of the erythroid lineage, as shown by similar absolute numbers (P > .75) of myeloid colonies in the presence or absence of VEGF-A165 (Figure 1C). Altogether, these data suggest a direct supportive role of VEGF-A165 on the erythroid lineage development rather than an indirect role through negative regulation of myeloid lineage development. As shown previously, hematopoietic commitment occurs after day 10 of human EB development in the presence of cytokines and BMP-4.29 To determine if VEGF-A165 was able to affect erythropoietic development subsequent to the commitment of hematopoietic cell fate, we examined the effect of VEGF-A165 treatment between day 10 and day 15 after hematopoietic commitment occurs within treated EBs. As shown in Figure 1C, VEGF-A165 had no effect on erythroid colony formation (both number and frequency) when added at day 10 and for the remaining 5 days of EB differentiation (days 10-15) compared with addition of VEGF-A165 during the entire 15-day period of EB development. Addition of VEGF-A165—neutralizing mAb completely abolished the detectable increase in the number of erythroid colonies derived from VEGF-A165—treated EBs (P = .02), without significantly affecting the number of colonies derived from control EBs (data not shown), suggesting the effects of VEGF-A165 were specific. Our results demonstrate that VEGF-A165 promotes erythroid lineage development from differentiating hESCs prior to hematopoietic cell fate commitment.
VEGF-A165 increases the erythroid colony formation resulting from EB treatment with cytokines+BMP-4. (A-D) Following 15 days of differentiation with cytokines+BMP-4 (-VEGF) or cytokines+BMP-4+VEGF-A165 (+VEGF), EBs were dissociated and subjected to erythroid-myeloid CFU assays by plating 1 × 105 EB cells in methylcellulose, as described in “Materials and methods.” (A) The mean numbers of erythroid colonies are plotted per 1 × 105 EB cells according to the indicated concentrations of VEGF-A165, added at the initiation of EB differentiation (n = 6 experiments for each hESC line). Total numbers of cells recovered from dissociated EBs at day 15 after treatment with or without VEGF-A165 were determined by trypan blue exclusion (inset; n = 11). (B) The percentage of the erythroid subtype among all CFU subtypes is shown for the indicated EB treatments (n = 6 for each treatment and each hESC line). (C) The mean numbers of myeloid (left) and erythroid (right) colonies generated after EB treatment with (+VEGF) or without (-VEGF) VEGF-A165 are shown (n = 11). (D) The mean numbers of erythroid colonies are plotted according to the indicated EB treatments. VEGF-A165 was added (+) or not (-) throughout the entire EB differentiation period, either at the initiation (days 0-15) or at day 10 (days 10-15). When stated, a neutralizing anti—VEGF-A165 mAb was also added (+) or not (-) at the initiation of EB (n = 4 experiments for each treatment). For A, C, and D, SDs are represented by vertical bars. *P < .05.
VEGF-A165 increases the erythroid colony formation resulting from EB treatment with cytokines+BMP-4. (A-D) Following 15 days of differentiation with cytokines+BMP-4 (-VEGF) or cytokines+BMP-4+VEGF-A165 (+VEGF), EBs were dissociated and subjected to erythroid-myeloid CFU assays by plating 1 × 105 EB cells in methylcellulose, as described in “Materials and methods.” (A) The mean numbers of erythroid colonies are plotted per 1 × 105 EB cells according to the indicated concentrations of VEGF-A165, added at the initiation of EB differentiation (n = 6 experiments for each hESC line). Total numbers of cells recovered from dissociated EBs at day 15 after treatment with or without VEGF-A165 were determined by trypan blue exclusion (inset; n = 11). (B) The percentage of the erythroid subtype among all CFU subtypes is shown for the indicated EB treatments (n = 6 for each treatment and each hESC line). (C) The mean numbers of myeloid (left) and erythroid (right) colonies generated after EB treatment with (+VEGF) or without (-VEGF) VEGF-A165 are shown (n = 11). (D) The mean numbers of erythroid colonies are plotted according to the indicated EB treatments. VEGF-A165 was added (+) or not (-) throughout the entire EB differentiation period, either at the initiation (days 0-15) or at day 10 (days 10-15). When stated, a neutralizing anti—VEGF-A165 mAb was also added (+) or not (-) at the initiation of EB (n = 4 experiments for each treatment). For A, C, and D, SDs are represented by vertical bars. *P < .05.
VEGF-A165 requires additional factors to optimally promote erythroid progenitors from hESCs
VEGF-A165 has been reported to synergize with BMP-4 to induce generation of lympho-myeloid CFUs including erythroid colonies from differentiated mouse ESCs.34 To determine whether the development of the hESC-derived erythroid lineage could be optimally promoted by combinations of either BMP-4+VEGF-A165, cytokines+BMP-4, cytokines+VEGF-A165, or required the mixture of cytokines+BMP-4+VEGF-A165, we performed CFU assays on cells from EBs treated with these combinations and with each factor alone. As shown in Figure 2A, treatment of EBs with BMP-4+VEGF-A165 enhanced the number of erythroid colonies by at least 2.5-fold as compared with BMP-4 or VEGF-A165 treatment alone (P = .01). Combinations of either cytokines+VEGF-A165 or cytokines+BMP-4 were not able to enhance the number of erythroid colonies as compared with each factor alone (P = .95 and .84, respectively). Only in the presence of cytokines+BMP-4, was VEGF-A165 able to augment the generation of erythroid progenitors (Figure 2A). The likelihood of an indirect effect of VEGF-A165 on erythropoiesis mediated through secretion of IL-6 and/or SCF, cytokines known to promote erythropoiesis,35 was doubtful based on the lack of significant effect (P = .5 for SCF; P = .8 for IL-6) on the number of erythroid colonies formed in the presence or absence of these cytokines (Figure 2A, inset).
VEGF-A165 requires the presence of additional factors to optimally promote erythroid colony formation. EBs were differentiated for 15 days with the indicated treatments and plated in CFU assays as described in Figure 1. (A-B) Mean numbers of erythroid colonies derived from EBs differentiated with the indicated treatments, with the corresponding SD (vertical bars) (n = 3 independent experiments for each EB treatment except for cytokines+BMP-4+VEGF-A165 with n = 6). Inset represents data from similar experiments in which IL-6 or SCF was removed from the cocktail of cytokines (n = 4 with [+] or without [-] IL-6, n = 2 with [+] or without [-] SCF). In panel B, EB differentiatiation was conducted in the presence (+) or absence (-) of EPO added at the initiation of differentiation (n = 3 independent experiments). (C) Morphology under light microscopy of erythroid colonies derived from EBs differentiated with the indicated treatments. Scale bar, 100μm. (D) A representative Giemsa staining performed on 20-day pooled erythroid colonies generated from both VEGF-A165—treated (+VEGF) and control EBs (-VEGF) (n = 2 for each EB treatment). Rare contaminating macrophages are also present. Scale bar, 100 μm.
VEGF-A165 requires the presence of additional factors to optimally promote erythroid colony formation. EBs were differentiated for 15 days with the indicated treatments and plated in CFU assays as described in Figure 1. (A-B) Mean numbers of erythroid colonies derived from EBs differentiated with the indicated treatments, with the corresponding SD (vertical bars) (n = 3 independent experiments for each EB treatment except for cytokines+BMP-4+VEGF-A165 with n = 6). Inset represents data from similar experiments in which IL-6 or SCF was removed from the cocktail of cytokines (n = 4 with [+] or without [-] IL-6, n = 2 with [+] or without [-] SCF). In panel B, EB differentiatiation was conducted in the presence (+) or absence (-) of EPO added at the initiation of differentiation (n = 3 independent experiments). (C) Morphology under light microscopy of erythroid colonies derived from EBs differentiated with the indicated treatments. Scale bar, 100μm. (D) A representative Giemsa staining performed on 20-day pooled erythroid colonies generated from both VEGF-A165—treated (+VEGF) and control EBs (-VEGF) (n = 2 for each EB treatment). Rare contaminating macrophages are also present. Scale bar, 100 μm.
To determine whether the promoting effect of VEGF-A165 on erythroid development derived from EBs treated with cytokines+BMP-4 could function cooperatively with EPO, we examined the erythroid CFU potential of both control and VEGF-A165—treated EBs, in the presence or absence of EPO. Addition of EPO had no effect on EBs differentiated in the presence of cytokines+BMP-4, but had a significant enhancement (2.5-fold) in the number of erythroid colonies derived from VEGF-A165—treated EBs (P = .01). This observation suggested that the erythroid precursors developing within VEGF-A165—treated EBs were responsive to EPO, whereas in the absence of VEGF-A165 signaling, cells within human EBs lack EPO responsiveness. We suggest that both cytokines and BMP-4 are required for VEGF-A165 to augment erythroid development from hESCs, and that this effect can be augmented synergistically with EPO addition.
As depicted in Figure 2C, the gross morphology of erythroid colonies scored with inverted microscopy appeared to differ among EB treatments. Approximately 70% of the colonies derived from EBs treated with VEGF-A165 alone or in the presence of cytokines+BMP-4 (VEGF-A165—treated EBs) possessed a lower cellularity compared with those derived from EBs treated with either cytokines+BMP-4 (control EBs) or each factor alone in the absence of VEGF-A165 (Figure 2C). Erythroid colonies were further examined by Giemsa staining of cytospin preparations. Larger nucleated erythroblasts were detected among cells comprising erythroid colonies derived from VEGF-A165—treated EBs in contrast to control treated EBs (Figure 2D). A morphologic difference of both erythroid progenitors and erythroblasts comprising colonies treated with VEGF-A165 suggests that VEGF-A165 may have an additional role during maturation of progenitors committed to the erythroid lineage.
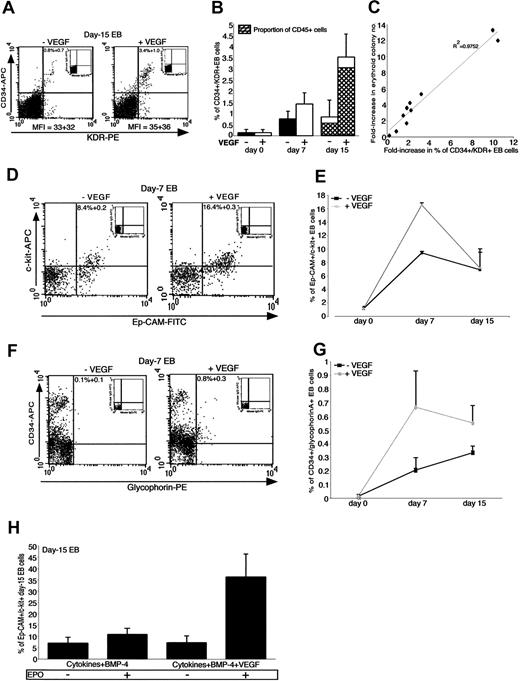
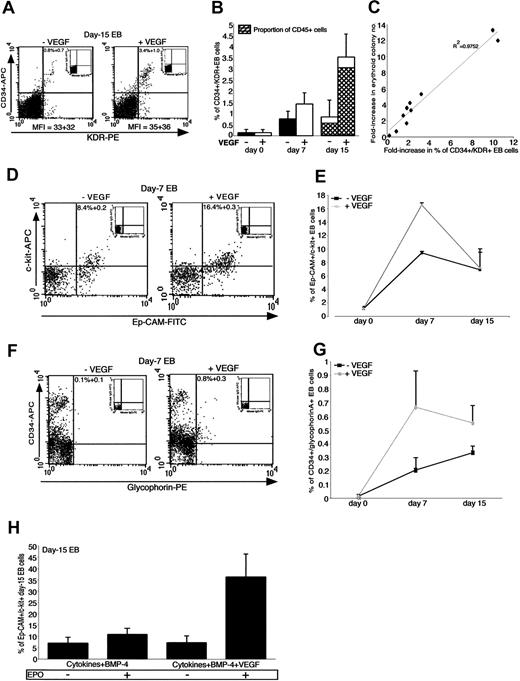
VEGF-A165 promotes the emergence of cells expressing phenotypic characteristics of early erythroid progenitors
Coexpression of CD34 and KDR has been associated with primitive cells possessing progenitor activity.36-38 In order to investigate the potential effect of VEGF-A165 on the emergence of erythroid progenitors during EB development, cells from dissociated EBs were analyzed by flow cytometry for expression of CD34 and KDR. Between days 7 and 15, cells within VEGF-A165—treated EBs coexpressed CD34 and KDR with a higher frequency but a similar fluorescence intensity than cells within control EBs (Figure 3A-B). By day 15, VEGF-A165—treated EBs comprised approximately 3.5% ± 1.0% of CD34+/KDR+ cells compared with 0.8% ± 0.7% for control EBs (P = .005; Figure 3A-B). Both populations comprised 86% ± 7.4% and 84% ± 5.0% cells positive for the hematopoietic marker CD45, respectively (Figure 3B), indicating their higher content in hematopoietic than in endothelial cells. Fold-increase in the percentage of CD34+KDR+ cells within VEGF-A165—treated EBs correlated with number of erythroid colonies (R2 = 0.9752; Figure 3C), whereas no significant correlation of CD34+/KDR+ frequency and erythroid progenitors occurred among EBs in the absence of VEGF-A165 treatment (data not shown).
VEGF-A165 increases the proportions of early progenitors/precursors during EB differentiation. EBs were differentiated in the presence of cytokines+BMP-4 (-VEGF) or cytokines+BMP-4+VEGF-A165 (+VEGF) for the indicated days and analyzed by flow cytometry for coexpression of CD34 and KDR (A-C) as well as of c-kit and Ep-CAM (D-E) and CD34 and glycophorin A (F-G). For panels A, D, and F, dot plot quadrants were based on their isotype controls shown as insets. (A) Represents a flow cytometric analysis performed at day 15 of EB differentiation. Mean fluorescence intensities (MFIs) for KDR expression are indicated. (B) Histograms represent the mean percentage of the CD34+/KDR+ subset in both types of EBs at the indicated days of differentiation, with the corresponding SD (vertical bars) (n = 7 experiments for day 15 and n = 3 for both days 0 and 7). At day 15, the proportion of cells coexpressing CD45 within both CD34+/KDR+ populations are represented by gray bars. (C) Plot showing the straight line fit for the predominance of the CD34+/KDR+ subset at day 15 of VEGF-A165—treated EBs versus the increase in the number of erythroid colonies derived from these EBs. (D, F) Representative flow cytometric analyses of Ep-CAM+/c-kit+ and CD34+/glycophorinA+ coexpressions respectively, performed on control (-VEGF) and VEGF-A165—treated (+VEGF) EBs differentiated for 7 days. (E, G) Kinetics analyses of the mean percentages of the above subsets at the indicated days of EB differentiation. SD are represented by vertical bars (n = 3 to 5 independent experiments for each subset and day). (H) Represents the mean percentages of the Ep-CAM+/c-kit+ subset within EBs differentiated for 15 days with the indicated treatments in the presence (+) or absence (-) of EPO. SD are represented by vertical bars (n = 3 independent experiments).
VEGF-A165 increases the proportions of early progenitors/precursors during EB differentiation. EBs were differentiated in the presence of cytokines+BMP-4 (-VEGF) or cytokines+BMP-4+VEGF-A165 (+VEGF) for the indicated days and analyzed by flow cytometry for coexpression of CD34 and KDR (A-C) as well as of c-kit and Ep-CAM (D-E) and CD34 and glycophorin A (F-G). For panels A, D, and F, dot plot quadrants were based on their isotype controls shown as insets. (A) Represents a flow cytometric analysis performed at day 15 of EB differentiation. Mean fluorescence intensities (MFIs) for KDR expression are indicated. (B) Histograms represent the mean percentage of the CD34+/KDR+ subset in both types of EBs at the indicated days of differentiation, with the corresponding SD (vertical bars) (n = 7 experiments for day 15 and n = 3 for both days 0 and 7). At day 15, the proportion of cells coexpressing CD45 within both CD34+/KDR+ populations are represented by gray bars. (C) Plot showing the straight line fit for the predominance of the CD34+/KDR+ subset at day 15 of VEGF-A165—treated EBs versus the increase in the number of erythroid colonies derived from these EBs. (D, F) Representative flow cytometric analyses of Ep-CAM+/c-kit+ and CD34+/glycophorinA+ coexpressions respectively, performed on control (-VEGF) and VEGF-A165—treated (+VEGF) EBs differentiated for 7 days. (E, G) Kinetics analyses of the mean percentages of the above subsets at the indicated days of EB differentiation. SD are represented by vertical bars (n = 3 to 5 independent experiments for each subset and day). (H) Represents the mean percentages of the Ep-CAM+/c-kit+ subset within EBs differentiated for 15 days with the indicated treatments in the presence (+) or absence (-) of EPO. SD are represented by vertical bars (n = 3 independent experiments).
In contrast to CD36 and CD71, which are expressed widely among early and late stages of human erythropoiesis,39 expression of the epithelial cellular adhesion molecule Ep-CAM has been shown to correlate with immature erythroid progenitors,26,40 whereas glycophorin A expression has served as a late erythroid marker.41 To examine the developmental stage of erythropoiesis affected by VEGF-A165, we compared Ep-CAM and glycophorin A expression on cells derived from EBs treated with or without VEGF-A165. In all experiments, cells expressing glycophorin A within EBs and their derived erythroid colonies never coexpressed CD45 or myeloid markers, indicating restriction to the erythroid lineage (data not shown).
At day 7, VEGF-A165—treated EBs contained 2-fold higher numbers of cells coexpressing Ep-CAM and c-kit (P = .01; Figure 3D) and 3-fold higher levels of cells expressing glycophorin A and CD34 (Figure 3F) compared with control EBs. These amplified differences were, however, transient since the frequency of both populations was similar in VEGF-A165—treated and —untreated EBs by day 15 (Figure 3E,G). In contrast to control treated EBs, EPO increased the percentage of cells coexpressing Ep-CAM and c-kit in VEGF-A165—treated EBs by 5-fold (P = .01; Figure 3H). This increase was only observed at day 15 and had no effect on frequencies of these subsets at day 7 (data not shown). Based on reported coexpression of CD34 and glycophorin A on clonogenic erythroid progenitors40 and of Ep-CAM and c-kit on both CFU-E and erythroblasts26 from human adult bone marrow, our data suggest that VEGF-A165 favored emergence of erythroid precursors coexpressing surface antigens characteristic of early erythroblasts, and these precursors could be sustained by synergistic effects of VEGF-A165 and EPO.
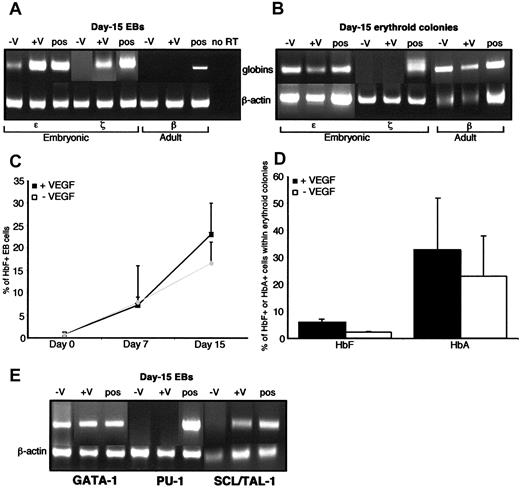
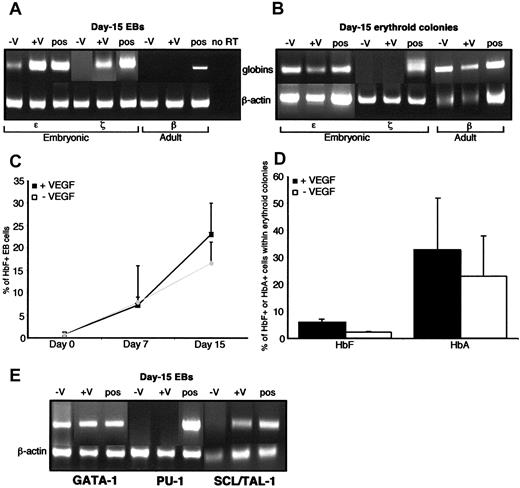
VEGF-A165 enhances the expression of both the embryonic ζ and ϵ globins
Studies on in vitro differentiating mouse ESCs have shown that erythropoietic differentiation within EBs recapitulates the transition from the primitive to the definitive lineages,42,43 as defined by a switch from embryonic (ζ) to adult (β) globin expression, respectively. To further characterize the erythroid subsets emerging from both control and VEGF-A165—treated EBs in the human, we assessed the transcriptional status of the embryonic and adult globin genes. For that purpose, mRNA was extracted from both types of EBs differentiated for different times and from their derived erythroid colonies and used for RT-PCR. A representative analysis of the expression of ϵ, ζ, and β globins (compared with and semiquantitatively normalized to β-actin expression, using equal input template) from EBs differentiated for 15 days is shown in Figure 4A. Both the embryonic ϵ and ζ globins were readily detectable in VEGF-A165—treated EBs whereas only ϵ globin was detected in control EBs at a 2-fold lower level (P = .046; Figure 4A). In VEGF-A165—treated EBs, ϵ globin was detected from at least day 7 (data not shown) and peaked at day 15, whereas in control EBs it was only detected at day 15 (Figure 4A). In contrast to control EBs, devoid of detectable expression of ζ globin throughout their entire period of differentiation, VEGF-A165—treated EBs expressed ζ globin at day 15 (Figure 4A). Both types of EBs were devoid of detectable expression of the adult β globin at days 0, 7 (data not shown), and 15 of differentiation (Figure 4A).
VEGF-A165 enhances the expression of bothζ and ϵ embryonic globins. (A-B) RT-PCR analyses of the embryonic (ϵ and ζ) and adult (β) globins compared in EBs differentiated for 15 days in the presence of cytokines+BMP-4 (-V) or cytokines+BMP-4+VEGF-A165 (+V) (A) and in their derived erythroid colonies aspirated from methylcellulose after 15 days of culture (B). Human fetal head cDNA (pos) was used as a positive control. Because no products were detectable in the absence of the reverse transcriptase (no RT), only one “no RT” reaction is shown in (A). β-actin PCR product signal intensity was used for standardization and relative quantitation. (C-D) Time course of the intracellular expression performed by flow cytometry of the HbF globin in EBs differentiated as indicated (C) and of both HbF and the HbA globins in the derived erythoid colonies (D). Results are expressed as the mean percentages of positive cells, with the corresponding SD (vertical bars) (n = 2 to 4 independent experiments in each condition). (E) RT-PCR analysis of GATA-1, PU-1, and SCL/Tal-1 transcription factors in EBs differentiated as indicated and described above (n = 3 independent experiments for each condition).
VEGF-A165 enhances the expression of bothζ and ϵ embryonic globins. (A-B) RT-PCR analyses of the embryonic (ϵ and ζ) and adult (β) globins compared in EBs differentiated for 15 days in the presence of cytokines+BMP-4 (-V) or cytokines+BMP-4+VEGF-A165 (+V) (A) and in their derived erythroid colonies aspirated from methylcellulose after 15 days of culture (B). Human fetal head cDNA (pos) was used as a positive control. Because no products were detectable in the absence of the reverse transcriptase (no RT), only one “no RT” reaction is shown in (A). β-actin PCR product signal intensity was used for standardization and relative quantitation. (C-D) Time course of the intracellular expression performed by flow cytometry of the HbF globin in EBs differentiated as indicated (C) and of both HbF and the HbA globins in the derived erythoid colonies (D). Results are expressed as the mean percentages of positive cells, with the corresponding SD (vertical bars) (n = 2 to 4 independent experiments in each condition). (E) RT-PCR analysis of GATA-1, PU-1, and SCL/Tal-1 transcription factors in EBs differentiated as indicated and described above (n = 3 independent experiments for each condition).
Using erythroid colonies generated from VEGF-A165—treated EBs, the expression of ζ globin was no longer detectable, whereas the expression of ϵ persisted in colonies derived from VEGF-A165—treated and untreated EBs (Figure 4B). This was associated with the appearance of the adult β globin at both the mRNA (Figure 4B) and protein (HbA) (Figure 4D) levels in colonies derived from both types of EBs. Since the antibody used for HbA staining was specific for the β chain, the expression of the protein (Figure 4D) correlated with that of the transcript (Figure 4B). As shown in Figure 4C, within VEGF-A165—treated or —untreated EBs, the proportion of cells expressing the HbF globin progressively increased at similar levels from no expression, at the onset of EB differentiation, to approximately 20% at day 15. This expression persisted in both types of erythroid colonies albeit at a lower level (2.5-fold) for those derived from VEGF-A165—treated EBs (P = .03; Figure 4D). However, the antibody used for this detection did not allow us to discriminate between the alpha and gamma chains that compose either HbF (α2γ2) or the embryonic Gower 2 (α2ϵ2) and Portland (ζ2γ2) hemoglobins.44 Thus, a different pattern of globin expression was observed between EBs and their derived erythroid colonies, consisting in the presence of embryonic ϵ and ζ globins and the absence of adult β globin in 15-day differentiated EBs followed by the disappearance of ζ globin and the appearance of β globin in 15-day derived erythroid colonies. We suggest that erythroid cells within EBs underwent in vitro globin gene switching toward the adult program during colony formation, potentially owing to development toward adult-like erythroid cells during differentiation in CFU assay conditions.
Since combinatorial control of transcription factors is believed to determine the molecular basis of erythroid lineage progression and globin synthesis,45 we further evaluated the expression of GATA-1, SCL/TAL-1, and PU-146-51 hematopoietic transcription factors in both VEGF-A165—treated and control EBs. The importance of SCL/Tal-1 and GATA-1 in the regulation of erythropoiesis was suggested by null mutations of their genes showing that the lack of SCL/Tal-1 abolished the embryonic erythropoiesis and globin expression52,53 whereas that of GATA-1 resulted in maturation arrest of both primitive and definitive erythroid cells at the proerythroblast stage.47,54-56 PU.1 was used as a negative control since it is not required for development of the erythroid lineage and antagonizes GATA-1—mediated erythroid differentiation.50,51 As shown in Figure 4E, control EBs expressed GATA-1 mRNA but were devoid of detectable expression of SCL/Tal-1 and PU-1 mRNAs whereas VEGF-A165—treated EBs expressed both GATA-1 and SCL/Tal-1 mRNAs. These mRNAs were not detected at both days 0 and 7 of EB differentiation (data not shown). Since SCL/Tal-1 seems to be critically involved in the early period of embryonic hematopoiesis, our combined observations suggest that VEGF-A165 acts on early development events leading toward hESC-derived erythropoiesis.
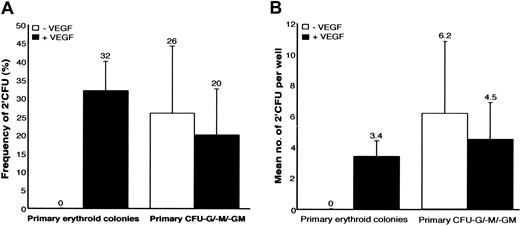
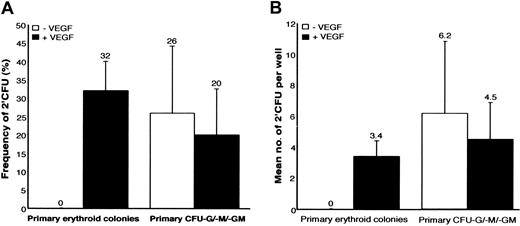
VEGF-A165 specifically promotes the self-renewal potential of human ESC—derived erythroid progenitors
Progenitor self-renewal is functionally defined by the ability of a single clonogenic CFU to retain CFU capacity upon secondary replating. Primary colonies derived from day-15 control and VEGF-A165—treated EBs were individually isolated from the methylcellulose at day 15, dispersed, and replated into secondary CFU assays as previously described.29 The frequency of self-renewal was determined by the number of wells in which 1 primary colony gave rise to at least one secondary colony (2′CFU), while its magnitude was reflected by the absolute number of 2′CFUs generated per individual primary colony. Our results indicated that primary erythroid colonies derived from VEGF-A165—treated EBs were capable of 2′CFU formation (Figure 5). Thirty-two percent of the 128 individual primary erythroid colonies replated from VEGF-A165—treated EBs possessed this capacity (Figure 5A) with each primary colony giving rise to 3.4 2′CFUs (Figure 5B). In contrast, 2′CFUs were never detected from primary erythroid colonies derived from control EBs (Figure 5A-B). Most of the secondary erythroid colonies derived from VEGF-A165—treated EBs were of erythroid origin and were morphologically similar under light microscopy to the primary progenitors (data not shown).
VEGF-A165 specifically promotes self-renewal of EB-derived erythroid progenitors. Individual primary colonies of either erythroid or granulo-monocytic origins derived from EBs differentiated for 15 days with cytokines+BMP-4 (-VEGF) or cytokines+ BMP-4+VEGF-A165 (+VEGF) were aspirated from the methylcellulose at day 15, washed, dispersed, and replated into 2′CFU assays. The frequency of self-renewal capacity and its magnitude are shown in (A) and (B) respectively from both primary erythroid and CFU-GM, CFU-G, and CFU-M colonies (n = 3 experiments for each EB treatment and each type of primary colonies). SDs are represented by vertical bars.
VEGF-A165 specifically promotes self-renewal of EB-derived erythroid progenitors. Individual primary colonies of either erythroid or granulo-monocytic origins derived from EBs differentiated for 15 days with cytokines+BMP-4 (-VEGF) or cytokines+ BMP-4+VEGF-A165 (+VEGF) were aspirated from the methylcellulose at day 15, washed, dispersed, and replated into 2′CFU assays. The frequency of self-renewal capacity and its magnitude are shown in (A) and (B) respectively from both primary erythroid and CFU-GM, CFU-G, and CFU-M colonies (n = 3 experiments for each EB treatment and each type of primary colonies). SDs are represented by vertical bars.
To determine whether only the erythroid lineage derived from VEGF-A165—treated EBs possessed such a renewal capacity, primary CFU-GM, CFU-G, and CFU-M colonies derived from control and VEGF-A165—treated EBs were replated into 2′CFU assays. VEGF-A165 was not capable of influencing the self-renewal potential of primary colonies of granulo-monocytic origin in terms of both frequency (Figure 5A) and magnitude (Figure 5B). The resulting secondary colonies exhibited a characteristic morphology (data not shown). The 2′CFUs of both erythroid and granulo-monocytic origins were analyzed by flow cytometry for expression of erythroid and myeloid markers and displayed similar phenotypic features than the primary colonies. Taken together, these results suggested a selective ability of VEGF-A165 to influence the self-renewal of hESC-derived erythroid progenitors.
Discussion
Evidence has already been provided demonstrating the growth/differentiation in vitro—enhancing effects of VEGF-A165 on the formation of human adult hematopoietic progenitors,7 as well as on the BMP-4—dependent hematopoietic development from mouse ESCs.34 Our report demonstrates that VEGF-A165 selectively supported the erythroid development from human ESCs but not the development of myeloid progenitors. Accordingly, our study differs from previous studies of mouse embryonic hematopoiesis or adult human hematopoiesis. These distinctions could be accounted for by obvious species and ontogenic differences, or potentially from unique culture conditions used during hESC propagation and EB development.
Our study suggests that enhancing the development of erythroid cells from hESCs requires 3 distinct factors: a mesoderm patterning factor (BMP-4), hematopoietic growth and differentiation cytokines (cytokines), and an angiogenic factor (VEGF-A165). Although we have not tested the other isoforms of VEGF-A (121, 145, 189, 206), their biologic properties suggested that they were unlikely to provide a distinct or stronger effect than the 165 isoform. The absence of BMP-4 during EB differentiation with cytokines+VEGF-A165 resulted in a lack of enhancement of erythroid colony formation and thus confirmed previous studies showing the requirement of BMP-4 to induce erythroid cell production and gene expression from mouse ESCs.57-60 According to the previously reported action of BMP-4 and VEGF-A165,34 one possibility is that BMP-4 may increase the expression of the VEGF-A165 receptor KDR, so that further activation by exogenous VEGF-A165 is able to allow a synergistic effect on the erythroid development. In the absence of a dose-response effect for each factor and of a neutralization of their activity with specific antibodies, the sequential order and cellular targets of these factors to orchestrate this complex developmental process remain to be determined.
The presence of EPO markedly increased the number of erythroid colonies generated from VEGF-A165—treated EBs but not from control EBs. The ability of VEGF-A165—treated EBs to respond to EPO in contrast to control EBs might reflect either a different expression of EPO receptor or different regulation mechanism(s) as previously reported for primitive and definitive erythropoiesis.61 However, hematopoietic progenitor CFU potential of human EBs treated with EPO alone, in the presence or absence of VEGF-A165, generated a comparable low number of erythroid colonies, suggesting that VEGF-A165 and/or EPO are not sufficient to promote the erythroid development from hESCs. Based on the observation that VEGF-A165 enhanced the production of CD34+ progeny cells from mouse ESCs,8 we expected to find a higher percentage of CD34+/KDR+ cells within VEGF-A165—treated EBs than within the controls. Although VEGF-A165 exerts most of its pleiotropic effects on endothelial cells through the KDR receptor, we cannot rule out the implication of the VEGFR1/Flt-1 receptor in the pro-erythropoietic activity of VEGF-A165, based on the evidence of heterodimerization and reciprocal activation of both receptors.62,63 Flow cytometry of surface antigens (Ep-CAM, glycophorin A) typifying defined stages of the erythroid maturation26,40,41 identified discrete subsets of erythroid progenitors emerging early and at a higher proportion during EB differentiation in the presence of VEGF-A165. In spite of a possible expression of Ep-CAM antigen on non—hematopoietic cells comprised within EBs such as epithelial cells,26,64 we considered that Ep-CAM-positive cells very likely represented cells of erythroid origin since they were also positive for glycophorin A.
Given the expression of the embryonic ζ and ϵ globins associated with the lack of expression of the adult β globin in VEGF-A165—treated EBs, erythroid precursors developing within human EBs display a molecular signature of primitive erythroid cells.9,21 On the basis of their expression of ϵ globin, the precursors present within control EBs could also be assigned to the primitive lineage. Whether the embryonic, fetal, and adult globins were coexpressed in the same erythroid cells as previously reported in human embryos65 remains to be determined. The presence of EPO in methylcellulose-based CFU assays may induce expression of adult β globin in both types of erythroid colonies, as previously reported.66,67 Prior to our study, the earliest expression of embryonic (ζ,ϵ), fetal (α,γ), and also some adult (β) globins was detected in 5- to 6-week-old human embryos24,25 where both primitive and definitive erythroblasts expressed ϵ, γ, and α whereas ζ was expressed at 5 weeks only in primitive cells followed by β globin at 6 weeks.25 Accordingly, our report provides an alternative model to examine the pattern of globin expression during the earliest steps of human erythropoietic development.
In addition to the ability of VEGF-A165 to enhance the number of primary erythroid progenitors, those progenitors appeared to possess a greater self-renewal capacity than those derived from control EBs. In contrast, progenitors of granulo-monocytic origin derived in the same conditions possessed an equivalent self-renewal potential whether EBs were treated with or without VEGF-A165. Since erythroid progenitors arising from VEGF-A165—treated EBs did not continue to receive VEGF-A165 signals after EB differentiation, they were able to show self-renewal properties subsequent to the VEGF-A165 signaling. However, we did not determine if VEGF-A165, which on its own gave rise to a small number of primary erythroid colonies, was also directly responsible for the activation of progenitor self-renewal programs or whether this effect was dependent on BMP-4 signaling, based on previous observations in our group29 and of sequential action of BMP-4 and VEGF-A165 signals.34 Although the major goal of many hematopoietic groups working with hESC is to successfully design transplantation assays to detect repopulating cells from hESCs in immunode-ficient recipients, the considerable difficulties encountered in detection of analogous cells types from mESCs have limited our efforts to characterize the VEGF-induced self-renewal properties of the progenitors only.68
Using this model, additional studies will assist in delineating the functional relations between VEGF-A165, BMP-4, and the hematopoietic cytokines required to promote the erythroid development from hESCs. Nevertheless, our report suggests that VEGF-A165 is a potentially important signal that selectively promotes the erythroid development and self-renewal during in vitro differentiation of hESCs. Considering the absence of evidence in the literature concerning factors that are capable of specifically regulating the development of a particular cell type from hESCs as well as the body of evidence of the “pleiotropic” effects of VEGF-A165 on hematopoiesis, our study provides a unique opportunity to further characterize the molecular commitment steps involved in the establishment of embryonic erythropoiesis in the human.
Prepublished online as Blood First Edition Paper, December 4, 2003; DOI 10.1182/blood-2003-07-2563.
Supported in part by a grant from Geron Corporation, CA; Menlo Park; The Krembil Foundation; and the Multiple Organ Transplant Initiative, London Health Sciences Centre; a Canadian Research Chair in Stem Cell Biology and Regenerative Medicine and Krembil Chair in Stem Cell Biology to M.B. and a visiting fellowship to C.C. from INSERM.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We would like to thank Farbod Shojaei and Michele Souyri for their insights toward completion of this work.

![Figure 2. VEGF-A165 requires the presence of additional factors to optimally promote erythroid colony formation. EBs were differentiated for 15 days with the indicated treatments and plated in CFU assays as described in Figure 1. (A-B) Mean numbers of erythroid colonies derived from EBs differentiated with the indicated treatments, with the corresponding SD (vertical bars) (n = 3 independent experiments for each EB treatment except for cytokines+BMP-4+VEGF-A165 with n = 6). Inset represents data from similar experiments in which IL-6 or SCF was removed from the cocktail of cytokines (n = 4 with [+] or without [-] IL-6, n = 2 with [+] or without [-] SCF). In panel B, EB differentiatiation was conducted in the presence (+) or absence (-) of EPO added at the initiation of differentiation (n = 3 independent experiments). (C) Morphology under light microscopy of erythroid colonies derived from EBs differentiated with the indicated treatments. Scale bar, 100μm. (D) A representative Giemsa staining performed on 20-day pooled erythroid colonies generated from both VEGF-A165—treated (+VEGF) and control EBs (-VEGF) (n = 2 for each EB treatment). Rare contaminating macrophages are also present. Scale bar, 100 μm.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/103/7/10.1182_blood-2003-07-2563/6/m_zh80070458870002.jpeg?Expires=1768084040&Signature=PZCpPGCkwiE~8tjjFxWhMhxhQs7SHVrFPdZbznmZps2kSZh2K7ViMqrzJqmj-RaW7zRi8hKlnyjzGUEKQM~2ni2cw4y7~zks8oeq2sfb2-52SPR7EhobrRXKRy2LHQtadOsYF2rjI0T1g1PO7hV6ekokf7X96I4Hlq1YiduQAVZ-1PdC6-vjkAamsWhW2TSjtLoXWzNtlwvZO2MCPrwEuZOinOcUtj6n2aZT-tIJEhvtsTVT4P5zHrjudcgyTjuO1rPIQ2ilPI4DUIyGF4DUM6HfskhXchDNXl5G8VsNh1lC-0RLv5JEZ1VA31wroocDvh0BF9UaDo77XNftxdeZjg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)

![Figure 2. VEGF-A165 requires the presence of additional factors to optimally promote erythroid colony formation. EBs were differentiated for 15 days with the indicated treatments and plated in CFU assays as described in Figure 1. (A-B) Mean numbers of erythroid colonies derived from EBs differentiated with the indicated treatments, with the corresponding SD (vertical bars) (n = 3 independent experiments for each EB treatment except for cytokines+BMP-4+VEGF-A165 with n = 6). Inset represents data from similar experiments in which IL-6 or SCF was removed from the cocktail of cytokines (n = 4 with [+] or without [-] IL-6, n = 2 with [+] or without [-] SCF). In panel B, EB differentiatiation was conducted in the presence (+) or absence (-) of EPO added at the initiation of differentiation (n = 3 independent experiments). (C) Morphology under light microscopy of erythroid colonies derived from EBs differentiated with the indicated treatments. Scale bar, 100μm. (D) A representative Giemsa staining performed on 20-day pooled erythroid colonies generated from both VEGF-A165—treated (+VEGF) and control EBs (-VEGF) (n = 2 for each EB treatment). Rare contaminating macrophages are also present. Scale bar, 100 μm.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/103/7/10.1182_blood-2003-07-2563/6/m_zh80070458870002.jpeg?Expires=1768084041&Signature=TvOnw~vbPH2m4mBcacUqu8x~EWFeKpE18SfKUbRTVXOiN9CDb5XJnDq1hXUBmkDaqjO0yrr7kTUprgrZ3a0e6ARaEiF5y~lx3pzn~SkRccSAgjhGlMvBznyipoFsuTlz1cJiELLHCo4hy8IOXNc-eHe7jIt58jQsoGg6PCemYjJF6NMGSE5ISRUKDKkfrhKOndLWZoWj6WButi2T57RdERE8uJdmPURxzmS6~g1ZHoQDKiEKA-59Mw06APMSo0xMQAv3HH18AROGWajfVojUKLPu9-35ATgaEH5ANmy5VQmKq-f12XMbfqBXkrIwfIa7Z~aBX1URk3NVdp50Q5vA6w__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)