Abstract
Dendritic cells (DCs) are the most potent of the antigen-presenting cells (APCs). Preparation of sufficient numbers of mature DCs, however, is both costly and time-consuming. We have examined here the possibility of using an alternative source of APCs that would be easier to obtain, would not require extensive culture, and thus would be more applicable to human immunotherapy protocols. We show here that freshly isolated human B cells can be efficiently infected by a replication-defective fowlpox recombinant vector, designated rF-TRICOM (TRIad of COstimulatory Molecules), to markedly increase surface expression of the human costimulatory molecule B7-1 and moderately increase expression of intercellular adhesion molecule-1 (ICAM-1) and leukocyte function-associated antigen-3 (LFA-3). Peptide-pulsed rF-TRICOM–infected B cells were highly efficient in activating antigen-specific human T cells and shown to be superior to the use of CD40L in enhancing APC potency. Moreover, when infection of freshly isolated B cells with rF-TRICOM was combined with CD40L, a still further marked enhancement of the antigen-presenting potency was observed. Ex vivo–generated antigen-specific T cells activated in this manner might be applied to experimental protocols or used for adoptive transfer in immunotherapy protocols.
Introduction
Effective antigen presentation by professional antigen-presenting cells (APCs) is required for effective activation of both CD4+ and CD8+ cells. Dendritic cells (DCs) are the most potent of the professional APCs (which include DCs, activated macrophages, and activated B cells), partly because of their higher levels of expression of costimulatory, adhesion, and major histocompatibility complex (MHC) molecules, as compared with other professional APCs,1-4 and also because DCs are highly efficient in migration, antigen capture, and antigen processing.5
Resting B cells, on the other hand, express little or no costimulatory molecules and have been demonstrated to be inefficient for in vitro presentation of antigens to T cells.6,7 Various activation signals that include contact with the antigen via Ag receptor, CD40 ligation, and lipopolysaccharide (LPS), among others, originate an increase in the levels of expression of costimulatory and adhesion molecules on the surface of B cells; thus, activated B cells become professional APCs for antigen presentation in vitro as well as in vivo.4,8
Because DCs are highly efficient at APC function, numerous experimental and clinical studies are employing DCs as immunogens.9 Generation of DCs from human peripheral blood has been achieved using whole peripheral blood mononuclear cells (PBMCs) obtained by leukapheresis or a CD34+-enriched fraction obtained from PBMCs. Because DCs constitute only 0.1% to 0.5% of PBMCs and their generation involves 6 to 7 days of in vitro culture in the presence of exogenous granulocyte-macrophage colony-stimulating factor (GM-CSF), interleukin-4 (IL-4), and other cytokines and reagents such as Flt-3L (some of which are often costly or difficult to obtain),10,11 preparation of sufficient numbers of highly enriched mature DCs is both costly and time-consuming. Given these limitations, we have examined the possibility of using alternative sources of APCs that might be easier to obtain, would not require extensive culture, and thus might be more applicable to human immunotherapy protocols. B cells constitute 10% to 15% of PBMCs. If one could efficiently infect B cells and induce expression of multiple T-cell costimulatory molecules in 4 to 6 hours and then re-infuse B cells without extensive culture or use of cytokines, they may constitute an alternative source to the use of DCs, which require in vitro cultivation and the use of cytokines.
Numerous costimulatory molecules have been demonstrated to be able to provide the second signal critical for the T-cell activation process,12,13 such as B7-1, intercellular adhesion molecule-1 (ICAM-1), and leukocyte function-associated antigen-3 (LFA-3). In previous reports we have demonstrated the ability of recombinant poxvirus vectors encoding B7-1, ICAM-1, and LFA-3 to efficiently infect and promote the hyperexpression of these costimulatory molecules in human DCs.14,15 An avipox (fowlpox, rF-) vector encoding B7-1, ICAM-1, and LFA-3, designated rFTRICOM (TRIad of COstimulatory Molecules), was used to infect human DCs prepared from PBMCs. When rF-TRICOM–infected DCs were used for in vitro antigen presentation of specific peptides to various antigen-specific T cells, a pronounced enhancement of T-cell activation was demonstrated, as compared with the activation observed when uninfected DCs were used as APCs.15
The studies reported here were designed to investigate a potential use of rF-TRICOM–infected human B cells (isolated from PBMCs) as an alternative source of APCs. We show here that human B cells could be efficiently infected by rF-TRICOM. Peptide-pulsed rF-TRICOM–infected B cells were more efficient than peptide-pulsed uninfected B cells to stimulate antigen-specific human T cells in vitro. The ability of rF-TRICOM–infected B cells to function as APCs approached that of DCs. In this study we have also compared the ability of CD40L-activated B cells with that of rF-TRICOM–infected B cells to stimulate antigen-specific T cells. Our results demonstrated that infection of B cells with rF-TRICOM is superior to activation of B cells (24 hours) with CD40L in terms of enhancing their APC potency. Moreover, when infection with rF-TRICOM was combined with activation of the B cells in the presence of CD40L, the result was a marked enhancement of the antigen-presentation potency of the B cells, as compared with that of B cells that were either infected with rF-TRICOM or activated with CD40L alone.
Thus, our results suggested that freshly isolated B cells infected with rF-TRICOM and simultaneously activated in the presence of CD40L could be used as highly efficient APCs to mediate activation of antigen-specific T cells. Ex vivo–generated antigen-specific T cells might be applied to experimental protocols or used for adoptive transfer in immunotherapy protocols.
Materials and methods
Cell cultures
The V8T-cell line is a CD8+ cytotoxic T-lymphocyte (CTL) line directed against the carcinoembryonic antigen peptide 1 (CAP-1) epitope of carcinoembryonic antigen (CEA).16,17 The T-1191 cell line is a CD8+ mucin 1 (MUC-1)–specific CTL line generated from PBMCs from a healthy donor that were in vitro stimulated using a MUC-1 peptide (native epitope).18 Both V8T and T-1191 cell lines were cultured as described previously.16
Peptides
The following HLA-A2 binding peptides were used in this study: (1) the CEA peptide CAP-116 ; (2) the CAP-1 agonist peptide designated CAP1-6D19 ; (3) a MUC-1 peptide18 ; (4) influenza matrix protein peptide 58-66, designated Flu peptide20 ; (5) human papillomavirus (HPV) type 16 E7 peptide 11-2021 ; (6) HIV Pol peptide 408-416 (ILKEPVHGV); and (7) a prostate-specific antigen (PSA) agonist peptide designated PSA-3A.22 All peptides were more than 96% pure and manufactured by American Peptide Company (Sunnyvale, CA).
Isolation of B cells and CD8+ T cells and generation of DCs from PBMCs
PBMCs were obtained from heparinized blood from healthy donors using lymphocyte separation medium gradient (Organon Teknika, Durham, NC); selected donors were HLA-A2 positive. B cells were isolated using anti–CD19 conjugated magnetic beads (Miltenyi Biotec, Auburn, CA); purity of the isolated cell population was assessed by flow cytometry. DCs were prepared from PBMCs as previously described15 ; adherent cells were cultured for 6 to 7 days in AIM-V medium (Invitrogen, Carlsbad, CA) containing 100 ng/mL of recombinant human GM-CSF (rhGM-CSF) and 20 ng/mL of recombinant human IL-4 (rhIL-4) (PeproTech, Rocky Hill, NJ). CD8+ T cells were negatively isolated from PBMCs using a CD8 isolation kit (Miltenyi Biotec).
Recombinant avipox viruses
The recombinant avipox (fowlpox) virus rF-TRICOM contains the genes for the human costimulatory molecules B7-1, ICAM-1, and LFA-3, and it was constructed as previously described.23-25 The recombinant fowlpox virus rF-CEA(6D)/TRICOM contains the entire open reading frame of human CEA, carrying a punctual amino acid change that corresponds to the position number 6 in the CAP-1 peptide sequence; it also contains the genes for the human costimulatory molecules LFA-3, ICAM-1, and B7-1.23-26 rF-CEA(6D) is a recombinant fowlpox virus that contains the modified CEA gene.
The recombinant fowlpox virus rF-MUC-1/TRICOM is a recombinant fowlpox virus that contains the MUC-1 gene and the human LFA-3, ICAM-1, and B7-1 genes; the rF-MUC-1 fowlpox vector contains only the MUC-1 sequence.18
The rF-PSA(3A)/TRICOM is a recombinant fowlpox virus that contains the PSA gene with a modified PSA-3 peptide (PSA-3A) sequence22 and the 3 human costimulatory molecules. Fowlpox virus wild type (FP-WT) was used as a control vector.
Infection of B cells with recombinant avipox virus and activation with CD40L
B cells (1 × 106) were incubated in 0.5 mL of Opti-MEM medium (Invitrogen) with the corresponding recombinant fowlpox virus for 2 hours at 37° C at a multiplicity of infection (MOI) of 40. The infected cells were then suspended in 2 mL of complete medium and cultured for 24 hours prior to being used as APCs.
B cells were activated in the presence of CD40L by incubation in complete medium containing 1 μg/mL of soluble noncovalent trimeric CD40L (PeproTech) for 24 hours at 37° C. When CD40L activation and infection with rF-TRICOM were combined, B cells were infected as described above and subsequently suspended in 2 mL of complete medium containing 1 μg/mL of CD40L. Cultures were kept at 37° C for 24 hours prior to being used as APCs.
Generation of PSA-specific T-cell lines
PSA-3A peptide-pulsed (25 μg/mL) rF-TRICOM–infected B cells, B cells infected with rF-TRICOM and simultaneously activated in the presence of CD40L, and uninfected DCs were used as APCs for the generation of PSA-specific T-cell lines. In addition, B cells infected with rF-PSA(3A)/TRICOM without exogenous peptide were also used as APCs. In all cases, nonadherent cells isolated from PBMCs were used as a source of effector cells; the APC/effector cell ratio was 1:10. Cultures were incubated for 3 days at 37° C and then supplemented with recombinant human IL-2 at a concentration of 20 U/mL for 7 days. The 10-day culture constituted one in vitro stimulation (IVS) cycle. Primary cultures were restimulated with the autologous APCs (each corresponding treatment) on day 11 to begin the next IVS cycle. Irradiated (220 Gy) autologous Epstein-Barr virus (EBV)–transformed B cells pulsed with 25 μg/mL of PSA-3A peptide were used as APCs after the third IVS cycle, at an APC/effector cell ratio of 2:1.
Results
Infection of human B cells with rF-TRICOM
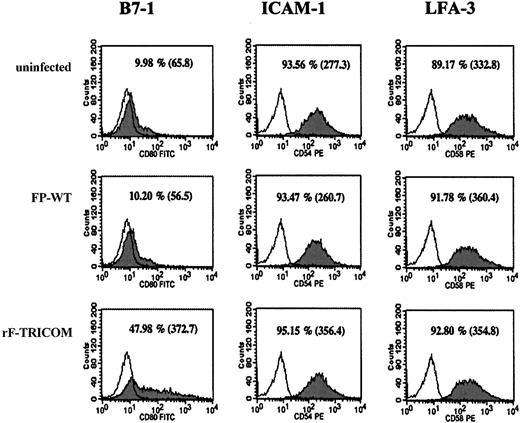
Phenotypic analyses were conducted to determine whether infection of human B cells with the rF-TRICOM vector would result in the surface expression of the encoded transgenes. B cells were isolated from PBMCs from healthy donors as described in “Materials and methods.” The purity of the isolated B-cell population was analyzed by flow cytometry. The isolated cells were 98% positive for CD20, 99% positive for class I and class II, 91% positive for CD40, and negative (< 2%) for CD3, CD14, and CD56. Figure 1 shows that the percentage of B cells expressing B7-1 and the surface expression levels of this marker (as indicated by the mean fluorescence intensity [MFI]) were markedly increased after infection with rF-TRICOM. On the other hand, surface expression levels of ICAM-1 and LFA-3 were high in uninfected B cells. While the percentage of B cells expressing ICAM-1 and the MFI for this marker were moderately increased after infection with rF-TRICOM, a minimal augment in LFA-3 levels of expression (MFI) but not in the percentage of positive cells was repeatedly observed from various donors after rF-TRICOM infection. Infection with a control vector (FP-WT) did not alter the expression of any of the phenotypic markers analyzed.
Phenotypic analysis of B cells infected with rF-TRICOM. B cells were infected as described in “Materials and methods.” After 24 hours of culture, B cells were stained with either fluorescein isothiocyanate (FITC)–conjugated antibody (Ab) directed against CD80, or phycoerythrin (PE)–conjugated Ab directed against CD54 and CD58 (shaded histograms). Isotype controls were anti-immunoglobulin (Ig)G1 and anti-IgG2 conjugated to FITC and PE, respectively (open histograms). Analysis was conducted using a FACScan and CellQuest software (BD Biosciences, San Jose, CA). Numbers indicate the percentage of positive cells for each marker; numbers in parentheses indicate MFI (mean fluorescence intensity).
Phenotypic analysis of B cells infected with rF-TRICOM. B cells were infected as described in “Materials and methods.” After 24 hours of culture, B cells were stained with either fluorescein isothiocyanate (FITC)–conjugated antibody (Ab) directed against CD80, or phycoerythrin (PE)–conjugated Ab directed against CD54 and CD58 (shaded histograms). Isotype controls were anti-immunoglobulin (Ig)G1 and anti-IgG2 conjugated to FITC and PE, respectively (open histograms). Analysis was conducted using a FACScan and CellQuest software (BD Biosciences, San Jose, CA). Numbers indicate the percentage of positive cells for each marker; numbers in parentheses indicate MFI (mean fluorescence intensity).
Infection of B cells with rF-TRICOM at different MOIs also was conducted. The results demonstrated that an MOI of 40 was able to induce optimal expression of B7-1, ICAM-1, and LFA-3, in both the percentage of positive B cells and the MFI (data not shown). We also have performed time course studies on the surface expression of the encoded transgenes after infection of B cells with the recombinant fowlpox-TRICOM vectors. It was observed in those studies that the increase in surface expression of the encoded molecules reaches a plateau between 4 and 6 hours of infection with the recombinant fowlpox-TRICOM vectors. Levels of expression of additional markers were also analyzed by fluorescence-activated cell sorting (FACS); uninfected B cells (> 98%) expressed high levels of class I and class II MHC molecules as well as CD40 (> 95%) and B7-2 (> 70%). None of these markers had changed after infection with rF-TRICOM (data not shown).
rF-TRICOM–infected human B cells induce higher Flu- and HPV-specific T-cell responses
In order to determine whether rF-TRICOM–infected human B cells were efficient APCs that could enhance the activation of antigen-specific T cells, as compared with uninfected B cells, we have measured interferon-γ (IFN-γ) production by Flu-specific T cells following stimulation with Flu peptide-pulsed uninfected versus rF-TRICOM–infected B cells. We also have compared the ability of rF-TRICOM–infected human B cells for presenting antigens to the T cells with that of human DCs (generated from PBMCs of the same donor by culturing for 7 days in the presence of GM-CSF and IL-4).
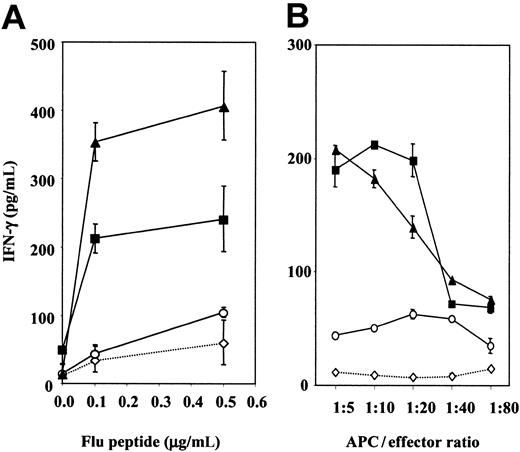
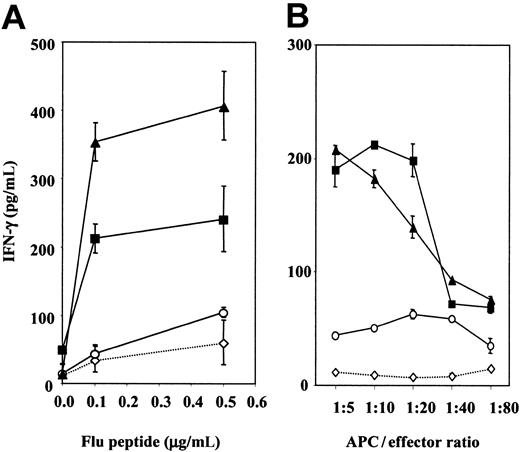
As shown in Figure 2A, a 4- to 7-fold increase and a 6- to 10-fold increase in IFN-γ production were observed when Flu-specific T cells were stimulated with various concentrations of Flu peptide-pulsed rF-TRICOM–infected B cells and DCs, respectively, as compared with FP-WT–infected B cells or uninfected B cells. Figure 2B shows the results from additional studies conducted with a different donor at various APC/effector cell ratios. Approximately 10-fold fewer rF-TRICOM–infected B cells were required to activate Flu-specific T cells to the levels of activation reached when FP-WT–infected or uninfected B cells were used as APCs. Similar results were obtained using DCs as APCs. In addition, a 15-fold increase in the production of IL-2 was observed when Flu-specific T cells were stimulated in the presence of autologous Flu peptide-pulsed rF-TRICOM–infected B cells, as compared with Flu peptide-pulsed uninfected B cells. There was little, if any, increase in the Th2 cytokines IL-10 and IL-4 as a result of the use of rF-TRICOM–infected B cells as APCs (data not shown).
Production of IFN-γ by CD8+ T cells isolated from PBMCs from healthy donors after stimulation with Flu peptide-pulsed autologous B cells and DCs. CD8+ T cells (1 × 106/mL) were stimulated with irradiated (30 Gy) autologous uninfected B cells (⋄), B cells infected with control vector FP-WT (○), B cells infected with rF-TRICOM (▪), or uninfected DCs from the same donor (▴). (A) Analysis at various Flu peptide concentrations at an APC/effector cell ratio of 1:10. (B) Analysis of rF-TRICOM–infected B cells versus DCs from a different donor at various APC/effector cell ratios when Flu peptide concentration was 0.5 μg/mL. Supernatants were collected and screened for IFN-γ after 24 hours of stimulation. Error bars represent SD of multiple determinations.
Production of IFN-γ by CD8+ T cells isolated from PBMCs from healthy donors after stimulation with Flu peptide-pulsed autologous B cells and DCs. CD8+ T cells (1 × 106/mL) were stimulated with irradiated (30 Gy) autologous uninfected B cells (⋄), B cells infected with control vector FP-WT (○), B cells infected with rF-TRICOM (▪), or uninfected DCs from the same donor (▴). (A) Analysis at various Flu peptide concentrations at an APC/effector cell ratio of 1:10. (B) Analysis of rF-TRICOM–infected B cells versus DCs from a different donor at various APC/effector cell ratios when Flu peptide concentration was 0.5 μg/mL. Supernatants were collected and screened for IFN-γ after 24 hours of stimulation. Error bars represent SD of multiple determinations.
Thus, our results demonstrated that rF-TRICOM–infected human B cells could function as efficient APCs to present antigens to antigen-specific T cells.
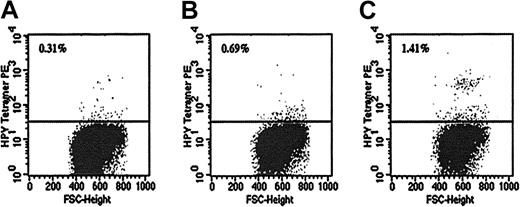
MHC/peptide tetramer analysis was then carried out to assess the expansion of HPV peptide-specific CD8+ T cells after in vitro stimulation with HPV peptide-pulsed uninfected, FP-WT–infected, or rF-TRICOM–infected autologous B cells. As shown in Figure 3, after 10 days of stimulation, 1.41% of the CD8+ T cells stained with the specific HPV-tetramer when rF-TRICOM–infected B cells were used as APCs. When stimulation was done in the presence of peptide-pulsed FP-WT–infected B cells or uninfected B cells, 0.69% and 0.31% of the CD8+ T cells, respectively, stained with the HPV tetramer. FACS data were acquired from 200 000 cells. The percentage of HPV tetramer-positive T cells observed using as APC peptide-pulsed rF-TRICOM–infected B cells, as compared with peptide-pulsed uninfected B cells or peptide-pulsed B cells infected with FP-WT, was statistically significant as determined using the Kolmogorov-Smirnov (K-S) 2-sample test (P ≤ .001).27 Since tetramer staining was conducted after 10 days of in vitro stimulation, it is probable that the observed results were due to proliferation of HPV-specific memory T cells rather than the in vitro priming of naive T cells, to generate HPV-specific T cells.
Binding of HPV tetramer to different CD8+ T cells isolated from PBMCs after in vitro stimulation with an HPV peptide. CD8+ T cells were isolated from PBMCs after 10 days of in vitro stimulation with autologous HPV-pulsed uninfected B cells (A); HPV-pulsed B cells infected with FP-WT (B); or HPV-pulsed B cells infected with rF-TRICOM (C). 1 × 106 CD8+ T cells were stained with PE-labeled HPV MHC-tetramer and subsequently analyzed by FACS. A total of 2 × 105 cells were acquired for each tube.
Binding of HPV tetramer to different CD8+ T cells isolated from PBMCs after in vitro stimulation with an HPV peptide. CD8+ T cells were isolated from PBMCs after 10 days of in vitro stimulation with autologous HPV-pulsed uninfected B cells (A); HPV-pulsed B cells infected with FP-WT (B); or HPV-pulsed B cells infected with rF-TRICOM (C). 1 × 106 CD8+ T cells were stained with PE-labeled HPV MHC-tetramer and subsequently analyzed by FACS. A total of 2 × 105 cells were acquired for each tube.
rF-CEA(6D)/TRICOM– and rF-MUC-1/TRICOM–infected B cells to stimulate CEA– and MUC-1–specific T cells, respectively
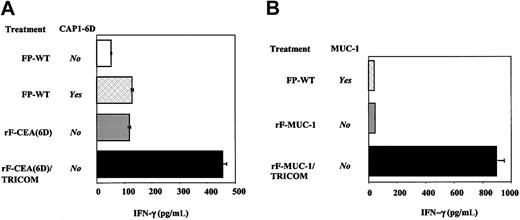
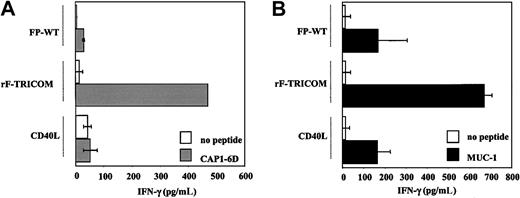
The ability of the recombinant avipox vectors rF-CEA(6D)/TRICOM and rF-MUC-1/TRICOM to deliver both signal 1 and a costimulatory signal (signal 2) to CEA-specific and MUC-1–specific T cells, respectively, has been investigated. A CEA-specific CTL line (V8T) was in vitro stimulated with allogeneic B cells isolated from PBMCs of a healthy donor that were infected with the control vector (FP-WT), the rF-CEA(6D) vector, and the rF-CEA(6D)/TRICOM vector. Stimulation was made in the absence of exogenous peptide to study the ability of these vectors to deliver the signal 1 to the T cells. As positive control for the stimulation experiments, FP-WT–infected B cells were exogenously pulsed with 25 μg/mL of the CEA peptide CAP1-6D. As shown in Figure 4A, stimulation of the V8T cells with rF-CEA(6D)–infected B cells in the absence of exogenous peptide (where the signal 1 was delivered to the B cells through the vector) increased the production of IFN-γ up to the levels obtained when peptide-pulsed FP-WT–infected B cells were used as APCs. The activation of the V8T cells was markedly enhanced when B cells infected with rF-CEA(6D)/TRICOM (in which both signal 1 and signal 2 were delivered through the vector) were used as APCs; an increase of almost 10-fold was observed in the levels of IFN-γ produced, as compared with those observed when T cells were stimulated with FP-WT–infected B cells without peptide.
Production of IFN-γ by antigen-specific T-cell lines stimulated with allogeneic B cells isolated from PBMCs. (A) CEA-specific V8T cells (0.5 × 106/mL) were stimulated with irradiated allogeneic B cells isolated from PBMCs that were infected with the recombinant fowlpox vectors rF-CEA(6D) or rF-CEA(6D)/TRICOM. As control, B cells were infected with FP-WT. Where indicated, the APCs were pulsed with 25 μg/mL of CAP1-6D peptide. Supernatants were collected after 24 hours of stimulation. (B) MUC-1–specific T cells (0.5 × 106/mL) were stimulated with irradiated allogeneic B cells that were infected with the recombinant fowlpox vectors rF-MUC-1 or rF-MUC-1/TRICOM. As control, B cells were infected with FP-WT. Where indicated, APCs were pulsed with 50 μg/mL of MUC-1 peptide. Supernatants were collected after 48 hours of stimulation. Error bars represent SD of multiple determinations.
Production of IFN-γ by antigen-specific T-cell lines stimulated with allogeneic B cells isolated from PBMCs. (A) CEA-specific V8T cells (0.5 × 106/mL) were stimulated with irradiated allogeneic B cells isolated from PBMCs that were infected with the recombinant fowlpox vectors rF-CEA(6D) or rF-CEA(6D)/TRICOM. As control, B cells were infected with FP-WT. Where indicated, the APCs were pulsed with 25 μg/mL of CAP1-6D peptide. Supernatants were collected after 24 hours of stimulation. (B) MUC-1–specific T cells (0.5 × 106/mL) were stimulated with irradiated allogeneic B cells that were infected with the recombinant fowlpox vectors rF-MUC-1 or rF-MUC-1/TRICOM. As control, B cells were infected with FP-WT. Where indicated, APCs were pulsed with 50 μg/mL of MUC-1 peptide. Supernatants were collected after 48 hours of stimulation. Error bars represent SD of multiple determinations.
Similar experiments were performed using a MUC-1–specific CTL line (T-1191). Allogeneic B cells that were infected with FP-WT vector, rF-MUC-1 vector, or rF-MUC-1/TRICOM vector were used as APCs. The levels of activation of the MUC-1–specific T cells observed when only signal 1 was delivered via vector (rF-MUC-1–infected B cells used as APCs) or when the signal 1 was mediated by the peptide exogenously provided to the B cells (FP-WT–infected B cells pulsed with MUC-1 peptide) were similar (Figure 4B). A remarkable enhancement (about 20-fold) of IFN-γ production was noticed when rF-MUC-1/TRICOM–infected B cells were used as APCs (where the vector delivered both the signal 1 and the signal 2), as compared with FP-WT–infected B cells.
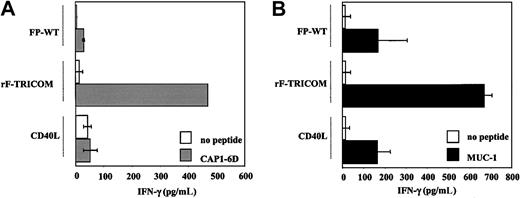
Comparison of the ability of rF-TRICOM–infected B cells versus CD40L-activated B cells for antigen presentation to T cells
Although resting B cells are not able to efficiently present antigens to T cells, activated B cells are considered to be professional APCs. It has been demonstrated previously that CD40L-activated B cells could mediate stimulation of antigen-specific T cells.28,29 In the present study we have compared the antigen-presenting ability of rF-TRICOM–infected B cells versus B cells activated for only 24 hours in the presence of soluble CD40L. Phenotypic studies were first conducted to define changes in the expression of B7-1, ICAM-1, and LFA-3 on the B-cell surface after infection with rF-TRICOM or 24 hours of activation with CD40L. While rF-TRICOM infection resulted in a marked increase in B7-1 surface expression and lower increments in ICAM-1 and LFA-3 expression, B cells incubated for 24 hours in the presence of CD40L showed a slight increment in B7-1 expression but a profound increase in ICAM-1 and LFA-3 expression (data not shown). Figure 5A shows that the CD40L-activated B cells were able to promote only a 2-fold increase in IFN-γ production by CEA-specific T cells as compared with FP-WT–infected B cells, while the use of rF-TRICOM–infected B cells resulted in a 5-fold increase in the levels of IFN-γ released. The same results were achieved using MUC-1–specific T cells. As shown in Figure 5B, only rF-TRICOM–infected B cells were able to increase the levels of IFN-γ secreted by the MUC-1–specific T cells in 4-fold over the levels secreted by the T cells stimulated with FP-WT–infected B cells. Little or no increase in antigen-presenting ability was observed when CD40L-activated B cells were used as APCs (Figure 5B).
rF-TRICOM–infected B cells versus CD40L-activated B cells to stimulate IFN-γ production by antigen-specific T-cell lines. (A) CEA-specific V8T cells (0.5 × 106/mL) were stimulated with irradiated allogeneic B cells isolated from PBMCs that were infected with rF-TRICOM or activated for 24 hours in the presence of 1 μg/mL of CD40L. As control, B cells also were infected with FP-WT. For each condition, APCs were pulsed with 25 μg/mL of CAP1-6D peptide or without peptide. Supernatants were collected after 24 hours of stimulation. (B) MUC-1–specific T cells (0.5 × 106/mL) were stimulated with irradiated allogeneic B cells isolated from PBMCs that were infected with rF-TRICOM or activated for 24 hours in the presence of 1 μg/mL of CD40L. As control, B cells were infected with FP-WT. For each condition, APCs were pulsed with 50 μg/mL of MUC-1 peptide or without peptide. Supernatants were collected after 48 hours of stimulation. Error bars represent SD of multiple determinations.
rF-TRICOM–infected B cells versus CD40L-activated B cells to stimulate IFN-γ production by antigen-specific T-cell lines. (A) CEA-specific V8T cells (0.5 × 106/mL) were stimulated with irradiated allogeneic B cells isolated from PBMCs that were infected with rF-TRICOM or activated for 24 hours in the presence of 1 μg/mL of CD40L. As control, B cells also were infected with FP-WT. For each condition, APCs were pulsed with 25 μg/mL of CAP1-6D peptide or without peptide. Supernatants were collected after 24 hours of stimulation. (B) MUC-1–specific T cells (0.5 × 106/mL) were stimulated with irradiated allogeneic B cells isolated from PBMCs that were infected with rF-TRICOM or activated for 24 hours in the presence of 1 μg/mL of CD40L. As control, B cells were infected with FP-WT. For each condition, APCs were pulsed with 50 μg/mL of MUC-1 peptide or without peptide. Supernatants were collected after 48 hours of stimulation. Error bars represent SD of multiple determinations.
Infection with rF-TRICOM and activation with CD40L have additive effect on the antigen-presenting ability of B cells
Because ICAM-1 and LFA-3 expression are markedly augmented on the surface of CD40L-activated B cells and, on the other hand, expression of B7-1 is highly increased in B cells after infection with rF-TRICOM, we sought to investigate the combined effect of infection with rF-TRICOM and activation with CD40L on the ability of B cells isolated from PBMCs to efficiently present antigens to the T cells.
Results in Table 1 show that treatment of rF-TRICOM–infected B cells with CD40L led to higher expression of B7-1, ICAM-1, and LFA-3 in both the percentage of positive cells and the MFI, as compared with those observed after either rF-TRICOM infection or CD40L activation alone. Table 1 (right columns) also shows that either uninfected or FP-WT–infected B cells were unable to stimulate Flu-specific T cells to produce IFN-γ. When activation was conducted in the presence of CD40L-activated B cells or rF-TRICOM–infected B cells, Flu-specific T cells secreted 19.7 and 30.5 pg/mL of IFN-γ, respectively. The maximum activation occurred in the presence of Flu peptide-pulsed B cells that received the 2 treatments (infection with rF-TRICOM and activation with CD40L, as described in “Materials and methods”); 59.7 pg/mL of IFN-γ were detected in the supernatants of that culture. Similar experiments conducted with HIV peptide-pulsed B cells resulted in no production of IFN-γ, thus demonstrating that the observed responses were indeed antigen specific.
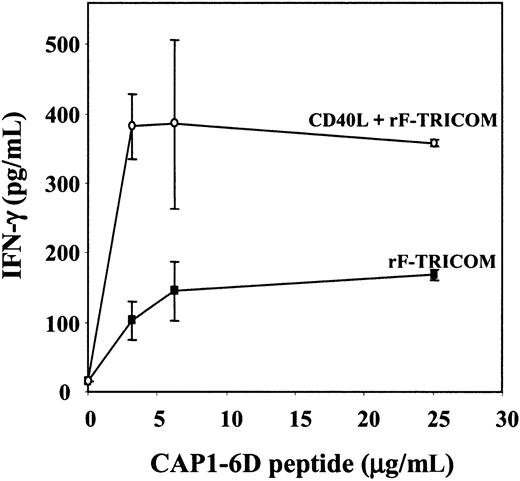
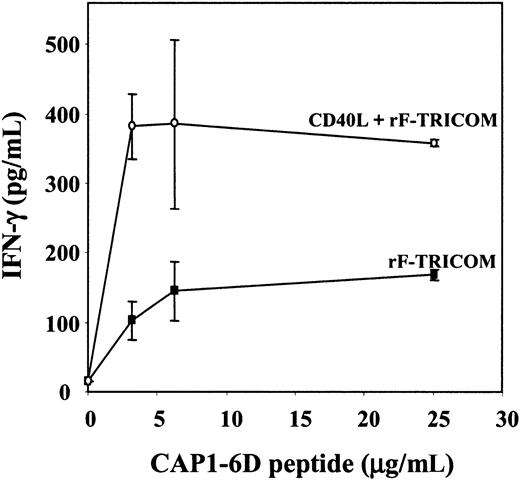
Results were then confirmed using the CEA-specific V8T-cell line that was stimulated in the presence of allogeneic B cells (isolated from a healthy donor) pulsed with various concentrations of CAP1-6D peptide. Peptide-pulsed B cells have been infected either with rF-TRICOM alone or with rF-TRICOM and simultaneously activated for 24 hours in the presence of CD40L. Results are shown in Figure 6; the combination of rF-TRICOM infection and CD40L activation resulted in a 2- to 4-fold enhancement of the APC potency of the B cells, as indicated by the higher levels of IFN-γ released, as compared with the levels observed when peptide-pulsed rF-TRICOM–infected B cells were used as APCs.
Production of IFN-γ by CEA-specific T cells after activation with peptide-pulsed B cells isolated from PBMCs. CEA-specific V8T cells (0.5 × 106/mL) were stimulated with irradiated allogeneic B cells that were infected with rF-TRICOM (▪) or infected with rF-TRICOM and activated for 24 hours in the presence of 1 μg/mL of CD40L (○) as described in “Materials and methods.” Various concentrations of CAP1-6D peptide were used to pulse the B cells. Supernatants were collected after 24 hours of stimulation. Error bars represent SD of multiple determinations.
Production of IFN-γ by CEA-specific T cells after activation with peptide-pulsed B cells isolated from PBMCs. CEA-specific V8T cells (0.5 × 106/mL) were stimulated with irradiated allogeneic B cells that were infected with rF-TRICOM (▪) or infected with rF-TRICOM and activated for 24 hours in the presence of 1 μg/mL of CD40L (○) as described in “Materials and methods.” Various concentrations of CAP1-6D peptide were used to pulse the B cells. Supernatants were collected after 24 hours of stimulation. Error bars represent SD of multiple determinations.
Establishment of antigen-specific T cells from PBMCs
Studies also were conducted to determine whether PSA peptide-pulsed rF-TRICOM–infected B cells, with or without activation with CD40L, as well as rF-PSA(3A)/TRICOM–infected B cells, could be used as efficient APCs to establish PSA-specific T-cell lines from “naive” T cells from an apparently healthy individual. In addition, PSA peptide-pulsed DCs generated from the same donor were used as APCs.
PSA-3A peptide-pulsed rF-TRICOM–infected B cells, with or without activation with CD40L, and DCs from the same donor were used in 3 consecutive IVS cycles to stimulate autologous T cells. In addition, T cells were stimulated for 3 IVS cycles in the presence of rF-PSA(3A)/TRICOM–infected B cells as a sole source of APCs (no peptide was exogenously added). The fourth IVS cycle was performed using autologous EBV-transformed B cells pulsed with 25 μg/mL of PSA-3A peptide as APCs; IFN-γ production was measured and results are shown in Table 2. Either peptide-pulsed rF-TRICOM–infected B cells or peptide-pulsed B cells infected with rF-TRICOM and activated with CD40L were able to establish PSA-specific T cells from PBMCs of a healthy donor, as indicated by the release of IFN-γ in response to PSA-3A peptide stimulation. Similar levels of IFN-γ also were detected when PSA-specific T cells that were established using peptide-pulsed DCs as APCs were stimulated in the presence of PSA-3A peptide. These results provide additional evidence that rF-TRICOM–infected B cells approach DCs in their ability to present antigens to the T cells.
Table 2 also shows that rF-PSA(3A)/TRICOM–infected B cells could be employed as a sole source of APCs (in the absence of exogenous peptide) to establish PSA-specific T cells from PBMCs.
Discussion
Because DCs are the most efficient of the professional APCs, numerous human immunotherapy protocols have been conducted using antigen-loaded DCs as adjuvants for vaccination of cancer patients as well as in the treatment of infectious diseases.9,30 Alternatively, DCs have been used for ex vivo generation of antigen-specific T cells for adoptive immunotherapy or experimental applications.31 Although highly efficient as APCs, DCs constitute a small population in the peripheral blood (0.1%-0.5% of PBMCs), and their maturation requires culture in the presence of expensive cytokines and growth factors. The preparation of mature DCs is a time-consuming and expensive procedure that limits the applicability of DC-based approaches, especially in terms of clinical protocols. After completion of the studies reported here, it was reported that autologous PBMCs loaded with a Melan-A peptide were used for vaccination of advanced melanoma patients, in combination with rhIL-12.32 The authors observed some clinical responses in the vaccinated patients that correlated with increases in the number of Melan-A–specific T cells in the blood of the responder patients. These authors also concluded that “this immunization approach may be more straightforward than dendritic cell strategies.”32
The objective of the present work was to investigate an alternative source of APCs that could be easily isolated from PBMCs, would not require extensive in vitro culture in the presence of expensive cytokines and growth factors, and could be efficiently used for ex vivo expansion of antigen-specific T cells, among other applications. Good candidates for this role are resting B cells because they constitute about 10%-15% of human PBMCs; very large numbers of B cells can be generated from a single phlebotomy as compared with the number of DCs that can be obtained from the same volume of peripheral blood. Still, antigen presentation by resting B cells is quite ineffective, and it is only after activation that B lymphocytes up-regulate costimulatory molecules and become competent APCs.8,33
In a previous report from our laboratory, the antigen-presenting ability of murine splenocytes (where more than 80% were B cells) was analyzed after infection with recombinant fowlpox and vaccinia vectors that simultaneously express B7-1, ICAM-1, and LFA-3 (named rF-TRICOM and rV-TRICOM, respectively). In vivo and in vitro assays have demonstrated that peptide-pulsed murine B cells infected with rF-TRICOM or rV-TRICOM vectors were almost as effective as peptide-pulsed DCs in eliciting T-cell responses.34 Oh et al have shown that the additional amount of signal 2 provided by the infection of murine splenocytes with a recombinant avipox-TRICOM vector not only contributes to increase the magnitude of the T-cell response but also improves the quality of the response, that is, high avidity CD8+ CTLs are selectively induced.35 It has previously been postulated36 that resting murine B cells are able to present antigens to antigen-specific murine T cells, but their antigen-presenting ability is radiosensitive. We have conducted experiments using irradiated (30 Gy) versus nonirradiated human B cells freshly isolated from PBMCs from various healthy donors; each was analyzed for its ability to present antigen to autologous Flu-specific CD8+ T cells. Our results showed that both nonirradiated and irradiated B cells were unable to stimulate IFN-γ production by Flu-specific T cells. All the experiments were thus conducted using irradiated B cells to avoid the proliferation of the APCs.
In the present study we have analyzed whether the capability of human B cells to present antigen to the T cells could be enhanced after infection with the avipox vector rF-TRICOM. Our results indicated that infection of B cells freshly isolated from human PBMCs with rF-TRICOM increased the surface expression of B7-1 and moderately increased ICAM-1 and LFA-3 levels of expression on the cell surface without modifying expression of class I and class II MHC molecules. One possible explanation for the varied expression of the 3 costimulatory molecules following infection with rF-TRICOM is that each of the transgenes encoding for these costimulatory molecules in the recombinant fowlpox vector is under the activity of a different promoter; it has previously been shown that these promoters can have different efficiencies in different cell types and thus presumably in different donors.37 Since 10%-15% of PBMCs are B cells and are demonstrating an infection efficiency average of 50%, the number of resulting infected B cells is still 10 times superior to the number of DCs that could be obtained from the same number of PBMCs. A similar comparison of the number of B cells versus DCs that could be obtained from PBMCs has been presented by others.28,29
The infected B cells were functionally assayed by measuring their ability to stimulate in vitro antigen-specific T cells. Two models were used in these studies: an autologous model in which T cells and B cells were isolated from the same healthy donor, and an allogeneic system in which antigen-specific pre-established T-cell lines (directed against CEA and MUC-1) were stimulated with B cells isolated from a different donor. Moreover, 2 types of peptides were used to provide the signal 1: (1) viral antigens: Flu-peptide (a strong immunogen) and an HPV peptide (a relatively weak antigen), and (2) “self”-tumor associated antigens: CEA, PSA, and MUC-1 peptides, considered to be weak immunogens. Our results demonstrated that peptide-pulsed rF-TRICOM–infected B cells were superior to peptide-pulsed uninfected B cells to stimulate antigen-specific T cells. The results were observed in the autologous as well as the allogeneic system, and with all different peptides assayed.
We also have conducted a comparison of the APC potency between rF-TRICOM–infected human B cells and human DCs (generated from PBMCs by culturing for 7 days in the presence of GM-CSF and IL-4). Our results have demonstrated that rFTRICOM–infected B cells approximated DCs in terms of their ability to present antigens to antigen-specific T cells in vitro. With some donors we have observed that peptide-pulsed DCs were more efficient than peptide-pulsed rF-TRICOM–infected B cells to activate antigen-specific T cells; in those cases, however, the difference in magnitude of T-cell activation could be easily overcome by increasing by about 10-fold the number of rF-TRICOM–infected B cells used for antigen presentation. The fact that B cells are more abundant and easier to obtain than DCs from peripheral blood makes it feasible to increase the ratio of B to T cells in order to achieve a more efficient activation of the T cells. It should be pointed out, however, that the studies reported here are not meant to prove that rF-TRICOM–infected B cells are as good as or better than DCs, but only to provide preclinical evidence for potential subsequent clinical evaluation and comparisons with DC approaches.
Vector-mediated delivery of antigenic epitopes into the B cells by using recombinant fowlpox vectors also was analyzed. Delivery of only a signal 1 to the B cells through infection with rF-CEA(6D) or rF-MUC-1 vectors did not mediate activation of CEA- and MUC-1–specific T cells, respectively. A simultaneous expression of the transgene protein and costimulatory molecules through infection with rF-CEA(6D)/TRICOM or rF-MUC-1/TRICOM, however, resulted in a marked enhancement of the T-cell activation. We also have been able to establish in vitro PSA-specific T cells from PBMCs of a healthy donor using B cells infected with rF-PSA-(3A)/TRICOM as a sole source of APCs. The use of B cells that endogenously express various CTL epitopes, as well as helper epitopes via vector infection, as an alternative to peptide-pulsed B cells allows broadening of the specificity of the expanded T cells and avoids the necessity of having different peptides corresponding to different MHC types.
From our results we conclude that B cells isolated from PBMCs infected with an avipox (rF)-TRICOM vector constitute an alternative source of efficient APCs that is easy to obtain and does not require extensive time in culture in the presence of expensive cytokines and growth factors.
The use of CD40L-activated human B cells as an alternative source of efficient APCs has been reported.28,29 In previous reports CD40L-activated B cells were generated from PBMCs by direct culture of whole PBMCs in the presence of soluble CD40L or by the coculture of whole PBMCs with irradiated CD40L-transfected cells, in both cases in the presence of IL-4 and cyclosporin A (CsA). Cultures were restimulated for up to 65 days; the expanded CD40L-activated B cells were shown to efficiently induce T-cell responses to various viral and tumor antigens. In the present study we sought to compare the APC potency of rF-TRICOM–infected B cells with that of CD40L-activated B cells. Unlike the previous reports on CD40L activation of B cells, the objective of this study was to establish a procedure for the generation of APCs that does not require long-term culture in the presence of expensive cytokines and growth factors. Therefore, we have conducted a short (24-hour) in vitro CD40L activation of freshly isolated B cells and have analyzed their capacity for antigen presentation, as compared with rF-TRICOM–infected B cells. Both CEA-specific T cells and MUC-1–specific T cells were stimulated in the presence of either peptide-pulsed rF-TRICOM–infected B cells or peptide-pulsed CD40L-activated B cells. Our results demonstrated that 24 hours of activation with CD40L was not sufficient to turn freshly isolated B cells into efficient APCs, as compared with rF-TRICOM–infected B cells. However, the combination of infection with rF-TRICOM and activation in the presence of CD40L resulted in an improved ability of the B cells for antigen presentation, as compared with that of B cells infected with rF-TRICOM or activated with CD40L alone.
We also have shown that PSA peptide-pulsed rF-TRICOM–infected B cells as well as peptide-pulsed B cells that were infected with rF-TRICOM and simultaneously activated with CD40L were able to establish PSA-specific T cells from PBMCs of a healthy donor, and their ability is similar to that of DCs. These results suggest that B cells infected with rF-TRICOM and simultaneously activated in the presence of CD40L for 24 hours may potentially be used as an efficient and accessible source of APCs for in vitro generation of antigen-specific T cells for experimental purposes as well as for potential adoptive immunotherapy protocols.
Prepublished online as Blood First Edition Paper, March 9, 2004; DOI 10.1182/blood-2003-09-3211.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.