Abstract
Regular monitoring of left ventricular ejection fraction (LVEF) for thalassemia major is widely practiced, but its informativeness for iron chelation treatment is unclear. Eighty-one patients with thalassemia major but no history of cardiac disease underwent quantitative annual LVEF monitoring by radionuclide ventriculography for a median of 6.0 years (interquartile range, 2-12 years). Intraobserver and interobserver reproducibility for LVEF determination were both less than 3%. LVEF values before and after transfusion did not differ, and exercise stress testing did not reliably expose underlying cardiomyopathy. An absolute LVEF of less than 45% or a decrease of more than 10 percentage units was significantly associated with subsequent development of symptomatic cardiac disease (P < .001) and death (P = .001), with a median interval between the first abnormal LVEF findings and the development of symptomatic heart disease of 3.5 years, allowing time for intervention. In 34 patients in whom LVEF was less than 45% or decreased by more than 10 percentage units, intensified chelation therapy was recommended (21 with subcutaneous and 13 with intravenous deferoxamine). All 27 patients who complied with intensification survived, whereas the 7 who did not comply died (P < .0001). The Kaplan-Meier estimate of survival beyond 40 years of age for all 81 patients is 83%. Sequential quantitative monitoring of LVEF is valuable for assessing cardiac risk and for identifying patients with thalassemia major who require intensified chelation therapy.
Introduction
Cardiac disease caused by transfusional iron overload remains the principal cause of death in patients with β-thalassemia major, despite improvements in iron chelation therapy during the past 25 years.1 For this reason, regular evaluation of cardiac function is recommended for all patients with thalassemia major2 and is now an integral part of their management. However, the value of monitoring cardiac function to the long-term management of thalassemia is unclear. This is partly because the prognostic significance of diastolic abnormalities, which appear early in the disease process, is unknown.3-5 Additionally, congestive heart failure (CHF) is often already present by the time systolic abnormalities have become manifest using echocardiography.6-11 These observations have led some workers to question the value of noninvasive monitoring of cardiac function in the management of thalassemia.12-14
Although recovery is possible in a proportion of patients with established CHF,15,16 overall long-term prognosis remains poor.17 Cardiac monitoring should, therefore, ideally identify patients at highest risk for cardiac decompensation before CHF develops. Sequential and reproducible quantification of ventricular function can in principle identify early changes in the left ventricular ejection fraction (LVEF) from baseline for each patient and could be used as a rationale for identifying patients at high risk. Radionuclide ventriculography using multigated acquisition (MUGA) gives a highly reproducible quantification of LVEF in normal and abnormal hearts.18-21 MUGA has been used prospectively as part of annual assessments at our center since 1981, and the value of these prospective data is addressed in this paper. For 20 years, we have used LVEF changes (absolute value less than 45% or decrease by more than 10 percentage units below baseline for each patient) to identify patients at greatest risk for cardiac decompensation. Here we report the outcome of this approach using sequential quantitative LVEF monitoring in 81 patients with thalassemia major and no cardiac disease history.
Patients, materials, and methods
Study design
The predictive value of sequential quantitative LVEF monitoring by MUGA for subsequent cardiac morbidity and mortality was examined in 81 patients with β-thalassemia major born between 1957 and 1987. Between March 1981 and February 2001, a strategy was adopted at University College London Hospitals for yearly MUGA monitoring of LVEF. MUGA data are available for 85 of 103 patients from this clinic for whom survival data have been previously reported.2 Eighty-one of the 85 patients had no history of cardiac disease at the time of study entry and are, therefore, those for whom the predictive value of MUGA monitoring is analyzed. Thirtynine patients are men and 42 are women, and the median age at which MUGA was initially performed was 19 years (interquartile range, 16-23 years). All patients underwent regular transfusions to maintain pretransfusion hemoglobin levels higher than 10.5 g/dL before 1995 and higher than 9.5 g/dL thereafter.
Routine cardiac evaluation consisted of a detailed clinical history, physical examination, resting and exercise electrocardiography (ECG), echocardiography, and MUGA. Twenty-four–hour Holter monitoring was performed in patients with palpitations or in patients with arrhythmias demonstrated by clinical examination, routine ECG, or both. Impaired left ventricular (LV) function was defined as a decrease in resting LVEF either to a value below the lower reference limit of 45% or by more than 10 percentage units between 2 consecutive measurements, regardless of the LVEF value. Thirty-four patients had evidence of LV dysfunction on at least one occasion during the period of observation (LVEF less than 45% in 28 patients and decrease by more than 10 percentage units in 6 patients).
Chelation therapy was performed exclusively with deferoxamine mesylate (DFO), which, in the absence of high-risk clinical features, consisted of a standard regimen (30-50 mg/kg per day by subcutaneous infusion 8-12 h/d, 5-7 d/wk). DFO treatment was intensified in the event of objective evidence of asymptomatic LV dysfunction at rest to prevent progression to frank CHF. Treatment was intensified using 1 of 3 modalities. The first modality was continuous intravenous DFO through an indwelling line at a dose of 50 to 100 mg/kg per 24 hours, as previously described in 17 patients,15 11 of whom were eligible for inclusion in this study because they had no preexisting cardiac disease. Data from 2 additional patients have also been included. The second modality was improvement in the subcutaneous DFO regimen, achieved by increasing the frequency, duration, or dose of administration. In the early years of the study, maximal 12-hour infusions were possible through mechanical pumps (up to 60 mg/kg per day). After 1994, subcutaneous DFO was given through 24-hour disposable balloon infusers22 at doses of 40 to 60 mg/kg per day up to 7 days a week. The third modality was continuous 24-hour intravenous infusion of DFO (100 mg/kg) diluted in 500 to 1000 mL normal saline and delivered though a peripheral vein on an inpatient basis for up to 1 week at a time to supplement ongoing subcutaneous treatment. Dosing intensification was reduced as serum ferritin values decreased in line with the therapeutic index, as previously described.15 The decision about which approach to adopt was based on extended interviews between the lead clinician and the patient and on the practicalities of each modality; the first was our preferred approach.
In addition, after 1995, this modality included interviews with a clinical psychologist, through whom underlying psychological issues pertinent to poor compliance were explored and rectified. Subsequent LVEF and serum ferritin findings were relayed to each patient as part of a sustained follow-up program. Compliance was monitored by patient interview, with the mean number of infusions per week used as a compliance end point.23
MUGA assessment
All LVEF studies were performed in the left anterior oblique position using IGE Portacamera (GE Medical Systems, Waukesha, WI)/Informatek Simis III (Informatek, Buc, France) and IGE Optima/Star 4000i (GE Medical Systems) configurations as previously described.15 The red cell labeling method15 had an efficiency of 98%. Image processing was carried out on the Portacamera/Informatek system as follows: after smoothing the raw data, Fourier phase, amplitude images, and end-diastolic and end-systolic images were displayed. A region of interest around the left ventricle was then assigned manually on the end-diastolic frame, always taking into account the end-systolic phase and amplitude image limits. After background correction of the region of interest using the method of Goris et al,24 ventricular time-activity curves were generated and LVEFs were calculated. Informatek supplied the data processing software. Data analysis on the Optima/Star configuration was broadly similar to the method described, except that SAGE software was used to determine the ventricular center (automatically) and the edge (semiautomatically). SAGE software was supplied by the manufacturer (GE Medical Systems) and was used unmodified.
The reproducibility of LVEF measurements was assessed on the 2 study configurations. On the IGE Portacamera/Informatek configuration, the interobserver correlation coefficient for a range of LVEF values (n = 60 patients) between 7% and 71% was 0.99 (P = .001), with a standard error of 2.79% between the results of 2 observers. Intraobserver reproducibility for a range of LVEF values (n = 66 patients) between 7% and 71% gave a correlation coefficient of 1.00 (P = .001), with a standard error of 2.57% between the results. On the IGE Optima/Star configuration, LVEF values calculated from 3 acquisitions carried out by the same observer on a range of values from 22% to 79% (n = 75 patients) gave a correlation coefficient of 0.98 (P < .001), with a standard error between the results of 2%. LVEF values calculated from 3 acquisitions by 2 independent observers at 2 different times on the same patients also showed a high correlation (r = 0.99), with a standard error of 1.8% between the results. Thus, there was no appreciable difference in reproducibility between the 2 systems. Changeover from the Portacamera/Informatek to the Optima/Star was effected in 1993 to 1994, with no systematic difference for LVEF values among approximately 50 patients without thalassemia studied on both configurations.
The reference range for the resting LVEF by MUGA in patients without thalassemia at our institution was 50% to 70%, with a 95% confidence interval for the lower value of 45% to 55%. The limits of reproducibility for the resting LVEF was 5 percentage units; thus, a change of more than 5 percentage units between serial measurements was defined as clinically significant. However, in this study, a change of more than 10 percentage units between serial measurements of resting LVEF was used as the trigger for treatment intensification because this is the limit of biologic variability in healthy subjects.21 Additionally, absolute LVEF values less than 45% were considered abnormal and triggered treatment intensification.
For exercise stress tests, LVEF measurements were obtained at rest, then after dynamic exercise in the supine position on a mechanically braked bicycle. Chest movements during exercise were minimized by the use of shoulder restraints, chest straps, and handgrips. Starting at 25 W, the load was increased in 25-W stages, each stage lasting 3 minutes, with continuous ECG monitoring using lead II and with pulse rate and blood pressure measurements at the end of each stage. Exercise was continued until maximum workload was achieved or until the patient developed fatigue, angina, dyspnea, significant hypotension, or ventricular arrhythmia. Data were acquired for the final 2 minutes of each stage. A normal response to dynamic exercise was defined as an increase in LVEF by more than 5 percentage units at maximal exercise. Serum ferritin measurements were generally measured monthly, as previously described.15
Outcome measures and statistical analysis
The outcome measures were CHF or arrhythmia requiring cardiac medication and cardiac death attributable to iron overload. CHF was defined by the criteria of the Task Force on Heart Failure of the European Society of Cardiology.25 The period of follow-up began on the date of a patient's first MUGA, and the cut-off point for follow-up was February 28, 2001. Patients leaving the study center for treatment abroad or in other centers were censored for analysis at the point of exit. The median follow-up period for the 81 patients was 5.8 years, with an interquartile range of 2.4 to 11.7 years and a maximum of 20 years.
Summary data are presented as median or as mean ± 1 SD. Pearson χ2 and Fisher exact tests were used to test the relationship between categorical variables. Differences between means of samples were analyzed using paired t tests. Survival was calculated using Kaplan-Meier survival analysis, and differences in survival between different groups of patients were compared using the log rank test. A logistic regression model, adjusted for serial tests on patients, was used to investigate the association between exercise response and subsequent CHF. All statistical analyses were performed using Stata software, version 7 (Stata Corporation, TX).
Results
Initial evaluation of MUGA for LVEF monitoring.
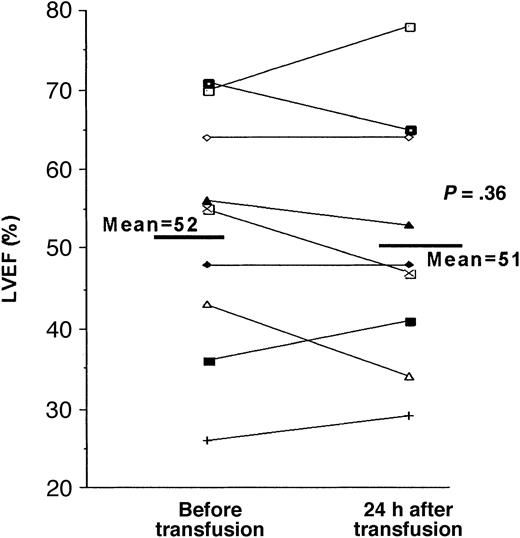
Effect of blood transfusion on LVEF. To determine whether it was necessary to stipulate when MUGA was performed during the blood transfusion cycle, paired measurements of LVEF were undertaken in 10 patients immediately before and 24 hours after transfusion. Mean pretransfusion and posttransfusion hemoglobin concentrations were 11.56 ± 1.16 g/dL and 15.0 ± 1.61 g/dL (P < .0001), with mean hematocrits of 0.34 ± 0.03 and 0.46 ± 0.06 (P < .0001). There was no significant difference between resting LVEF before (52% ± 14%) and 24 hours after (51% ± 15%) blood transfusion (P = .36) (Figure 1). The relatively high pretransfusion mean hemoglobin value reflects the transfusion policy used at the time (to keep pretransfusion hemoglobin levels higher than 10.5 g/dL) and reflects that some patients in this study underwent transfusion in mid-cycle. There was no relationship between the change in LVEF before and after transfusion and either the hemoglobin increment with transfusion or the pretransfusion hemoglobin value.
Effect of blood transfusion on LVEF measurement by MUGA. LVEF by MUGA at rest is shown in 10 patients with thalassemia major before and 24 hours after blood transfusion. There was no significant difference between mean pretransfusion and mean posttransfusion LVEF (P = .36).
Effect of blood transfusion on LVEF measurement by MUGA. LVEF by MUGA at rest is shown in 10 patients with thalassemia major before and 24 hours after blood transfusion. There was no significant difference between mean pretransfusion and mean posttransfusion LVEF (P = .36).
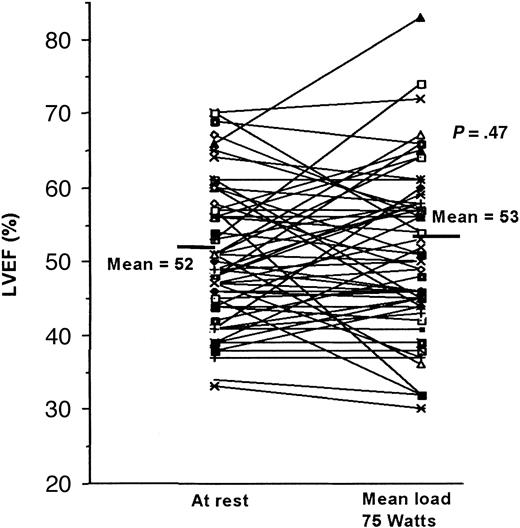
Effect of dynamic exercise on LVEF. Sixty paired LVEF exercise studies were performed sequentially on 27 patients with thalassemia major in a 5-year period. Fatigue and dyspnea were the reasons for terminating exercise, and in more than half of these tests patients failed to achieve 85% of the predicted heart rate after exercise. In those with normal resting LVEF, the mean peak exercise load achieved was 78 ± 21 W. By contrast, the mean peak exercise level attained in 25 control subjects (4 healthy volunteers and 21 patients with angiographically normal hearts) was 155 W (range, 125-200 W), with only 5 of the 25 subjects failing to achieve the desired hemodynamic response.26 Forty tests showed abnormal responses (with failure to show an increased LVEF of more than 5 percentage units), and 20 showed normal responses.
In all 27 thalassemia patients, there was no significant difference between LVEF values before and after exercise (52% ± 8% and 53% ± 11%; P = .47) (Figure 2). Exercise-induced changes in the subgroup of patients with normal resting LVEF (n = 19) again showed no difference between in LVEF values before and after exercise (54% ± 7% and 54% ± 12%; P = .91). In the 25 control subjects, mean LVEF values increased from 64% ± 10% to 73% ± 8% (P < .01).26
Effect of dynamic exercise on LVEF measurement by MUGA. LVEF is shown before and after fatigue-limited exercise in 60 paired observations in 27 patients. There was no significant difference in mean LVEF before and after exercise (P = .47).
Effect of dynamic exercise on LVEF measurement by MUGA. LVEF is shown before and after fatigue-limited exercise in 60 paired observations in 27 patients. There was no significant difference in mean LVEF before and after exercise (P = .47).
Investigation of cardiac outcomes after each of the 60 studies in the 27 patients using logistic regression analysis adjusted for serial tests on patients provided no evidence to support an added prognostic value of exercise testing. Exercise response was not significantly associated with subsequent heart failure, even after adjusting for peak exercise load.
Value of LVEF in predicting and managing cardiac disease.
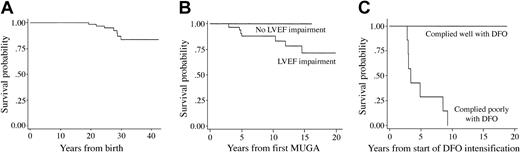
Relationship between impaired LVEF and long-term survival (Table 1). The Kaplan-Meier estimate of survival beyond 40 years of age was 83% in the entire cohort of 81 patients monitored regularly with resting MUGA for LVEF (Figure 3A). In patients in whom LV dysfunction was demonstrated by MUGA, subsequent symptomatic heart disease and cardiac death occurred more frequently. Thus, in patients with asymptomatic LVEF changes, as defined in “Patients, materials, and methods,” the odds of subsequent heart disease were 25 times those of patients with normal LVEF (P < .001). Only 1 of 47 patients for whom there was no decrease in LVEF experienced a cardiac event. There was also a significant difference in the frequency of cardiac death between the groups with and without asymptomatic LVEF changes (P = .001). The median time interval between the first abnormal LVEF value and the development of symptomatic heart disease was 3.5 years (range, 1.7-10.9 years), and 7 of these patients died after a median of 3.8 years (range, 2.9-9.3 years) from the time of the initial LVEF decrease. These findings show that LVEF changes identified with sequential quantitative monitoring generally precede and predict subsequent significant clinical cardiac decompensation by a sufficient period to allow treatment intensification. Although all treatment decisions were made on the basis of an LVEF less than 45% or a decrease of more than 10 percentage units, we also retrospectively examined the relative importance of absolute LVEF less than 45% compared with a decrement of more than 10 percentage units with respect to subsequent survival and cardiac complications. This comparison showed that whereas there were no deaths or cardiac disease among patients whose LVEF decreased by more than 10 percentage units while absolute values remained greater than 45%, only 57% of patients in whom LVEF decreased below this value had no cardiac disease, with only 75% surviving long-term.
Survival in 81 patients with thalassemia major monitored regularly with MUGA for LVEF. (A) Kaplan-Meier estimate of survival beyond 40 years of age is 83% in the entire cohort of 81 patients monitored regularly with MUGA for LVEF. (B) Kaplan-Meier estimates of survival in category 1 (n = 34) and category 2 (n = 47). It can be seen that all deaths (n = 7) occurred in category 1 patients, namely, patients with demonstrable left ventricular dysfunction during the period of observation. (C) Kaplan-Meier estimates of survival are shown in 34 category 1 patients subdivided on the basis of compliance with DFO intensification therapy. All deaths (n = 7) occurred in patients who did not sustain compliance with DFO (P < .0001, log rank test).
Survival in 81 patients with thalassemia major monitored regularly with MUGA for LVEF. (A) Kaplan-Meier estimate of survival beyond 40 years of age is 83% in the entire cohort of 81 patients monitored regularly with MUGA for LVEF. (B) Kaplan-Meier estimates of survival in category 1 (n = 34) and category 2 (n = 47). It can be seen that all deaths (n = 7) occurred in category 1 patients, namely, patients with demonstrable left ventricular dysfunction during the period of observation. (C) Kaplan-Meier estimates of survival are shown in 34 category 1 patients subdivided on the basis of compliance with DFO intensification therapy. All deaths (n = 7) occurred in patients who did not sustain compliance with DFO (P < .0001, log rank test).
Interventional treatment with DFO based on LVEF and long-term survival. Patients were categorized into 2 groups, those with resting LVEF less than 45% or more than a 10 percentage unit drop (category 1) and those with resting LVEF greater than 45% (category 2), in accordance with predetermined criteria for DFO intensification (“Patients, materials, and methods”). When survival was compared between both groups of patients based on LVEF, it was seen that all deaths occurred in category 1 patients (Table 1; Figure 3B). Figure 3C shows that among the 34 category 1 patients, all deaths (n = 7) occurred in those who did not sustain improvements in compliance with intensified DFO therapy after the LVEF abnormality had been identified. Median survival in this group with abnormal LVEF plus poorly sustained compliance with intensification was only 3.8 years from the initial deterioration in resting LVEF. This is in contrast to those patients who adhered to sustained intervention with DFO (n = 27), none of whom have died during a follow-up period of up to 20 years (median, 11.7 years) after the initial decrease in LVEF.
The influence of the DFO route (subcutaneous or intravenous) used for therapy intensification on outcomes among the 34 category 1 patients was also examined (Table 2). As previously reported, there is a significant improvement in LVEF after intravenous DFO through the Port-A-Cath (Pharmacia Deltec, St Paul, MN).15 However, Table 2 clearly shows that there was significant improvement in LVEF after subcutaneous DFO intensification. These findings show that sustained responses can be achieved with either route, provided compliance is maintained.
Among the 27 surviving patients who received treatment intensification on the basis of LVEF, the cumulative DFO dose to the point when cardiac function stabilized was estimated in 22 patients for whom adequate records are available. The median cumulative DFO dose was 36 g/kg body weight (range, 16-139 g/kg) over a median of 3 years (range, 1.3-8 years). When the cumulative dose for each patient was calculated on a daily basis, the median value was 43 mg/kg per day, suggesting that conventional doses of DFO are efficacious in preventing and reversing LV dysfunction, provided there is sustained patient compliance with the prescribed regimen.
Relationship between other risk factors and cardiac complications
Patient age at the start of standard subcutaneous DFO therapy27 and serum ferritin levels27 have been identified as predictors of cardiac risk in patients with thalassemia major. Therefore, we examined their predictive value for cardiac risk in relation to that of sequential LVEF monitoring. Although myocarditis has been identified as a precipitant of heart failure in a small portion of thalassemia patients, no patients in this study had evidence of myocarditis as a precipitant of cardiac decompensation.28
Effect of age on cardiac risk at initiation of subcutaneous DFO therapy. As seen in Table 1, 78 patients had evaluable data with respect to age of DFO commencement. Therapy started when 42 of these patients were younger than 10 years of age and for 36 of these patients when they were older than 10. Symptomatic heart disease occurred more frequently in patients who started subcutaneous DFO after age 10 than in those in whom this treatment was started at an earlier age (odds ratio, 5.0; P = .005). This was also true of death from cardiac causes (odds ratio, 7.0; P = .01)
Serum ferritin and cardiac risk. To examine the relationship between serum ferritin concentration and cardiac risk, we divided the study cohort into 2 groups using the risk stratification criteria identified by Olivieri et al.27 This analysis examines the effect of consistently high ferritin values (higher than 2500 μg/L) on at least two thirds of occasions on survival. Table 1 shows that cardiac outcome was significantly better in those patients who maintained serum ferritin values lower than 2500 μg/L on at least two thirds of occasions. The odds ratio for cardiac complications in patients who failed to maintain ferritin levels lower than 2500 μg/L on at least two thirds of occasions was 3.25 (P = .05). The risk for death from iron overload was also significantly increased in this group (P = .002).
Survival was significantly worse in the group with chronically elevated serum ferritin values (P = .02) (not shown). This was also true in the subgroup of patients in whom decreases in LVEF had been recorded (n = 34) and in whom deaths from cardiac disease (n = 7) only occurred in patients who failed to maintain ferritin values lower than 2500 μg/L on at least two thirds of occasions. No deaths were seen in those patients with LVEF decrements in whom ferritin values remained lower than 2500 μg/L on at least two thirds of occasions.
Discussion
Although resting and exercise LVEF responses using MUGA have been described in the follow-up of small groups of thalassemia patients for periods up to 4 years,11,29 this is the first study to investigate the long-term prognostic value of monitoring for asymptomatic LV dysfunction in a large group of thalassemia patients with unlimited access to DFO chelation therapy. In our group of patients, LVEF performed with MUGA and serum ferritin were the regular tools for monitoring and adjusting therapy. Although this approach was adopted for all patients beginning in the early 1980s, the procedure was not set up through a formal, prospective study; consequently, there is heterogeneity in patients' follow-up times and prior chelation histories. It is clear, however, that the overall survival is excellent (83% at 40 years) and indeed is the best so far reported, suggesting that this approach is useful. Our findings show that, using MUGA, a decrease in LVEF of more than 10 percentage units or an absolute value below the reference range is associated with progression to clinical heart failure within a median of 3.5 years and to death within a median of 3.8 years if DFO intensification is not achieved. Further analysis of the data suggested that under the conditions of observation and intervention adopted in this study, a decrease to an absolute value of less than 45% is more discriminatory for survival than a relative decrement of more than 10 percentage units.
Previous studies in thalassemia major using MUGA suggested that systolic dysfunction may precede frank CHF and that a successful clinical outcome may be achieved with appropriate intensification of DFO therapy.15,29-32 In this paper, we have observed LVEF changes over a median period of 6 years, with 25% of the patients being observed between 12 and 20 years. It is clear that detectable changes in systolic function precede the development of clinical heart failure sufficiently early for a useful intervention strategy to be adopted. After an initial rapid improvement in systolic function with intensification of DFO as previously described,15 there was characteristically a more gradual improvement that took several years of sustained treatment for maximal effect (data not shown). In all but 1 patient in the present study, LVEF changes were demonstrable before cardiac symptoms appeared.
Our findings may underestimate the effectiveness of the strategy used for LVEF monitoring and treatment intensification because in the older patients, baseline LVEF values were not obtained during childhood or early adolescence. Thus, a decrease in LVEF of 10 percentage units or more from the true baseline value could have been overlooked, and intensification might have been delayed. Indeed, among patients born after 1975 who were exposed to DFO early in life and have been monitored from an earlier age, survival is 100% at 25 years.2 These data contrast strikingly with the survival of patients in the United Kingdom as a whole, in whom survival is only 50% by the age of 35 years,33 and they reflect the effectiveness of DFO therapy when used in a center in which monitoring and intervention are given high priority. However, the optimal age at which monitoring of ventricular function should be started remains unclear. In the prechelation-era study by Engle et al,34 the first signs of cardiac involvement emerged at approximately 10 years of age, with patients becoming symptomatic in middle to late adolescence. In our study, one patient already had a reduced LVEF of 39% when her initial MUGA was performed at 13 years of age, although she was clinically asymptomatic at the time. We suggest that yearly quantitative LVEF monitoring of patients should begin ideally by 10 years of age.
Longitudinal monitoring of LV systolic function in thalassemia was traditionally considered of limited value because changes were only demonstrable as late events using echocardiography.6,8,9,12 However, the limitations of echocardiography for sequential quantitative LVEF measurement are well recognized: the technique is heavily reliant on operator skill, and assumptions have to be made about ventricular geometry, resulting in greater interobserver variability for LVEF,35 more so in severely impaired ventricles. Indeed, early studies in thalassemia major showed that MUGA was a more sensitive indicator of declining cardiac function than M-mode echocardiography, both at rest and on exercise.7 In addition, the earliest echocardiographic studies were conducted before current standard subcutaneous and intensive intravenous DFO regimens were available and used either no chelation or subtherapeutic doses of DFO.6,8,9,12 Thus, there was no effective salvage therapy for patients with deteriorating ventricular function, and mortality was high. Doppler echocardiography has been used to evaluate diastolic function3,36 and, more recently, to examine regional wall motion.37 Although abnormalities in diastolic function and regional wall motion can be identified before those of systolic dysfunction, no studies have been conducted on how these affect prognosis or how these might be used as a trigger for treatment intensification. Unlike echocardiography, MUGA does not require any geometric assumptions about ventricular shape; it is thus highly reproducible for quantification of LVEF, even for abnormal hearts. The recognized reliability of MUGA for assessing ventricular function was demonstrated by its selection as the method of choice for several major cardiac intervention studies in the 1980s and 1990s.38-41 The intraobserver and interobserver reproducibility of less than 3% for resting LVEF in our hands is comparable to that reported by other workers.18,19,21 Although MUGA was the tool available for sequential quantitative monitoring from the early 1980s, quantitative monitoring of LVEF is now possible with magnetic resonance imaging (MRI),42-44 which also has excellent reproducibility. Recently, MRI techniques have been used to estimate myocardial iron and, by inference, cardiac risk.45,46 However, the long-term prognostic significance of this modality has yet to be verified, and it is unclear how chelation treatment should be stratified based on such a measurement. Our study, on the other hand, shows that LVEF can be used as an easily available and effective tool for treatment stratification and intervention and that it has a demonstrable impact on cardiac disease and survival.
Our findings show that the excellent reproducibility achieved with MUGA is unaffected by blood transfusion under the conditions of this study. A mean pretransfusion hemoglobin level exceeding 10.5 g/dL was policy at the time of the paired measurements and was relatively high compared with current transfusion practice. However, analysis of the individual changes in LVEF with transfusion shows that these are unaffected by the variability in pretransfusion hemoglobin values seen in this study. These results are in keeping with electrocardiography findings observed by Henry et al,9 who found no change in LVEF 2 to 4 hours after transfusion in thalassemia major patients in whom pretransfusion values were lower than in our patient group.
Exercise stress testing appeared to be of limited additional value in our patient group. LVEF values determined by MUGA were reported to be abnormal after exercise compared with at rest in a higher proportion of thalassemia patients who had not undergone chelation therapy, with an invariable increase in LVEF noted in control subjects.32 However, subsequent work showed a wide variation in exercise responses in healthy persons, and exercise-induced increments are not invariably seen.47 Furthermore, a wide overlap between LVEF responses of subjects with angiographically normal hearts and those with coronary artery disease is now recognized,48 whereas invariable increases in LVEF had been reported initially.49 Exercise LVEF testing using MUGA with a follow up of 1 to 4 years was reported by Freeman et al29,31 in 23 thalassemia major patients receiving subcutaneous DFO. Although a minority of patients had abnormal resting LVEF values, most showed abnormal exercise responses, suggesting an increased sensitivity of exercise compared with resting LVEF. However, neither increased specificity nor prognostic significance was demonstrated. In our own study, subsequent clinical heart failure or cardiac death were no more common in those with abnormalities demonstrated with exercise than in those at rest. A confounding factor in our study was that peak exercise load, an independent determinant of the exercise response,47 was variable between and within patients. Because exercise testing was undertaken at variable points in the transfusion cycle, in principle this could have contributed to the variation in exercise tolerance. In practice, however, this was unlikely because pretransfusion values were typically greater than 10.5 g/dL. It has been suggested that pharmacologic stressing might reduce variability related to patient cooperation during exercise testing. In our hands, dobutamine at doses up to 40 μg/kg per minute often led to unacceptable symptoms such as flushing and lightheadedness. Although low-dose dobutamine (5 μg/kg per minute) has been reported to expose underlying cardiomyopathy in thalassemia patients using echocardiography,50 no peer-reviewed papers have been published on its effects on LVEF in thalassemia patients using MUGA.
Clearly, there are a number of useful approaches to monitoring iron overload in thalassemia major, some of which have been shown to have prognostic value with DFO use, such as serum ferritin,27 liver iron,51 and treatment compliance.23,51 Although our findings support a relationship between serum ferritin and outcome, we recognize the limitations of using serum ferritin, particularly as a single measurement at an arbitrary time point, because many factors other than body iron burden affect serum ferritin. It is of note that the association of ferritin with prognosis in this study and in a previous study by Olivieri et al27 linked prognosis to sustained increases in serum ferritin over many years, not simply single ferritin measurements. The relationship between liver iron and prognosis has not been examined in this paper because this was not one of the determinants used for regular monitoring and, thus, for chelation stratification. Outcome, however, is likely to include a component of the duration of exposure to high liver iron levels, as in the Brittenham analysis,51 in which survival was examined in relation to the ratio between cumulative transfusional iron loading and DFO use over time.
In conclusion, it is clear that sequential quantitative monitoring of LVEF, combined with timely and sustained intensification of DFO where necessary, can be used to achieve excellent long-term prognoses in patients with thalassemia major. Contrary to some traditional thinking, changes can be identified sufficiently early to prevent further deterioration of LVEF, to reverse cardiac dysfunction, and to achieve excellent long-term survival. For this approach to be effective, however, LVEF measurements must be quantitative, highly reproducible, and performed regularly (at least annually). Our data show that single measurements at arbitrary time points will have less prognostic value than those obtained by sequential analysis. We suggest that when new or established monitoring tools are used to identify cardiac risk, sequential changes of the marker in question and full transfusional and chelation histories should be taken into account.
Prepublished online as Blood First Edition Paper, March 4, 2004; DOI 10.1182/blood-2003-08-2841.
J.B.P. currently acts on the safety board for Cox 189 (Novartis) and on advisory boards for ICL670 (Novartis).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.