Abstract
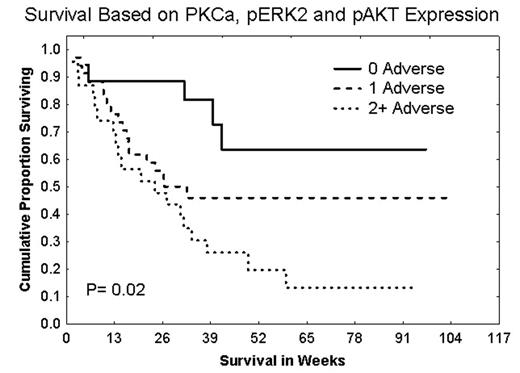
The disregulation of signal transduction pathways (STPs) provides AML cells with proliferative and survival advantages in vivo. Redundancy and/or “crosstalk” within STPs could trigger the activation of multiple downstream effectors. In retrospective studies we have demonstrated that high levels of PKCα and phosphorylated ERK2 (pERK2) in AML blasts were adverse prognostic indicators. Therefore, we conducted a prospective study to determine if the activation of three STPs (i.e., PKCα, ERK2, and AKT) was associated with the clinical response of 188 newly diagnosed AML patients. The STP protein expression levels in patient samples were evaluated by Western blot analysis. Patients whose AML cells expressed high levels of PKCa had a lower incidence of complete remission (CR, 31% vs. 58%, p=0.01), tended to have higher relapse rates (60% vs. 44%), and experienced a shorter duration of CR (29 vs. 38 weeks) resulting in a lower overall median survival (12 vs. 41 weeks, P= 0.00003). Higher expression of ERK2 did not affect the CR (53% vs. 53%) or relapse rates (48% vs. 44%) of AML, but was associated with a trend for shorter CR durations (32 vs. 44 weeks) combining to result in inferior overall median survival (44 vs. 59 weeks, p= 0.02). pERK2 was undetectable in 27% of the patient samples, and was weakly or strongly expressed in 38.5% or 34% respectively. Strong expression of pERK2 was associated with trends for lower CR rates (45% vs. 57%), higher relapse rates (57% vs. 42%), somewhat shorter CR durations (30 vs. 38 weeks), and statistically significantly shorter overall median survival (32 vs. 44 weeks, p= 0.04). pAKT was undetectable, weakly, moderately, or strongly expressed in 9%, 27%, 38%, or 32% of the samples, respectively. Patients with low levels of pAKT had better CR rates (59% vs. 45%), and a statistically significant longer median survival (not reached vs. 26 weeks, p= 0.02). There were no significant differences in gender, Zubrod PS, or cytogenetics between the favorable and adverse groups for any of these proteins. We hypothesized that activation of multiple pathways would be a more adverse finding. We observed adverse expression levels of 0, 1 or 2+ STP proteins in 24%, 45% and 31% of the cases, respectively. Isolated high PKCa expression did not occur. Isolated strong pERK2 or strong pAKT expression occurred in 8% or 35% of the patient samples. Only 6% of the patients had high levels of all 3 proteins. Survival was inversely correlated with the number of proteins with adverse expression with long-term survival approximating 64%, 46%, and 13% for those with none, one or two or more proteins with adverse expression. This study demonstrates that the downstream activation of STP effectors is common in AML, and that multiple effector activation is common, occurring in approximately 33% of the cases. Agents targeting individual STPs are undergoing clinical evaluation. Our data suggest that, to improve the efficacy of therapy for AML, it may be crucial to match the agent to the STP(s) activated in a given patient, and that combined blockade may be required when multiple STPs are activated.
Author notes
Corresponding author