Abstract
X-linked lymphoproliferative disease (XLP) is a congenital immunodeficiency that is characterized by an abnormal immune response to primary Epstein-Barr virus (EBV) infection. After EBV exposure, affected patients often develop fulminant infectious mononucleosis (FIM), a life-threatening condition marked by the uncontrolled expansion and activation of T and B lymphocytes and macrophages. We hypothesized that the rapid elimination of B cells immediately following EBV exposure might reduce the severity of primary EBV infection in patients with XLP. To test this possibility, we administered the anti-CD20 antibody rituximab to 2 patients who presented with acute infection. Following treatment, both patients exhibited a complete resolution of symptoms and no longer demonstrated detectable EBV DNA within circulating lymphocytes. Moreover, neither patient has developed FIM or lymphoma in more than 2 years of follow-up. These data suggest that the pre-emptive use of B-cell–directed therapy may reduce the morbidity and mortality of primary EBV infection in XLP-affected individuals.
Introduction
X-linked lymphoproliferative disease (XLP) is a congenital immunodeficiency associated with an inappropriate anti–Epstein-Barr virus (EBV) immune response.1 After primary infection, patients commonly develop a hemophagocytic syndrome known as fulminant infectious mononucleosis (FIM), which is characterized by the polyclonal expansion of EBV-infected B cells and the dysregulated expansion and activation of T cells and macrophages. FIM leads to hepatic and bone marrow (BM) failure and is fatal in more than 92% of cases.1
XLP results from germ line mutations in the SH2D1A gene, which encodes the adaptor protein signaling lymphocytic activation molecule–associated protein (SAP).2-4 SAP is expressed in T lymphocytes and natural killer (NK) cells, where it binds to the cytoplasmic domain of the signaling lymphocytic activation molecule (SLAM) and to several structurally related receptors.5 While the roles of SLAM are only beginning to be understood, studies suggest that this receptor functions in a homotypic fashion to bridge adjacent SLAM-expressing cells. SLAM ligation enhances antigen receptor–induced T- and B-cell proliferation and B-cell antibody production and modulates T-cell cytokine secretion.5 As SLAM expression is rapidly up-regulated on activated lymphocytes, the physical interaction between SLAM-expressing EBV-infected B cells and reactive CD4+ and CD8+ T cells might guide the development of a normal anti-EBV immune response. Thus, in the absence of functional SAP, SLAM or other SAP-associated receptors might not signal properly, which could compromise the control of EBV-infected B cells and facilitate the secondary expansion of T cells and macrophages. Despite improved understanding of its genetics and biology, XLP remains a fatal disorder curable only by allogeneic hematopoietic stem cell transplantation (HSCT).6-10
There is no evidence that SAP-deficient B cells function differently than normal B cells. Nonetheless, the entry of EBV into B cells is critical for establishing virus infection.11 In addition, it remains possible that EBV-infected B cells could promote FIM due to perturbations in SLAM-induced responses in SAP-deficient T cells. The anti-CD20 monoclonal antibody rituximab eliminates B cells, a property that has encouraged its use in the treatment of B-cell lymphomas and EBV-associated posttransplantation lymphoproliferative disorders.12 Based on these features, we explored rituximab's potential to alter the historically fatal outcome of primary EBV infection in patients with XLP. Here we describe 2 individuals who presented with acute infection and were successfully treated with regimens including rituximab.
Study design
Patient no. 1
Patient no. 1 was a 26-year-old white man who presented with a 3-week history of fever, headache, sore throat, and fatigue and a 1-week history of lymphadenopathy. He had 4 siblings who had died from XLP. Previous genetic studies revealed that he carried a germ line G383C SH2D1A mutation, which was predicted to lead to the substitution of arginine for serine at codon 28 of SAP.13 Prior to the current illness, patient no. 1 had been healthy. He had received monthly intravenous gammaglobulin as prophylaxis against EBV infection.
At presentation, patient no. 1 showed a mild leukocytosis with a marked lymphocytosis (Table 1). Large granular lymphocytes and atypical lymphocytes were noted on a peripheral smear. Flow cytometric studies revealed an inverted CD4/CD8 ratio (1:4.4) with natural killer (NK) cells representing 10% to 15% of circulating lymphocytes (not shown). He also exhibited a mild elevation in liver transaminases. On examination, patient no. 1 had pharyngeal erythema, cervical adenopathy, and a palpable liver edge approximately 2 cm below the costal margin. Serologic testing for EBV revealed a positive index of 3.26 for IgM antibody to viral capsid antigen. Quantitative EBV-specific polymerase chain reaction (EBV-PCR) revealed a viral load of 18 164 copies of EBV genome/mL of blood.14
Patient no. 2
Patient no. 2, a 25-year-old white male with 3 brothers who died from XLP, was known to harbor a germ line SH2D1A deletion. He presented with a 4-day history of fever, chills, myalgia, headache, sore throat, nausea, and vomiting. Two years earlier, patient no. 2 had undergone splenectomy during a work-up for nonmalignant pulmonary nodules and splenomegaly. On examination, patient no. 2 appeared mildly ill, but had no lymphadenopathy, hepatomegaly, or jaundice. Laboratory testing revealed normal peripheral blood counts and minimally elevated transaminases (Table 1). Serologic testing for acute EBV infection was not performed. Qualitative EBV-PCR was positive on the day of presentation. A subsequent quantitative EBV-PCR was obtained on day 8 after initiation of therapy and revealed a viral load of 2000 copies of EBV genome/mL of blood.
Treatment regimens
Both patients were treated in compliance with institutional review board–approved guidelines at the Dana-Farber Cancer Institute (Boston, MA) and the Hospital of the University of Pennsylvania. Informed consent was obtained in accordance with the Declaration of Helsinki.
On the day of presentation, patient no. 1 was treated with intravenously administered methylprednisone (1 mg/kg), immunoglobulin (10 g), ganciclovir (5 mg/kg; given every 12 hours; 2 doses), and rituximab (375 mg/m2). On day 2, he began oral acyclovir (800 mg) 5 times per day, which was continued for 6 months. He received a second 10-g dose of immunoglobulin on day 4.
On the fourth day after presentation, patient no. 2 was treated with oral prednisone (30 mg) twice daily, intravenously adminstered immunoglobulin (1 g/kg), and oral acyclovir (800 mg, 5 times per day). Prednisone was administered for 1 week and tapered over 3 days. Acyclovir was continued for 3 months. On day 5, he received intravenously administered rituximab (375 mg/m2), which was repeated on day 12 due to persistent atypical lymphocytosis and elevated serum transaminase concentrations.
Results and discussion
Allogeneic HSCT is the treatment of choice for the prevention of EBV-related morbidity and mortality in XLP.6-10 For patients who do not undergo transplantation, acute EBV infection poses a therapeutic challenge as patients rapidly develop FIM. Antiviral therapies, such as acyclovir, ganciclovir, and interferon-α have not been successful in preventing or treating FIM.15,16 While steroids, etoposide, and cyclosporine provide symptomatic benefit in some cases of EBV-induced hemophagocytosis,17,18 FIM remains the most common cause of death for patients with XLP.1,19
Work from several laboratories has shown that SAP-deficient T and NK cells exhibit defects in cytotoxic function and interferon γ (IFNγ) production, factors that might interfere with clearance of EBV-infected B cells.5 As persistence of these cells might subsequently promote the proliferation and activation of reactive T cells and macrophages, we hypothesized that the rapid eradication of EBV-infected B cells immediately after exposure might reduce viral burden and prevent the secondary hemophagocytic syndrome that typifies FIM. Because anti-CD20 immunotherapy with rituximab leads to the elimination of more than 80% of circulating B cells within days,20 we developed individualized therapies centered around this medication for 2 patients with XLP presenting with acute EBV infection. These regimens varied slightly based on the preferences of treating oncologists, who were from different institutions. However, in both regimens, rituximab was combined with steroids to suppress T-cell activation. Based on historic approaches, both regimens also included more traditional antiviral agents, such as acyclovir and ganciclovir.
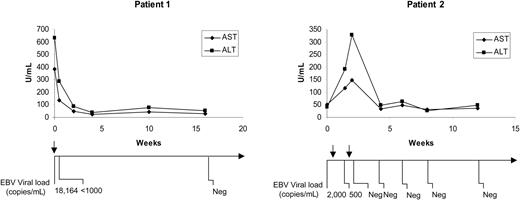
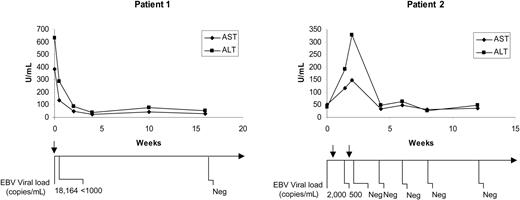
Following initiation of treatment, both patients demonstrated a rapid reduction of B cells to 1% or less of circulating lymphocytes (not shown). This decrease in B-cell number was associated with a decline in peripheral blood leukocyte-associated EBV DNA to levels below the limit of detection (Figure 1). In both patients, clinical improvement occurred within 24 to 48 hours, as was evident by a return to normal body temperature and disappearance of malaise and fatigue. Notably, neither patient developed hemophagocytosis. Despite rapid improvement in clinical and virologic features, certain laboratory parameters, such as elevations in transaminases, white blood cell count, and percentage of atypical lymphocytes, required 4 to 16 weeks to return to baseline levels (Figure 1 and not shown). When compared with the prolonged convalescence seen in adult immunocompetent individuals with mononucleosis, the rapid recovery of these patients suggests that rituximab exerts a positive effect on the course of acute EBV infection.
Changes in liver transaminases and EBV DNA levels are shown for patients no. 1 and no. 2 following treatment with rituximab. The timelines below the figures indicate the time points at which quantitative EBV-PCR was performed and the values that were obtained. The arrows above the timelines indicate when rituximab was administered. AST indicates aspartate aminotransferase; ALT, alanine aminotransferase; and Neg, negative.
Changes in liver transaminases and EBV DNA levels are shown for patients no. 1 and no. 2 following treatment with rituximab. The timelines below the figures indicate the time points at which quantitative EBV-PCR was performed and the values that were obtained. The arrows above the timelines indicate when rituximab was administered. AST indicates aspartate aminotransferase; ALT, alanine aminotransferase; and Neg, negative.
Rituximab reduces the number of circulating B cells for up to 6 months or longer.20 Although lymphomas are known to occur in EBV-positive and EBV-negative patients with XLP, the development of lymphoma occurs earlier in EBV-infected individuals.21 We do not know whether the reduction in B-cell number that resulted following rituximab therapy will prevent the development of lymphoma in these treated patients. However, neither patient has developed lymphoma in more than 24 months of follow-up. Interestingly, surveillance monitoring in patient no. 1 revealed the onset of hypogammaglobulinemia 5 months after treatment with rituximab, and re-emergence of detectable EBV DNA at 14 months after treatment (not shown). Thus, rituximab may not prevent the natural progression of hypogammaglobulinemia or lead to long-term control of EBV infection in certain patients with XLP. As neither patient has undergone testing for EBV-specific T- or B-cell immunity since treatment with rituximab, it is not possible to discern how this therapy will influence their long-term immunologic response to EBV.
Rituximab induces a rapid improvement in the clinical symptoms associated with acute EBV infection in patients with XLP. We recommend that rituximab be considered as part of the initial management for patients with XLP following primary EBV exposure. Furthermore, the pre-emptive use of rituximab may benefit the management of other disorders associated with EBV-induced hemophagocytosis, such as the familial or acquired hemophagocytic lymphohistiocytoses.
Prepublished online as Blood First Edition Paper, October 19, 2004; DOI 10.1182/blood-2004-07-2965.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We would like to thank the patients who participated in this investigation.