Abstract
Background: Patients with HD and NHL have been treated with autologous stem cell transplantation (SCT) since the 1980s at the University of Nebraska Medical Center. A wide variety of conditioning regimens have been used. TBI was a standard component until the mid-1990s. AML and MDS are known risks following chemotherapy, radiotherapy and transplant. Cases of sAML/MDS following autologous SCT have ranged from 4–15%. Various patient- and treatment-specific factors have been shown to increase that risk, such as specific chemotherapy drugs, number of pre-auto SCT regimens, TBI vs non-TBI containing conditioning regimens, and prior cytogenetic abnormalities. The development of sAML/MDS leads to poor prognosis. M&M: All patients who received their first autologous SCT between 1985–2003 for HD or NHL who survived and/or had follow-up data for at least 17 months post-transplant at UNMC were reviewed. Patients who developed sAML/MDS following SCT were assessed and its incidence computed. Risk factors at the time of auto-SCT were evaluated for their association with the development of sAML/MDS and include: age, sex, race, HD vs NHL, interval time from diagnosis to transplant, disease stage, number of prior chemotherapy regimens, chemosensitivity, bone marrow involvement, extranodal involvement, LDH levels, graft type, year of transplant, and conditioning regimen- TBI vs non-TBI.
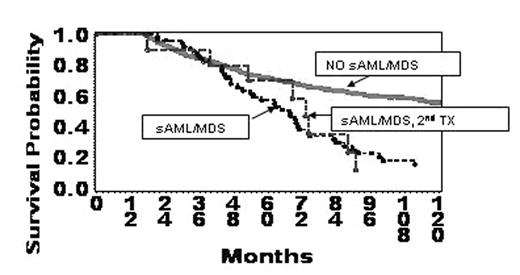
Results: 910 patients were eligible for review. Sixty-two cases of sAML/MDS were identified. The incidence rate was 6.9% at 5 years. Mean time to develop sAML/MDS post-SCT was 52 months (range 12–168). The following factors were associated with increased risk based on univariate analysis: older age (49 vs 43, p=0.003), longer interval from diagnosis to transplant (27 vs. 20 mos, p=0.03), TBI vs non-TBI based conditioning regimens (p<0.001), and number of regimens pre-transplant (<3 vs. ≥3, p<0.001). Overall survival at 8 years post-SCT was better for those without versus those with sAML/MDS (60 vs. 21%, p<0.001). A small number of patients (n=9 allo, n=1 auto) received second transplants during their disease course and showed a modest early survival advantage (within 1 year post-2nd SCT) than those who did not have second transplants
Conclusions: In the absence of a prospective cohort study it appears that elimination of TBI from auto-SCT conditioning regimens at UNMC has decreased the risk of sAML/MDS as shown by fewer occurrences after the mid-1990s and in those who did not receive TBI in comparison to those who did. In addition, fewer chemotherapeutic regimens pre-transplant, shorter interval from diagnosis to transplant, and younger age at the time of transplant have lesser risk for development of sAML/MDS. Perhaps these variables, as well as others not yet identified, can be manipulated to further decrease the risk. Donor SCT following autoSCT for sAML/MDS or relapsed disease warrants further investigation.
Author notes
Corresponding author