Abstract
Beginning in 1985, patients in British Columbia with Hodgkin lymphoma (HL) that was not controlled by conventional chemotherapy routinely underwent high-dose chemotherapy and autologous stem cell transplantation (HD-ASCT). Long-term complications of HD-ASCT have become apparent as more patients survive without recurrence of HL. Data were obtained retrospectively on the first 100 patients that underwent HD-ASCT for HL in Vancouver, focusing on relapse, treatment-related complications, and the occurrence of late events. Fifty-three patients remain alive (median follow-up, 11.4 years [range, 10.0-17.4 years]) with an overall survival (OAS) of 54% at 15 years. OAS was significantly better in patients in first relapse (67%) than in patients with primary refractory-induction failure (39%) and advanced disease (29%) (P = .002). The major cause of death was progression of HL (32% at 15 years). Treatment-related mortality, including death from second malignancy, was 17% at 15 years. Cumulative risk of a second malignancy was 9% at 15 years. Karnofsky performance status was at least 90% in 47 patients although hypogonadism (20 patients), hypothyroidism (12 patients), unusual infections (10 patients), anxiety or depression (7 patients), and cardiac disease (5 patients) were not uncommon in survivors. HD-ASCT can lead to durable remissions in relapsed or refractory HL with acceptable but definite late toxicity. The occurrence of late events necessitates lifelong medical surveillance. (Blood. 2005;106:1473-1478)
Introduction
High-dose chemotherapy followed by autologous stem cell transplantation (HD-ASCT) is now the accepted therapy for most patients with Hodgkin lymphoma (HL) that is not controlled by conventional multiagent chemotherapy and can result in long-term progression-free survival (PFS) in a significant proportion of patients.1-11 Patients with HL successfully treated with conventional therapy are at greater risk of cardiovascular, pulmonary, and endocrine dysfunction; may be unusually susceptible to infection; and appear to have an increased incidence of second malignancy.12-16 Less is known about the incidence of late complications in survivors of HD-ASCT for HL. Beginning in 1985, patients with HL at our institution who either failed to enter complete remission or progressed after multiagent chemotherapy were routinely referred for HD-ASCT. To determine prognostic factors for a successful outcome and to better define long-term complications, data were collected and analyzed on the first 100 patients who underwent HD-ASCT for HL in Vancouver.
Patients and methods
Patient characteristics
Between March 1985 and June 1992, 100 patients with HL were enrolled on a HD-ASCT protocol approved by the Institutional Review Boards of the British Columbia Cancer Agency, Vancouver General Hospital, and the University of British Columbia. All patients provided written informed consent. Patient characteristics for the entire group are shown in Table 1. All patients in this study have previously been included in one or more published reports from our center.8,9,17 To be eligible for HD-ASCT, patients had to have either failed to enter a complete remission or progressed after conventional multiagent chemotherapy. Patients with localized nodal recurrences considered potentially curable with extended field radiotherapy were specifically excluded from enrolment.18 To proceed to HD-ASCT, patients had to be aged 60 years or younger and had to have adequate cardiac, pulmonary, hepatic, and renal function.
Conventional cytoreduction prior to HD-ASCT
Patients that had not received conventional chemotherapy during the previous 3 months were routinely given 2 cycles of MVPP (mechlorethamine, vinblastine, procarbazine, and prednisone)19 to allow time to arrange for a bed on the transplantation unit. Those who had received more recent chemotherapy and in whom systemic disease was not rapidly progressing proceeded directly to HD-ASCT. In addition, all patients with bulky disease (nodal masses greater than 5 cm or mediastinal disease greater than one third of the transthoracic diameter) or disease easily encompassed within a single, previously untreated field received local radiotherapy prior to HD-ASCT.
Disease status
Disease status was determined at protocol entry, not at the time of HD-ASCT. Patients were not formally restaged after conventional cytoreductive therapy, and all patients enrolled went on to HD-ASCT. Patients in first relapse (REL1) were distinguished from primary refractory or induction failure (IF) patients by the requirement for a period of at least 3 months without disease progression following completion of first-line chemotherapy. To proceed to HD-ASCT, patients with IF were required to have persistent or progressive HL after primary chemotherapy as determined by either a tissue biopsy or unequivocal diagnostic imaging. Patients in second or subsequent relapse were grouped together as having advanced disease (AD). Characteristics specific to patients in REL1 are shown in Table 2.
Conditioning and supportive care
The first 29 patients received high-dose intravenous cyclophosphamide 1.8 g/m2, carmustine 0.6 g/m2, and etoposide 2.4 g/m2 (CBV). Beginning in January 1988, this regimen was modified, and the final 71 patients received CBVP (CBV with a reduced dose of carmustine [0.5 g/m2] plus cisplatin 150 mg/m2) as previously described.20 Supportive care was standardized but did vary over time according to institutional policy.8,9,17,20 After HD-ASCT, all patients were advised to have an influenza vaccination annually, a pneumococcal vaccination every 5 years, and a diphtheria-tetanus vaccination every 10 years.
Stem-cell transplantation
Most patients received unmanipulated, cryopreserved autologous bone marrow (n = 91). Patients who had active marrow involvement with HL initially underwent “steady-state” blood stem-cell collections (ie, without growth factor mobilization) (n = 3). Beginning in November 1990, patients with either bone marrow involvement with HL or primary refractory HL (n = 6) received intravenous cyclophosphamide (7 g/m2) and recombinant human granulocyte-macrophage colony-stimulating factor (Sargramostim; Immunex, Seattle, WA) to facilitate blood stem-cell collections. One patient with primary refractory disease had inadequate blood stem-cell collections and also required bone marrow harvesting. The median nucleated cell count of the infused product was 3.47 × 108/kg (range, 0.9-11.6 × 108/kg).
Data collection
The date of HD-ASCT was considered day 0, and follow-up was to the date of last medical examination. Standard follow-up consisted of complete blood counts, serum creatinine, alkaline phosphatase, bilirubin, and thyroid-stimulating hormone (TSH); physical examination and chest radiograph; and additional imaging studies as warranted by symptoms. Determination of remission status and cause of death and monitoring for the occurrence of a second malignancy or other late complication was performed by reviewing charts, medical correspondence, death certificates, and autopsy information, when available. Most survivors were still being seen annually by their physician, but, if medical follow-up was lacking, the patient was contacted and asked to answer a standardized health questionnaire. All 53 survivors were located, and detailed medical information was available on 49 patients. Extensive documentation was found on the terminal care of many of the deceased, including autopsy reports on 10 patients. Cause of death was verified with the responsible physician and classified as progressive HL (including death from treatment for recurrent HL after HD-ASCT), treatment-related mortality (TRM) (including organ failure or second malignancy, even if not clearly attributable to HD-ASCT), or accidental. The occurrence of second malignancies was independently verified by cross-linkage with the separately maintained BC Cancer Registry. Karnofsky performance status (KPS) and ability to return to normal activity levels (at work, school, and/or home) were determined for all survivors.
Statistical analysis
Survival analyses were performed according to the method of Kaplan and Meier21 and compared using the log-rank test. Overall survival (OAS) was calculated from the date of HD-ASCT to the date of death from any cause or until the date of last known follow-up. PFS was calculated from the date of HD-ASCT to the date of death or to the date of progression or relapse of HL. The only accidental death (without evidence of progression of HL) was censored in the survival analyses at the time of death. To account for competing risks, a cumulative incidence function22 was used to estimate the actuarial risk of TRM, relapse, and second malignancy. The following were evaluated as potential prognostic factors for PFS (at initial diagnosis and/or prior to HD-ASCT): age; sex; histology; stage; presence of bulk disease or extranodal disease; B symptoms; duration of first complete remission (CR1); hemoglobin level; serum lactate dehydrogenase level; disease status (REL1, IF, or AD); KPS; radiotherapy (any versus none; peritransplantation versus none; mediastinal versus other); number of drugs in the primary chemotherapy regimen (4-5 versus 7-8); number of prior regimens of chemotherapy, excluding MVPP cytoreduction (1 versus ≥ 2); use of chemotherapy cytoreduction (MVPP) prior to HD-ASCT; conditioning regimen used (CBV versus CBVP); and stem cell source (bone marrow versus peripheral blood). Univariate and multivariate analyses were performed using a Cox proportional hazards technique.23
Results
Outcome
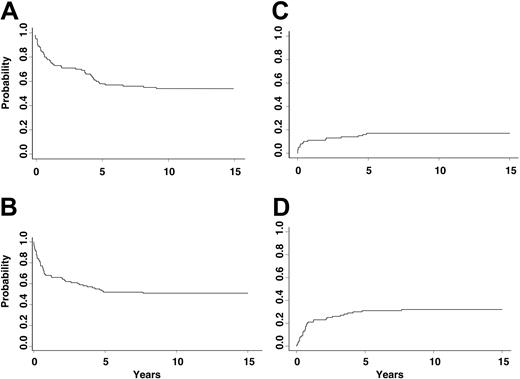
Fifty-three patients are alive without evidence of HL with a median follow-up of 11.4 years (range, 10.0-17.4 years); 49 of these patients have been in a continuous CR since the time of HD-ASCT. Eighteen patients died of TRM, and 1 patient died in an accident while in complete remission 4 years after HD-ASCT. Thirty-two patients developed evidence of progressive HL, and 28 patients died as a result. The actuarial probabilities of OAS, PFS, TRM, and relapse at 15 years are 54% (confidence interval [CI], 44%-63%), 51% (CI, 41%-60%), 17% (CI, 10%-25%) and 32% (CI, 23%-41%), respectively (Figure 1). OAS was superior for patients in REL1 (67% [CI, 53%-77%]) compared with patients with IF (39% [CI, 20%-58%]) and patients with AD (29% [CI, 11%-51%]) (P = .002). Similarly, PFS was better for patients in REL1 (62% [CI, 48%-73%]) compared with patients with IF (39% [20%-58%]) and patients with AD (29% [CI, 11%-51%]) (P = .016). For these subgroups, the actuarial risks of TRM were 12%, 13%, and 41%, respectively (P = .008), and the actuarial risks of relapse were 27%, 48%, and 29%, respectively (P = .16).
Outcome after autologous stem cell transplantation for Hodgkin lymphoma. (A) Overall survival. (B) Progression-free survival. (C) Cumulative incidence of treatment-related mortality. (D) Cumulative incidence of relapse.
Outcome after autologous stem cell transplantation for Hodgkin lymphoma. (A) Overall survival. (B) Progression-free survival. (C) Cumulative incidence of treatment-related mortality. (D) Cumulative incidence of relapse.
Performance status
Most survivors (47 patients, 89%) have a KPS of at least 90% and have been able to return to normal activity levels. However, 4 patients remain on full disability, and 1 patient is on partial disability.
Treatment-related mortality
Deaths attributable to TRM included 8 deaths prior to day +100 (pulmonary toxicity in 3 patients, cardiac toxicity in 3 patients, and sepsis in 2 patients), 6 deaths (between day +133 and day +1567) from delayed lung toxicity, and 4 deaths from second malignancies.
Progression of HL after HD-ASCT
Progression of HL was detected in 32 patients at a median of 7.9 months (range, 0.1-7.7 years) after HD-ASCT. Progression occurred during the first 2 years in 22 (69%) of these patients; however, 3 patients relapsed more than 4 years following HD-ASCT (4.1, 4.8, and 7.7 years). The majority of patients with progression of HL received palliative chemotherapy-radiotherapy after which median survival was 7.3 months (range, 0.1-72.0 months). Four patients with localized recurrences after HD-ASCT in sites not previously irradiated have been in a continuous CR of more than 10 years following salvage radiotherapy.
Prognostic factors for PFS
Univariate analysis using the entire cohort identified number of prior chemotherapy regimens (1 versus ≥ 2) (P < .001) and disease status at HD-ASCT (P = .02) as predictive of PFS (Table 3). In multivariate analysis, more than one prior chemotherapy regimen was the only independent risk factor (P < .001). Since disease status was significant in univariate analysis, a subset analysis was performed on patients in REL1. Univariate analysis in this subgroup demonstrated that more than one prior chemotherapy regimen (P = .006), extranodal disease at relapse (P = .005), use of blood stem cells (P = .04), and B symptoms at relapse (P = .04) were all risk factors for inferior PFS. The corresponding multivariate model confirmed that more than one prior chemotherapy regimen (P = .004) and extranodal disease at relapse (P = .009) were independent risk factors (Table 3).
Second malignancy
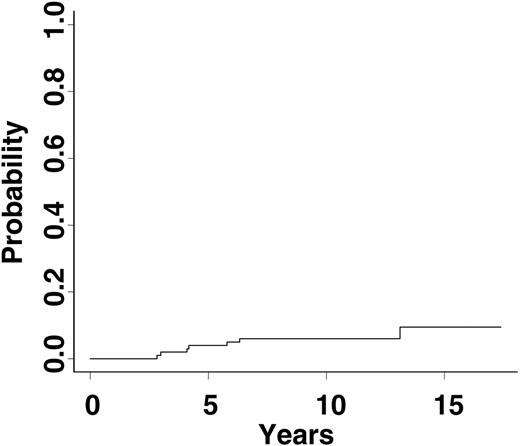
Seven patients developed second malignancies (myelodysplastic syndrome [MDS] and/or acute myeloid leukemia [AML], 2 patients; glioblastoma, renal cell carcinoma (Ca), colorectal Ca, breast Ca, and non-Hodgkin lymphoma (NHL), 1 patient each], and 1 patient developed a third malignancy (MDS). The median time to development of a second cancer was 4.2 years (range, 2.8-13.1 years) with a 15-year cumulative risk of 9% (CI, 3%-20%) (Figure 2). Four patients died of complications of the second malignancy (1 patient at 16.8 years after ASCT), 1 succumbed to progressive HL, 1 remains on treatment for breast cancer, and 1 is malignancy free 6 years after completing chemotherapy for NHL.
Infectious complications
Eighteen survivors (34%) developed dermatomal (n = 15) or disseminated (n = 3) varicella zoster virus infections at a median of 6 months (range, 0.3-127 months) after HD-ASCT. Six patients became infected with a transfusion-associated virus (hepatitis C, n = 4; hepatitis B and human T-cell leukemia virus type I, n = 1 for each). Ten patients reported the occurrence of unusual cutaneous and/or respiratory infections more than 5 years following HD-ASCT, including Staphylococcus aureus and Aspergillus pneumonia, streptococcal necrotizing fasciitis, and bacterial endocarditis. Only one of these patients had previously undergone a splenectomy; 6 other splenectomized patients had no history of late infectious complications.
Cardiac problems
Three patients had acute myocardial infarctions (MIs) 4, 7, and 11 years after HD-ASCT. Ages at the time of MI were 43, 44, and 46 years, and all 3 patients subsequently had normal coronary angiograms. Two other patients developed cardiac complications (dysrhythmia and aortic stenosis). Four of the 5 patients with cardiac complications had received mediastinal radiation for HL.
Endocrine deficiencies
Of the surviving patients, 20 (38%) were on hormone replacement therapy for hypogonadism (women, n = 18; men, n = 2). However, 5 women who underwent HD-ASCT at age 18 to 27 years, successfully conceived and delivered a total of 10 healthy children. None of the men reported fathering children after HD-ASCT. Twelve patients (23%) were on thyroid replacement, and all had received prior neck irradiation. Three patients experienced avascular necrosis of the femoral head, with 2 requiring total hip replacement, and a fourth patient was placed on a bisphosphonate for osteoporosis after having a wrist fracture.
Cumulative risk of second malignancy following high-dose chemotherapy and autologous stem cell transplantation for Hodgkin lymphoma.
Cumulative risk of second malignancy following high-dose chemotherapy and autologous stem cell transplantation for Hodgkin lymphoma.
Other complications
Two patients reported long-standing and debilitating lymphedema in the lower extremities from prior lymph node biopsy or pelvic irradiation. Seven patients reported significant anxiety or depression within the previous 5 years, and 4 patients had developed a substance abuse disorder.
Discussion
This report involves a minimum 10-year follow-up of a large single institution cohort of patients with primary refractory or relapsed HL who underwent HD-ASCT. The study findings indicate that HD-ASCT can lead to durable remissions and that the vast majority of survivors have a satisfactory performance status. The early TRM (prior to day +100) of 8% is consistent with what was commonly observed at transplantation centers more than a decade ago. With better patient selection, improved supportive care, and the introduction of blood stem cells, the early TRM associated with HD-ASCT has decreased to less than 5%.2,3,24,25 With this in mind, the remaining limitations of HD-ASCT for HL are disease recurrence and late complications.
A 15-year OAS of 67% and PFS of 62% for patients in REL1 has been demonstrated in our study cohort. This result is particularly gratifying, because it was unlikely to have been influenced by patient selection. The treatment approach was applied in a standard fashion for all patients in British Columbia during the time period of the study, and chemosensitivity was not a prerequisite for proceeding to HD-ASCT. It should also be noted that patients expected to have a favorable outcome with salvage radiotherapy alone were excluded from the study.18,26
A previous analysis indicated that CR1 duration of fewer than 12 months, B symptoms, or extranodal disease at relapse were all independent predictors of decreased PFS for patients in REL1.2 The current univariate analysis confirmed the significance of the latter 2 factors, but, in multivariate analysis, extranodal disease at relapse and number of prior chemotherapy regimens were the only independent risk factors identified. Since our results demonstrate that disease status and number of prior chemotherapy regimens are predictive of outcome, early consideration of HD-ASCT should optimize PFS for patients with HL failing conventional chemotherapy.
The 15-year PFS of 39% for patients with primary refractory HL after HD-ASCT is consistent with results reported by other groups.4,5 While these patients have an increased risk of relapse following HD-ASCT compared with patients in REL1, the highest risk period for disease progression is early, and survival is well maintained beyond the first year.
In our experience, relapse was the primary contributor to an unsuccessful outcome after HD-ASCT and can occur up to 8 years after HD-ASCT, as has previously been described.27 Patients that relapse after HD-ASCT are usually treated palliatively, but note that 4 of our patients with a localized recurrence became long-term survivors following limited radiotherapy. This finding would suggest that some patients with HL resistant to HD-ASCT may show selective radiosensitivity and that localized relapses in an area not previously irradiated may still be treated with curative intent.
The most common cause of death in our patient cohort, aside from progression of HL, was pulmonary toxicity. Interstitial pneumonitis after HD-ASCT appears to be related to the use of either high-dose carmustine (BCNU) or total body irradiation (TBI) in the conditioning regimen.8,9,19,20 During the study period, the CBV regimen was modified by the addition of cisplatin (CBVP) and reduction in the BCNU dose from 600 mg/m2 to 500 mg/m2. These modifications did result in less mucosal and hepatic toxicity but did not reduce the incidence of pulmonary toxicity (24% versus 21%; P = .98). Furthermore, the treatment-related mortality (26% verus 23%; P = .40) and the risk of relapse (43% versus 36%; P = .62) were not significantly different between the 2 conditioning regimens.20 However, in recent years, the management of patients with suspected BCNU lung toxicity at our center has become more aggressive, with prompt institution of high-dose corticosteroids at the first sign of dyspnea.
With the decline in early TRM, greater interest has focused on late complications of HD-ASCT. Unfortunately, few studies have adequate long-term follow-up to address this issue in patients with HL, but HD-ASCT survivors may be at risk for second malignancies.28-31 French registry data were used to compare the incidence of second malignancy in patients with HL treated with HD-ASCT with a conventionally treated cohort.32 The actuarial risk of developing any second cancer at 5 years was 8.9% after HD-ASCT, with the incidence of solid tumors being significantly higher than after conventional therapy (relative risk [RR], 5.19, P = .001). The incidence of MDS/AML was similar in both patient cohorts, suggesting that this disorder may result from exposure to alkylating agents prior to HD-ASCT. In contrast to the French data, a recent comparative analysis done at our institution concluded that the risk of any second malignancy in patients with HL having had HD-ASCT is the same as that observed in a large cohort of patients treated with conventional chemotherapy alone.33
Although our study attempted to identify late adverse effects attributable to the HD-ASCT protocol, it did not involve prospective, systematic evaluation of major organ function. It is quite likely that our retrospective analysis underestimated the incidence of long-term complications following HD-ASCT. Many of the long-term complications seen in our study (cardiac and pulmonary disease, late infections, endocrine dysfunction, avascular necrosis, and psychological problems) have previously been described following conventional treatment for HL.12-16,34-36
Mediastinal irradiation is thought to be responsible for damage to the coronary arteries and other structures of the heart that has been seen in conventionally treated patients with HL,35 and mortality from heart disease in this patient population is exceeded only by mortality resulting from a progression of HL or the development of a second neoplasm.12-16 Four of the 5 patients in our cohort with long-term cardiac sequelae had received mediastinal irradiation. Hypothyroidism is uncommon in patients with HL not having received neck irradiation, which is known to increase the 20-year risk to 30% to 50%.36 All of the patients on thyroid replacement in our study had received neck irradiation, and it seems unlikely that the HD-ASCT was responsible for this complication. While the HD-ASCT may have contributed to its development, gonadal dysfunction is almost universal in men treated with MOPP (mechlorethamine, vincristine, procarbazine, and prednisone) or MVPP, and half the women similarly treated will have persistent amenorrhea. Avascular necrosis is a well-known complication of high-dose glucocorticoid therapy, implicating MOPP and/or MVPP as the probable cause of the 3 cases observed in our analysis.
Unusual and/or recurrent infections occurring more than 5 years after HD-ASCT were reported by 10% of our survivors. Serious late infections, although rare, do occur after HD-ASCT and, even after conventional chemotherapy,37 immunoreconstitution can be delayed in patients with HL. Although 7 patients had previously undergone splenectomy during initial disease staging, this did not appear to contribute to the development of late infections. As recommended to our patients, a regular immunization schedule may be useful in protecting survivors from common community-acquired pathogens and should be incorporated into long-term care of all patients with HL, including those who have undergone HD-ASCT.
Although most HD-ASCT survivors in the current study were leading a normal life at the time of their last medical evaluation, long-lasting psychological problems were observed. This is not unexpected in light of the physical and emotional trauma associated with developing cancer, receiving chemoradiotherapy, and coping with the fear of relapse.38,39 Preservation of fertility is an important issue for young patients with HL, and we were able to confirm that young women treated with non-TBI-conditioning regimens, particularly those undergoing HD-ASCT prior to age 30 years, may still be able to conceive following HD-ASCT.24
In conclusion, it is now clear that, with HL, HD-ASCT leads to a durable remission in the majority of patients and that most survivors have an excellent performance status. However, with longer follow-up, late relapses are seen, and second malignancies and infectious, cardiac, endocrine, and psychological complications do occur in a significant proportion of patients. Reporting late complications after HD-ASCT is important to ensure awareness in physicians and patients so that clinical follow-up can be maintained and appropriate screening and intervention programs devised.
Prepublished online as Blood First Edition Paper, May 3, 2005; DOI 10.1182/blood-2004-12-4689.
Presented in abstract form at the 45th annual meeting of the American Society of Hematology, San Diego, CA, December 2003.33
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We acknowledge the contribution of the medical and nursing staff of Leukemia/BMT Ward T15A, BMT Daycare at the Vancouver General Hospital, and 6 West Ward at the British Columbia Cancer Agency as well as the physicians of British Columbia for patient referral and assistance with long-term follow-up. We also thank Janet Nitta for data assistance, Alan Le for statistical support, and Shawna Moore for help with manuscript preparation.