Comment on Koptyra et al, page 319
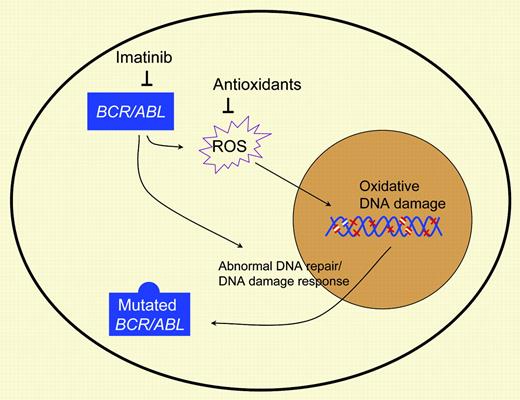
BCR/ABL-induced reactive oxygen species promote self-mutation of the BCR/ABL kinase and resistance to imatinib treatment. Administration of antioxidants could decrease BCR/ABL self-mutagenesis and the emergence of imatinib resistance.
Imatinib mesylate, a potent inhibitor of the BCR/ABL tyrosine kinase that is responsible for transformation of a primitive hematopoietic cell in chronic myeloid leukemia (CML), represents a remarkable success in efforts to develop treatments that target key molecular mechanisms of cell transformation in cancer. Imatinib effectively inhibits leukemia-cell growth and restores normal hematopoiesis in the majority of CML patients. Moreover, remissions have been sustained in the majority of the patients thus far, and imatinib has established itself as the frontline treatment for CML. However, the drug fails to eliminate all leukemia cells. Primitive leukemia stem cells, in particular, demonstrate relative resistance to imatinib and remain a potential source of leukemia relapse, which is seen on discontinuation of the drug or through outgrowth of drug-resistant cells.
The most common mechanism of imatinib resistance is through mutations in the BCR/ABL kinase domain resulting in reduced imatinib binding and kinase inhibition. Why are CML cells prone to develop mutations in the BCR/ABL kinase domain? Genetic instability appears to be an inherent feature of CML cells contributing to disease progression to accelerated phase and blast crisis. Koptyra and colleagues report that BCR/ABL kinase activity stimulates reactive oxygen species (ROS), causing oxidative damage to DNA and enhancing acquisition of kinase domain mutations associated with imatinib resistance (see figure). Inhibition of ROS using antioxidants decreased the mutagenesis rate and the frequency of imatinib resistance, an effect that was enhanced by simultaneous administration of imatinib and an antioxidant (see figure). Although BCR/ABL expression has been recognized to result in increased ROS activity for several years, the biologic significance of this observation has been controversial. The results reported by Koptyra and colleagues indicate a role for ROS-mediated DNA damage in predilection for BCR/ABL self-mutagenesis and acquisition of imatinib resistance. Clearly, other factors are also likely to contribute to enhanced mutation acquisition in CML, including defects in DNA repair and the cellular response to DNA damage in BCR/ABL-expressing cells reported by this group and others.
BCR/ABL-induced ROS promotes oxidative DNA damage, which, in combination with impaired DNA damage response, enhances acquisition of BCR/ABL kinase mutations. Kinase inhibitors and antioxidants may reduce mutation acquisition.
BCR/ABL-induced ROS promotes oxidative DNA damage, which, in combination with impaired DNA damage response, enhances acquisition of BCR/ABL kinase mutations. Kinase inhibitors and antioxidants may reduce mutation acquisition.
There is obvious clinical interest in the development of strategies to prevent emergence of drug resistance in patients receiving imatinib. Koptyra and colleagues suggest that inhibition of ROS could potentially diminish mutagenesis and emergence of imatinib resistance. This is supported by experimental data that inhibition of ROS in mice harboring BCR/ABL-expressing cell lines reduced generation of imatinib-resistant cells. This is an interesting idea that bears further study particularly in the context of primary leukemia cells. Alternative approaches to reduce emergence of drug resistance include the use of combinations of imatinib with other tyrosine kinase inhibitors with different kinase-binding properties or with other signaling inhibitors. There is evidence that the BCR/ABL kinase may be overexpressed and possibly not effectively inhibited by imatinib in leukemia stem cells, which could remain at risk for acquisition of kinase mutations and emergence of resistance over time. Studies evaluating the effects of imatinib, second-generation kinase inhibitors, and antioxidant treatments on genetic instability in these cells will be of considerable interest. ▪