Abstract
Purpose: To analyse hematopoietic engraftment after allogeneic stem cell transplantation (SCT) in patients with chronic lymphocytic leukemia (CLL) who had received Campath prior to SCT.
Patients and Methods: 40 patients with relapsed CLL were included into the analysis. All patients received Busulphan 8 mg/kg and Fludarabine 150 mg/m2 as conditioning regimen. The first 20 patients (Bu/Flu/Cam) received a cumulative dose of 75 mg Campath on days -9 to -5 and Cyclosporine (CSA) as GVHD-prophylaxis. The second 20 patients (preCam/Bu/Flu) received a conventional treatment (3 × 30 mg weekly) with Campath prior to SCT. Transplantation was scheduled 14 days from the last dose of Campath and GVHD-prophylaxis consisted of CSA and Methotrexate. The two groups did not differ in age, median number of prior chemotherapy regimens, prior fludarabine treatment or donor type. The observation of late secondary graft failure during the first phase of the study led to the analysis of lineage-specific engraftment (CD4+T-cells, CD8+T-cells, NK-cells and Neutrophils) and of Campath levels with an ELISA at the day of transplant. Complete donor chimerism was defined as more than 95% donor-DNA in a specimen.
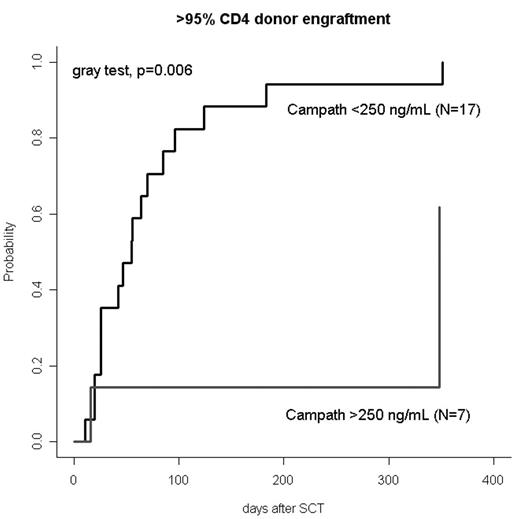
Results: Campath levels are available for 22 patients. The median antibody level was 307 ng/mL (range, 41 to 1820 ng/mL) after Bu/Flu/Cam and 62 ng/mL (detection limit to 490 ng/mL) after preCam/Bu/Flu. All patients reached neutrophil engraftment (>0.5/nl) after a median of 18 days (range, 14 to 27). The cumulative incidence of complete leukocyte chimerism at day +100 was 75% after Bu/Flu/Cam and 78% after preCam/Bu/Flu (p=0.858). The cumulative incidences of CD4+ and CD8+ T-cell donor chimerism at day +100 were 45% after Bu/Flu/Cam and 70% after preCam/Bu/Flu for both T-cell subsets (CD4+subset, p=0.481; CD8+subset, p=0.398). Of note, the Campath-level at the day of transplantation discriminated better between patients with prompt versus impaired T-cell engraftment. The incidences of complete CD4+ and CD8+ T-cell chimerism at day +100 were 14% and 29% in patients with Campath levels >250 ng/mL compared to 82% and 82% in patients with antibody levels <250 ng/mL (CD4-subset, p=0.006 (Figure 1); CD8-subset, p=0.017). Other potential factors like prior transplant, CD34-count and CD3-count of the graft or donor type did not have a significant impact on the kinetics T-cell engraftment. Of note, 3 out of 7 patients with Campath levels > 250 ng/mL compared to 0 out of 17 patients with Campath levels <250 ng/mL needed donor lymphocyte infusions to convert incomplete T-cell chimerism (p=0.017).
Conclusions: T-cell chimerism should be analysed in patients who have received Campath recent to SCT. The level of Campath at the day of transplant may be an important factor for delayed T-cell engraftment.
Disclosures: Supported by the German José Carreras Stiftung (R 03/01) and an unrestricted research grant from Schering Inc., Germany.
Author notes
Corresponding author