Abstract
Hematopoietic progenitor cell trafficking is an important phenomenon throughout life. It is thought to occur in sequential steps, similar to what has been described for mature leukocytes. Molecular actors have been identified for each step of leukocyte migration; recently, CD99 was shown to play a part during transendothelial migration. We explored the expression and role of CD99 on human hematopoietic progenitors. We demonstrate that (1) CD34+ cells express CD99, albeit with various intensities; (2) subsets of CD34+ cells with high or low levels of CD99 expression produce different numbers of erythroid, natural killer (NK), or dendritic cells in the in vitro differentiation assays; (3) the level of CD99 expression is related to the ability to differentiate toward B cells; (4) CD34+ cells that migrate through an endothelial monolayer in response to SDF-1α and SCF display the highest level of CD99 expression; (5) binding of a neutralizing antibody to CD99 partially inhibits transendothelial migration of CD34+ progenitors in an in vitro assay; and (6) binding of a neutralizing antibody to CD99 reduces homing of CD34+ progenitors xenotransplanted in NOD-SCID mice. We conclude that expression of CD99 on human CD34+ progenitors has functional significance and that CD99 may be involved in transendothelial migration of progenitors.
Introduction
Hematopoiesis is a tightly regulated process during which mature and functional cells that belong to different lineages are continuously renewed through differentiation from a small pool of ancestral cells termed “stem cells.” Throughout adult life, low numbers of stem and progenitor cells circulate in the peripheral blood. Myeloablative chemotherapy or administration of hematopoietic growth factors lead to transient increases in the number of circulating stem cells to therapeutically useful values allowing collection with apheresis procedures, a process termed “mobilization.” On the other hand, these cells have the property to engraft to the bone marrow (BM) and to fully reconstitute the hematopoietic system, a process referred to as “homing.” Thus, mechanisms controlling stem cell motility (migration, homing, retention, and release) play a critical role in the regulation of hematopoiesis.
Although the migration of leukocytes to the inflammatory sites is well documented, the different factors controlling the migration of hematopoietic stem cells are still poorly understood. Studies have provided evidence that the chemokine stromal cell-derived factor-1α (SDF-1α; CXCL12) and its receptor CXCR4 are involved in the control of the migration of hematopoietic stem cells.1-5 Mice with gene inactivation at the CXCR4 or SDF-1α loci die shortly after birth, with severe defects in stem cell trafficking and failure to establish hematopoiesis to the BM.6-9 However, CXCR4-/- fetal liver cells can successfully engraft in the BM of wild-type mice.10,11 These results suggest that human hematopoietic stem cell trafficking is only partially dependent on the SDF-1α/CXCR4 interactions and that other molecular mediators exist.
Hematopoietic stem cell trafficking involves interactions with BM endothelial cells that line vessels and marrow sinusoids. Transmigration of hematopoietic progenitors through BM endothelium is thought to occur in sequential steps, similar to what has been described for leukocytes migrating to the inflammatory sites.12 The initial tethering and rolling steps mediated by selectins and their ligands result in the slowdown of hematopoietic cells that escape the bloodstream. Tight adhesion is mostly mediated by β integrins and immunoglobulin superfamily members.13,14 Transmigration itself is the last step, and molecular actors involved at this stage have recently begun to be identified. The complexity of this process is exemplified by the description of transcytosis as an alternative to interendothelial cell transmigration.15,16
Different molecules present at interendothelial junctions are candidates to be actors in transendothelial migration. Antibodies against some of these molecules modulate leukocyte extravasation. This is the case for CD31 (PECAM-1),17 CD99,18 Jam-A,19 and Jam-C.20 More recently, the role of CD155 (PVR), a member of the nectin family, and its ligand DNAM-1, in monocyte transmigration through human umbilical vein endothelial cells (HUVECs) has been evidenced, using either blocking monoclonal antibodies (mAbs) or soluble forms of these molecules.21,22 Among these molecules, a role in the transmigration of hematopoietic progenitors has only been documented for PECAM-1.19,20,22-25
The role of CD99 in the migration of monocytes has recently been described18 and occurs downstream of PECAM-1 blockade. CD99 is a highly O-glycosylated type I transmembrane protein of 32 kDa encoded by the MIC2 gene that has no apparent structural homology with most molecules involved in cell-to-cell interactions.26 CD99 is involved in multiple cellular events such as E-rosetting for T lymphocytes,27 T-cell adhesion,28-30 apoptosis of immature thymocytes31 and Ewing sarcoma cells in a caspase-independent way,32 up-regulation of T-cell receptor,33 and major histocompatibility complex molecules.34,35 The CD99 gene encodes 2 different proteins produced by alternative splicing,36 the short form harboring a deletion in the cytoplasmic domain. Differential expression of these 2 forms is associated with distinct behaviors for phenomena such as CD99-induced cell adhesion or T-cell death.36,37 The short CD99 isoform is a negative regulator of neural differentiation38 and is also involved in the induction of motility and invasiveness of human breast cancer cells.39
Although the expression of CD99 on hematopoietic cells, especially at the early stage of B-cell, T-cell, or neutrophil differentiation has been reported,40 little is known about CD99 expression and function in the hematopoietic progenitor compartment. Here, we investigated the expression of CD99 on human CD34+ hematopoietic progenitors and its relation to their proliferative and differentiation abilities. Further, we investigated the role of CD99 in trafficking of CD34+ cells, using an in vitro model of transendothelial migration and homing of xenotransplanted human CD34+ cells in NOD-SCID mice.
Materials and methods
Primary cells and cell lines
Following informed consent in accordance with the Declaration of Helsinki, apheresis samples were obtained from patients with poor-prognosis cancers, who underwent mobilization with recombinant human granulocyte colony-stimulating factor (rhG-CSF; Neupogen, Amgen, Thousand Oaks, CA, or Granocyte, Chugai, Paris, France), alone or in association with chemotherapy. Approval for these studies was obtained from the Institut Paoli-Calmettes institutional review board (Comite d'Orientation Strategique). Mononuclear cells were enriched by density gradient separation over Lymphoprep (d = 1.077 g/mL; AbCys, Paris, France). CD34+ and CD14+cells were immunoselected, using the magnetic-activated cell sorting (MACS) technique (Miltenyi Biotec, Bergisch-Gladbach, Germany). The average CD34+ cell content of the enriched fractions determined by fluorescence-activated cell sorting (FACS) analysis with a PE-conjugated anti-CD34 mAb was 94.7% (± 0.9%).
Cord blood (CB) samples were obtained from mothers after they provided informed consent and had normal deliveries. BM samples were obtained from healthy donors undergoing marrow collection for allogeneic transplantation, following informed consent.
The human bone marrow endothelial cell (HBMEC) line was a gift of B. Weksler (Cornell University, New York, NY). This SV-40 immortalized cell line is derived from adult human HBMECs and retains characteristics of primary cells.41 HBMECs were cultured in flasks coated with 0.2% gelatin (Sigma-Aldrich, St Louis, MO), in DMEM containing 1% glucose (Cambrex, Verviers, Belgium) supplemented with 5% (vol/vol) heat-inactivated fetal calf serum (FCS; Invitrogen, Paisley, United Kingdom), 10 mM HEPES (Invitrogen), 3 mM glutamine (Invitrogen), 1 μg/mL folate (Sigma-Aldrich), 100 U/mL penicillin, and 100 μg/mL streptomycin (Invitrogen).
Nalm6 cells and MS-5 cells were maintained in RPMI 1640 (Cambrex) or in DMEM (Cambrex), respectively, supplemented with 10% (vol/vol) heat-inactivated FCS, 100 U/mL penicillin, and 100 μg/mL streptomycin. Cells were incubated at 37°C in 5% CO2 in a humidified atmosphere.
Antibodies and reagents
Anti-CD99 mAbs clones 12E7 and O662 were a gift from A. Bernard (UMR 576 Inserm, Nice, France); the hec2 anti-CD99 mAb was a gift from W. A. Muller (Cornell University, New York, NY). Anti-CD31 (PECAM-1, clone CLB/HEC75) was purchased from Sanquin (Amsterdam, The Netherlands). Anti-CD106 (VCAM-1, clone 1G11) was purchased from Beckman Coulter (Miami, FL). The anti-CD155 mAb (PVR, clone PV.404) was previously described.42 The following mAbs and their isotypic controls were purchased from Beckman Coulter: phycoerythrin (PE)-conjugated anti-CD1a, PE-conjugated anti-CD3, fluorescein isothiocyanate (FITC)-conjugated anti-CD10, PE-conjugated anti-CD14, FITC-conjugated anti-CD16, PE-conjugated anti-CD19, PE-conjugated anti-CD33, FITC-conjugated anti-CD36, PE-cyanin 5.1 (PC5)-conjugated anti-CD34, PE- and PC5-conjugated anti-CD45, FITC-conjugated anti-CD80, FITC-conjugated anti-CD83, PE-conjugated anti-CD111 (nectin1), PE-conjugated anti-CD117 (c-Kit). Allophycocyanin (APC)-conjugated anti-CD3, PE-conjugated anti-CD34, PE-conjugated anti-CD56, PE-conjugated anti-CD71, FITC-conjugated anti-CD86, PE-conjugated anti-CDw90 (Thy1), FITC- and PE-conjugated anti-CD99, PE-conjugated anti-CD235a (glycophorin A [GPA]) were from Becton Dickinson (San Jose, CA); FITC-conjugated anti-CD105 and PE-conjugated anti-CD184 (CXCR4) were from R&D Systems (Minneapolis, MN).
SDF-1α, monocyte chemotactic protein-1 (MCP-1), IL-15, and TNF-α were purchased from R&D Systems. SCF, IL-3, and IL-6 were a gift of Amgen. Other cytokines used in this study were granulocyte-macrophage colony-stimulating factor (GM-CSF; Leucomax, Novartis, Rueil-Malmaison, France), G-CSF (Neupogen, Amgen), and erythropoietin (Epo; Eprex, Janssen-Cilag, Issy-les-Moulineaux, France).
Flow cytometry studies and cell sorting
Flow cytometry analyses were conducted with a FACSCalibur (Becton Dickinson Immunocytometry Systems [BDIS], San Jose, CA). Cells were incubated with direct-labeled antibodies for 30 minutes on ice. Isotype control antibodies were used to exclude false-positive cells. Dead cells were gated out by staining with Topro3 (Molecular Probes, Eugene, OR).
Cell sorting was performed on a FACSAria flow cytometer (BDIS). Briefly, CD34+ cells were stained with a FITC-conjugated anti-CD99 and a PC5-conjugated anti-CD34 as described and sorted into CD34+/CD99low and CD34+/CD99high, each fraction representing approximately 20% of the total CD34+ cell population.
Aldehyde dehydrogenase assay
Intracellular levels of aldehyde dehydrogenase (ALDH) in CD34+ cells were assessed by staining with Aldefluor reagent (StemCell Technologies, Vancouver, BC, Canada). ALDH substrate (0.6 μg) was added to 106 CD34+ cells suspended in 1 mL assay buffer. Then, 0.5 mL of these cells was immediately transferred to a control tube containing 5 μL 1.5 mM diethylaminobenzaldehyde (DEAB), a specific ALDH inhibitor. Cells were then incubated for 30 minutes at 37°C to allow the conversion of the ALDH substrate into a fluorescent product. Cells were then costained with PE-conjugated anti-CD99 and PC5-conjugated anti-CD34 and analyzed by flow cytometry.
RNA extraction and quantitative real-time polymerase chain reaction (RQ-PCR)
Total RNA was isolated from 5 × 105 cells using an RNA extraction kit (Macherey-Nagel, Hoerdt, France). Total RNA was denatured at 65°C for 10 minutes and reverse transcribed using Superscript II reverse transcriptase (Invitrogen).
For detection of the 2 CD99 isoforms that differ by their intracytoplasmic tail, 2 sets of previously published oligonucleotides38 were used, and real-time polymerase chain reaction (PCR) was carried out using the Light Cycler 2.0 instrument and the software version 4.0 (Roche Applied Science, Mannheim, Germany). The 20-μL reaction mixture contained 4 μL of 5 × Master Mix (Roche Applied Science), 0.5 μM of each primer, and 1 μL cDNA sample. After initial incubation at 95° for 10 minutes, 60 cycles were carried out (10 seconds at 95°C, 10 seconds at 60°C for the long form, or 1 second at 60°C for the spliced variant and the control GAPDH, and 20 seconds at 72°C). For quantification, a standard curve was obtained from serial dilutions of a cDNA control and the relative expressions of the 2 isoforms were normalized to GAPDH expression.
Differentiation assays
Clonogenic cultures. Two hundred fifty CD34+/CD99high or CD34+/CD99low cells were seeded in triplicate in 0.5 mL semisolid medium (Methocult 4230, StemCell Technologies) supplemented with rhIL-3, rhIL-6, rhGM-CSF, rhG-CSF (10 ng/mL each), rhSCF (100 ng/mL), and rhEpo (2 U/mL). Colonies were scored after 14 days of culture at 37°C, 5% CO2.43
For high proliferative potential (HPP)-colony-forming cells (HPP-CFCs) enumeration, double-layer agarose (Caltag Laboratories, Burlingame, CA) cultures supplemented with rhIL-3, rhIL-6, rhG-CSF, rhGM-CSF, rhSCF, and rhFlt3-L (20 ng/mL each) were seeded at 1000 cells/well, as previously described.44 Colonies were enumerated on day 21. HPP-CFCs were defined as progenitors giving rise to dense colonies more than 1 mm in diameter, with a dense core.
Limiting dilution analysis of cobblestone area colony-forming cells (CAFCs). Monolayers of MS-5 stromal cell line were established in 96-well plates and allowed to reach confluence. Serial dilutions of CD34+/CD99low or CD34+/CD99high cells were then seeded on the monolayers in IMDM medium supplemented with 10% FCS without any human recombinant cytokine. CAFCs were scored at week 5.45,46
Erythroid cell differentiation assay. The technique was adapted from a previously published report.47 CD34+/CD99low or CD34+/CD99high cells (104/mL) were cultured in IMDM supplemented with 20% BIT (StemCell Technologies), 900 ng/mL ferrous sulfate, and 90 ng/mL ferric nitrate (Sigma-Aldrich). From days 0 to 8, 10-6 M hydrocortisone (Sigma-Aldrich), 100 ng/mL SCF, 5 ng/mL IL-3, and 3 U/mL Epo were added to the cultures. On day 4, cultures were diluted in 4 volumes of the same medium. On day 9, cells were suspended at 3 × 105 cells/mL and cocultured on MS-5 layer in medium supplemented with Epo. Analysis of specific markers was performed at day 12.
B- and NK cell differentiation assays. Layers were established in 96-well plates with the murine stromal cell line MS-5. Then, 10 000 CD34+/CD99low or CD34+/CD99high cells were added to the layers. B-cell differentiation was assessed after 5 weeks of culture without any human recombinant cytokine in IMDM supplemented with 5% FCS and 5% human AB serum (Institut Jacques Boy, Reims, France). In separate experiments, 20 ng/mL IL-15 and 50 ng/mL SCF were added to the cultures to favor NK cell differentiation in IMDM supplemented with 15% FCS. Specific markers were analyzed after 5 weeks.
Dendritic cell differentiation assays. CD34+/CD99low or CD34+/CD99high cells (10 000/mL) were cultured in 24-well plates in RPMI 1640 medium (Cambrex) supplemented with 10% FCS, 20 ng/mL SCF, 100 ng/mL GM-CSF, 2.5 ng/mL TNF-α, and 20 ng/mL Flt3-L. At day 7, cultures were diluted in the same medium at the concentration of 5 × 105 cells/mL. Specific markers were analyzed after 14 days.
Cell cycle analyses. The percentages of cells in G0/G1, S, and G2/M phases were evaluated by staining living cells with propidium iodide. A total of 5 × 104 to 105 cells were fixed in 70% ethyl alcohol (Carlo Erba Reagenti, Milan, Italy) for 15 minutes, then treated with 200 to 300 μLof a 10-μg/mL DNase-free RNase solution (Roche Diagnostics, Indianapolis, IN) for 15 minutes at 37°C. An equal volume of a 50-μg/mL propidium iodide solution was added, and cells were incubated for 1 hour at 37°C before flow cytometry analysis.46
Detection of apoptotic cells. Apoptosis was determined by monitoring phosphatidyl serine exposure at the outer cell membrane, using an assay based on binding of annexin V-Cy5 (Molecular Probes); Sytox was used as a viability probe. Apoptosis was evaluated after 5 hours in the absence of cytokines and after 24 hours of culture in a medium supplemented with IL-3, IL-6 (10 ng/mL each), and SCF (100 ng/mL).
Adhesion assay
Thirty-thousand HBMECs were established in 96-well plates and allowed to grow to confluence for 72 hours; confluent cells were incubated for 1 hour at 37°C with the relevant blocking mAbs. Simultaneously, mobilized peripheral blood (mPB) CD34+ cells in IMDM (Cambrex) supplemented with 20% BIT (StemCell Technologies) were incubated with various mAbs at 4°C. An anti-CD34 mAb was used as control. Five to 10 × 104 mAb-treated CD34+ progenitors were cocultured with mAb-treated HBMECs for 1 hour at 37°C. Wells were then filled with culture medium, covered with a plastic film, placed upside down, and centrifuged at 50 g for 5 minutes to eliminate nonadherent cells. Adherent cells were then detached with 5 mM EDTA, incubated with an anti-CD45 mAb (to exclude HBMECs), and the addition of a known number of calcein-AM-labeled (Molecular Probes) Nalm6 cells allowed for the estimation of their number by flow cytometry.
Transendothelial migration studies
Migration assays were performed in transwell culture inserts (Costar, Cambridge, MA) of 6.5 mm diameter and 5-μm pore filters, coated with 0.2% gelatin (Sigma-Aldrich). HBMECs were plated at 30 000 cells/transwell and allowed to grow to confluence for 72 hours. Before migration assays, the monolayers were washed once with assay medium (IMDM supplemented with 20% BIT). Then, 100 000 CD34+ cells or 500 000 mononuclear cells in 0.1 mL were seeded in the upper compartment, and 0.6 mL of assay medium was added to the lower chamber. In blocking experiments, the hematopoietic and the endothelial cells were preincubated with mAbs (20 μg/mL) for 30 minutes at 37°C for the layer or at 4°C for the hematopoietic cells. The mAbs were present during the migration assay. Cells were allowed to migrate for 4 hours in response to SDF-1α (100 ng/mL) for CD34+ cells or to MCP-1 (200 ng/mL) for monocytes. In some experiments, SCF (100 ng/mL) was added to SDF-1α. Before collecting the transmigrated cells, a fixed number of control Nalm6 cells labeled with calcein-am was added to the lower compartment; cells were then collected and labeled with a PE-conjugated anti-CD45 mAb (for CD34+ cells) or a PE-conjugated anti-CD14 (for mononuclear cells) to eliminate contaminating HBMECs. After FACS analysis, the ratio between PE-labeled cells and calcein-labeled Nalm6 cells allowed us to determine the number of cells that had migrated from the upper to the lower chamber.
Homing of CD34+ progenitors in NOD-SCID animals
The model has been adapted from a previously published report.48 Briefly, NOD-SCID animals were bred in our animal facility under germ-free conditions. Following sublethal total body irradiation at 350 cGy, 2 × 106 human mPB CD34+ progenitors were injected in the tail vein after preincubation with Immu133 (anti-CD34 mAb), 12E7 (anti-CD99 mAb), or IgG1 (20 μg/mL). Animals were killed 18 to 24 hours after injection. BM cells were collected from femurs and tibias. Mononuclear cells were separated by density gradient and analyzed for the presence of human cells by using a human-specific anti-CD45 mAb; cells from nontransplanted mice were used as negative controls; human mononuclear cells were used as positive controls to establish the threshold for CD45 positivity; dead cells were excluded with Topro3 staining. Homing efficiency was determined by the percentage of CD45+ (human) cells among total number of recipient mononuclear BM cells. Only experiments in which at least 0.1% human cells were detectable in the BM of all control animals were kept for further analyses and interpretation.
Statistical analyses
Data are presented as the mean ± SEM. Differences were tested by using the nonparametric Wilcoxon signed rank test for paired observations (differentiation assays) or the Mann-Whitney test in case of independent populations (migration experiments). P values below .05 were considered significant.
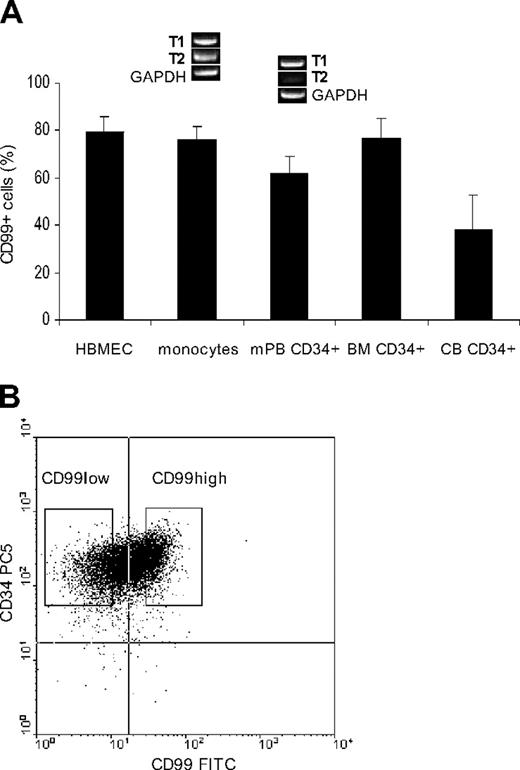
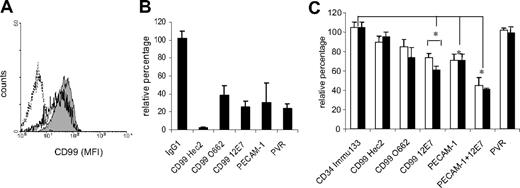
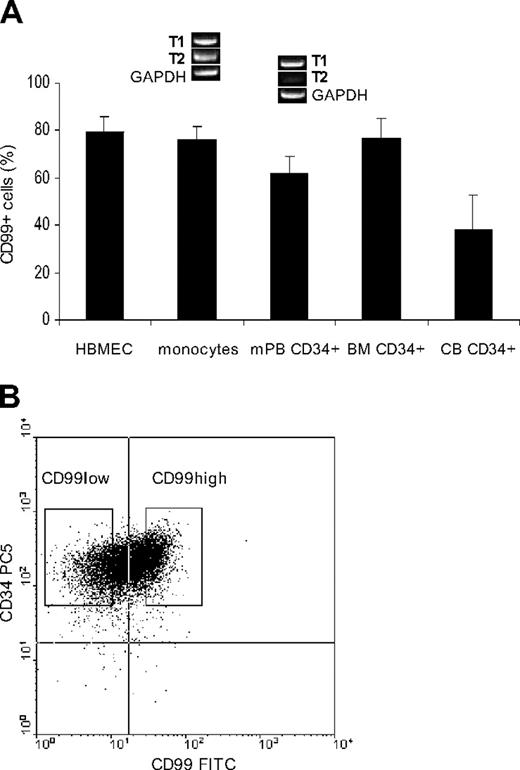
Expression of CD99. (A) Expression of CD99 on the HBMEC line, on human CD14+ mobilized peripheral blood (mPB) monocytes, and on mPB CD34+ cells (n = 14), on bone marrow CD34+ cells (BM, n = 5) and cord blood CD34+ cells (CB, n = 4). Error bars represent SEM. The detection of the 2 isoforms, T1 (the full-length form) and T2 (the truncated form), shows the relatively low level of the T2 isoform in mPB CD34+ progenitors when compared with mPB CD14+ monocytes (a representative illustration of gel electrophoresis of RQ-PCR products for CD14+ and CD34+ cells immunoselected from the same apheresis sample). (B) Representative flow cytometric detection of CD34 and CD99 expression on immunoselected CD34+ progenitors obtained from an adult patient undergoing apheresis.
Expression of CD99. (A) Expression of CD99 on the HBMEC line, on human CD14+ mobilized peripheral blood (mPB) monocytes, and on mPB CD34+ cells (n = 14), on bone marrow CD34+ cells (BM, n = 5) and cord blood CD34+ cells (CB, n = 4). Error bars represent SEM. The detection of the 2 isoforms, T1 (the full-length form) and T2 (the truncated form), shows the relatively low level of the T2 isoform in mPB CD34+ progenitors when compared with mPB CD14+ monocytes (a representative illustration of gel electrophoresis of RQ-PCR products for CD14+ and CD34+ cells immunoselected from the same apheresis sample). (B) Representative flow cytometric detection of CD34 and CD99 expression on immunoselected CD34+ progenitors obtained from an adult patient undergoing apheresis.
Results
CD99 is expressed at varying levels on CD34+ cells from different sources
Most CD34+ cells appear to express CD99, although the level of expression varies depending on cell source: 76.5% ± 8.5% (n = 5) of BM CD34+ cells express CD99, 61.9% ± 6.9% (n = 14) of adult mPB CD34+ progenitors express CD99, and 38% ± 14.5% (n = 4) of CB CD34+ cells express CD99 (n = 4; Figure 1A). As already described, CD99 is also expressed on monocytes.18 The HBMEC line expresses CD99, similar to what has been shown with HUVECs18 ; pretreatment of HBMECs with TNF-α did not change the level of CD99 expression (data not shown).
Because 2 isoforms of CD99 that differ by their intracytoplasmic tail have been described, we used RQ-PCR and specific oligonucleotides38 to study their relative expression in human monocytes and CD34+ progenitors. Figure 1A shows a representative illustration, where the short and truncated (T2) isoform expressed in monocytes is barely detectable in CD34+ cells; this result was reproduced in 7 paired experiments with monocytes and progenitors from the same individuals.
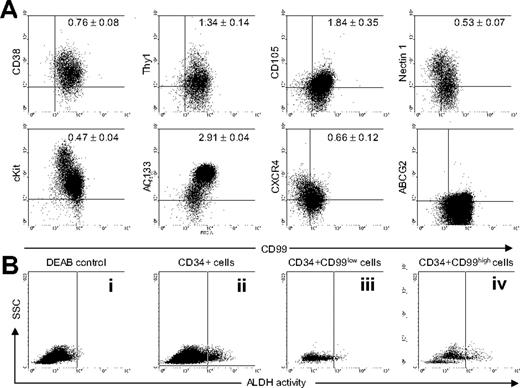
The expression pattern of CD99 within the CD34+ mPB cells does not discriminate a clearly positive population but suggests a continuum of expression (Figure 1B), the highest expression of CD99 being associated with the highest expression of CD34. In further experiments, we defined CD34+/CD99low and CD34+/CD99high cells as CD34+ cells with the lowest and highest mean fluorescence intensity (MFI) for CD99, each of these 2 subsets representing approximately 20% of the total CD34+ cell population. We next studied the relative expression of CD99 and several antigens within the CD34+ cell population. As shown in Figure 2A, the higher expression level for CD99 is associated with a lower level of expression of CD38 and nectin1, and on the other hand, with a higher level of expression of CD90 (Thy1), CD105 (a component of the TGF-β receptor), and CD133 (AC133), suggesting that the CD34+/CD99high subset is enriched with the most immature progenitors. Only rare cells appeared to be ABCG2+, an ABC transporter expressed on early hematopoietic progenitors49 ; these ABCG2+ cells expressed CD99 at higher levels than the majority of CD34+ cells. The coexpression of CD99 with c-Kit and CXCR4, the receptors of the chemoattractants SCF and SDF-1α, respectively, used in this study, indicates that c-Kit and CXCR4 expression is higher in the CD34+/CD99low subset. Finally, the Aldefluor assay demonstrated that the CD34+/CD99high cell subset possessed higher levels (4 ± 0.9-fold, n = 4) of ALDH activity than its CD34+/CD99low counterpart; a representative experiment is shown in Figure 2B.
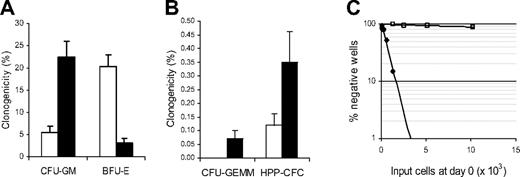
Clonogenic progenitors and CAFCs are present at different frequencies in the mPB CD34+/CD99high and CD34+/CD99low cell subsets
To further explore whether the level of CD99 expression is associated with different functional abilities within CD34+ cells, we sorted the CD34+/CD99low and CD34+/CD99high cell populations (Figure 1B).
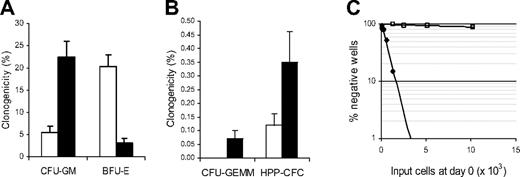
As shown in Figure 3A-B, the CD34+/CD99high subset contains the majority of granulocyte-macrophage colony-forming units (CFU-GMs) and HPP-CFCs, whereas erythroid clonogenic progenitors are mostly present in the CD34+/CD99low subset. The frequency of more immature clonogenic progenitors (granulocyte, erythrocyte, megakaryocyte, macrophage colony-forming units [CFU-GEMMs] and HPP-CFCs) is significantly higher in the CD34+/CD99high subset. Figure 3C provides an estimate of CAFC frequency in the 2 tested cell subpopulations; CAFCs are mostly present within the CD34+/CD99high subset (approximately 1/3,000 cells versus 1/50 000 for CD34+/CD99low cells).
Coexpression of different markers with CD99 within the mPB CD34+ cell subset. (A) CD99 expression levels increase simultaneously with Thy1, CD105, and AC133. Conversely, levels of CD38, nectin1 (CD111), c-Kit, and CXCR4 tend to decrease, whereas levels of CD99 increase. The rare ABCG2+ cells express high levels of CD99. For each antigen, values in the dot plots represent the ratio of MFI for this specific marker in the CD34+/CD99high population versus the CD34+/CD99low population, as defined in Figure 1B (data are mean ± SEM of 9 experiments). Due to the low percentage of ABCG2+ cells, this value was not computed for this marker. (B) A representative experiment showing detection of ALDH activity in total CD34+ cells and gated CD34+/CD99low and CD34+/CD99high cells. (i) Aldefluor-stained CD34+ cells incubated with DEAB, a specific ALDH inhibitor; (ii) total CD34+ cells incubated with Aldefluor, analysis of Aldefluor-positive cells gated on (iii) CD34+/CD99low cells and (iv) CD34+/CD99high cells.
Coexpression of different markers with CD99 within the mPB CD34+ cell subset. (A) CD99 expression levels increase simultaneously with Thy1, CD105, and AC133. Conversely, levels of CD38, nectin1 (CD111), c-Kit, and CXCR4 tend to decrease, whereas levels of CD99 increase. The rare ABCG2+ cells express high levels of CD99. For each antigen, values in the dot plots represent the ratio of MFI for this specific marker in the CD34+/CD99high population versus the CD34+/CD99low population, as defined in Figure 1B (data are mean ± SEM of 9 experiments). Due to the low percentage of ABCG2+ cells, this value was not computed for this marker. (B) A representative experiment showing detection of ALDH activity in total CD34+ cells and gated CD34+/CD99low and CD34+/CD99high cells. (i) Aldefluor-stained CD34+ cells incubated with DEAB, a specific ALDH inhibitor; (ii) total CD34+ cells incubated with Aldefluor, analysis of Aldefluor-positive cells gated on (iii) CD34+/CD99low cells and (iv) CD34+/CD99high cells.
Detection of clonogenic progenitors. (A-B) Detection of clonogenic progenitors from CD34+/CD99low (□) and CD34+/CD99high (▪) cells sorted from different apheresis samples (n = 6). (A) Detection of committed progenitors (BFU-Es and CFU-GMs). (B) Detection of immature clonogenic progenitors (CFU-GEMMs and HPP-CFCs). (A-B) Error bars represent SEM. (C) Scoring of CAFCs in limiting dilution analyses of CD34+/CD99low (□) and CD34+/CD99high (♦) cells (n = 3). Data are from a representative experiment.
Detection of clonogenic progenitors. (A-B) Detection of clonogenic progenitors from CD34+/CD99low (□) and CD34+/CD99high (▪) cells sorted from different apheresis samples (n = 6). (A) Detection of committed progenitors (BFU-Es and CFU-GMs). (B) Detection of immature clonogenic progenitors (CFU-GEMMs and HPP-CFCs). (A-B) Error bars represent SEM. (C) Scoring of CAFCs in limiting dilution analyses of CD34+/CD99low (□) and CD34+/CD99high (♦) cells (n = 3). Data are from a representative experiment.
mPB CD34+/CD99high and CD34+/CD99low cells respond differently to cytokine combinations that induce erythroid, NK, B, or dendritic cell differentiation in the in vitro cultures
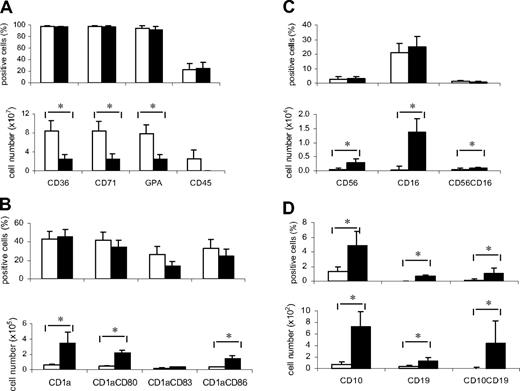
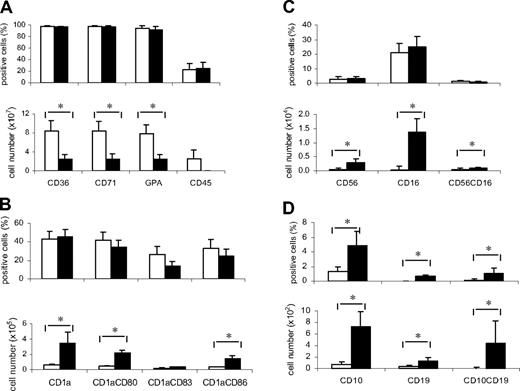
In 3 of the 4 tested differentiation conditions, CD34+/CD99high and CD34+/CD99low cells differed only by their expansion ability; differentiated cells shared a similar phenotype. When cultured with cytokine conditions that favor erythroid differentiation, CD34+/CD99low cells produced higher numbers of CD36+, CD71+, or GPA+ cells than their CD34+/CD99high counterparts (Figure 4A). Conversely, CD34+/CD99high cells expanded to a higher degree toward the NK and dendritic lineages as indicated by the increased number of cells expressing CD16 and CD56 (NK lineage, Figure 4B), or CD1a, CD80, CD83, and CD86 (dendritic lineage, Figure 4C), leading to a greater output of differentiated cells. By contrast, coculture with the MS-5 cell line demonstrated that B-cell progenitors were mostly present in the CD34+/CD99high cell subset, suggesting a difference in differentiation potential in addition to different proliferative abilities (Figure 4D).
These differences cannot be accounted for by a difference in cell cycling activity; both cell subsets had low and comparable percentages of cells in G2/M phase, immediately after cell sorting (0.6% ± 0.09%; n = 4).
Response to cytokine combinations that induce cell differentiation. CD34+/CD99low (□) and CD34+/CD99high (▪) cells were induced to differentiate in different culture conditions. Specific markers were analyzed for each differentiation assay. Results are expressed as the percentage of positive cells for each marker (top panels) and as the absolute number of cells expressing these markers (bottom panels). Analyses were performed at 12 days of culture for erythroid conditions (A), 15 days for dendritic conditions (B), and 5 weeks for NK (C) and B-cell differentiation (D). Data are mean ± SEM of 6 experiments for each differentiation assay. *P < .05.
Response to cytokine combinations that induce cell differentiation. CD34+/CD99low (□) and CD34+/CD99high (▪) cells were induced to differentiate in different culture conditions. Specific markers were analyzed for each differentiation assay. Results are expressed as the percentage of positive cells for each marker (top panels) and as the absolute number of cells expressing these markers (bottom panels). Analyses were performed at 12 days of culture for erythroid conditions (A), 15 days for dendritic conditions (B), and 5 weeks for NK (C) and B-cell differentiation (D). Data are mean ± SEM of 6 experiments for each differentiation assay. *P < .05.
A blocking mAb to CD99 inhibits the transmigration of human mPB CD34+ progenitors through HBMECs in response to SDF-1α with or without SCF
Before testing different anti-CD99 mAbs for their ability to interfere in hematopoietic progenitor-endothelial cell interactions, we checked whether they induced apoptosis of mPB CD34+ cells, because induction of apoptosis in T cells was described with the O662 mAb.50 Figure 5 shows that none of the 3 12E7, O662, and Hec2 mAbs induced apoptosis after 5 hours (in conditions mimicking those used for transmigration assays); the 12E7 mAb apparently protects CD34+ cells from apoptosis, because the percentage of annexin V+ cells tended to be lower than in the control conditions. After 24 hours in serum-free medium with IL-3, IL-6, and SCF, an approximately 3-fold increase in annexin V+ cells was detected when mPB CD34+ cells were exposed to the O662 mAb, whereas no increase was induced by exposure to the 12E7 or Hec2 mAb.
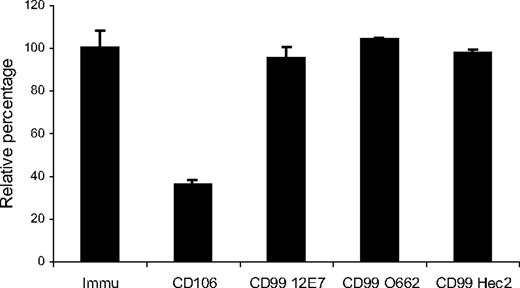
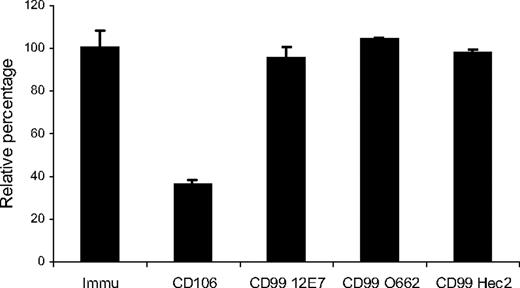
Next, we checked whether CD99 is involved in hematopoietic progenitor-endothelial cell adhesion. As expected,4,51 a blocking mAb against CD106/VCAM-1 decreased the adhesion of CD34+ cells on HBMECs by more than 60%. By contrast, treatment with a blocking mAb against CD99 did not affect the adhesion of mPB CD34+ cell to HBMECs (Figure 6; n = 3).
Induction of apoptosis by different anti-CD99 mAbs. mPB CD34+ cells were incubated with 20 μg/mL 12E7 (▪), O662 (□), and hec2 ( ). The proportion of annexin V+ cells relative to the untreated control (arbitrarily 100%) was evaluated after 5 hours in the absence of cytokines and after 24 hours of culture in a medium supplemented with IL-3, IL-6 (10 ng/mL each), and SCF (100 ng/mL). Data are mean ± SEM of 3 experiments.
). The proportion of annexin V+ cells relative to the untreated control (arbitrarily 100%) was evaluated after 5 hours in the absence of cytokines and after 24 hours of culture in a medium supplemented with IL-3, IL-6 (10 ng/mL each), and SCF (100 ng/mL). Data are mean ± SEM of 3 experiments.
Induction of apoptosis by different anti-CD99 mAbs. mPB CD34+ cells were incubated with 20 μg/mL 12E7 (▪), O662 (□), and hec2 ( ). The proportion of annexin V+ cells relative to the untreated control (arbitrarily 100%) was evaluated after 5 hours in the absence of cytokines and after 24 hours of culture in a medium supplemented with IL-3, IL-6 (10 ng/mL each), and SCF (100 ng/mL). Data are mean ± SEM of 3 experiments.
). The proportion of annexin V+ cells relative to the untreated control (arbitrarily 100%) was evaluated after 5 hours in the absence of cytokines and after 24 hours of culture in a medium supplemented with IL-3, IL-6 (10 ng/mL each), and SCF (100 ng/mL). Data are mean ± SEM of 3 experiments.
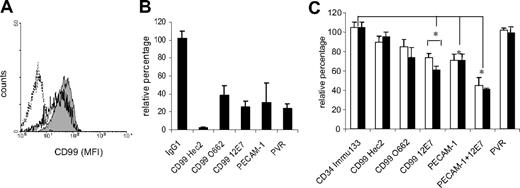
Finally, to assess whether CD99 may play a role in transendothelial migration, human mPB CD34+ progenitors were induced to migrate in vitro through a monolayer of HBMECs, in response to SDF-1α alone (100 ng/mL),24 or in response to a combination of SDF-1α and SCF (100 ng/mL). In response to SDF-1α alone, 8.6% ± 2.8% (n = 15) of the CD34+ population migrated into the lower chamber after 4 hours, whereas 11.5% ± 1.2% (n = 25) migrated in response to a combination of SDF-1α and SCF. When cells that had migrated to the lower chamber were compared with cells that had remained in the upper chamber for their phenotypes, it appears that cells that had migrated displayed higher levels of CD99 expression (a 20% ± 7% increase; n = 4; Figure 7A).
To validate our transmigration assay, experiments were run in parallel, in which monocytes and CD34+ cells were induced to migrate in response to MCP-1 or to SDF-1α with or without SCF, respectively. Several mAbs were tested for their ability to block or reduce transmigration. Figure 7B shows that monocyte transmigration through HBMECs in response to the MCP-1 chemoattractant was strongly inhibited by blocking mAb to PECAM-1, CD99 (clones 12E7, O662, and Hec2), and PVR as previously reported in the literature.17-19,22 Following incubation of CD34+ cells and HBMECs with a blocking antibody to PECAM-1, a partial inhibition of the transmigration of mPB CD34+ progenitors was observed (Figure 7C), as previously demonstrated.23,24 Conversely, incubation with Immu133, an anti-CD34 mAb, did not affect the migration of CD34+ cells, again consistently with previously published results.24 Incubation of CD34+ cells and HBMECs with 12E7 resulted in a significant decrease in the transmigration of mPB CD34+ progenitors (P < .05); in contrast, preincubation of mPB CD34+ cells with Hec2 produced no inhibition of transmigration, and a nonsignificant reduction in transmigration was observed following preincubation with O662. The inhibition of transmigration observed after blocking of CD99 with 12E7 appears to be in the same range as the inhibition observed after blocking of PECAM-1 with Hec75; a combination of 12E7 and Hec75 resulted in an additive effect and an increased inhibition of transmigration. Inhibition was more apparent when CD34+ cells migrated in response to a combination of SDF-1α and SCF, rather than in response to SDF-1α alone (P < .05). No inhibition of CD34+ cell transmigration was observed when CD34+ cells and HBMECs were preincubated with a blocking mAb to PVR.
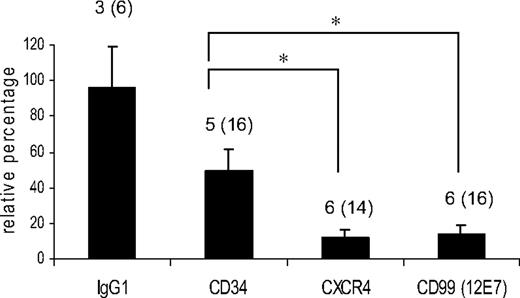
Homing of human mPB CD34+ progenitors in sublethally irradiated NOD-SCID mice is reduced by pretreatment with a 12E7 anti-CD99 mAb
To check whether in vitro observations could be confirmed in an independent in vivo model, we pretreated immunoselected mPB CD34+ cells with various mAbs, before tail vein injection in sublethally irradiated NOD-SCID mice. Human cells recovered from the BM of xenotransplanted animals after 18 to 24 hours were identified as CD45+ cells. The average percentage of human cells recovered from mice given transplants with untreated CD34+ cells was 0.69% ± 0.15% of mononuclear cells. Pretreatment with Immu133, an mAb targeting the CD34 antigen and with no effect in the in vitro transmigration assays (Figure 7C), resulted in a partial inhibition of homing to the BM, 18 to 24 hours after tail vein injection (Figure 8). Pretreatment with either the 12E7 anti-CD99 mAb or the 12G5 anti-CXCR4 mAb resulted in a near-complete inhibition of homing of human CD34+ cells, similar to what has been previously demonstrated for CXCR452 ; homing efficiency was significantly different in animals receiving injections of mPB CD34+ cells that were pretreated with 12E7 or Immu133.
Discussion
Expression and function of CD99 on T lymphocytes have been largely explored. CD99 is involved in T-cell interactions with neighboring cells in T-cell apoptosis.31,50,53 More recently, CD99 appeared to play a role in the transmigration of monocytes through endothelial junctions, using HUVECs as a model of primary endothelial cells.18 Although the expression of CD99 has been documented on various subsets of hematopoietic cells, little is known of its expression and role in the human hematopoietic progenitor compartment.
Here, we demonstrate that CD99 is expressed on a majority of human BM and mPB CD34+ cells, whereas less than 50% of CB CD34+ cells express CD99. The pattern of CD99 expression among CD34+ cells of different origins suggests a continuum of expression and some degree of heterogeneity within the progenitor cell subset, and allows for the delineation and sorting of CD34+/CD99low and CD34+/CD99high subsets. Phenotypic studies suggest that a high level of CD99 expression among mPB CD34+ cells is associated with characteristics of early stages of hematopoietic differentiation: CD38-, CD90+, CD105+, CD133+, ABCG2+,49 and high ALDH activity.54 Indeed, the level of CD99 expression among mPB CD34+ cells appears to be related to their differentiation ability. Most immature and granulocyte-macrophage clonogenic progenitors (HPP-CFCs, CFU-GEMMs, CAFCs, and CFU-GMs) appear to be present in the CD34+/CD99high subset. On the contrary, most erythroid progenitors (erythroid burst-forming units [BFU-Es]) appear to be present in the CD34+/CD99low subset. Consistent with this observation, CD34+/CD99low cells cultured in conditions that favor erythroid differentiation produced higher numbers of cells with phenotypic features that characterize erythroid cells than their CD34+/CD99high counterparts. Similarly, the level of expression for CD99 on CD34+ cells appears to be associated with different proliferative capacities; when differentiated toward the dendritic or NK cell lineages, mPB CD34+/CD99high cells and CD34+/CD99low cells acquire a similar phenotype; however, the expansion of the CD34+/CD99high population far exceeds the expansion of the CD34+/CD99low population. These differences cannot be explained by an initial difference in cell cycle activity because sorted CD34+/CD99high and CD34+/CD99low cells had a similarly low percentage of cells in the G2/M phase, consistent with the known low cell cycle activity of human circulating progenitors.55 Conversely, B-cell progenitors, as detected during coculture with the murine stromal cell line MS-5, appear to be mostly present in the CD34+/CD99high subset.
Adhesion of mPB CD34+ cells on HBMECs. Adhesion assays were run in the presence of 20 μg/mL of the different antibodies. The number of mAb-pretreated cells that had adhered was compared with nonpretreated cells (100% arbitrarily). An anti-CD106 mAb was used as a positive control of the inhibition of adhesion. Data are mean ± SEM of 3 experiments.
Adhesion of mPB CD34+ cells on HBMECs. Adhesion assays were run in the presence of 20 μg/mL of the different antibodies. The number of mAb-pretreated cells that had adhered was compared with nonpretreated cells (100% arbitrarily). An anti-CD106 mAb was used as a positive control of the inhibition of adhesion. Data are mean ± SEM of 3 experiments.
Transmigration of human mPB CD34+ cells and monocytes through HBMEC monolayers, in response to specific chemoattractants SDF-1α (with or without SCF) and MCP-1, respectively. (A) CD99 expression on CD34+ cells recovered from the lower chamber (migrated cells, gray area) and from the upper chamber (nonmigrated cells, white area), 4 hours after addition of SDF-1α in the lower chamber; one representative experiment; dotted line represents isotypic control. (B) Transmigration of human monocytes through HBMEC monolayers, in response to MCP-1 (200 ng/mL). An irrelevant IgG1 was used as a negative control. Data are mean ± SEM of 6 experiments with control, 12E7, PECAM-1, and PVR, and 3 experiments with hec2 and O662. (C) Transmigration of mPB CD34+ cells through HBMEC monolayers, in response to SDF-1α 100 ng/mL (□) or SDF-1α plus SCF (100 ng/mL; ▪).The Immu133 antibody that binds to CD34+ cells and HBMECs was used as a negative control. Data are mean ± SEM of 10 experiments with control, 12E7, PECAM-1 and PVR, and 3 experiments with hec2, O662, and the combination of 12E7 and PECAM-1. In both sets of experiments, the indicated mAbs were tested at a concentration of 20 μg/mL for their ability to inhibit transmigration. The 100% value corresponds to the number of untreated cells that migrate in response to chemoattractant(s). Chemotaxis in response to chemoattractant was assessed for 4 hours. *P < .05.
Transmigration of human mPB CD34+ cells and monocytes through HBMEC monolayers, in response to specific chemoattractants SDF-1α (with or without SCF) and MCP-1, respectively. (A) CD99 expression on CD34+ cells recovered from the lower chamber (migrated cells, gray area) and from the upper chamber (nonmigrated cells, white area), 4 hours after addition of SDF-1α in the lower chamber; one representative experiment; dotted line represents isotypic control. (B) Transmigration of human monocytes through HBMEC monolayers, in response to MCP-1 (200 ng/mL). An irrelevant IgG1 was used as a negative control. Data are mean ± SEM of 6 experiments with control, 12E7, PECAM-1, and PVR, and 3 experiments with hec2 and O662. (C) Transmigration of mPB CD34+ cells through HBMEC monolayers, in response to SDF-1α 100 ng/mL (□) or SDF-1α plus SCF (100 ng/mL; ▪).The Immu133 antibody that binds to CD34+ cells and HBMECs was used as a negative control. Data are mean ± SEM of 10 experiments with control, 12E7, PECAM-1 and PVR, and 3 experiments with hec2, O662, and the combination of 12E7 and PECAM-1. In both sets of experiments, the indicated mAbs were tested at a concentration of 20 μg/mL for their ability to inhibit transmigration. The 100% value corresponds to the number of untreated cells that migrate in response to chemoattractant(s). Chemotaxis in response to chemoattractant was assessed for 4 hours. *P < .05.
Although other ligands may exist in mice56 and mycoplasma,57 the only interactions described for human CD99 are homotypic interactions. Because CD99 is expressed on endothelial cells, preferentially at the interendothelial junctions, and because several structurally unrelated molecules expressed at interendothelial junctions have recently been shown to be involved in leukocyte transendothelial migration, we hypothesized that interactions between human CD34+ progenitors and endothelium may involve CD99-CD99 homotypic interactions.18 We first checked that HBMECs, our model cell line for BM vascular microenvironment, expressed CD99. We then tested whether several mAbs known to block various CD99 functions blocked adhesion of mPB CD34+ cells on HBMECs; in contrast with the known observation that a mAb to CD106/VCAM-1 reduces adhesion, we observed no significant inhibition. This lack of effect is consistent with the absence of modulation of LFA-1 expression on mPB CD34+ cells, following binding of CD99 (data not shown), an effect previously reported for T cells.36
Homing of human mPB CD34+ cells in the BM of sublethally irradiated NOD-SCID mice following preincubation with an irrelevant IgG1, the Immu133 (anti-CD34), 12E7 (anti-CD99), or 12G5 (anti-CXCR4) mAbs. Values on the y-axis represent homing of pretreated cells relative to homing of untreated cells. Human cells were detected by flow cytometry using an anti-CD45 mAb. *P < .05. Number of experiments (number of animals) is indicated for each group. Error bars represent SEM.
Homing of human mPB CD34+ cells in the BM of sublethally irradiated NOD-SCID mice following preincubation with an irrelevant IgG1, the Immu133 (anti-CD34), 12E7 (anti-CD99), or 12G5 (anti-CXCR4) mAbs. Values on the y-axis represent homing of pretreated cells relative to homing of untreated cells. Human cells were detected by flow cytometry using an anti-CD45 mAb. *P < .05. Number of experiments (number of animals) is indicated for each group. Error bars represent SEM.
We next tested the potential role of CD99 in the transendothelial migration of mPB CD34+ cells, using an in vitro assay. Cells were allowed to migrate in response to SDF-1α with or without SCF. A combination of these 2 chemoattractants was more efficient than SDF-1α alone to induce CD34+ cell migration through HBMECs, an observation that may result from the already described mobilization of intracellular CXCR4 in response to SCF.58 Cells that migrated displayed higher levels of CD99 expression, than cells that did not migrate, an indirect argument for a potential CD99-mediated interaction between progenitors and endothelial cells. Preincubation of both mPB CD34+ cells and HBMECs with several mAbs targeting CD99 produced different results; preincubation with 12E7 resulted in a significant decrease in the number of mPB CD34+ cells that transmigrated, whereas preincubation with Hec2 or O662 produced no or little effect. In contrast to what was reported for T cells and the O662 mAb,50 the 12E7 mAb failed to induce apoptosis of mPB CD34+ cells within 24 hours; this mechanism may thus not be suspected to explain our observations. The inhibition following preincubation with 12E7 was higher when CD34+ cells migrated in response to a combination of SDF-1α and SCF than to SDF-1α alone. It is interesting that CD34+/CD99high cells also displayed the lowest levels of c-Kit and CXCR4; in addition to the observation that the intracellular pool of CXCR4 can be mobilized in response to SCF,58 higher expression of CD99 may counterbalance the lower level of receptors for chemoattractants in this subset.
Results obtained with CD34+ progenitors are in sharp contrast with those obtained with human monocytes. Preincubation of mPB monocytes with any of the 3 anti-CD99 mAbs produced a strong inhibition of transmigration through HBMECs; in this set of experiments, the Hec2 mAb was more efficient than the O662 or 12E7 mAbs, as previously reported in experiments conducted with HUVECs.18 The 12E7 and O662 mAbs recognize different epitopes of the CD99 molecule,50 which may contribute to different functional effects. In addition, it is possible that the different ratios of the 2 CD99 isoforms in CD14+ monocytes and CD34+ progenitors, as shown in Figure 1, may contribute to this observation; monocytes express higher levels of the T2 isoform, which has been shown to play a role in the migration of breast cancer cells.39
PECAM-1 is considered to be the prototypic antigen involved in human hematopoietic transendothelial migration23-25 ; however, all published results demonstrate only a partial inhibition of progenitor transmigration, results that contrast with the stronger inhibition observed in similar in vitro experiments when mature leukocytes, monocytes, or lymphocytes, are studied.17 Inhibition of transmigration of mPB CD34+ cells through HBMECs after preincubation with an anti-CD99 mAb appears to be of the same order of magnitude, and thus only partial, than after preincubation of progenitors and endothelial cells with an anti-PECAM-1 mAb. The preincubation of CD34+ progenitors with a combination of a mAb to CD31 and a mAb to CD99 (12E7) resulted in an additive inhibitory effect. Previously published experiments with monocytes suggest that PECAM-1 and CD99 may get involved in different anatomic zones of the transendothelial junctions18 during monocyte-endothelial cell interactions; similar mechanisms may explain our observations.
No inhibition of CD34+ cell transmigration was observed following blockade of the CD155/PVR-DNAM-1 interaction, whereas the transmigration of mature CD14+ monocytes was abrogated, as previously reported.22 This suggests either that molecular actors involved in CD34+ cell transmigration may be different than those identified for mature leukocyte transmigration or that a significant proportion of progenitors may use alternative mechanisms to transit from the marrow compartment to the blood compartment.15
To further evaluate the potential role of CD99 in progenitor cell trafficking, we evaluated the homing of mPB CD34+ cells in the NOD-SCID mice after tail vein injection of CD34+ cells. Preincubation of mPB CD34+ cells with the 12E7 anti-CD99 mAb resulted in a strong inhibition of homing, at a level similar to what has previously been reported with an anti-CXCR4 mAb59 and reproduced in our hands. Part of this inhibition may be due to nonspecific mechanisms; mPB CD34+ cells coated with the anti-CD34 Immu133 mAb homed with a significantly lower efficiency to the BM than CD34+ cells preincubated with an irrelevant IgG1. However, the decrease in homing efficiency following preincubation with 12E7 was significantly different than after preincubation with Immu133. The rationale to use the NOD-SCID model of human progenitor xenotransplantation heavily relies on the structural homologies of CXCR4 between human and mouse. It is yet unknown whether a structural and functional homolog of human CD99 exist in mice; the only homologous murine molecules that have been identified share approximately 45% of their sequence with human CD99.56,60 Thus, the observed inhibition cannot be attributed to the targeting of homologous CD99 interactions with certainty, and further evaluation of the role of CD99 in progenitor cell trafficking will more appropriately use genetically modified strains for CD99 and murine models of transplantation.
In conclusion, we here demonstrate that CD99 expression is not limited to human hematopoietic mature cells but can also be detected in the progenitor compartment, as identified by CD34 membrane expression. Within this compartment, CD99 expression is heterogeneous and is apparently linked with the level of maturation. The level of CD99 expression is associated with significant changes in the differentiation and proliferative potential of CD34+ cells; of special interest, B-cell progenitors appear to belong preferentially to the CD34+/CD99high subset. Targeting CD99 with a blocking mAb does not affect adhesion of mPB CD34+ cells to human marrow endothelial cells. It reduces their ability to transmigrate through a monolayer of these cells in response to SDF-1α with or without SCF, and the homing to the marrow of sublethally irradiated NOD-SCID mice. Elucidating the exact contribution of CD99 in stem cell physiology will deserve further work.
Prepublished online as Blood First Edition Paper, July 6, 2006; DOI 10.1182/blood-2005-12-010827.
Supported, in part, by Institut Paoli-Calmettes and by a grant from the European Economic Community (EEC) (EUROCORD III program; C.C.). G.B. is the recipient of a grant from a joint research training program established by the French and Algerian governments.
Presented, in part, at the First European School of Hematology (ESH)-European Group for Blood and Marrow Transplantation (EBMT)-EUROCORD Euroconference on stem cell research in Cascaïs, Portugal, April 15, 2005.61
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
The authors thank Prof. Alain Bernard for his support in the conduct of this work. The authors thank all personnel at the Tumor Cell Collection (Biological Resource Center) and at the Centre de Thérapie Cellulaire et Génique (Cell and Gene Therapy Facility) for access to apheresis and cord blood samples. They also thank Rémy Galindo at the Flow Cytometry Facility for his help during the conduct of these studies, and Boris Calmels for critical reading of the manuscript.

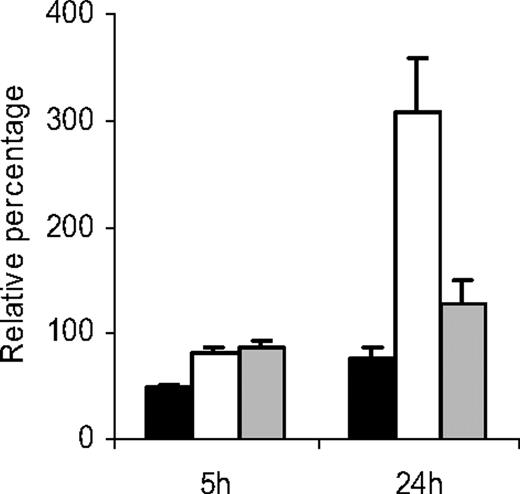



 ). The proportion of annexin V+ cells relative to the untreated control (arbitrarily 100%) was evaluated after 5 hours in the absence of cytokines and after 24 hours of culture in a medium supplemented with IL-3, IL-6 (10 ng/mL each), and SCF (100 ng/mL). Data are mean ± SEM of 3 experiments.
). The proportion of annexin V+ cells relative to the untreated control (arbitrarily 100%) was evaluated after 5 hours in the absence of cytokines and after 24 hours of culture in a medium supplemented with IL-3, IL-6 (10 ng/mL each), and SCF (100 ng/mL). Data are mean ± SEM of 3 experiments.