Abstract
Although it is now generally accepted that imatinib is the best initial treatment for patients newly diagnosed with chronic myeloid leukemia (CML) in chronic phase, a number of questions remain unanswered. For example, (1) Is imatinib the best initial treatment for every chronic-phase patient? (2) At what dose should imatinib be started? (3) How should response to treatment be monitored? (4) For how long should the drug be continued in patients who have achieved and maintain a complete molecular response? (5) How does one handle a patient who achieves a 2-log but not a 3-log reduction in BCR-ABL transcripts? (6) How should response or failure be defined? (7) For the patient deemed to have failed imatinib, should one offer dasatinib or nilotinib? (8) For the patient who has failed imatinib but has a possible allogeneic transplant donor, should one offer dasatinib or nilotinib before recommending a transplantation? (9) Should the transplantation be myeloablative or reduced intensity conditioning? (10) How should one treat the patient who relapses after allografting? This paper will address these issues, many of which cannot yet be answered definitively.
Introduction
Although the entity we refer today as chronic myeloid leukemia (CML) was probably first described in the early nineteenth century, there was little progress in understanding its biology until the discovery of the Philadelphia (Ph) chromosome in 1960.1 Subsequent important landmarks were the recognition that the Ph chromosome results from a t(9;22) translocation, the demonstration that the leukemia probably originates from a single hematopoietic “stem cell,” the identification of the breakpoint cluster region (BCR) on chromosome no. 22 and subsequently of the BCR-ABL fusion gene, and more recently the development of a murine model simulating the human disease.2,3 Treatment in the 19th century was unsatisfactory, although arsenicals induced some degree of symptomatic control. In the early 20th century, radiotherapy was helpful, but it was replaced in the 1950s by busulfan, which remained popular for some years, despite the emerging suspicion that this alkylating agent might in fact predispose to progression to advanced-phase disease. In due course, hydroxycarbamide replaced busulfan, but interferon-alfa, the first agent to induce any degree of Ph-chromosome negativity in the bone marrow, was introduced in the early 1980s and became the treatment of choice for patients not eligible for allogeneic stem cell transplantation. Between 1980 and 2000, allografting, despite the risks of morbidity and mortality, was the recommended initial treatment for younger patients with HLA-matched donors. Therapy has now been “revolutionized” by the introduction of imatinib (imatinib mesylate, IM), the original Abl tyrosine kinase inhibitor (TKI), which was used first in the clinic in 1998.4 This paper will attempt to define approaches to management of the newly diagnosed patient with CML in chronic phase (CP) that are favored in 2007, but it is most probable that these recommendations will need to be updated as further experience is gained with the use of TKIs
Imatinib
Imatinib is a 2-phenylaminopyridimine compound developed for clinical use as a result of a collaboration between Brian Druker and investigators at Ciba-Geigy (subsequently merged with Sandoz to form Novartis Pharma) in Basel that started in the early 1990s5 (Figure 1). Initially, the preclinical program moved slowly because many in the field believed that a small molecule that effectively blocked the kinase activity of the Bcr-Abl protein would lack specificity and would inhibit also other protein tyrosine kinases essential for normal cell survival. However, study of cell lines and primary material collected from patients with CML suggested that it did indeed selectively inhibit proliferation of CML cells,6,7 and phase 1/2 clinical studies started in patients judged to be resistant to interferon-alfa in 1998. The new agent formulated for oral administration, then termed STI571, induced cytogenetic responses, some complete, in a high proportion of patients and had limited toxicity; the maximum tolerated dose was not established, but a starting dose of 400 mg daily for adults was recommended. The drug was eliminated predominantly by hepatic metabolism; it had a plasma half-disappearance time of 18 hours, which provided the rationale for once daily administration. Subsequently phase 2 studies for patients resistant to or intolerant of interferon undertaken in various countries confirmed these initial clinical findings.8
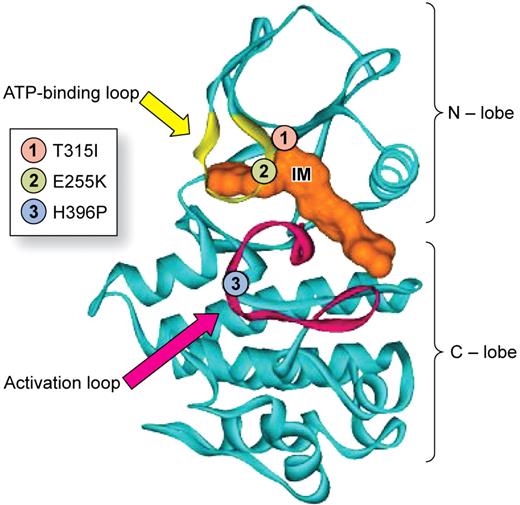
Abl protein with the activation loop in the closed configurations showing the manner in which imatinib (marked IM) occupies the ATP-binding site (also known as the phosphate- or P-loop). Note also the relative position of 3 of the more commonly mutated residues: (1) T315I in the gateway position, (2) E255K in the P-loop, and (3) H396P in the activation loop. Adapted with permission from Deininger et al.5 © The American Society of Hematology.
Abl protein with the activation loop in the closed configurations showing the manner in which imatinib (marked IM) occupies the ATP-binding site (also known as the phosphate- or P-loop). Note also the relative position of 3 of the more commonly mutated residues: (1) T315I in the gateway position, (2) E255K in the P-loop, and (3) H396P in the activation loop. Adapted with permission from Deininger et al.5 © The American Society of Hematology.
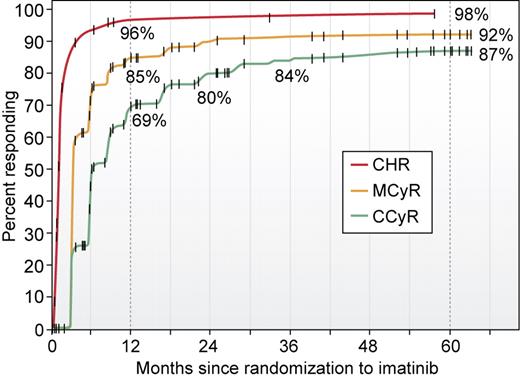
A phase 3 study (the IRIS study) designed to compare prospectively the administration of IM 400 mg daily with the combination of interferon-alfa and cytarabine in previously untreated CP recruited 1106 patients from 16 countries in 2000 and preliminary results were published in 2003.9 With a median follow-up of 19 months, the estimated rates of complete hematologic response (CHR) for patients whose initial treatment was IM were 96%; of major cytogenetic response (MCyR), 87%; and of complete cytogenetic response (CCyR), 76%. (The term MCyR includes both CCyR and partial cytogenetic responses.) The results of this study were recently updated.10 With 5 years of follow-up, the estimated cumulative best rates of CHR and CCyR were 98% and 87%, respectively (Figure 2). These numbers include, of course, a minority of patients who did achieve CHR or CCyR, respectively, but subsequently lost their responses or died of unrelated causes while still responding. The number of patients in CCyR who were still known to be taking IM at 5 years was 368 (68%) of the 553 who started IM as initial therapy. For the patients in the first-line IM arm, overall survival at 5 years was 89.6%.
Survival for previously untreated chronic-phase patients who received imatinib 400 mg daily as initial therapy for newly diagnosed CML in chronic phase. The curves show the estimated cumulative best complete hematologic response, major cytogenetic response, and complete cytogenetic response rates, respectively, at 5 years from start of therapy. The vertical dotted lines show the 1- and 5-year values. Reprinted with permission from Druker et al.10 © 2006 Massachusetts Medical Society. All rights reserved.
Survival for previously untreated chronic-phase patients who received imatinib 400 mg daily as initial therapy for newly diagnosed CML in chronic phase. The curves show the estimated cumulative best complete hematologic response, major cytogenetic response, and complete cytogenetic response rates, respectively, at 5 years from start of therapy. The vertical dotted lines show the 1- and 5-year values. Reprinted with permission from Druker et al.10 © 2006 Massachusetts Medical Society. All rights reserved.
Because many of the patients who started IM as second-line therapy in the IRIS study switched therapy to IM, a formal comparison of the longer term results of treatment with IM and interferon-alfa/cytarabine was not possible. In practice, the rates of CHR and CCyR for these patients defined on an “intention-to-treat” basis were not significantly different from comparable rates for first-line IM patients. Moreover, recent comparisons of survival for patients treated initially with IM with that of historical control patients who received interferon-alfa or IFN-containing regimens in a French multicenter study and at the M. D. Anderson Cancer Center in Houston both showed significant superiority for survival of patients treated with IM.11,12
Allogeneic stem-cell transplantation
Until the advent of IM, it was conventional to offer patients with newly diagnosed CML in chronic-phase treatment with high-dose chemotherapy or chemoradiotherapy followed by transfusion of hematopoietic stem cells provided they were relatively young (eg, younger than 50 years) and had suitable HLA-identical siblings, HLA-matched family members, or HLA-matched volunteer unrelated donors. Although the morbidity and indeed mortality attributable to the procedure were both appreciable, the probability of survival could be predicted with reasonable accuracy by the scoring system developed for the European Group for Blood and Marrow Transplantation (EBMT).13,14 Thus “good risk” patients with low scores (ie, 0-2) had a probability of being alive at 5 years of 60% to 80%. In some specialist centers even better results were achieved.15 The probability of subsequent relapse for patients free of detectable disease at 5 years was extremely low,16,17 and so it has been widely accepted that allogeneic stem-cell transplantation (allo-SCT) can eradicate all evidence of disease in a given patient followed for more than 1 or 2 decades—a status tantamount to cure.
The fact that this “cure” appears to result from the combined effects of the high-dose chemotherapy or chemoradiotherapy used as “conditioning” before the transplantation and a graft-versus-leukemia effect mediated by immunologically competent cells in the donor inoculum provided the rationale for reducing the intensity of the conditioning and exploiting the use of donor-derived T-cells to effect cure. Such “nonmyeloablative” or “reduced intensity conditioning” transplantations should be particularly valuable for patients older than 50 years or younger patients with comorbid conditions. Although a number of small single-center series and an analysis of outcome for 186 patients treated in 38 centers reporting to the EBMT have been published,18-22 it is not yet possible to conclude that a reduced intensity conditioning allo-SCT offers a major advantage for the younger patient who would otherwise be a candidate for an allograft with conventional conditioning. It is undoubtedly an option for the older patient who could not normally be considered for a transplantation with myeloablative conditioning.
Initial therapy for the patient in chronic phase
The issue of how best to treat the new CML-CP patient was controversial for some while after the introduction of IM, but has now been largely resolved. Thus the clinician and his/her patient had to balance the notion that a transplantation, although associated with appreciable risks, could if successful cure the leukemia against the knowledge that early results with IM promised to prolong life without any definite prospect of “cure” and that possible late toxicity could not be predicted. In the event, the annual number of transplantations performed for CML on both sides of the Atlantic has fallen markedly in the last 5 years,23,24 and most hematologists today recommend initial treatment with IM as a single agent or entry into a clinical trial in which IM or another TKI is initial therapy. A case can be made for offering an upfront transplantation to the new patient who is poor risk by Sokal or Hasford criteria25,26 and also good risk for surviving a transplantation by EBMT criteria,13 but in practice most hematologists would start treatment with IM even for this small subgroup of patients.
There may be 2 exceptions to this general rule. First, some pediatricians believe that initial treatment by allo-SCT may be the preferred approach for children who have HLA-identical sibling donors but even this view is giving way to the notion that an initial trial of IM may be preferable. Second, in a situation where the cost of continuing treatment with IM for some considerable number of years is prohibitive, then upfront allografting should be considered, especially if this procedure can be carried out more cheaply than is usual in the western world.
In summary, the majority or all patients who present with CML in chronic phase should if possible receive initial treatment with imatinib.
Starting dose of IM
The recommended starting dose of IM in the IRIS study was 400 mg daily regardless of the size of the patient, and this remains the “standard” dose. Investigators in Houston have started treatment for a relatively large cohort of newly diagnosed patients with 800 mg daily.27 Hematologic and cytogenetic responses were obtained more rapidly than with historical control patients who started treatment with 400 mg daily; major and complete molecular responses were more frequent and were achieved more rapidly. An alternative approach was incorporated into an Australian study in which patients started treatment with 400 mg daily but increased IM dosage if they failed to reach defined landmarks at 3-month intervals.28 Currently, there is no definite evidence that starting treatment with doses greater than 400 mg daily or escalating dosage for patients who appear to be responding is associated with reduced risk of disease progression or prolonged survival, but prospective studies addressing this issue are in progress.
In summary, the starting dose for patients not in a clinical study should be 400 mg daily.
Predicting the response to imatinib in an individual patient
In general, a major factor to be considered when deciding how to start treatment for a given CP patient is whether he or she has disease features that might predict for a response that is better or worse response than average. Thus Sokal et al in 1984 identified 4 features at diagnosis that enabled them to divide patients into good, intermediate, and poor prognosis categories defined on the basis of subsequent survival.25 The Sokal score was derived from a population of patients treated predominantly with busulfan, but an updated version continued to have validity in the interferon era.26 The Sokal score appears also to influence the probability of achieving CCyR and major molecular response (MMR) in the IM era.9 It is likely however that newer laboratory-based techniques such as gene expression profiling,29,30 measurement of drug transport,31 or assessment of imatinib IC5032,33 will eventually be more informative than the Sokal score.
Adverse effects of IM
The absorption and metabolism of IM may be affected by other concomitant medications, and the clinician should therefore check carefully for the possible adverse effects of drug interactions.
A significant proportion of patients sustains some degree of hematologic toxicity after starting treatment with IM at 400 mg daily, and the proportion is higher in those who receive 800 mg daily.34,35 The toxicity may take the form of reduced cell numbers in a single lineage or pancytopenia. The cause of this myelosuppression is not entirely clear. It unlikely to be due to a direct effect of IM on residual normal hematopoiesis because it is rare in patients treated with IM for gastrointestinal stromal tumors (GISTs). It may be due to inadequate reserve of normal stem cells in some patients, but if so the basis for this heterogeneity is unknown. Neutropenia can often be managed by administration of granulocyte colony-stimulating factor (G-CSF) 300 μg/kg (daily, alternate daily, or once weekly),36 and anemia usually responds to erythropoietin. Severe thrombocytopenia may necessitate temporary interruption of IM. It is recommended that the drug should be stopped entirely and then resumed when the cytopenia has resolved rather than reducing the dosage lower than 300 mg/day.
IM can cause a variety of nonhematologic toxic effects. A significant minority of patients experiences infraorbital edema or rarely more generalized edema. Pains in bones and joints may occur. A variety of rashes may be seen. There may be abnormalities of liver enzymes that necessitate interrupting treatment. Hypo-phosphatemia associated with decreased levels of calcium, 25-hydroxyvitamin D, and 1,25 hydroxyvitamin D has been seen in some patients.37 Occasional patients have proceeded to hepatic failure. In many cases where IM has had to be interrupted, the drug can subsequently be resumed without recurrence of toxicity, with or without judicious use of corticosteroids. In other cases, the patients must be judged “intolerant” and offered therapy with a newer TKI. Adverse effects attributable to IM do not usually recur when the patient is treated with other TKIs.
There is a recent report of 10 patients treated with IM who developed congestive cardiac failure while receiving IM, mostly at doses greater than 400 mg.38 The authors performed a series of elegant experiments in which they administered high doses of IM to experimental animals, some of which developed cardiac failure with specific abnormalities in myocardial mitochondria. This led other clinicians to search diligently for evidence of cardiac failure in large numbers of patients treated at many different centers worldwide; they concluded that the incidence of cardiac failure in a large population of patients was no greater than would be expected in previously healthy persons of similar age.39-41 For the present, one may conclude that the original proposition that IM at standard dosage causes cardiac failure in humans has received no independent support.
Studies in experimental animals have suggested that IM could be teratogenic, and female patients are therefore routinely advised to avoid conception while taking IM. Inevitably, some women taking IM have conceived, and some pregnancies have proceeded to term. It appears that the incidence of fetal abnormalities is higher than might be expected in a comparable healthy population,42,43 which means that the advice to avoid conception while on IM is probably well founded.
There is a report from France documenting the occurrence of urothelial tumors in patients treated with IM.44 Three patients who developed Ph-negative acute myeloid leukemia are reported from the United States.45 One cannot conclude from these 2 uncontrolled series that there is any increased risk of second malignancy attributable to IM.
In summary, various different adverse effects are attributable to IM but most can be managed with relatively straightforward measures. Nine years' experience with use of IM suggests that serious adverse effects are very rare.
How long should IM be continued in the responding patient?
There is preliminary evidence that the incidence of disease progression in responders diminishes with each successive year on IM. Moreover, there is no suggestion that the incidence of toxicity increases with duration of treatment. Anecdotal evidence suggests that most patients who stop taking IM lose within weeks or months the response they did achieve. These facts taken together suggest that the best advice for individual patients responding to IM is that the drug should be continued indefinitely, although whether this should be at full dose (400 mg daily) or at reduced dose is not yet established.
A small number of patients in whom BCR-ABL transcripts have been undetectable for more than 1 or 2 years have stopped taking IM for various reasons. In the largest series published thus far, 6 of 12 patients showed evidence of relapse at the molecular level within 5 months of stopping IM, but the other 6 remained in “complete molecular remission” at a median follow-up of 15 months.46 This observation does raise the intriguing possibility that IM continued for long enough might eradicate residual leukemia in selected patients, perhaps particularly in those who have previously been treated with interferon-alfa. In vitro studies however suggest that “quiescent” leukemia stem cells are highly resistant to IM,47 and thus some at least are likely to survive long term even in patients who achieve a complete molecular remission, a conclusion supported by mathematic modeling of changes in BCR-ABL transcript numbers in responding patients.48 Whether this is clinically relevant remains to be seen.49
In summary, responding patients should continue IM indefinitely until such time as the results of prospective studies suggest otherwise.
Clinical trials for new patients
The impressive success of IM 400 mg daily used as a single agent has raised a number of questions in relation to optimal dosage and use of IM in combination that cannot yet been answered. Perhaps the most pressing question relates to optimal starting dose, and for this reason prospective studies comparing 400 mg and 800 mg for new CP patients have been initiated on both sides of the Atlantic. Other prospective studies address the combination of IM plus interferon-alfa at low dosage and IM plus cytarabine. The results of using IM alternating with interferon-alfa, G-CSF, second-generation tyrosine kinase inhibitors, or specific signal transduction inhibitors will also be of great interest.
Monitoring patients on imatinib
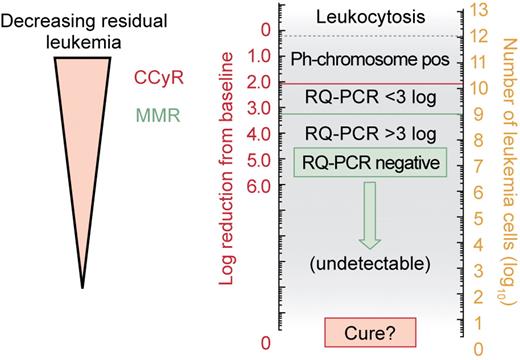
The response to IM in newly diagnosed CP patients varies quite considerably both in speed of response and in the degree to which the drug reduces the quantity of disease in a patient's body (Figure 3). This is probably due to the intrinsic heterogeneity of the leukemia, but fundamental differences between patients in the way in which the drug is handled in the body may also influence the speed and level of response (Table 1). It is thus logical to try to assess the level of response at different time points and if necessary at some point to classify a patient as a nonresponder. Because response to treatment in CML proceeds in an orderly manner, first with restoration of spleen size to normal and normalization of the blood count, then with reversion of the bone marrow to Ph negativity, and eventually with reduction in the number of BCR-ABL transcripts in the blood and marrow to very low or undetectable levels, these criteria can be used sequentially to monitor the response in an individual patient.50 There are 2 important reasons for monitoring a patient's response fairly closely. First, the degree to which the total quantity of disease in a patient's body is reduced (as judged by surrogate markers that include bone marrow cytogenetics and BCR-ABL transcript numbers in the blood) correlates inversely with the probability of subsequent progression to advanced-phase disease,51 and second, it is important to recognize a patient who responds poorly or who having responded loses his/her response in order to revise therapeutic strategy.52
Schematic representation of decreasing residual disease related to numbers of BCR-ABL transcripts in the peripheral blood (left scale) and estimated number of residual leukemia cells in a patient's body (right scale).
Schematic representation of decreasing residual disease related to numbers of BCR-ABL transcripts in the peripheral blood (left scale) and estimated number of residual leukemia cells in a patient's body (right scale).
The majority of patients achieve normal blood counts within 3 months, and more than 90% will have achieved CHR by 6 months after start of treatment. Approximately 40% of previously untreated patients will have achieved a MCyR (< 35% Ph-positive marrow metaphases) by 6 months, and 65% will have achieved a CCyR after 1 year of therapy. A small minority of those who achieve CCyR will subsequently regain evidence of marrow Ph positivity, and an even smaller proportion will eventually progress to advanced-phase disease.
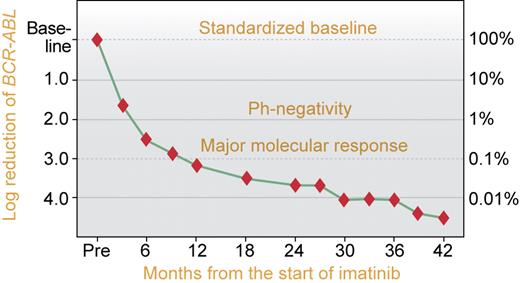
Once a patient has achieved a CCyR, undoubtedly the most sensitive method for monitoring the quantity of residual disease in his/her body is to measure BCR-ABL transcript numbers (Figure 4). The use of blood or marrow for this purpose gives equivalent results but obviously the former is more convenient. The current methodology involves using real-time quantitative polymerase chain reaction (RQ-PCR) whereby the BCR-ABL transcript numbers are related to transcript numbers of a control gene that ideally is expressed in the leukemia cells at approximately the same level as in normal cells. The result is expressed in 1 of 2 ways—either as the ratio of BCR-ABL control gene transcript numbers on a log10 scale × 100% or as the “log reduction” from a standardized baseline derived from results obtained in a series of untreated patients.51,53 ABL is a reliable control gene when measuring low levels of residual leukemia, but other genes, such as β-glucuronidase, BCR, or β-2-microglobulin, are also suitable.51 Efforts are now being directed to ensure that results achieved in a given diagnostic laboratory can be converted to an international scale that would be applicable worldwide.
Schematic representation of the reduction in BCR-ABL transcript numbers after start of imatinib for CML in chronic phase. The scales show log reduction from a standardized baseline (left scale) and the ratio of BCR-ABL transcript numbers to a control gene expressed as a percentage (right scale). Reproduced with permission from Dr Timothy Hughes (Adelaide).
Schematic representation of the reduction in BCR-ABL transcript numbers after start of imatinib for CML in chronic phase. The scales show log reduction from a standardized baseline (left scale) and the ratio of BCR-ABL transcript numbers to a control gene expressed as a percentage (right scale). Reproduced with permission from Dr Timothy Hughes (Adelaide).
In general, a falling level of BCR-ABL transcripts correlates closely with increasing cytogenetic response, but the RQ-PCR result becomes most informative for a patient in CCyR. Thus, a patient who achieves a 2-log reduction in BCR-ABL transcripts will typically be Ph negative in a study of bone marrow cytogenetics, and a patient who achieves a 3-log reduction in BCR-ABL transcripts is defined as having achieved a major molecular response. In most laboratories, BCR-ABL transcripts can no longer be detected when the reduction reaches 4 to 5 logs, a status that has been designated a complete molecular response. It is worth emphasizing, however, that the level of leukemia transcripts below which the assay is negative depends on the sensitivity of the assay, which differs in different laboratories; even with the most sensitive assay, complete molecular remission is consistent with the persistence in the patient's body of up to 106 or 107 leukemia cells.50
The frequency with which these tests should be performed on a patient who appears to be responding well has been the subject of some debate. A reasonable recommendation is to perform bone marrow examination to assess Ph positivity at diagnosis and then at 3-month intervals until CCyR.52 Identification of a BCR-ABL gene before starting treatment is a useful confirmation of the Ph positivity (and is of course essential in patients thought to have Ph-negative CML), although transcript levels vary widely in untreated patients. After diagnosis, molecular studies can reasonably be performed at 3-month intervals indefinitely. For a patient who has achieved MMR, further bone marrow tests will not reveal Ph positivity, but they may uncover features of cytogenetic abnormalities in Ph-negative cells (see “Clonal cytogenetic changes in Ph-negative cells”) or features of myelodysplasia. Fluorescence in situ hybridization (FISH) for the BCR-ABL gene performed on peripheral blood cells may be more sensitive than routine marrow cytogenetics but does not approach the sensitivity of RQ-PCR and is not therefore suitable for monitoring the patient in MMR.
In summary, patients should be monitored by bone marrow cytogenetics at diagnosis and at 3-month intervals until achieving CCyR. Thereafter, marrow cytogenetics may be performed at one-year intervals but is not mandatory. BCR-ABL transcript numbers should be measured at 3-month intervals after starting IM, but a pretreatment value may not be very informative. In patients with increasing proportions of Ph-positive marrow metaphases or increasing BCR-ABL transcript numbers, the frequency of monitoring should be increased.
Clonal cytogenetic changes in Ph-negative cells
There are now more than 20 published reports of clonal cytogenetics change in Ph-negative metaphases in patients responding to treatment with IM.54-56 The abnormalities include especially +8, −7q, and −Y. In some cases, they appear to be transient, but in other cases they persist or even increase in proportion with time. They do not seem to harbinger progression to myelodysplasia or acute myeloid leukemia. It seems unlikely that they are the direct result of treatment with IM because they have been seen on rare occasions in patients responding to interferon-alfa and they have not be seen in patients who received IM as treatment for GIST. They might reflect genomic instability in a cell population that preceded the acquisition of the Ph chromosome, or they may be an abnormal response to stress consequent on restoration of Ph-negative and presumably normal hematopoiesis.
Defining and managing failure on IM
Although experience with use of IM is still relatively limited, a number of attempts have been made to identify criteria that would enable the clinician to define a patient as having failed IM at 400 mg daily.57 A panel of international experts proposed recently that patients not responding optimally to IM may be classified as “failure” or “suboptimal response” (Table 2).52 Patients in the category “failure” should be changed to alternative therapy and patients classified as “suboptimal response” should be considered for a change in therapeutic strategy. A third category, “warnings,” was used to identify a patient who might for one or another reason be expected to respond less well to IM. Such patients should presumably continue IM but should be monitored more closely than average.
Resistance to imatinib
Primary resistance
A very small proportion of newly diagnosed chronic-phase patients never achieves a complete hematologic response, and others never achieve durable cytogenetic responses when treated with IM, even after the dose is increased to 600 or 800 mg daily. This may be due to undefined mechanisms that dictate the intrinsic heterogeneity of the leukemia or to individual variations in pharmacokinetics. For example, cellular uptake of IM is an active process mediated by human organic cation transporter 1 (hOCT1), the levels of which vary greatly in different patients.31 Moreover, IM is a substrate for P-glycoprotein, the product of the multidrug resistance gene (MDR-1), and high prevailing levels of P-glycoprotein could increase drug efflux and thus render cells constitutionally resistant to IM, as had been demonstrated in cell lines and in cells from patients with blastic-phase CML.60
Secondary resistance
Secondary or acquired resistance is somewhat better understood. An important minority of patients who start IM treatment in chronic phase appear initially to respond, achieving either cytogenetic or indeed major molecular responses, and then lose their response. This sequence of events is more common in patients who start treatment in advanced phases of CML, implying that even patients in blastic transformation usually have a disease that is still at least partially dependent on BCR-ABL–related mechanisms. In some cases, the secondary resistance is thought to be due to acquired amplification of the BCR-ABL gene with associated overexpression of the Bcr-Abl oncoprotein. In other cases, the resistance may be due to overexpression of the P-glycoprotein. In a high proportion of patients who develop secondary resistance after initial responses, Ph-positive subclones characterized by point mutations in the BCR-ABL kinase domain have been identified, and these are often associated with reactivation of the dysregulated enzymatic activity of the Bcr-Abl protein, which is most usually assessed in vitro by the capacity of the oncoprotein to phosphorylate the CRKL protein. Such mutations are more commonly found in patients treated in advanced-phase than in chronic-phase CML. The first such mutation identified was a nucleotide change that coded for the replacement of a threonine by an isoleucine at amino acid position 315 in the Abl component of the Bcr-Abl (termed T315I).59 Subsequently other mutations were reported at codon positions 253, 255, 317, and 396, each of which alters an amino acid that is predicted by x-ray crystallography to make contact with IM. Approximately 50 such mutations have now been identified, but the most important one still seems to be the T315I, referred to sometimes as the “gateway” mutation, because this mutant subclone is uniformly resistant to treatment with IM and second-generation TKIs. Other mutations are associated with various degrees of resistance to IM,62 such that some are certainly clinically significant and others less obviously so.63 In general, these mutations can be identified at low level in IM-naive patients and are thought therefore to expand as a result of selective pressure exerted by IM. Mutations occurring in the P-loop of the kinase domain are usually associated with resistance to IM and may or may not also predispose to disease progression.64,65
A proportion of patients with secondary resistance to IM has no demonstrable restoration of Bcr-Abl kinase activity, and IM resistance must then be due to the capacity of other signaling mechanisms to “replace” the Bcr-Abl pathway. In some cases, the Src kinase family gene LYN is overexpressed and may substitute for Bcr-Abl,66 but in many cases the mechanism of this Bcr-Abl–independent secondary resistance is not known.
In summary, resistance to IM may be primary or secondary as assessed by hematologic, cytogenetic, and/or molecular criteria. Patients who fail treatment with IM should be screened for the presence of kinase domain mutations, especially the T315I.
What to do for the IM-resistant patient still in chronic phase
The principles for managing primary and secondary resistance are very similar. The first issue confronting the clinician will be to decide that the patient has failed imatinib at the prescribed dose. Patient compliance seems to be an important consideration, and the clinician must do his/her best to exclude the possibility that the patient is not taking the drug or is taking it at reduced or intermittent dosage. The next and easiest step will be to increase the dosage from 400 mg to 600 or 800 mg daily, and this may induce or reinduce cytogenetic responses, although they may not be prolonged.67,68 Moreover, not all patients can tolerate the 800-mg dosage.
In general terms, a patient who satisfies cytogenetic criteria for resistance to the highest feasible dose of IM should be considered for treatment with a second-generation TKI (below). The possible presence of a kinase domain mutation should be sought at this stage. If the patient does not have a T315I clone there is at present little to choose between dasatinib and nilotinib as secondary therapy, assuming both are available. If the T315I is identified, one can predict that response to either of these 2 drugs will be poor, and it may be reasonable to switch treatment to hydroxycarbamide, interferon-alfa, or possibly cytarabine. The new aurora kinase inhibitor, MK-0457, may prove valuable for patients with T315I mutations.69
If the patient with IM-resistant leukemia is relatively young and has an HLA-matched donor, the possibility of proceeding to allo-SCT should be considered. This option may be preferable to use of further chemotherapy if the patient has a T315I mutation.68 In the past, delay between diagnosis and allo-SCT has been regarded as an adverse prognostic factor but this may not apply in the IM era. There is no evidence that prior treatment with IM increases the risk of transplantation-related mortality,71,72 but experience is still limited. If a transplantation is to be undertaken, the issue of whether to use standard or reduced intensity conditioning remains unresolved. For the older patients (eg, older than 50 years), a transplantation using reduced intensity conditioning may be preferable to use of standard conditioning.
In summary, the best available definitions of failure are currently those recommended by the European LeukemiaNet panel.52 Patients who fail IM and are ineligible for transplantation should be offered dasatinib or nilotinib. For those with possible matched donors, no firm recommendations can yet be made. One possible compromise is to administer a second-generation TKI for a finite period (eg, 6 or 9 months) and to proceed with an allogeneic stem-cell transplantation in the absence of a durable response. If a transplantation is advised, use of a myeloablative conditioning is probably appropriate for the younger patient, but for those older than 50 years or those with other concomitant disease the use of reduced intensity conditioning should be considered.
Clinicians and indeed patients often wonder how to continue treatment for a patient who achieves a CCyR but whose BCR-ABL transcript numbers then achieve a “plateau” above the level of MMR that extends for 6 or months or longer (ie, he/she has only achieved a 2- to 3-log reduction). There is no consensus as to how such patients should be managed. The options include making no change in IM dosage, increasing IM to 600 mg or 800 mg daily, or switching to a newer TKI.
Newer tyrosine kinase inhibitors
Various new agents are now in early stages of clinical development, at least 3 of which could prove superior to IM (Table 3).
Dasatinib
Dasatinib is an orally available Abl kinase inhibitor that differs from IM in that it can bind both to the active and inactive conformations of the Abl kinase domain and also inhibits Src family kinases including Src and Lyn. Thus, it has been referred to as a dual inhibitor. It is approximately 300 times more active than IM and in vitro is active against most of the IM-resistant mutant subclones, with the notable exception of the T315I clone73 and probably also of a F317L mutant clone.74 Thus far, the drug has been used predominantly in CML patients judged to be resistant to or intolerant of IM.75 In phase 2 study of 186 patients with imatinib-resistant or imatinib-intolerant CML who received dasatinib at 140 mg daily, complete hematologic responses were achieved in 90% of patients and major cytogenetic responses were seen in 52% of evaluable patients.76 Responses were maintained in 95% of the responding patients. Responses occurred with equal frequency in patients who did and in those who did not have kinase domain mutations. Patients with T315I mutations proved resistant. Its use in CML was approved in 2006 by the Food and Drug Administration (FDA) in the United States and the European Agency for the Evaluation of Medical Products (EMEA) in Europe. Studies to test the efficacy of the drug at a dose of 100 mg daily in previously untreated patients have now been initiated.
The drug is not without toxicity. Adverse events have included neutropenia, thrombocytopenia, diarrhea, vomiting, nausea, gastrointestinal hemorrhage, rashes, and edema.77 Of particular interest has been the occurrence in some patients of pleural and pericardial effusions, most of which resolved when the drug was stopped. These last complications may be rarer in previously untreated patients who receive the lower dose of dasatinib.
Nilotinib
Nilotinib is an orally active aminopyrimidine derivative that resembles IM but has been modified to increase the binding affinity to the ATP pocket of the Bcr-Abl oncoprotein. It has 20 to 50 times the inhibitory activity of IM in IM-sensitive cell lines and is active against all IM-resistant cell lines bearing Abl kinase domain mutations with the exception of the T315I. The Y253H mutant clone may also be relatively resistant to nilotinib.78 In a phase 1 dose escalation study of 46 patients with IM-resistant CML in accelerated phase, 33 had hematologic responses and 22 had cytogenetic responses.79 Of 12 patients with CML in “active” chronic phase resistant to IM, 12 had hematologic responses; of 17 chronic-phase patients evaluable for cytogenetic responses, 9 patients responded and had CCyR. There was no difference in response rates between patients who did and those who did not have Abl kinase domain mutations.
The doses used in this phase 1 study ranged from 50 mg once daily through 600 mg twice daily. Adverse events included rashes, pruritus, constipation, increased lipase levels and hepatic enzymes, and increased unconjugated bilirubin. In general, toxic effects attributable to IM were not seen when the same patient was treated with nilotinib. The recommended dosage is now 800 mg daily. It is anticipated that the drug will be licensed by the FDA in the United States and EMEA in Europe later this year.
In summary, both dasatinib and nilotinib seem to be equally active in patients deemed to have failed IM. Neither agent is recommended for the patient with a T315I mutant clone predominating.
Bosutinib (previously SKI-606)
This is a 4-anilino-3-quinolinecarbonitrile that inhibits Abl and Src kinases and can thus also be classified as a dual kinase inhibitor. It is very much more active than IM against CML cell lines and murine lines transfected with BCR-ABL. It was active also against cell lines carrying 3 of the 4 kinase domain mutations that were tested.80 Initial clinical studies are under way on both sides of the Atlantic.81
Inno-406 (previously NS-187)
This agent is another aminopyrimidine variant of IM modified in a manner designed to increase its binding to the Bcr-Abl ATP pocket. It is active against Bcr-Abl and Lyn, and can therefore be classified, like dasatinib, as a dual kinase inhibitor. Preclinical studies showed that it was approximately 20 to 50 times more active than IM in vitro and active against cell lines bearing all Bcr-Abl mutations other than T315I. Unlike IM, it appears to cross the blood-brain barrier in a murine model system.82
Interferon-alfa as a single agent
The introduction of IM has entirely replaced the use of interferon-alfa as primary treatment for CML in chronic phase. However, for the patient who achieved CCyR on interferon-alfa in the 1990s and maintains stable minimal residual disease, the issue of whether to switch to IM or to continue interferon is controversial, and no useful recommendations can be offered. However, a rising level of BCR-ABL transcripts should suggest the need to change treatment to IM.
Other new agents and experimental combinations
Because first- and second-generation tyrosine kinase inhibitors are inactive against leukemia cells with a T315I mutation, efforts have been directed to developing inhibitory molecules that target cells with this particular mutation.
MK-0457
This agent, previously known as VX-680, is an aurora kinase inhibitor shown in vitro to be active against cell lines carrying the native BCR-ABL fusion gene and also BCR-ABL mutants including the T315I mutation. Aurora kinases are involved in the regulation of chromosome segregation at mitosis and control aspects of the cell cycle. MK-0457 is highly effective in inhibiting growth of tumors in a murine xenograft model. A preliminary report of its use in 3 patients with IM-resistant leukemia and T315I mutations, 2 with CML and one with Ph-positive acute lymphoblastic leukemia, suggests that this drug may prove valuable in suppressing this highly resistant subclone.69
Other new agents
A number of other new agents are in development and some will enter clinical trials before too long. These include ON012380, a small molecule that blocks the Abl substrate binding site; in vitro studies suggest that it is active against all BCR-ABL mutants including the notorious T315I.83 Farnesyl transferase inhibitors (FTI) have some activity in acute leukemia, and preclinical studies suggest that the combination of imatinib with the FTI BMS-214662 may be particularly effective in targeting the quiescent stem cell population84 ; a phase 1/2 clinical study may start soon in the United Kingdom.
Immunotherapy
The convincing demonstration that graft-versus-leukemia plays a central role in leukemia eradication after allogeneic SCT was one of the reasons for rekindling interest in the possible value of immunotherapy outside the context of transplantation. Candidate antigenic targets fall into 3 general categories, leukemia-specific, leukemia-associated, and allogeneic. Because the Bcr-Abl junction codes for a single unique amino acid, vaccine strategies have been developed to target this component of the oncoprotein in the context of HLA restriction. Preliminary reports suggest that patients who have responded to interferon-alfa or imatinib may have further reduction in residual disease following vaccination,85,86 but further controlled studies are required. Other candidate antigens, such as proteinase 3, elastase, Wilms tumor-1, and PRAME, which are not leukemia-specific but may be classified as “associated,” may be targeted in the expectation that residual leukemia may be reduced or eliminated.87,88 The third promising approach is to immunize a patient against minor histocompatibility antigens that may be expressed preferentially on leukemia cells. None of these immunotherapeutic approaches can yet be considered for routine clinical use. In summary, immunotherapy should be offered only in the context of a clinical trial.
Management of patients who relapse after allogeneic stem-cell transplantation
Donor lymphocyte infusions (DLI) are very effective in restoring complete remission for patients who relapse to chronic phase after allogeneic stem-cell transplantation for leukemia, but they may cause graft-versus-host disease (GvHD), which may be life-threatening. Conversely, administration of IM may also induce remissions, but leukemia usually recurs when the drug is stopped.89-91 A possible compromise would be to use IM followed by judicious use of low-dose DLI provided the patient does not already have significant GvHD.
Management of patients who present with advanced-phase disease
Although some patients who present with accelerated-phase disease may fare as well with IM as those treated for chronic-phase disease, in general the response to IM for advanced-phase disease patients is short-lived.92-94 It is logical to start treatment with higher doses of IM than are routinely used for CP disease (eg, 600 or 800 mg daily), and then to proceed at the earliest opportunity to allogeneic stem-cell transplantation93 or standard combination chemotherapy. There is still limited experience with the use of dasatinib or nilotinib as primary treatment for blastic-phase disease,94 but either of these drugs could prove superior to IM. Patients with HLA-matched donors should be considered for allo-SCT.
Acknowledgments
I am grateful to colleagues, especially Drs David Marin, Eduardo Olavarria, and Dragana Milojkovic, who read various drafts of this paper and helped to improve it.
The limit on the number of references means inevitably that I have not been able to cite a number of important papers in the field, and I apologize to the authors. For the same reason, I have chosen in some cases to cite reviews rather than original sources.
Authorship
Conflict-of-interest disclosure: The author declares no competing financial interests.
Correspondence: John M. Goldman, Department of Haematology, Imperial College at Hammersmith Hospital, Du Cane Road, London W12 0NN, United Kingdom; e-mail: jgoldman@imperial.ac.uk.