Abstract
Isolated central nervous system (CNS) relapse involving the brain parenchyma is a rare complication of systemic non-Hodgkin lymphoma. We retrospectively analyzed patient characteristics, management, and outcomes of this complication. After complete response to initial non-Hodgkin lymphoma treatment, patients with isolated CNS relapse with the brain parenchyma as initial relapse site were eligible. Patients with isolated CNS relapse involving only the cerebrospinal fluid were not eligible. Information on 113 patients was assembled from 13 investigators; 94 (83%) had diffuse large B-cell lymphoma. Median time to brain relapse was 1.8 years (range, 0.25-15.9 years). Brain relapse was identified by neuroimaging in all patients; in 54 (48%), diagnostic brain tumor specimen was obtained. Median overall survival from date of brain relapse was 1.6 years (95% confidence interval, 0.9-2.6 years); 26 (23%) have survived 3 years or more. Median time to progression was 1.0 year (95% confidence interval, 0.7-1.7 years). Age less than 60 years (P = .006) at relapse and methotrexate use (P = .008) as front-line treatment for brain relapse were significantly associated with longer survival in a multivariate model. Our results suggest systemic methotrexate is the optimal treatment for isolated CNS relapse involving the brain parenchyma. Long-term survival is possible in some patients.
Introduction
Central nervous system (CNS) relapse occurs in approximately 5% of patients with systemic non-Hodgkin lymphoma and may involve the brain parenchyma, spinal cord, leptomeninges, or eyes.1-4 When CNS relapse occurs during progression or after recurrence of systemic lymphoma, this complication is often an expression of end-stage disease, refractory to most therapeutic strategies.1-3,5,6 In contrast, isolated CNS relapse with no evidence of lymphoma outside the CNS at the time of relapse occurs in approximately 1% of patients with systemic non-Hodgkin lymphoma.2 Isolated CNS disease, as the initial relapse site after a complete response (CR) to systemic treatment, may be potentially treatable.1,2,7-9
This report focuses on patients with systemic non-Hodgkin lymphoma who develop isolated CNS relapse involving the brain parenchyma, a rare relapse site that has not been well characterized.10-13 There has not been a large series report describing clinical characteristics, therapeutic management, and outcomes of patients with brain parenchyma relapse, and there is little information available to guide the clinical management of these patients. The optimal treatment for this complication has not been determined.
The International Primary CNS Lymphoma Collaborative Group (IPCG) is a multidisciplinary group from Europe, North America, and Australia. The IPCG was established in 2002 under the sponsorship of the International Extranodal Lymphoma Study Group.14 Given its rarity, isolated CNS relapse involving the brain parenchyma following initial diagnosis and treatment of systemic non-Hodgkin lymphoma was identified as a complication for which international collaborative work may further our understanding of this disease. We report a retrospective analysis of 113 cases of isolated CNS relapse involving the brain parenchyma.15 The cases were assembled from 13 IPCG investigators in 8 countries.
Methods
A data collection form for information regarding brain parenchyma relapse was sent to investigators affiliated with the IPCG. Requested information included patient characteristics, CNS symptoms which heralded the relapse, date of radiographic evidence of brain disease (or date of brain biopsy if done), Eastern Cooperative Oncology Group Performance Status (ECOG PS) at the time of brain relapse, site and number of brain parenchyma lesion(s), presence or absence of lymphoma cells in the cerebrospinal fluid (CSF), front-line therapeutic management of brain relapse, date and site of disease progression (CNS, systemic or both) after front-line treatment of brain relapse, subsequent salvage treatment (chemotherapy, radiotherapy, both, or none), grade 3 or 4 nonhematologic treatment-related toxicities that occurred after front-line treatment of brain relapse, survival status, and cause of death. In addition, the form requested information regarding clinical characteristics at the initial presentation of systemic non-Hodgkin lymphoma (date of diagnosis, histologic subtype, ECOG PS, serum lactate dehydrogenase (LDH) level, disease stage, extranodal site(s) involved at diagnosis, International Prognostic Index (IPI) score, type of initial therapeutic modality for systemic disease, and response to initial therapy).
Each IPCG investigator received ethics committee approval for the release of case information that was rendered anonymous. After diagnosis and treatment of systemic non-Hodgkin lymphoma, cases with brain parenchyma as the initial relapse site with no evidence of lymphoma elsewhere in the body at the time of brain relapse, and diagnosed be-tween 1980 and 2004, were eligible for this retrospective study. Cases with isolated CNS relapse involving only the CSF and cases with brain, spine, or leptomeningeal involvement at the time of systemic non-Hodgkin lymphoma diagnosis were not eligible. Central pathology review was not performed.
The outcomes evaluated were survival time and time to progression (TTP). Both of these started with the date of diagnosis of brain parenchyma relapse. Survival time was estimated as time to death or time to last date of follow-up for each patient. TTP was estimated to a date of progression. For patients for whom the cause of death was CNS or systemic lymphoma but no date of progression was available or for whom there was an unknown site of progression, the date of death was used as the date of progression.
Descriptive summaries include proportions for categorical variables and medians, minimums, and maximums for numeric variables. For time to event variables (overall survival (OS) and TTP), Kaplan-Meier product limit estimation was used to estimate medians and confidence intervals.16 For stratified analyses, comparisons of 2 or more survival curves across strata (eg, sex) were made using generalized Wilcoxon tests or log-rank tests (if the assumption of proportional hazards were consistent with the graph of the estimated times). Stratification variables included sex, age (less than 60 years vs 60 years or greater), ECOG PS (0 to 2 vs 3 or 4), number of brain lesions (1 vs 2 or more), lesion location (only cerebral hemisphere vs any deep brain), CSF cytology for lymphoma cells (negative vs positive) at the time of brain relapse, and the number of extranodal lesions (0 or 1 vs 2 or more) at the time of systemic disease diagnosis. These variables were tested as potential predictors of survival in univariate analyses. Each of 4 treatment modalities (chemotherapy, methotrexate, whole brain radiotherapy (WBRT), and combinations) were coded as present or absent (ie, there were 4 separate treatment variables) and also tested in univariate models. Cox proportional hazards models were used to compare 2 or more stratification variables. A variable selection scheme minimizing Akaike's Information Criterion was used to estimate the best multivariable model.16 All analyses were run using SAS Version 9.1 for Windows (SAS Institute, Cary, NC).
Results
Information regarding a total of 113 patients was assembled. The patients had achieved CR after initial treatment of systemic non-Hodgkin lymphoma, and all had radiographic evidence of brain parenchyma disease with no obvious evidence of HIV-1 infection. CSF cytology was reported in 67 patients (60%); 11 of the 67 (16%) had malignant cells in the CSF. Three patients were reported to have ocular involvement at the time of brain relapse; however, the total number of patients clinically evaluated for ocular involvement in this series is not known.
Clinical features
Patient characteristics at initial presentation of systemic non-Hodgkin lymphoma are summarized in Table 1. A total of 94 patients (83%) had diffuse large B-cell lymphoma (DLBCL), 5 patients (4%) had follicular lymphoma, 3 patients (3%) had Burkitt lymphoma, 2 patients (2%) had small lymphocytic lymphoma, 5 patients had other histologic subtypes, and in 4 patients the histologic subtype was not specified. The median age at systemic non-Hodgkin lymphoma diagnosis was 61 years (range, 16-85 years). Sixty patients (53%) were 60 years of age or older. The IPI was reported in 63 patients (56%); 34 of the 63 patients (54%) had intermediate to high or high IPI (defined by the presence of more than 2 of the IPI prognostic factors, that is, age more than 60 years, stage III/IV disease, elevated LDH, ECOG PS 2 or more, and more than one extranodal site of disease) at diagnosis. Serum LDH was reported in 56 patients (50%); 33 of the 56 patients (59%) had elevated LDH. Number of extranodal sites was reported in 98 patients (87%); 86 of the 98 patients (88%) had extranodal disease at diagnosis and 29 (30%) had involvement of 2 or more extranodal sites.
Nineteen patients (17%) were diagnosed and received treatment for systemic non-Hodgkin lymphoma during the years 1980 to 1990, 59 patients (52%) were diagnosed and received treatment between 1990 and 1999, and 35 patients (31%) between 2000 and 2004. The therapeutic regimens used as initial treatment are summarized in Table 2; 45 patients (40%) received cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP), and 28 patients (25%) received rituximab plus CHOP (R-CHOP). In addition to systemic chemotherapy, 7 patients (6%) received intrathecal methotrexate (n = 6) or intrathecal cytarabine (n = 1).
The median time from systemic non-Hodgkin lymphoma diagnosis to brain parenchyma relapse was 1.8 years (range, 0.25-15.9 years). Seventy-six patients (67%) relapsed in the brain parenchyma less than 3 years after the diagnosis of systemic non-Hodgkin lymphoma. The patient characteristics regarding brain parenchyma relapse are summarized in Table 3. The median age at the time of brain relapse was 65 years (range, 19-85 years). Seventy patients (62%) were 60 years of age or older. Median ECOG PS at brain relapse was 2 (not reported in 18 patients), and 44 patients (39%) had a PS greater than 2. Neurologic symptoms that heralded brain relapse are summarized in Table 3. Forty-three patients (38%) had neurologic symptoms in more than one category.
Brain parenchyma relapse was identified by brain imaging (computed tomography [CT] or magnetic resonance imaging [MRI]) in all patients. A diagnostic brain tumor sample was obtained in 54 of the 113 patients (48%). The original brain biopsy pathology reports were available in 42 of the 54 patients. In 21 patients, the brain biopsy histopathology was described as “diffuse large B-cell,” in 11 patients as “large B-cell,” and in 1 patient as “T-cell, large cell.” In 8 patients, the pathology was reported as “large cell lymphoma” without phenotypic description. One pathology report listed “brain lymphoma” without cellular or phenotypic description. In 12 patients, information regarding the brain biopsy histology was extracted from databases or other medical records. In 11 of the 12 patients, the histopathology was coded or described as “diffuse large B-cell” and in 1 patient as “large cell anaplastic lymphoma.”
Based on the data that were reported, in 47 of the 54 patients who underwent diagnostic brain tumor biopsy, the brain tumor pathology was compatible with the histology of the systemic lymphoma. Of the remaining 7 patients, 2 had histologic subtype of small lymphocytic lymphoma at systemic diagnosis and 1 patient had follicular lymphoma; in 4 patients, the histologic subtype at systemic lymphoma diagnosis was not reported. However, we did not centrally review and compare histopathologic samples as part of this study.
A total of 56 patients (50%) had 2 or more brain lesions at the time of brain relapse. Forty-five patients (40%) had involvement of deep brain structures such as the basal ganglia, brainstem, corpus callosum, and cerebellum. CSF cytology was reported in 67 patients (60%). Bulky disease and large lesions in the brain parenchyma may have been a contraindication to performing lumbar puncture in some patients and may account for some of the missing values for CSF cytology.
Therapeutic management of brain relapse
Front-line treatment for brain parenchyma relapse was chemotherapy with or without WBRT in 78 patients (69%). A total of 34 patients (30%) received WBRT without chemotherapy. One patient had surgical resection of the brain lesion, did not receive chemotherapy or radiotherapy, and was not included in the statistical analyses of treatment–related characteristics. Details of the front-line treatments for brain relapse are summarized in Table 4.
Methotrexate was the most commonly used drug (n = 71), either alone (n = 12) or in combination with other drugs (n = 59). Methotrexate was administered intravenously in 52 patients. In 11 patients, methotrexate was administered intravenously or intra-arterially with osmotic blood-brain barrier disruption (BBBD). The intravenous (or intra-arterial) dose of methotrexate ranged from 1 g/m2 to 8 g/m2 (median, 3.5 g/m2), and the number of methotrexate courses ranged from 1 to 12. In 11 patients, the methotrexate was administered intrathecally, either with intravenous methotrexate (n = 3) or without intravenous methotrexate (n = 8). Sixteen patients (14%) received intrathecal cytarabine as part of front-line treatment of brain relapse, and 9 patients (8%) received rituximab, administered either intravenously (n = 7) or intrathecally (n = 2). Ten patients underwent high-dose chemotherapy with peripheral blood stem cell or marrow transplantation after treatment with methotrexate (n = 9) or radiotherapy (n = 1). An additional 7 patients were treated with other chemotherapy regimens that did not include methotrexate (Table 4).
Sixty patients (53%) received WBRT with or without chemotherapy. In these patients, the radiation dose ranged from 6 to 54 Gy (median, 30 Gy), and the number of fractions ranged from 2 to 25 (median, 20 fractions). Three patients with ocular lymphoma at the time of brain relapse were treated with ocular radiotherapy (n = 2) or intravenous methotrexate (n = 1).
Outcome
A total of 78 patients (69%) have died. The causes of death are summarized in Table 5. Fifty-eight of the 78 patients (74%) died of disease progression, with CNS disease as the cause of death in 49 of 78 patients (63%) and both CNS and systemic disease as the cause of death in 5 more (6%). In 12 of 78 patients (15%), the cause of death was treatment–related toxicity, either CNS toxicity (n = 6) or systemic (n = 6). The treatment–related CNS toxicities were dementia (n = 3), leukoencephalopathy (n = 1), Brown-Sequard syndrome (n = 1), and not specified (n = 1); and the systemic toxicities were septic shock (n = 3), liver failure (n = 1), pancytopenia (n = 1), and not specified (n = 1). Of the 35 patients alive at data cut-off, 13 had evidence of disease progression.
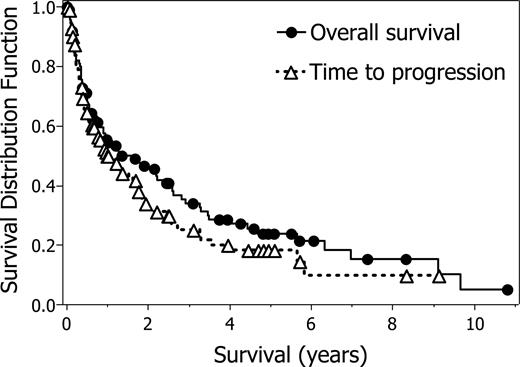
The median OS calculated from the date of brain relapse for all patients was 1.6 years (95% confidence interval [CI], 0.9-2.6 years), and the median time to disease progression was 1.0 years (95% CI, 0.7-1.7 years) (Figure 1). Twenty-six patients (23%) have survived 3 years or more after brain relapse, 18 patients (16%) have survived 4 years or more, and 12 patients (11%) have survived 5 years or more after relapse.
Overall outcome. Time to progression (median 1.0 year; 95% CI, 0.7-1.7 years) and overall survival (median 1.6 years; 95% CI, 0.9-2.6 years) from date of brain parenchyma relapse (113 patients, 78 deaths). Symbols indicate censored observations.
Overall outcome. Time to progression (median 1.0 year; 95% CI, 0.7-1.7 years) and overall survival (median 1.6 years; 95% CI, 0.9-2.6 years) from date of brain parenchyma relapse (113 patients, 78 deaths). Symbols indicate censored observations.
After front-line treatment of brain relapse, 77 of 113 (68%) patients developed disease progression. In 56 of the 77 patients (73%), the site of progression was the CNS; 11 of 77 patients (14%) progressed systemically; and 7 of 77 (9%) progressed in both the CNS and systemically. The site of progression was unknown in 3 patients (3%). Salvage treatment was administered in 30 patients. This consisted of chemotherapy in 18 patients, radiotherapy in 7 patients, and combined modalities in 5 patients.
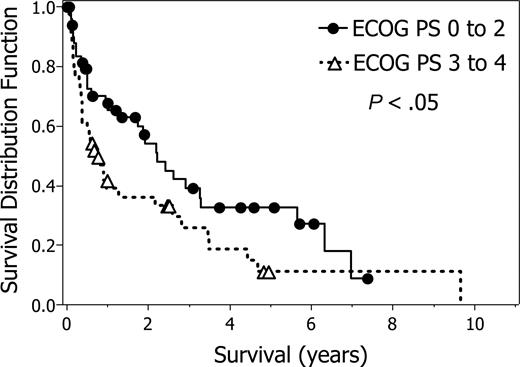
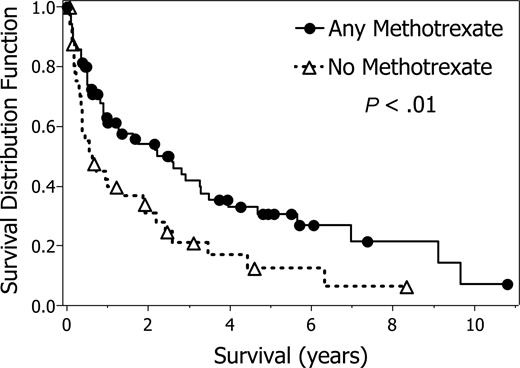
Age (< 60 years vs ≥ 60 years) (P = .0055), PS (0 to 2 vs 3 or 4) (P = .033), and CSF cytology for lymphoma cells (negative vs positive) (P = .048) at brain relapse; and number of extranodal lesions (0 or 1 vs 2 or more) (P = .0037) at initial diagnosis, were significantly associated with survival, whereas the other 3 potential predictors were not significant (P > .15). Survival plots stratified by age and by PS are shown in Figures 2 and 3, respectively. Among the treatment–related variables, treatment that included methotrexate (yes vs no) (P = .0076) and treatment with any chemotherapy (yes vs no) (P = .019) as front-line treatment for brain relapse are significant predictors of survival, whereas WBRT (yes vs no) and WBRT with methotrexate (both vs all other) were not significant (P = .20 and P = .16, respectively). Survival for front-line methotrexate treatment for brain relapse is shown in Figure 4. The comparison of the survival curves across strata for the baseline characteristics and for the front-line treatment variables for brain relapse as potential predictors of survival are summarized in Table 6.
Survival according to age. Survival from date of brain parenchyma relapse stratified by age at relapse, less than 60 years (43 patients) or greater than or equal to 60 years (70 patients; P = .006). Symbols indicate censored observations.
Survival according to age. Survival from date of brain parenchyma relapse stratified by age at relapse, less than 60 years (43 patients) or greater than or equal to 60 years (70 patients; P = .006). Symbols indicate censored observations.
Survival according to Eastern Cooperative Oncology Group Performance Status (ECOG PS). Survival from date of brain parenchyma relapse stratified by ECOG PS at relapse, PS 0 to 2 (51 patients) or PS 3 and 4 (44 patients) (P = .033). Performance status was not reported in 18 patients. Symbols indicate censored observations.
Survival according to Eastern Cooperative Oncology Group Performance Status (ECOG PS). Survival from date of brain parenchyma relapse stratified by ECOG PS at relapse, PS 0 to 2 (51 patients) or PS 3 and 4 (44 patients) (P = .033). Performance status was not reported in 18 patients. Symbols indicate censored observations.
Survival according to methotrexate treatment. Survival from date of brain parenchyma relapse stratified by front-line treatment with methotrexate at relapse, any methotrexate (71 patients) or no methotrexate (42 patients) (P = .0076). Symbols indicate censored observations.
Survival according to methotrexate treatment. Survival from date of brain parenchyma relapse stratified by front-line treatment with methotrexate at relapse, any methotrexate (71 patients) or no methotrexate (42 patients) (P = .0076). Symbols indicate censored observations.
Although this report summarizes the experience of a large number of patients, this is a case series with potential weaknesses, including selection bias and confounding. Additional analyses were undertaken to address these issues, to the limits of data availability. With respect to confounding, if patients who received methotrexate had less severe disease or were younger than those who did not receive methotrexate, this could explain the improved survival in those treated with methotrexate. Because PS is missing in 16% of the patients and the number of extranodal lesions is missing in 13% of the patients, the best model using these 2 variables and age less than 60 years was estimated. This best model contained only age; the other 2 variables were not significant once age less than 60 years was included in the model. That is, the other 2 variables were not significant once one controlled for age. A proportional hazards model was fit that included age 60 years or older (hazard ratio = 1.85, P = .016) and methotrexate (hazard ratio = 0.588, P = .024). Thus, methotrexate is a significant predictor when one controls for age.
Another potential bias may occur from inclusion of histologic subtypes other than DLBCL. Survival curves were estimated for only patients diagnosed with DLBCL (n = 94), and these curves were very similar to estimates from the survival curves for the full series (n = 113). Similarly, 8 of the 113 patients received intrathecal methotrexate alone, with no systemic (intravenous or intra-arterial) methotrexate. Survival curves comparing systemic methotrexate to all others (that is, placing those who received intrathecal methotrexate alone into the no-methotrexate group) were estimated. The survival curves, the estimated median survival times, and the tests comparing intravenous or intra-arterial methotrexate to all others were similar to the comparison of intravenous or intra-arterial methotrexate including intrathecal methotrexate, with all others. Thus, inclusion of patients with histologic subtypes other than DLBCL and inclusion of patients who received intrathecal methotrexate alone with patients who received systemic methotrexate did not change the results. Although these additional analyses do not address all issues related to potential confounding and bias with respect to the association of methotrexate with improved survival, they are consistent with improved survival of patients treated with methotrexate.
For TTP, the only significant baseline predictors were number of extranodal lesions (0 or 1 vs 2 or more) (P = .001) at initial diagnosis and PS (0 to 2 vs 3 or 4) (P = .032) at brain relapse. However, neither of these was significant in a univariate proportional hazards model. Among the treatment–related variables, treatment with methotrexate (P = .012), treatment with any chemotherapy (P = .018), and treatment with both methotrexate and WBRT (P = .019) were all significant. The best predictive model for TTP is the single-variable model with methotrexate plus WBRT vs all other treatments (hazard ratio 0.45, P = .013).
Toxicity
Grade 3 and 4 treatment–related nonhematologic toxicities occurred in 17 patients treated with chemotherapy alone as front-line treatment for brain relapse. Systemic toxicities were infection (n = 6), renal (n = 4), hepatic (n = 2), and gastrointestinal (n = 1). Four patients had neurologic complications, including leukoencephalopathy (n = 1), arachnoiditis (n = 1), paraplegia (n = 1), and steroid-induced confusion (n = 1). Eight patients treated with chemotherapy and WBRT for brain relapse developed grade 3 and 4 neurologic toxicity, including leukoencephalopathy (n = 4), dementia (n = 1), transient ischemic attack (n = 1), and Brown-Sequard syndrome (n = 1); and one patient developed sepsis. Six patients treated with WBRT alone at relapse developed grade 3 and 4 neurologic toxicity; 5 of the 6 patients developed dementia and one patient had a transient ischemic attack.
Patients surviving more than 2.5 years
Thirty-one patients (27%) survived longer than the upper limit for the 95% CI for median survival time (2.5 years) from the date of brain relapse (Table 7). Methotrexate was administered as front-line treatment for brain relapse in 24 of the 31 patients (77%); in22 patients, at a dose of 3.5 g/m2 or more. In 18 patients, the methotrexate was administered intravenously; in 5 patients, intravenous or intra-arterial in conjunction with osmotic BBBD; and in 1 patient intrathecally. After methotrexate, 5 long-term survivors received high-dose chemotherapy with peripheral blood stem cell or marrow transplantation. Two of the 5 patients received chemotherapy in conjunction with BBBD before peripheral blood stem cell or marrow transplantation. WBRT was administered to 16 of the 31 patients (52%). Twenty of the 31 patients developed disease progression; in 15 of the 20, the site of progression was the CNS.
Discussion
Several studies of homogeneously treated patients with non-Hodgkin lymphoma have assessed the incidence and risk factors for isolated CNS relapse.1,17-20 Although retrospective, our international collaboration allowed us to assemble the largest series to date of patients with CNS relapse in the brain parenchyma as initial relapse site. Our eligibility criteria were very select. For example, in the setting of isolated CNS relapse, patients must have had brain parenchyma involvement assessed by neuro-imaging; and patients with only CSF involvement at relapse were not eligible. These strict criteria may partially explain the longer median time from systemic non-Hodgkin lymphoma diagnosis to brain relapse and the longer overall survival in our series, compared with other series.1,17-20 Participating IPCG investigators searched their databases and registries for eligible patients between the years 1980 and 2004 and submitted available information. The dataset is not comprehensive, contains missing values, may not be representative, and cannot determine the incidence of this complication. Patient evaluation and therapeutic management were heterogenous across participating centers and across more than 2 decades; thus, prognostic analysis is subject to bias. The authors acknowledge these limitations; nevertheless, certain patient- and treatment-related findings may be helpful to the clinician managing this rare complication.
The neurologic symptoms that heralded isolated CNS relapse in our series were similar to those reported by other investigators.18,21,22 Patients with suspected brain relapse require urgent contrast-enhanced MRI of the cerebrospinal axis,10 CSF cytopathology, and ophthalmologic examination. Because isolated CNS relapse of systemic non-Hodgkin lymphoma rarely involves the brain parenchyma, if single or multiple brain lesions are identified on neuroimaging, then pathologic verification by stereotactic biopsy is recommended.10
The median OS in this series was 1.6 years. Among the treatment-related characteristics, treatment with methotrexate (P = .008) and treatment with chemotherapy (P = .019) were significantly associated with survival. When added to the regression model with age included, treatment with methotrexate remains significant (P = .024). The best predictor of TTP was treatment with methotrexate plus WBRT (ie, combination therapy prolonged TTP). This information suggests that methotrexate-based regimens should be considered for patients with brain parenchyma relapse. Although WBRT is effective for the initial control of CNS lymphoma, it is associated with an increased likelihood of delayed treatment-related neurotoxicity, especially in patients older than 60 years.23-25 Minimizing the risk of treatment-related neurotoxicity is a very important therapeutic objective in patients with isolated CNS relapse.
In our series, the CNS was the main site of disease progression and CNS lymphoma was the main cause of death. The tendency for consecutive relapse or progression in the CNS supports the importance of intensive therapy with CNS penetrating agents to control brain parenchyma progression,26 as well as intensive systemic therapy to prevent future systemic relapse.7,13,27,28 Encouraging results have been reported with the use of dose intensive chemotherapy in relapsed primary CNS lymphoma (PCNSL).29 CNS-directed therapy, such as enhanced chemotherapy delivery with BBBD, may improve disease response and survival by increasing drug delivery to the CNS.26,30 In our series, 8 of 31 patients who survived more than 2.5 years received either methotrexate (intravenously) followed by consolidation with high-dose chemotherapy and peripheral blood stem cell transplantation; or methotrexate (intraarterially or intravenously) in conjunction with osmotic BBBD, as treatment for brain relapse (Table 7).
There are similarities between patients in our series and patients with PCNSL. Age and PS have been reported as the 2 most consistent prognostic factors in predicting survival in PCNSL.31,32 Similarly, our study supports the role of age and PS as prognostic factors in predicting survival in patients with brain parenchyma relapse. The majority of PCNSL are of B-cell origin. A total of 94 patients (83%) in our series had DLBCL at presentation. Diagnostic brain tumor sample was obtained in 54 patients; tumor histopathology was confirmed as B-cell phenotype in 43 of the 54 patients. Symptoms at disease presentation are comparable and primarily neurologic, rather than systemic “B” symptoms, such as fever, weight loss, and night sweats. Similar to PCNSL, the majority of patients (67%) presented with lesions in the cerebral hemispheres. Involvement of deep brain structures was not associated with a significant difference in outcome in our series.
Several studies have reported an increased risk of CNS relapse associated with factors such as more than one site of extranodal disease, elevated LDH, and high-risk IPI at the time of non-Hodgkin lymphoma diagnosis.1,4,17,19,20 In our series, the available data showed that 54% of the patients had intermediate to high or high IPI score and 59% had elevated LDH at diagnosis. The incidence of initial extranodal involvement was exceedingly high in our series (88%), with 30% having 2 or more extranodal sites, including sites often considered to be at high-risk for subsequent CNS relapse.7,28 However, initial prophylactic treatment was reported only in a minority of patients. Although the aim of our study was not to identify patients at risk for brain relapse, the available data suggest the need for CNS prophylaxis in high-risk patients. Of note, the propensity for testicular non-Hodgkin lymphoma to involve the CNS at relapse is well known; this frequently occurs as isolated relapse and often involves the brain parenchyma.7,28 The baseline patient characteristics in our series suggest that a wide range of extranodal sites may be present at diagnosis in patients who later develop isolated brain relapse.1,3
Indeed, involvement of more than one extranodal site as well as an elevated IPI score and increased LDH level have been confirmed as independent risk factors in recent large series.33,34 However, the identification of patients who actually need CNS prophylaxis and the best prophylactic modalities remain uncertain.4,9,12,13,19,34-36 The effectiveness of intrathecal prophylaxis is judged controversially,33,37 but there is some evidence of good efficacy when intrathecal chemotherapy and high-dose systemic methotrexate are used in combination.34-36 On the other hand, high-dose systemic methotrexate may adequately treat the meningeal involvement, and the combination with intrathecal treatment may increase the risk of unwanted side effects. This issue is clinically relevant and worthy of further investigation because patients who do not need it should not be exposed to the potential complications associated with CNS prophylaxis.
Our series includes 19 patients (17%) diagnosed and treated for systemic non-Hodgkin lymphoma between 1980 and 1990 and 94 patients (83%) diagnosed and treated between 1990 and 2004. The difference in the number of patients across decades may be the result of the difficulty retrieving information on patients diagnosed 2 decades ago and more, and possibly also the result of the increased use of modern neuroimaging techniques.10 In combination with these possible factors, the use of monoclonal antibodies has transformed therapeutic approaches and has led to marked improvement in clinical outcomes for patients with DLBCL. The addition of rituximab to CHOP chemotherapy (R-CHOP) has significantly improved survival and has been adopted as the new standard of care for patients with this disease.38,39 However, the addition of intravenous rituximab does not appear to influence the risk of CNS relapse, possibly because of poor CNS penetration.2,40,41 As survival improves, new therapeutic approaches may better control systemic lymphoma. However, these novel treatments may not necessarily affect the CNS as a potential disease sanctuary; therefore, brain parenchyma involvement may in the future become more frequently the cause of treatment failure,9,42-44 and the development of effective prophylactic strategies may play a larger role.
The rarity of brain parenchyma relapse makes prospective studies of this complication difficult to perform. International collaboration across several specialties is essential to advance the understanding and management of this complication. It is currently unknown whether late delayed involvement of the CNS represents a true recurrence of the original systemic lymphoma, or rather a second new lymphoma.45 Further understanding of the genetic and molecular characteristics of CNS relapse may help answer this question and in the future may assist clinicians in selecting the appropriate treatment for individual patients.45 New therapeutic approaches aimed at penetrating the CNS to achieve durable CNS responses while maintaining systemic disease control are essential.
The online version of this article contains a data supplement.
Presented as a poster at the 48th annual meeting of the American Society of Hematology, Orlando, FL, December 10, 2006.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Dr James Armitage, Dr Franco Cavalli, and Dr Joseph Connors for their encouragement to study brain parenchyma involvement in the setting of isolated CNS relapse of systemic non-Hodgkin lymphoma.
Authorship
Contribution: N.D.D. designed research, collected data, analyzed data, and wrote the manuscript; L.E.A., T.N.S., T.S., J.E.C.B., E.A.N., C.S., K.J., P.J., G.I., D.S., T.B., and S.M. collected data and reviewed the manuscript; D.F.K performed statistical analysis and reviewed the manuscript; and E.Z. designed research, collected data, and reviewed the manuscript.
A complete list of the members of the International Primary CNS Lymphoma Collaborative Group appears in Document S1, available on the Blood website; see the Supplemental Materials link at the top of the online article.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Nancy D. Doolittle, Department of Neurology, L 603, Oregon Health and Science University, 3181 SW Sam Jackson Park Rd, Portland, OR 97239; e-mail: doolittl@ohsu.edu.