Abstract
Mice defective in both granulocyte colony-stimulating factor (G-CSF) and granulocyte-macrophage colony-stimulating factor (GM-CSF) have severely impaired neutrophil production and function, yet these mice respond to acute pathogen challenge with a significant neutrophil response. We have recently reported the development of an in vitro system to detect granulopoietic cytokines secreted from cells isolated from G-CSF, GM-CSF double knockout mice. The conditioned media produced by these cells after stimulation with lipopolysaccharide or Candida albicans supports the production and differentiation of granulocytes (ie, the conditioned media contains neutrophil promoting activity [NPA]). We now show that the NPA in the G-CSF−/−/GM-CSF−/− conditioned media requires interleukin-6 (IL6), is abolished by soluble gp130, and can be specifically immunodepleted by an anti-IL6R antibody. NPA effects on bone marrow cells are also mimicked by Hyper-IL6, and the soluble IL6R is present in NPA. These results show that the IL6/sIL6R complex is the major effector of NPA. NPA production by mice defective for both G-CSF and GM-CSF uncovers an alternative pathway to granulocyte production, which is activated after exposure to pathogens.
Introduction
Neutrophils and monocytes play a pivotal role in host defenses against bacterial and fungal infections. The main modulators of granulocyte production and activation are the classic hemopoietic cytokines granulocyte-macrophage colony-stimulating factor (GM-CSF) and granulocyte colony-stimulating factor (G-CSF).1-4 Indeed, several studies have shown that mice defective in both G-CSF and GM-CSF have profound chronic neutropenia, granulocyte, and macrophage progenitor cell deficiency, impaired neutrophil mobilization, impaired reproductive capacity, perturbed neonatal granulopoiesis, and amyloidosis.5-7 However, acute challenge of G-CSF−/− and GM-CSF−/− mice with pathogens, such as Candida albicans, results in elevated numbers of monocyte and granulocyte progenitor cells in the bone marrow and in a significant peripheral neutrophilia,8 suggesting that there must be alternative regulators of neutrophil production in response to acute inflammatory challenges.
We have reported recently that conditioned media (CM) from mouse embryo fibroblasts (MEFs) derived from compound G-CSF−/−/GM-CSF−/− animals exposed to lipopolysaccharide (LPS) or heat-inactivated C albicans stimulate a mixed population of myeloid progenitor cells to produce mature neutrophils in vitro.9 Thus, cytokines other than G- and GM-CSF, produced by MEFs in response to LPS challenge, can stimulate neutrophil production and function. We have ruled out the contribution of some cytokines, including interleukin-3 (IL3), SCF, MIP1α, and RANTES,9 to this neutrophil-promoting activity (NPA) Surprisingly, we uncovered a critical role for M-CSF in the production of NPA; however, M-CSF itself is not sufficient for the generation of neutrophils in vitro from myeloid progenitor cells of compound mutant G-CSF−/−, GM-CSF−/− mice.9
IL6 levels are elevated in the CM collected from LPS-stimulated MEFs of G-CSF−/−/GM-CSF−/− mice. However, addition of IL6 directly to the bone marrow cells or to NPA-negative CM (ie, non–LPS-stimulated MEFs derived from compound G-CSF−/−, GM-CSF−/−), while increasing granulocyte clusters, does not restore NPA levels.9 IL6 is known to promote neutrophil production both in vitro and in vivo and may exert its effects in conjunction with G-CSF,10 particularly during emergency granulopoiesis.11 IL6 signals by binding to the transmembrane ligand binding receptor α subunit (IL6R) followed by higher-order receptor oligomerization with the signaling β-receptor subunit gp130. In addition, cells that do not express endogenous IL6R (eg, embryonic stem cells12 and hemopoietic progenitor cells13,14 ) will respond to IL6 if the cytokine is complexed to a processed soluble version of IL6R (sIL6R) supplied by other cells in a mechanism referred to as “transsignaling.”15 Expansion of the spectrum of IL6 responsive cells via transsignaling is particularly relevant to granulopoiesis: indeed, sIL6R and IL6 double-transgenic mice, which overexpress both proteins, develop extramedullary hemopoiesis, with predominant granulocytic differentiation in the liver.16 Thus, whereas purified IL6 cannot replace NPA in the in vitro generation of neutrophils,9 we have investigated the relationship between NPA, classic IL6 signaling, and IL6 transsignaling.
IL6 has been previously shown to be dispensable for granulopoiesis in G-CSF–deficient mice8,17 ; however, bone marrow cells from these mice generate significant numbers of neutrophils in vitro when cultured in the presence of GM-CSF, raising the possibility that GM-CSF contributes to maintaining granulopoiesis in compound mutant IL6−/−/G-CSF−/− mice. To simultaneously ablate both major sources of granulocytic cytokines, we conducted our present study using cells from G-CSF−/−/GM-CSF−/− compound mutant mice.
Here, we report that cells simultaneously lacking the genes encoding IL6, G-CSF, and GM-CSF (ie, triple-knockout mice) do not produce NPA in response to LPS. However, NPA in media conditioned by LPS-challenged cells from G-CSF−/−/GM-CSF −/− mice cannot be neutralized by anti-IL6 antibodies. For the first time, we show that NPA can be mimicked by the designer cytokine Hyper-IL6, comprising a fusion protein between IL6 and the sIL6R, and is abolished by the specific sIL6R antagonist, soluble gp130Fc (sgp130Fc), which sequesters the soluble IL6/sIL6R complex but does not affect the membrane-associated IL6/IL6R complex. These results suggest that the sIL6R/IL6 complex is necessary for NPA. We demonstrate that immunologically detectable sIL6R is present in active, highly enriched prepara-tions of NPA and that NPA is specifically immunodepleted by anti-IL6R antibodies.
Thus, the absence of both the “classic” neutrophil promoting cytokines, G-CSF and GM-CSF, unmasks a third neutrophil-promoting activity, the bioactive sIL6R/IL-6 complex. We propose that IL6 transsignaling plays an important role during emergency granulopoiesis, whereas G-CSF and GM-CSF are required to maintain steady-state granulopoiesis.
Methods
Reagents
Purified IL6 was obtained from Chemicon International (Temecula, CA); goat antimouse IL6R (AF1830) antibody was purchased from R&D Systems (Minneapolis, MN); hyper-IL618 and sg130Fc19 were prepared as described. Purified, recombinant sIL6R and polyclonal neutralizing anti-IL6 antibody were a gift from Dr Robert Moritz (Ludwig Institute for Cancer Research, Melbourne, Australia). LPS from Escherichia coli 0127:B8 was purchased from Sigma-Aldrich (St Louis, MO). The neutralizing IL6R Ab LEAF antimouse CD126 (anti IL6R, clone D7715A7 from BioLegend, San Diego, CA), was used for immunodepletions, and the goat antimouse IL6R (AF 1830 from R&D Systems) was used for immunoblotting. Anti-EGFR monoclonal antibody 528 was purified from hybridoma supernatant fluid.
Animals
G-CSF−/−/GM-CSF−/− mice20 and G-CSF−/−/GM-CSF−/−/IL6−/− mice were used for these studies.
GM-CSF−/−/G-CSF−/−/IL6−/− mice were generated by intercrossing IL-6−/− mice21 with G-CSF−/−/GM-CSF−/− mice. Genotyping for IL6 was conducted using the following primers:
P1 (mutant, sense): TTC, TCA, TTT, CCA, CGA, TTT, CCC, AG
P2 (wildtype, sense): TTC, CAT, CCA, GTT, GCC, TTC, TTG, G
MK 3.3B (common, antisense): GAC, CGC, TTC, CTG, GTG, CTT, TAC, GGT
G-CSF−/−, GM-CSF−/−, IL6−/− mice were housed in a micro-isolator facility and at weaning their progeny were treated orally for 2 weeks with 175 mg/L Enrofloxacin (Baytril antibiotic, Lyppard Pharmaceuticals, Cheltenham, Australia).
All animal experiments were conducted according to the guidelines of the National Health and Medical Research Council of Australia. All animal procedures were approved by the Ludwig Institute & Department of Surgery Animal Ethics Committee.
Murine embryonic fibroblast culture
G-CSF−/−/GM-CSF−/− or G-CSF−/−/GM-CSF−/−/IL6−/− pregnant female mice were killed on the 13th to 15th day of pregnancy by cervical dislocation. Embryonic carcasses, after removal of soft tissues, were digested in trypsin at 37°C for 30 minutes followed by overnight incubation at 4°C. Embryonic fibroblasts were cultured in Dulbecco modified Eagle medium (DMEM) containing 15% heat inactivated fetal calf serum (FCS) and were passaged on reaching confluence at a 1:3 dilution. Cells from individual embryos were also collected at this time for genotyping at the GM-CSF, G-CSF, and IL6 loci by polymerase chain reaction analysis.
G-CSF−/−/GM-CSF−/− fibroblasts, immortalized with the SV40 antigen as described,9 were routinely passaged in DMEM supplemented with 10% FCS.
Production of CM
Embryonic fibroblasts at P2, or SV40-transfected G-CSF−/−/GM-CSF−/− embryonic fibroblasts, were seeded at 107 in 175 cm2 flask in phenol red-free DMEM (Invitrogen, Carlsbad, CA) supplemented with 1% human albumin solution (CSL, Melbourne, Australia) and 1 mM sodium pyruvate (Invitrogen). Cells were stimulated with LPS (0.05 μg/mL), and CM were harvested after 48 hours as described.9
NPA assay
Bone marrow cells from G-CSF−/−/GM-CSF−/− were enriched for myeloid progenitors as described.9 Cells were cultured in 8-well LabTek chamber slides (Nalge Nunc International, Rochester, NY) at 5 × 103 cells/well in a total volume of 200 μL of 1:1 RPMI and IMEM supplemented with 10% heat-inactivated FCS and nonessential amino acids (Invitrogen). After 4 days in culture, the slides were stained with May-Grünwald/Giemsa (Merck, Darmstadt, Germany) and examined using a Nikon Microphot-FX microscope. Granulocyte clusters, containing between 5 and 50 cells, were identified by morphology or by specific staining with naphthol AS-D chloroacetate esterase.9 NPA is expressed in units per milliliter, where 1 unit is the activity required to generate 1 granulocyte cluster from 5 × 103 bone marrow cells after 4 days in liquid culture.
Partial purification of NPA
A total of 1.5 L of filtered CM was pumped through an 800 mL Blue Sepharose 6FF column (GE Healthcare Bio-Sciences, Uppsala, Sweden) at a flow rate of 7.5 mL/min at 4°C. The column was washed with 20 mM Tris HCl pH 7.4/0.005% (v/v) Tween 20, eluted with the same buffer containing 1 M NaCl, followed by further elution with a 2 M NaCl buffer. Samples of breakthrough, wash and eluate were taken for NPA assay. This procedure was repeated with a further 1.5L CM. The active fractions (breakthrough and wash) were concentrated (×100) on Vivaspin 5000 molecular weight cut-off filters (VivaScience, Hanover, Germany) and 1 mL was loaded onto a Superose 12 HR 10/30 column (GE Healthcare Bio-Sciences) and eluted with phosphate-buffered saline (PBS)/0.005% Tween 20, at a flow rate of 0.25 mL/min at 23°C. Samples of the fractions were assayed in the NPA assay. Two distinct peaks of NPA were detected: pool A was a higher molecular weight species, containing less overall protein, and pool B included the major UV absorbing peak. The remainder of the concentrate was treated in the same way, and all of the active fractions were combined to form pool A or pool B. A sample of pool A was concentrated and buffer exchanged as previously before running on a MonoQ 5/50 GL column (GE Healthcare Bio-Sciences). Proteins were eluted with a linear gradient from 20 mM Tris HCl, pH 7.4/0.005% (v/v) Tween 20 to 20 mM Tris HCl, pH 7.4/500 mM NaCl/0.005% (v/v) Tween 20 over 90 minutes, at a flow rate of 0.5 mL/min and a column temperature of 23°C. Samples of the fractions were assayed, and the procedure was repeated with the remainder of pool A. A flow chart of the purification is shown in Figure S1 (available on the Blood website; see the Supplemental Materials link at the top of the online article).
Immunodetection of sIL6-R
Active fractions from Mono-Q chromatography were pooled and concentrated 20-fold using Vivaspin concentrators (5000 molecular weight cutoff, VivaScience). Purified recombinant sIL6-R (20 ng/lane), NPA-containing CM (40 μL/lane), Superose-12 active pool (40 μL/lane), and concentrated (Vivaspin) Mono-Q active pool (40 μL/lane) were loaded on a 4% to 12% Bis-Tris gel (Novex, Invitrogen). Proteins were transferred electrophoretically to PVDF membrane (Millipore, Billerica, MA), and the membrane was probed with anti-IL6R antibody AF1830. Immunoreactive bands were visualized by chemiluminescence.
Neutralization of NPA by antibodies and soluble proteins
Fractions containing NPA or recombinant murine IL6 were preincubated with anti-IL6 antibody or with sgp130-Fc (0.25-4.8 nM) at 37°C for 30 minutes in chamber slides before adding the bone marrow cells. Immunodepletion of active NPA fractions was performed with antibodies to the IL6R (LEAF antimouse CD126) or, as a control, antibodies to the EGFR (mAb528). Duplicate samples (0.5-0.9 mL) were incubated with either the IL6R or EGFR antibodies (both at 1 μg/tube) for 2 hours at room temperature, followed by incubation with Protein G beads for 45 minutes. Starting materials (no immunodepletion) and immunodepleted samples were adjusted for dilution factors and tested for residual NPA in the assay described.
Results
LPS enhances neutrophils and monocytes production in G-CSF−/−/GM-CSF−/− mice
We have shown previously that mutant G-CSF−/− mice develop neutrophilia after exposure to C albicans,8 strongly suggesting that pathogen challenge can induce at least one other cytokine to compensate for the deficiency in the G-CSFs. Furthermore, we have found that in an in vitro culture system C albicans as well as LPS stimulate the production of NPA by G-CSF−/−/GM-CSF−/−-deficient MEFs. NPA sustains the generation of neutrophilic granulocytes from bone marrow of G-CSF−/−/GM-CSF−/− mice, and NPA production is much stronger in cells exposed to LPS rather than C albicans.9 To test the physiologic significance of these findings, we monitored the effects of LPS administration on granulocyte production in vivo by compound mutant G-CSF−/−/GM-CSF−/− mice. G-CSF−/−/GM-CSF−/− mice were injected intraperitoneally with LPS (30 μg/mouse) or PBS (vehicle control) and killed at different times. At each time point, blood and bone marrow cells were collected and analyzed for the presence of myeloid cells.
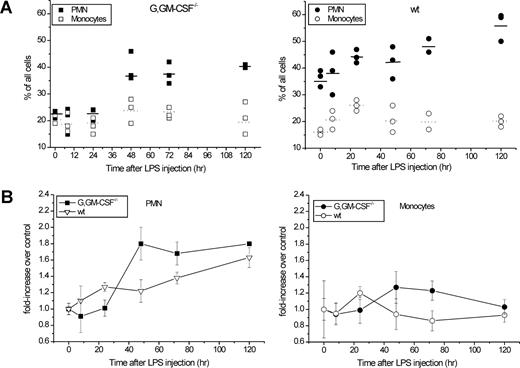
The number of neutrophils and monocytes in the blood of wild-type (WT) or G-CSF−/−/GM-CSF−/− mice, as a function of time after exposure to LPS, is shown in Figure 1A. Neutrophil counts increase rapidly and dramatically (∼8-fold) after injection of the G-CSF−/−/GM-CSF−/− mice with LPS. Whereas the absolute neutrophil counts (ANCs) in the blood of G-CSF−/−/GM-CSF−/− mice never reaches the levels observed in WT mice, the fold increase over the basal level (Figure 1B left panel) is very similar irrespective of the genotype. Surprisingly, after a single injection of LPS, this increase in neutrophils is sustained for up to 5 days. There is a subtle but significant difference in the kinetics of neutrophil blood counts between WT and G-CSF−/−/GM-CSF−/− mice. In WT mice, there are 2 phases of neutrophilia, a rapid and relatively transient increase (8- to 24-hour time point), which may reflect mobilization from other hemopoietic compartments, followed by a later sustained increase. In G-CSF−/−/GM-CSF−/− mice, the initial phase is insignificant, suggesting that this early response is mediated by G-CSF and/or GM-CSF. There is also a small, LPS-mediated increase in blood monocytes (Figure 1B right panel), which is more marked in WT mice at the earliest time point; however, the difference is barely significant.
Absolute neutrophils and monocytes counts in the blood of LPS-injected mice. Compound mutant G-CSF−/−/GM-CSF−/− (G,GM-CSF−/−) and wild-type (wt) mice were injected with LPS (30 μg/mouse in 100 μL PBS) or with PBS. 3 mice were killed at each time point after injection. Total WBC for each sample were determined using a Sysmex K1000 automated counter. Blood smears were stained with May Grünwald/Giemsa and differential counts were performed on a Nikon 90 I microscope using a 60× oil lens. (A) Absolute blood counts for polymorphic neutrophils (PMNs, solid symbols) and monocytes (open symbols) in G-CSF−/−/GM-CSF−/− and wt mice, respectively. Symbols refer to individual values for each mouse with the average for each group indicated by horizontal bars. (B) Fold increase in the total number of PMNs (left panel) and monocytes (right panel) with time after exposure to LPS. Closed symbols, G-CSF−/−/GM-CSF−/− mice; open symbols, wild-type mice.
Absolute neutrophils and monocytes counts in the blood of LPS-injected mice. Compound mutant G-CSF−/−/GM-CSF−/− (G,GM-CSF−/−) and wild-type (wt) mice were injected with LPS (30 μg/mouse in 100 μL PBS) or with PBS. 3 mice were killed at each time point after injection. Total WBC for each sample were determined using a Sysmex K1000 automated counter. Blood smears were stained with May Grünwald/Giemsa and differential counts were performed on a Nikon 90 I microscope using a 60× oil lens. (A) Absolute blood counts for polymorphic neutrophils (PMNs, solid symbols) and monocytes (open symbols) in G-CSF−/−/GM-CSF−/− and wt mice, respectively. Symbols refer to individual values for each mouse with the average for each group indicated by horizontal bars. (B) Fold increase in the total number of PMNs (left panel) and monocytes (right panel) with time after exposure to LPS. Closed symbols, G-CSF−/−/GM-CSF−/− mice; open symbols, wild-type mice.
The increase in blood neutrophils after LPS challenge is mirrored in the bone marrow compartment (Figure 2). Notably, the relative increase in bone marrow neutrophils is greater in G-CSF−/−/GM-CSF−/− mice than in their WT counterparts and reached a plateau earlier (Figure 2B left panel). The majority of neutrophils in the bone marrow samples from both G-CSF−/−/GM-CSF−/− and WT mice were band forms (data not shown). Monocytes increased only marginally in the bone marrow of mice of both genotypes, and there was a tendency for this trend to be sustained longer in G-CSF−/−/GM-CSF−/− mice (Figure 2B right panel). It remains unclear whether these trends would have any bearing on the physiologic responses to gram-negative bacteria
Proportion of neutrophils and monocytes in bone marrow cytospins from LPS-injected mice. G-CSF−/−/GM-CSF−/− (G,GM-CSF−/−) and wild-type (wt) mice were injected with LPS as described in the legend to Figure 1. Bone marrow cells were collected from both femura and prepared for cytospins. Slides were stained with May-Grünwald/Giemsa, and differential counts were performed using a Nikon 90 I microscope with a 60× oil lens. (A) Proportion of polymorphic neutrophils (PMN, solid symbols) and monocytes (open symbols) in G-CSF−/−/GM-CSF−/− mice and wt mice, respectively. Symbols refer to values for individual mice, with averages for each group indicated by horizontal bars. (B) Fold increase in the proportion of neutrophils (left panel) and monocytes (right panel) with time after challenge of mice with LPS. Solid symbols, G-CSF−/−/GM-CSF−/− mice; open symbols, wt mice. Error bars represent SE.
Proportion of neutrophils and monocytes in bone marrow cytospins from LPS-injected mice. G-CSF−/−/GM-CSF−/− (G,GM-CSF−/−) and wild-type (wt) mice were injected with LPS as described in the legend to Figure 1. Bone marrow cells were collected from both femura and prepared for cytospins. Slides were stained with May-Grünwald/Giemsa, and differential counts were performed using a Nikon 90 I microscope with a 60× oil lens. (A) Proportion of polymorphic neutrophils (PMN, solid symbols) and monocytes (open symbols) in G-CSF−/−/GM-CSF−/− mice and wt mice, respectively. Symbols refer to values for individual mice, with averages for each group indicated by horizontal bars. (B) Fold increase in the proportion of neutrophils (left panel) and monocytes (right panel) with time after challenge of mice with LPS. Solid symbols, G-CSF−/−/GM-CSF−/− mice; open symbols, wt mice. Error bars represent SE.
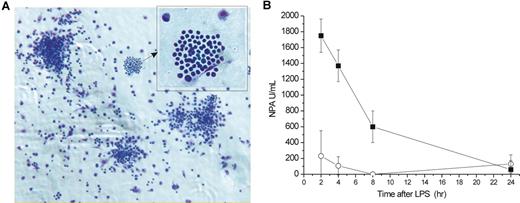
Given the parallel between in vivo (Figures 1,2) and in vitro9 enhancement of granulocyte generation after LPS, we tested the sera of the LPS-injected G-CSF−/−/GM-CSF−/− mice for NPA9 (Figure 3A). Figure 3B shows that sera of LPS-challenged mice did indeed cause the rapid appearance of an NPA-like activity in the blood. The type of granulocyte clusters generated in this assay, and the morphology of the cells within the clusters, were indistinguishable from those generated by in vitro produced NPA (Figure 3A; data not shown). The NPA properties of the sera could not be explained by the presence of residual LPS, as LPS does not stimulate the growth of granulocyte clusters when added directly into this assay9 (data not shown). Thus, NPA, which is produced in vitro by the cells of G-CSF−/−/GM-CSF−/− mice, is also produced in mice following systemic challenge with LPS.
Serum from LPS-injected mice contains NPA. (A) NPA-mediated generation of granulocytes clusters in vitro from bone marrow cells of G-CSF−/−/GM-CSF−/− exposed to medium conditioned by LPS-challenged G-CSF−/−/GM-CSF−/− MEFs (May-Grünwald/Giemsa stain, original magnification ×40). Inset: same field (original magnification ×60). Micrographs were acquired on cytospin slides stained with May-Grünwald-Giemsa on a Nikon 90i microscope (Nikon, Tokyo, Japan) fitted with a 40×/0.6 numeric aperture Plan Fluor dry objective or with a 60×/1.4 numeric aperture Plan Apo oil objective, a DXM 1200c camera (Nikon), and NIS-AR image acquisition software (v 2.30; Nikon). (B) NPA in sera from G-CSF−/−/GM-CSF−/− mice injected intraperitoneally with PBS (○) or with LPS (30 μg/mouse, ■). Sera from 3 mice per experimental point were individually tested for NPA as described in “NPA assay.” Data are mean plus or minus SE for each group. One unit of NPA is defined as the activity required to generate one granulocyte cluster from 5 × 103 bone marrow cells after 4 days in a liquid culture assay. Error bars represent SE.
Serum from LPS-injected mice contains NPA. (A) NPA-mediated generation of granulocytes clusters in vitro from bone marrow cells of G-CSF−/−/GM-CSF−/− exposed to medium conditioned by LPS-challenged G-CSF−/−/GM-CSF−/− MEFs (May-Grünwald/Giemsa stain, original magnification ×40). Inset: same field (original magnification ×60). Micrographs were acquired on cytospin slides stained with May-Grünwald-Giemsa on a Nikon 90i microscope (Nikon, Tokyo, Japan) fitted with a 40×/0.6 numeric aperture Plan Fluor dry objective or with a 60×/1.4 numeric aperture Plan Apo oil objective, a DXM 1200c camera (Nikon), and NIS-AR image acquisition software (v 2.30; Nikon). (B) NPA in sera from G-CSF−/−/GM-CSF−/− mice injected intraperitoneally with PBS (○) or with LPS (30 μg/mouse, ■). Sera from 3 mice per experimental point were individually tested for NPA as described in “NPA assay.” Data are mean plus or minus SE for each group. One unit of NPA is defined as the activity required to generate one granulocyte cluster from 5 × 103 bone marrow cells after 4 days in a liquid culture assay. Error bars represent SE.
IL6 contributes to NPA
We have previously shown that LPS challenge of cells from G-CSF−/−/GM-CSF−/− mice in vitro induces a range of inflammatory cytokines, and tested some of these cytokines for their ability to induce myeloid progenitors from G-CSF−/−/GM-CSF−/− mice to form granulocyte clusters. IL6 is much less potent than NPA in stimulating granulocyte clusters9 : its activity on bone marrow progenitors does not exceed 50% of the NPA in the same assay. However, IL6 remains a candidate as a potential contributor to NPA. IL6 is detectable in CM from G-CSF−/−/GM-CSF−/− embryonic fibroblasts, its level (as detected by cytokine arrays) is higher after stimulation of the cells with LPS and is reduced in the CM from G-CSF−/−/GM-CSF−/−/M-CSF−/− cells9 : thus, the presence of IL6 correlates with the presence of NPA. Furthermore, it has been reported that IL6 secretion after bacterial infection is dramatically reduced in op/op mice (M-CSF null) and that M-CSF augments IL6 secretion.22,23 This is consistent with our results9 showing an obligate role for M-CSF in the production of NPA. These observations prompted us to investigate further the contribution of IL6 to NPA.
We generated triple-knockout (G-CSF−/−/GM-CSF−/−/IL6−/−) mice by intercrossing G-CSF−/−/GM-CSF−/− mice5 with IL6−/− mice.21 We found that G-CSF−/−/GM-CSF−/−/IL6−/− mice housed in conventional, non–specific pathogen free (SPF) conditions died shortly after birth or at weaning. Postnatal viability, however, was dramatically improved by supplementing the drinking water with antibiotics, suggesting that mortality was associated with an impairment of immunity (Table 1). We derived primary embryonic fibroblasts (MEFs) from the G-CSF−/−/GM-CSF−/− (double-knockout) and the G-CSF−/−/GM-CSF−/−/IL6−/− (triple-knockout) mice and compared their ability to produce NPA in response to in vitro LPS stimulation (Figure 4A). Medium conditioned by G-CSF−/−/GM-CSF−/−/IL6−/− cells generated approximately 40% of the NPA com-pared with G-CSF−/−/GM-CSF−/− cells, and the addition of recombinant murine IL6 to medium conditioned by G-CSF−/−/GM-CSF−/−/IL6−/− fully restored the level of NPA (Figure 4A). Clearly, IL6 contributes significantly to NPA and indeed is necessary for full activity. It is important to note that, whereas IL6 is able to fully restore NPA when added to the MEFs during LPA challenge, it does not replace NPA when added directly into the bone marrow assay, generating a much lower number of granulocyte clusters compared with NPA (Figure 6; data not shown).
Contribution of IL6 to the generation of granulocytes in vitro. (A) MEFs derived from individual G-CSF−/−/GM-CSF−/−/IL6+/+or G-CSF−/−/GM-CSF−/−/IL6−/− embryos were exposed to control medium (□), LPS (0.05 μg/mL, ■), or LPS (0.05 μg/mL) plus IL6 (50 ng/mL, ▨) for 48 hours. The resultant CM were tested for NPA in a standard bone marrow assay as described in “NPA assay.” Conditioned media were produced from individual embryos in 3 separate litters for each genotype; the data for embryos with identical genotype have been pooled and are presented as mean plus or minus SD. (B) Conditioned medium from G-CSF−/−/GM-CSF−/− immortalized embryonic fibroblast (■) or recombinant IL6 (50 ng/mL, ○) were preincubated with increasing concentrations of a neutralizing antibody to murine IL6 before their assay on bone marrow cells in liquid culture. Data are presented as percentage of the activity in the absence of added antibody. Error bars represent SE.
Contribution of IL6 to the generation of granulocytes in vitro. (A) MEFs derived from individual G-CSF−/−/GM-CSF−/−/IL6+/+or G-CSF−/−/GM-CSF−/−/IL6−/− embryos were exposed to control medium (□), LPS (0.05 μg/mL, ■), or LPS (0.05 μg/mL) plus IL6 (50 ng/mL, ▨) for 48 hours. The resultant CM were tested for NPA in a standard bone marrow assay as described in “NPA assay.” Conditioned media were produced from individual embryos in 3 separate litters for each genotype; the data for embryos with identical genotype have been pooled and are presented as mean plus or minus SD. (B) Conditioned medium from G-CSF−/−/GM-CSF−/− immortalized embryonic fibroblast (■) or recombinant IL6 (50 ng/mL, ○) were preincubated with increasing concentrations of a neutralizing antibody to murine IL6 before their assay on bone marrow cells in liquid culture. Data are presented as percentage of the activity in the absence of added antibody. Error bars represent SE.
To determine directly the contribution of IL6 to NPA, we attempted to block IL6 activity in LPS-stimulated CM with a neutralizing antibody to murine IL6. Samples were incubated with a neutralizing antimurine IL6 antibody before their assessment for NPA on bone marrow cells. Granulocyte clusters formation by recombinant murine IL6 was reduced by more than 80% by the anti-IL6 antibody. In contrast, the potency of the CM (NPA) was only marginally decreased (Figure 4B). The discrepancy between the results in Figure 4A,B suggests that either IL6 contributes to the secretion of NPA, but is not an NPA component, or alternatively IL6 is present in NPA but is resistant to antibody neutralization, possibly through masking of the epitope by complex formation with other components of NPA.
sIL6R is a potential component of NPA
The extracellular domain of the IL6R is generated by alternative splicing or by proteolytic cleavage from the cell surface (shedding). Shedding can be triggered by toxins and bacterial infection24-26 and proteolytic cleavage is mediated by the matrix-metalloproteinase ADAM 10 and ADAM 17.27,28 sIL6R binds to IL6 and the sIL6R/IL6 complex associates with transmembrane gp130, which is expressed on most cells of the body. This mechanism, referred to as “transsignaling,” results in activation of the signal transduction machinery in cells that do not express the membrane-bound IL6 receptor. One of the targets of sIL6R transsignaling is the hemopoietic compartment: double transgenic mice overexpressing IL6 and sIL6R are characterized by massive extramedullary hemopoiesis with elevated numbers of granulocytes and myeloid progenitor cells.16 The biology of sIL6R shedding and its site of action suggest sIL6R as a potential component of NPA. Indeed, the presence of sIL6R/IL6 complex in the media conditioned by MEFs would be consistent with a requirement for IL6 in NPA, as well as with the failure of the anti-IL6 antibody to neutralize NPA, assuming that the IL6 epitope is masked by sIL6R.
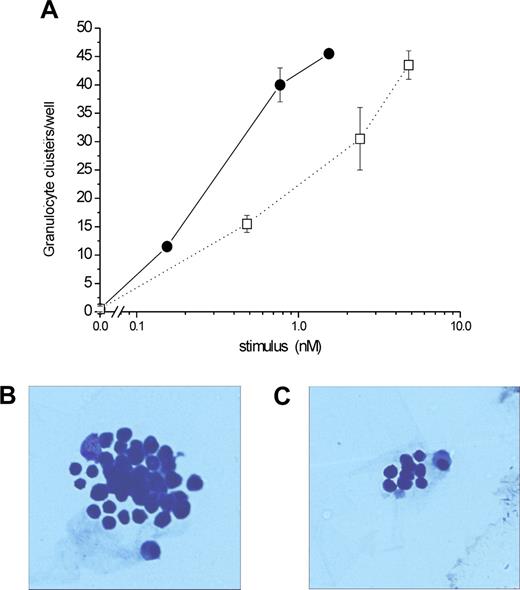
We initially tested this hypothesis by measuring the NPA of Hyper-IL6, a chimeric designer cytokine consisting of a fusion protein between IL6 and the sIL6R.18 Hyper-IL6 would be expected to mimic the action of the natural IL6/sIL6R complex (Figure 5). Indeed, Hyper-IL6 was more potent than IL6 in the NPA assay (EC50, 0.3 nM vs 1.7 nM) and generated granulocyte clusters of similar morphology and size to those obtained in cultures treated with NPA, whereas IL6-stimulated clusters were significantly smaller (Figure 5B,C).
Hyper-IL6 stimulates the formation of granulocyte clusters in vitro. (A) Hyper-IL6 (•) and mIL6 (□) were compared directly for their ability to generate granulocyte clusters from the bone marrow of G-CSF−/−/GM-CSF−/− mice. Results are plotted as molar concentration vs the number of granulocyte-containing clusters generated after 4 days in liquid culture. (B,C) Typical clusters arising from bone marrow cultures stimulated with Hyper-IL6 (B) or IL6 (C). The images have been cropped to show a single cluster, and were acquired as in Figure 3A.
Hyper-IL6 stimulates the formation of granulocyte clusters in vitro. (A) Hyper-IL6 (•) and mIL6 (□) were compared directly for their ability to generate granulocyte clusters from the bone marrow of G-CSF−/−/GM-CSF−/− mice. Results are plotted as molar concentration vs the number of granulocyte-containing clusters generated after 4 days in liquid culture. (B,C) Typical clusters arising from bone marrow cultures stimulated with Hyper-IL6 (B) or IL6 (C). The images have been cropped to show a single cluster, and were acquired as in Figure 3A.
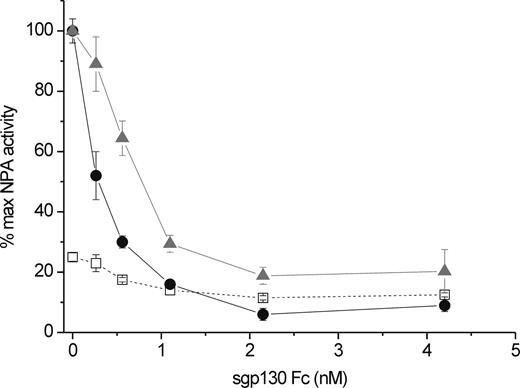
The sIL6R/IL6 complex exerts its action by binding to the cell surface gp130.15 The soluble form of gp130 (sgp130) has been reported to inhibit IL6 transsignaling specifically, while leaving unaffected IL6 responses through membrane-bound IL6R.19 Therefore, we next tested whether sgp130-Fc would interfere with NPA. Hyper-IL6 was used in these experiments as a positive control, and IL6 as a negative control for sgp130-Fc specificity. sgp130-Fc inhibits Hyper-IL6 and NPA with similar IC50 (0.3 and 0.7 nM, respectively; Figure 6); however, IL6 activity was only marginally affected by sgp130Fc (Figure 6), in accordance with previous reports. By contrast, sgp130 abolished 95% of Hyper-IL6 and 80% of NPA activities. Collectively, these data suggest that NPA action is mediated via cell-surface gp130 and is independent of the cell-surface IL6R, thus strengthening the case for an involvement of bioactive sIL6R/IL6 complex in NPA.
Inhibition of granulocyte cluster formation by sgp130Fc. Bone marrow cells from G-CSF−/−/GM-CSF−/− mice were incubated in chamber slides with NPA (conditioned medium from G-CSF−/−/GM-CSF−/− MEFs, at a final concentration of 30% v/v,  ), Hyper-IL6 (20 ng/mL, •), or murine recombinant IL6 (20 ng/mL, □) in the presence of increasing amounts of sgp130-Fc. Four days later, slides were stained with May-Grünwald/Giemsa, and the number of granulocyte clusters was assessed by light microscopy. Means plus or minus SE of duplicate wells are plotted as percentage of the maximal activity detected in the assay (granulocyte clusters/well generated by NPA in the absence of sgp130-Fc). The mean numbers of clusters generated by each stimulus in the absence of sgp130 were 91 plus or minus 7 (Hyper-IL6), 95 plus or minus 6 (NPA), and 25 plus or minus 1 (IL6).
), Hyper-IL6 (20 ng/mL, •), or murine recombinant IL6 (20 ng/mL, □) in the presence of increasing amounts of sgp130-Fc. Four days later, slides were stained with May-Grünwald/Giemsa, and the number of granulocyte clusters was assessed by light microscopy. Means plus or minus SE of duplicate wells are plotted as percentage of the maximal activity detected in the assay (granulocyte clusters/well generated by NPA in the absence of sgp130-Fc). The mean numbers of clusters generated by each stimulus in the absence of sgp130 were 91 plus or minus 7 (Hyper-IL6), 95 plus or minus 6 (NPA), and 25 plus or minus 1 (IL6).
Inhibition of granulocyte cluster formation by sgp130Fc. Bone marrow cells from G-CSF−/−/GM-CSF−/− mice were incubated in chamber slides with NPA (conditioned medium from G-CSF−/−/GM-CSF−/− MEFs, at a final concentration of 30% v/v,  ), Hyper-IL6 (20 ng/mL, •), or murine recombinant IL6 (20 ng/mL, □) in the presence of increasing amounts of sgp130-Fc. Four days later, slides were stained with May-Grünwald/Giemsa, and the number of granulocyte clusters was assessed by light microscopy. Means plus or minus SE of duplicate wells are plotted as percentage of the maximal activity detected in the assay (granulocyte clusters/well generated by NPA in the absence of sgp130-Fc). The mean numbers of clusters generated by each stimulus in the absence of sgp130 were 91 plus or minus 7 (Hyper-IL6), 95 plus or minus 6 (NPA), and 25 plus or minus 1 (IL6).
), Hyper-IL6 (20 ng/mL, •), or murine recombinant IL6 (20 ng/mL, □) in the presence of increasing amounts of sgp130-Fc. Four days later, slides were stained with May-Grünwald/Giemsa, and the number of granulocyte clusters was assessed by light microscopy. Means plus or minus SE of duplicate wells are plotted as percentage of the maximal activity detected in the assay (granulocyte clusters/well generated by NPA in the absence of sgp130-Fc). The mean numbers of clusters generated by each stimulus in the absence of sgp130 were 91 plus or minus 7 (Hyper-IL6), 95 plus or minus 6 (NPA), and 25 plus or minus 1 (IL6).
sIL6R protein is present in NPA fractions and mediates its activity
To further substantiate our strong, but circumstantial, evidence that sIL6R is a component of NPA, we next tested partially purified, NPA-positive fractions for immunoreactivity with an antibody to the murine IL6R. We attempted to monitor the presence of sIL6R in CM positive or negative for NPA, as well as in semipurified fractions with high NPA. The protocol for partial purification of NPA from crude CM of LPS-challenged MEFs is detailed in Figure S1.
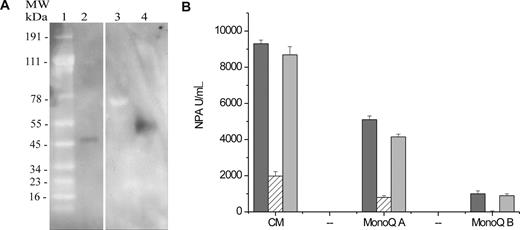
Briefly, albumin-depleted CM was chromatographed on a Superose 12 column, and NPA-positive fractions were pooled and rechromatographed on a Mono-Q column (Figure S1). Fractions from MonoQ chromatography were tested for NPA, active fractions were pooled, and the pool was concentrated 20-fold as described in “Partial purification of NPA.” The high content of unrelated proteins in the crude CM and in samples at the early stages of purification prevented successful detection of sIL6R by SDS-PAGE and immunoblotting. However, a specific, IL6R-reactive band was detectable in the most highly purified preparation (pooled active fractions from Mono-Q chromatography: Figure 7A). The apparent molecular weight of recombinant murine sIL6R is 50 kDa, whereas the IL6R-reactive band from the NPA preparation migrates with an apparent molecular weight of 55 to 60 kDa, similar to the reported size of sIL6R in human urine and plasma29-31 and significantly less than would be expected for the full-length IL6R (80 kDa).
Biochemical and functional demonstration of sIL6R in purified NPA from MEFs CM. (A) Immunodetection of sIL6R in NPA-positive fractions. Purified murine sIL6R or NPA at different stages of purification (Figure S2) were loaded on a 4% to 12% gradient gel, immunoblotted onto PVDF membrane, and probed with an antibody specific for murine IL6R. Reactive bands were detected with an HRP-coupled antigoat Ig antibody. Lane 1, molecular weight markers; lane 2, recombinant sIL6R, 20ng; lane 3, Superose-12 active pool A; lane 4, Mono-Q active pool A. This blot is representative of 2 separate experiments. (B) Selective immunodepletion of NPA by anti-IL6R antibody. Crude NPA-containing conditioned medium (CM) or semipurified NPA preparations (MonoQ A and B, Figures S1,S2) were preincubated with vehicle ( ), anti-IL6R antibody (▨), or anti-EGFR antibody (
), anti-IL6R antibody (▨), or anti-EGFR antibody ( ). The immune complexes were depleted from the samples using protein G-Sepharose as described in “Neutralization of NPA,” and the supernatants were assayed for NPA. Data are expressed as total NPA and have been adjusted for the small dilution factor resulting from antibody immunodepletion. All samples were tested in triplicate. Error bars represent SE.
). The immune complexes were depleted from the samples using protein G-Sepharose as described in “Neutralization of NPA,” and the supernatants were assayed for NPA. Data are expressed as total NPA and have been adjusted for the small dilution factor resulting from antibody immunodepletion. All samples were tested in triplicate. Error bars represent SE.
Biochemical and functional demonstration of sIL6R in purified NPA from MEFs CM. (A) Immunodetection of sIL6R in NPA-positive fractions. Purified murine sIL6R or NPA at different stages of purification (Figure S2) were loaded on a 4% to 12% gradient gel, immunoblotted onto PVDF membrane, and probed with an antibody specific for murine IL6R. Reactive bands were detected with an HRP-coupled antigoat Ig antibody. Lane 1, molecular weight markers; lane 2, recombinant sIL6R, 20ng; lane 3, Superose-12 active pool A; lane 4, Mono-Q active pool A. This blot is representative of 2 separate experiments. (B) Selective immunodepletion of NPA by anti-IL6R antibody. Crude NPA-containing conditioned medium (CM) or semipurified NPA preparations (MonoQ A and B, Figures S1,S2) were preincubated with vehicle ( ), anti-IL6R antibody (▨), or anti-EGFR antibody (
), anti-IL6R antibody (▨), or anti-EGFR antibody ( ). The immune complexes were depleted from the samples using protein G-Sepharose as described in “Neutralization of NPA,” and the supernatants were assayed for NPA. Data are expressed as total NPA and have been adjusted for the small dilution factor resulting from antibody immunodepletion. All samples were tested in triplicate. Error bars represent SE.
). The immune complexes were depleted from the samples using protein G-Sepharose as described in “Neutralization of NPA,” and the supernatants were assayed for NPA. Data are expressed as total NPA and have been adjusted for the small dilution factor resulting from antibody immunodepletion. All samples were tested in triplicate. Error bars represent SE.
To validate these findings, we next tested the susceptibility of NPA-positive fractions to immunodepletion of the sIL6R. Anti-IL6R antibody or anti-EGFR antibody (as negative control) was added to crude CM or to NPA-positive, semipurified preparations, and the immunocomplexes were removed by incubation with protein G-Sepharose. Starting material and immunodepleted samples were then tested in the NPA assay. Figure 7B clearly shows that immunodepletion of the sIL6R specifically reduced NPA by approximately 80%: thus, sIL6R is the major biologically active component of NPA. There is, however, some residual NPA that is not abolished by immunodepletion, and its levels are consistent with the residual NPA we observed in the presence of sgp130-Fc (Figure 6), suggesting that a minor component of NPA may not be associated with sIL6R, and its activity is not mediated by gp130.
Discussion
Experimental models of acute infection using compound mutant mice have shown that both G-CSF and IL6 are dispensable for emergency granulopoiesis; however, these models used mice that still express at least one of the classic regulators of granulopoiesis, either GM-CSF17 or IL6.8 Indeed, on a genetic background of G-CSF deficiency, both GM-CSF and IL6 contribute significantly to neutrophilia after C albicans infection.8 The use of compound mutant mice lacking all 3 cytokines as in vivo models for responses to pathogens is severely limited by their extreme sensitivity to infection (Table 1). To overcome this obstacle, we have investigated the possibility of using a surrogate in vitro system to address the contribution of IL6 to granulopoiesis in the absence of G-CSF and GM-CSF and to identify the major granulocyte-stimulating cytokine produced by cells deficient in G-CSF and GM-CSF. In the present work, we have established a link between the in vivo and in vitro responses to LPS in G-CSF−/−/GM-CSF−/− mice. We show that LPS challenge of G-CSF−/−/GM-CSF−/− mice results in neutrophilia and in the appearance of a factor in the serum, which supports in vitro granulopoiesis. Similarly, in vitro exposure to LPS of embryonic fibroblasts derived from G-CSF−/−/GM-CSF−/− mice leads to secretion of pro-granulocytic factors.9 This system allowed us to identify the IL6/sIL6R complex as a potent stimulus for the generation of granulocytes and the most likely candidate for the neutrophilic responses of G-CSF and GM-CSF-deficient mice exposed to infectious agents or bacterial products.
IL6 and its soluble receptor, sIL6R, are important molecules in innate and acquired immunity, and the corresponding IL6 trans-signaling appears to be a requirement in neutrophil activation and recruitment.32-34 Furthermore, IL6R shedding by apoptotic neutrophils may play a crucial role in the resolution of inflammatory response.35 However, the role of IL6 in de novo granulopoiesis has been difficult to assess because of the presence of other cytokines, which regulate granulopoiesis and neutrophil activation, mainly G-CSF and GM-CSF. We have now used cells from G-CSF−/−/GM-CSF−/− compound mutant mice, with or without a functional IL6 gene, to show that the IL6/sIL6R complex stimulates granulopoiesis.
It is clear that the IL6 transsignaling components are regulated during infection in WT mice: circulating IL6 levels and M-CSF secretion are increased,36 whereas sIL6R shedding is triggered by bacterial toxins24,25 and stimulated by neutrophil apoptosis.35 Thus, in mice expressing a full complement of granulocytic cytokines, all the components of IL6 transsignaling are present and are elevated during infection, suggesting that they are important mediators of the inflammatory response. However, the role of IL6 transsignaling during steady state or emergency granulopoiesis in WT mice remains to be defined. The pharmacokinetics of the IL6R/IL6 complex in the circulation and its role in the regulation of myelopoiesis in normal individuals should provide further insight into the pathophysiologic responses to the control of infections and may provide potential avenues for new therapeutic interventions.
An Inside Blood analysis of this article appears at the front of this issue.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Professor Ashley Dunn, Dr Glen Begley, and Dr Christiaan Saris for stimulating discussions during the early stages of this work.
This work was supported in part by Amgen.
Authorship
Contribution: F.W. designed the experiments, interpreted the data, performed some of the experiments, and wrote the manuscript; H.-H.Z. established the triple (G-CSF−/−/GM-CSF−/−/IL6−/−) knockout mouse colony and performed all the animal experiments and the in vitro NPA assays; E.C.N. designed, and J.W. carried out, the chromatographic purification of NPA; M.E., V.M., and S.R.-J. provided essential reagents, advice on experimental design, and critical reading of the manuscript; A.W.B. assisted with the interpretation of experiments and provided insightful comments and critical advice during the preparation of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Francesca Walker, Ludwig Institute for Cancer Research, PO Box 2008, RMH Melbourne, Victoria, 3050, Australia; e-mail: francesca.walker@ludwig.edu.au.