Abstract
In the past 50 years, we have witnessed explosive growth in the understanding of normal and neoplastic lymphoid cells. B-cell, T-cell, and natural killer (NK)–cell neoplasms in many respects recapitulate normal stages of lymphoid cell differentiation and function, so that they can be to some extent classified according to the corresponding normal stage. Likewise, the molecular mechanisms involved the pathogenesis of lymphomas and lymphoid leukemias are often based on the physiology of the lymphoid cells, capitalizing on deregulated normal physiology by harnessing the promoters of genes essential for lymphocyte function. The clinical manifestations of lymphomas likewise reflect the normal function of lymphoid cells in vivo. The multiparameter approach to classification adopted by the World Health Organization (WHO) classification has been validated in international studies as being highly reproducible, and enhancing the interpretation of clinical and translational studies. In addition, accurate and precise classification of disease entities facilitates the discovery of the molecular basis of lymphoid neoplasms in the basic science laboratory.
Introduction
Mature B-cell and T/natural killer (NK)–cell neoplasms are clonal tumors of B cells, T cells, or NK cells that in many respects recapitulate stages of normal B-cell or T-cell differentiation. Although classifications of lymphoid malignancies have historically treated lymphomas and leukemias separately, this distinction is now appreciated as artificial. However, as the precursor neoplasms—lymphoblastic lymphomas/leukemias and acute myeloid leukemias—are closely related from a clinical and biological perspective, they will not be covered in this review. In addition, plasma cell neoplasms often have been treated separately from other lymphoid neoplasms, but this segregation is equally artificial, and the World Health Organization (WHO) classification of lymphoid neoplasms1 includes plasma disorders. A recent review by Kyle and Rajkumar in this series comprehensively discussed plasma cell myeloma,2 and thus we will not include it further in this review.
As immunologists and pathologists have come to understand the ontogeny of lymphoid cells, it has been tempting to base the classification of lymphoid malignancies strictly on the corresponding normal stage. However, some neoplasms—for example, hairy cell leukemia—do not clearly correspond to a normal B-cell differentiation stage, and some clinically distinctive neoplasms may exhibit immunophenotypic heterogeneity, such as hepatosplenic T-cell lymphoma, which is derived from either α/β or γ/δ T cells. Thus, the normal counterpart of the neoplastic cell cannot at this time be the sole basis for classification.
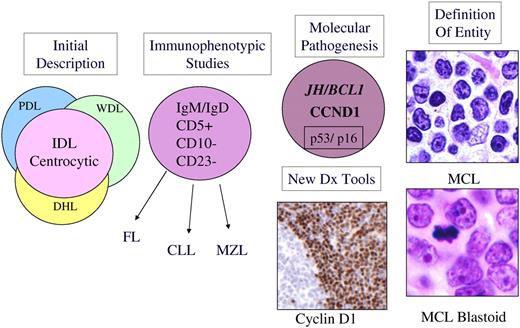
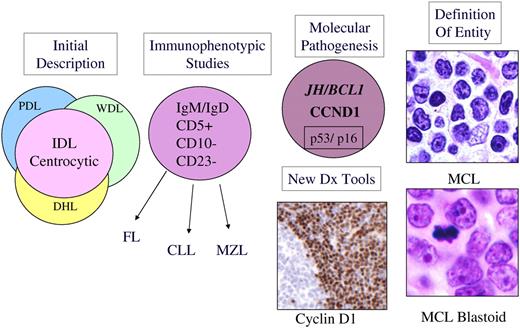
Cancers are increasingly recognized as genetic diseases, with precise molecular alterations often defining entities. However, progress in identifying the molecular pathogenesis of lymphoid malignancies has in most instances followed an accurate description of the disease by pathologists, based on morphologic, immunophenotypic and clinical parameters (Table 1). This paradigm is exemplified by both mantle cell lymphoma (MCL)3,4 and anaplastic large cell lymphoma (ALCL),5 in which careful pathologic descriptions preceded the recognition of CCND1 and ALK, respectively, as genes critical to their pathogenesis. However, the process is iterative, and once the underlying molecular cause is known, we gain access to new diagnostic tools that help better define the borderlines of the disease (Figure 1). Thus, the use of monoclonal antibodies reactive in routine sections to cyclin D1 and the ALK tyrosine kinase helped define the morphologic spectrum of MCL and ALCL. This partnership between the pathologist and the molecular biologist is crucial in the classification of disease, and should be equally applicable to other organ systems.
Schematic diagram illustrating evolution of the entity MCL. MCL was recognized in Kiel classification and modified Rappaport classification as centrocytic lymphoma and lymphocytic lymphoma of intermediate differentiation (IDL), respectively.6 Precise criteria for the distinction from other morphologically similar lymphomas were lacking. The recognition of a characteristic immunophenotype (CD5+, CD23−, CD10−, monoclonal B cell) helped better define the entity. The identification of the t(11;14) resulting in CCNDI/IGH translocation in virtually all cases of MCL led to the use of cyclin D1 detection by immunohistochemistry for diagnosis. In addition, secondary genetic events such as p53 and p16 deletion/mutation were identified in high-grade variants of MCL, which had been recognized histologically as the “blastoid” subtype. The data derived from immunophenotypic and genetic studies are integrated, culminating in our current definition of the disease. PDL indicates poorly differentiated lymphocytic; WDL, well-differentiated lymphocytic; DHL, diffuse histiocytic lymphoma; and MZL, marginal zone lymphoma.
Schematic diagram illustrating evolution of the entity MCL. MCL was recognized in Kiel classification and modified Rappaport classification as centrocytic lymphoma and lymphocytic lymphoma of intermediate differentiation (IDL), respectively.6 Precise criteria for the distinction from other morphologically similar lymphomas were lacking. The recognition of a characteristic immunophenotype (CD5+, CD23−, CD10−, monoclonal B cell) helped better define the entity. The identification of the t(11;14) resulting in CCNDI/IGH translocation in virtually all cases of MCL led to the use of cyclin D1 detection by immunohistochemistry for diagnosis. In addition, secondary genetic events such as p53 and p16 deletion/mutation were identified in high-grade variants of MCL, which had been recognized histologically as the “blastoid” subtype. The data derived from immunophenotypic and genetic studies are integrated, culminating in our current definition of the disease. PDL indicates poorly differentiated lymphocytic; WDL, well-differentiated lymphocytic; DHL, diffuse histiocytic lymphoma; and MZL, marginal zone lymphoma.
Historical background: the early years
The first description of what we now recognize as a lymphoma is generally attributed to Thomas Hodgkin in 1832 (Table 2).46 The first use of the term lymphosarcoma is attributed to Rudolf Virchow in 1863 (reviewed in Trumper et al8 ). In 1898 and 1902, Carl Sternberg and Dorothy Reed independently described the characteristic binucleate and multinucleate giant cells that came to be called the Reed-Sternberg or Sternberg-Reed cell.7 Sternberg felt that Hodgkin disease was an inflammatory process, related to tuberculosis, but Reed disagreed.47 She made several other key observations: the general health of the patient before the onset of the disease is usually excellent; there was an early peak among children and young adults; and Hodgkin disease usually presents as painless progressive cervical adenopathy without leukemia. She proposed that the pathologic picture is sufficient for diagnosis. Having considerable success as a fellow in pathology, she sought a teaching post at Johns Hopkins Medical School. Her chairman, William Welch, answered, “No women had ever held a teaching position in the school, and there would be great opposition to it.”47 In her diary she noted, “Suddenly, as I saw what I had to face in acceptance of injustice—I knew that I couldn't take it.”47 She left pathology and took up a career in public health.
The term “reticulum cell sarcoma” is attributed to Ewing, Oberling, and Roulet, who each described tumors of large cells, thought to be related to the supporting fibrous reticulum of lymphoid tissues.8 While the origin and function of these cells were unknown, the term reticulum cell sarcoma came to be used for “large cell” neoplasms—as distinguished from “lymphosarcoma,” which was applied to those composed of smaller cells more recognizable as lymphocytes.
In 1925, Brill and colleagues described patients with enlargement of lymph nodes and spleen, characterized pathologically by a proliferation of lymphoid follicles9 ; additional cases were reported by Symmers,10 who also described progression to a large-cell neoplasm.11 In 1941, Edward A. Gall and Tracy B. Mallory, pathologists at Massachusetts General Hospital, proposed a morphologic classification, based on review of their own collection of 618 patients for whom clinical data were available.12 They recognized follicular lymphoma (FL) as a distinctive morphologic and clinical entity, and described instances of histologic progression over time.13 This was the first widely used classification of lymphomas in the United States; this classification included Hodgkin disease as a separate type of lymphoma, but further subdivisions of Hodgkin disease were proposed by Jackson and Parker.48
Beginning of the modern era
The Rappaport classification was initially published in 1956 in a report primarily focused on FL,18 and fully developed in the Armed Forces Institute of Pathology (AFIP) fascicle of 1966. Rappaport questioned the concept of the time that FL could arise from reactive lymphoid follicles, and to avoid this confusion, he proposed the term “nodular” to replace “follicular” when describing the pattern of the lymphoma. He further observed that most cytologic types of lymphoma could have either a nodular or diffuse pattern, including Hodgkin lymphoma. Thus, the Rappaport classification took as its primary stratification the pattern of the lymphoma—nodular or diffuse.19 The previously well-defined “FL” of Gall and Mallory was lost amid 4 categories of “nodular lymphoma”: well differentiated lymphocytic, poorly differentiated lymphocytic, mixed lymphocytic and histiocytic, and histiocytic. Within each tumor type, those with a nodular pattern in general had a better prognosis than those with a diffuse pattern. Despite the fact that by 1966, the phenomenon of lymphocyte transformation had been recognized,15 the Rappaport classification continued to regard neoplasms of large cells as derived from nonlymphoid stromal or other cell types. Thus, the term “histiocytic” replaced the terms “reticulum cell or clasmatocyte,” and “undifferentiated” replaced the “stem cell” of Gall and Mallory. This classification was widely accepted in the United States, where the high frequency of FL meant that simply recognition of a nodular pattern was highly clinically useful in predicting prognosis.
In the same era, in 1966, Lukes and Butler published a new classification of Hodgkin disease, recognizing the new categories of nodular sclerosis and mixed cellularity types, formerly lumped together as “Hodgkin granuloma.”20 They also defined what came to be known as nodular lymphocyte predominant Hodgkin lymphoma (NLPHL), describing 2 forms rich in normal lymphocytes and histiocytes that could have either a nodular or predominantly diffuse growth pattern. This subtype contained a variant of the classical Reed-Sternberg cell, which they termed the L&H cell, often informally referred to as a “popcorn cell.” The subsequent Rye conference reduced the 6 subtypes of Lukes and Butler to 4, combining the nodular and diffuse forms of lymphocytic and histiocytic into lymphocytic predominance (LP), and the reticular and diffuse fibrosis forms of Hodgkin disease into lymphocyte depleted.49 The lymphocyte depleted group was the most problematic of the Lukes-Butler scheme, and probably included cases of classical Hodgkin lymphoma as well as pleomorphic B-cell and T-cell lymphomas.50 Nevertheless, the subsequent 50 years have seen remarkably few changes in the Lukes-Butler classification of Hodgkin lymphoma, with most of its basic principles affirmed by subsequent biological studies.51,52
In the 1960s, 2 discoveries revolutionized the understanding of the immune system and its neoplasms. These were (1) the potential of lymphocytes—which had been thought to be end-stage, terminally differentiated cells—to transform into large, proliferating cells in response to mitogens or antigens;15 and (2) the existence of several distinct lymphocyte lineages (T, B, and NK) that could not be reliably predicted by morphology, but that had different functions and physiology (Figures 2, 3).53,54 In the early 1970s, lymphoid cells were found to have surface antigens or receptors that could be exploited to identify the lineage of both normal and neoplastic cells.55,56 These observations led to the recognition that lymphomas were tumors of the immune system. One of the first lymphomas to be subjected to this analysis was Rappaport's nodular lymphoma, which was shown to be of follicular B-cell origin using these new techniques.24 Similarly, tissue lysates created from biopsy specimens of “reticulum cell sarcomas” showed high levels of IgM, providing evidence for a B-cell derivation.21 The “E rosette” phenomenon used sheep erythrocytes to identify the as-yet-undiscovered CD2 antigen on T cells; this method identified the cells of Sezary syndrome and most lymphoblastic lymphomas to be of T-cell derivation.57,58
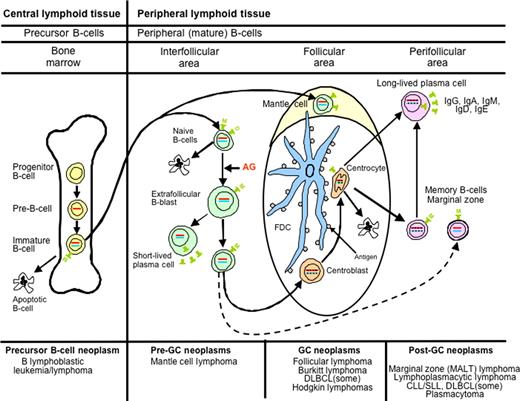
Diagrammatic representation of B-cell differentiation and relationship to major B-cell neoplasms. B-cell neoplasms correspond to stages of B-cell maturation, even though the precise cell counterparts are not known in all instances. Precursor B cells that mature in the bone marrow may undergo apoptosis or develop into mature naive B cells that, following exposure to antigen and blast transformation, may develop into short-lived plasma cells or enter the germinal center (GC), where somatic hypermutation and heavy chain class-switching occur. Centroblasts, the transformed cells of the GC, either undergo apoptosis or develop into centrocytes. Post-GC cells include both long-lived plasma cells and memory/marginal zone B cells. Most B cells are activated within the GC, but T cell–independent activation can take place outside of the GC and also probably leads to memory-type B cells. Monocytoid B cells, many of which lack somatic hypermutation, are not illustrated. AG indicates antigen; and FDC, folllicular dendritic cell. Red bar represents immunoglobulin heavy chain gene (IGH@) rearrangement; blue bar, immunoglobulin light chain gene (IGL) rearrangement; and black insertions in the red and blue bars indicate somatic hypermutation.
Diagrammatic representation of B-cell differentiation and relationship to major B-cell neoplasms. B-cell neoplasms correspond to stages of B-cell maturation, even though the precise cell counterparts are not known in all instances. Precursor B cells that mature in the bone marrow may undergo apoptosis or develop into mature naive B cells that, following exposure to antigen and blast transformation, may develop into short-lived plasma cells or enter the germinal center (GC), where somatic hypermutation and heavy chain class-switching occur. Centroblasts, the transformed cells of the GC, either undergo apoptosis or develop into centrocytes. Post-GC cells include both long-lived plasma cells and memory/marginal zone B cells. Most B cells are activated within the GC, but T cell–independent activation can take place outside of the GC and also probably leads to memory-type B cells. Monocytoid B cells, many of which lack somatic hypermutation, are not illustrated. AG indicates antigen; and FDC, folllicular dendritic cell. Red bar represents immunoglobulin heavy chain gene (IGH@) rearrangement; blue bar, immunoglobulin light chain gene (IGL) rearrangement; and black insertions in the red and blue bars indicate somatic hypermutation.
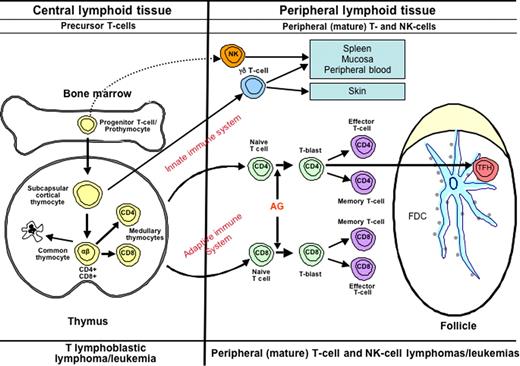
Diagrammatic representation of T-cell differentiation and function. Lymphoid progenitors enter the thymus where precursor T cells develop into varied types of naive T cells. The cells of the innate immune system include NK cells, γδ T cells, and NK-like T cells. These cells constitute a primitive type of immune response that lacks both specificity and memory. In the adaptive immune system, αβ T cells leave the thymus, where, upon exposure to antigen, they may undergo blast transformation and develop further into CD4+ and CD8+ effector and memory T cells. T cells of the adaptive immune system are heterogeneous and functionally complex, and include naive, effector (regulatory and cytotoxic), and memory T cells. Another specific type of effector T cells is the follicular helper T-cell that is found in GCs (TFH). Upon antigenic stimulation, T-cell responses may occur independent of the GC, or in the context of a GC reaction. The lymphomas of the innate immune system are predominantly extranodal in presentation, mirroring the distribution of the functional components of this system.113 T-cell lymphomas of the adaptive immune system present primarily in adults, and are mainly nodal in origin.
Diagrammatic representation of T-cell differentiation and function. Lymphoid progenitors enter the thymus where precursor T cells develop into varied types of naive T cells. The cells of the innate immune system include NK cells, γδ T cells, and NK-like T cells. These cells constitute a primitive type of immune response that lacks both specificity and memory. In the adaptive immune system, αβ T cells leave the thymus, where, upon exposure to antigen, they may undergo blast transformation and develop further into CD4+ and CD8+ effector and memory T cells. T cells of the adaptive immune system are heterogeneous and functionally complex, and include naive, effector (regulatory and cytotoxic), and memory T cells. Another specific type of effector T cells is the follicular helper T-cell that is found in GCs (TFH). Upon antigenic stimulation, T-cell responses may occur independent of the GC, or in the context of a GC reaction. The lymphomas of the innate immune system are predominantly extranodal in presentation, mirroring the distribution of the functional components of this system.113 T-cell lymphomas of the adaptive immune system present primarily in adults, and are mainly nodal in origin.
In response to the new information, pathologists appropriately began to apply it to the classification of lymphomas. In the 1970s, several European and American groups published proposals for the classification of lymphomas.59-62 The first and most significant of these efforts was led by Karl Lennert in Kiel, Germany, who first recognized that many lymphomas resembled germinal center cells, and had used ultrastructural studies to identify follicular dendritic cells in normal and neoplastic lymph nodes, linking lymphomas with a nodular growth pattern to the lymphoid follicle.63 The Kiel classification was published in final form in 1974, fully described in a monograph in 1978,64 and later updated.65 Lymphomas were classified according to a hypothetical scheme of lymphocyte differentiation, and the nomenclature reflected the putative normal counterpart of the neoplastic cells. Although the majority of the neoplasms described were B-cell, several well-defined types of T-cell lymphomas were included. The neoplasms were grouped according to histologic features into low-grade malignancy (predominance of small cells or “-cytes”) and high-grade malignancy (predominance of “-blasts”). This classification became widely used in Europe, but never supplanted the Rappaport classification, popular among clinicians, in the U.S.
During the same era, clinicians were advancing their knowledge regarding the clinical behavior of lymphomas and patterns of spread through advances in the treatment and staging of lymphoid neoplasms.66,67 As treatment regimens improved, the heterogeneity among different types of lymphomas became more apparent.68,69 However, the use of different classification systems in clinical studies made it difficult to compare published results from different centers. Several meetings were held to try to break the deadlock, the last of which was held at Airlie House in Warrenton, Virginia, in 1975.8 The inability of the pathologists to develop consensus and agree on a common approach led to a National Cancer Institute–directed study to evaluate the 6 published schemes. None of the schemes proved clearly superior in predicting survival, and since the pathologists would not agree to using one scheme over the others, the Working Formulation (WF) for the non-Hodgkin lymphomas (NHL) was developed to translate among them.25
The WF stratified lymphomas according to clinical outcome, based on the survival of patients in clinical trials conducted in the 1970s.25 It co-opted terminology from the pathology literature related to cytologic grade (low grade, intermediate grade, and high grade) and created clinical groupings that were intended to provide a clinical guide for patient management. The categories closely followed those of the Rappaport classification,19 with updated terminology from Lukes and Collins.59 Since the scheme did not use immunophenotyping, which was felt at the time to be beyond the reach of the routine pathology laboratory, and since it attempted to cover all entities in all classifications in a few categories, the categories were of necessity heterogeneous. It is therefore not surprising that pathologists could not use these categories reproducibly.70 The WF substituted the term “large cell” for “histiocytic” and divided large cell lymphomas into 2 types: large cell and large cell immunoblastic. This separation split the diffuse large-cell lymphomas into 2 different treatment groups (intermediate and high grade), based on questionable morphologic distinctions.71 These distinctions were not reproducible, and the clinical groupings could not be validated. In many respects the WF was a step backward, since it did not recognize well-defined entities such as centrocytic lymphoma from the Kiel classification, which is now known as mantle cell lymphoma (MCL), and made no use of widely available immunologic knowledge techniques for classification or diagnosis—for example, lumping both T-cell lymphomas and many diffuse B-cell lymphomas in a single category (diffuse mixed small and large cell).
Although not intended to serve as a freestanding classification scheme, the WF was a convenient guide to therapy, quickly became popular among clinicians, and was adopted for use in many centers in the U.S. for clinical trials. Following the publication of the WF, the political situation was unchanged. The Kiel classification remained popular in Europe and in Asia; the WF largely replaced the Rappaport classification in the U.S., but many centers used the Lukes-Collins classification. This situation caused continued problems for both pathologists and clinicians in interpreting the results of published studies. In addition, in the 1980s and early 1990s, many new diseases were described that were not included in either classification, including anaplastic large cell lymphoma (ALCL), lymphomas of the mucosa-associated lymphoid tissues (MALT), and adult T-cell leukemia/lymphoma.
The immunologic and genetic revolutions
In 1975, Kohler and Milstein created the hybridoma technology that led to the development of monoclonal antibodies.72 Before this revolution, cell-surface marker and immunohistochemistry studies had been performed with rabbit or sheep polyclonal antisera, but these reagents were hampered by limited supply, lack of standardization, and the relatively few antigens that were recognized. In 1979, the first monoclonal antibody against a human lymphocyte differentiation antigen was generated against an antigen expressed on normal thymocytes.29 The antigen recognized by NA1/34 was later designated as CD1a in the human leukocyte differentiation antigen (HLDA) system.34 The CD nomenclature, which stood for “clusters of differentiation,” came into use through a series of workshops organized to bring order out of chaos in this newly emerging field. The initial workshops dealt only with antigens expressed on the cell membrane, all of which were given a CD designation, but later workshops began to look at antigens expressed in the nucleus and cytoplasm.73 By the most recent eighth meeting of what is now called Human Cell Differentiation Molecules workshop, a total of 350 CD designations had been defined.
In these early years, monoclonal antibodies were applied to cells in suspension, or somewhat later to cryostat tissue sections. However, a paradigm shift occurred when David Mason and others not only adapted the techniques to routine formalin-fixed paraffin embedded (FFPE) sections, but changed the strategy for screening monoclonals to look for those antibodies that would have optimal reactivity in FFPE sections.23,30,74 These advances had a dramatic impact on the field. First, one did not have to ensure that tissues were snap-frozen or made into cell suspension to perform immunophenotypic studies. Second, the better morphology of paraffin sections improved the pathologist's ability to characterize positive and negative cells. This technology was rapidly adopted by pathologists both at academic centers and in community hospitals. Characteristic immunophenotypes for many B-cell and T-cell malignancies were becoming recognized, and the ready accessibility of monoclonal antibodies adapted for use in immunohistochemistry in routine paraffin sections made new discoveries easily transportable and testable in different laboratories.
In parallel, there was equally dramatic progress in understanding the genetics of lymphoid malignancies. Recurrent cytogenetic abnormalities were identified, following the early observations of recurring cytogenetic alterations in myeloid leukemias.75 The first to be recognized were the t(14;18)(q32;q21) of FL, and t(8;14)(q24;q32) of Burkitt lymphoma.27,28,37 Subsequent studies led to the cloning of the genes involved in these translocations. The laboratories of Philip Leder and Carlo Croce in 1982 both identified MYC as the gene that was translocated into the immunoglobulin genes in human Burkitt lymphoma,35,36 and other similar discoveries soon followed, such as the BCL2/IGH@ in FL76 and the CCND1/IGH@ in MCL.77,78 The most common paradigm for translocations involving the immunoglobulin heavy chain gene, IGH@ at 14q24, is that a cellular proto-oncogene comes under the influence of the IGH@ promoter. There are also less frequent but parallel alterations involving the T-cell receptor genes in T-cell malignancies.
The process of rearrangement of the immunoglobulin and T-cell receptor genes during normal lymphoid cell development was discovered, and the technology exploited by using rearrangement of the antigen receptor genes as markers of both lineage and clonality in lymphoid neoplasms.79 It was later shown that B cells that have transited the germinal center show evidence of somatic hypermutation of the IGH@ variable region genes.80 Thus, this knowledge could be exploited, not only to show lineage, but stage of differentiation, at least within the B-cell system.81,82
In addition, the development of polymerase chain reaction (PCR)– and fluorescence in situ hybridization (FISH)–based strategies meant that genetic testing no longer required karyotyping of viable cells or labor-intensive Southern blot analysis of fresh or snap-frozen material. The new techniques permitted analysis of antigen receptor gene and oncogene rearrangements on FFPE sections, facilitating the testing of routine biopsies for clinical diagnosis.83-86 Another critical advantage of the PCR-based strategies was the ability to investigate genetic alterations at the single-cell level. This was particularly important in the study of Hodgkin lymphoma, in which the neoplastic cells represented only a minor component of the entire tumor mass. PCR techniques coupled with single-cell microdissection led to the demonstration of IGH@ gene rearrangements in Reed-Sternberg cells, ending the long debate regarding the origin of the malignant cell.41,87
While translocations involving oncogenes or tumor suppressor genes were demonstrated to be of major importance in the pathogenesis of many lymphomas, integration of viral genomes into the neoplastic cells was demonstrated for several lymphoid malignancies. Epstein-Barr virus (EBV) was shown to be especially promiscuous and capable of transformation of B cells, T cells, and NK cells.17,88-90 HTLV1 and HHV-8/KSHV were identified as playing a role in the pathogenesis of adult T-cell leukemia/lymphoma,91 primary effusion lymphoma,92 and the lymphoma associated with multicentric Castleman disease.93-95
Identifying Hodgkin disease as a lymphoid neoplasm
From its initial description until the 1990s, the nature and lineage of the Reed-Sternberg cell and the inflammatory infiltrate that comprise Hodgkin disease was debated—was this an infectious or inflammatory process with bizarre cells infected by a virus, or a malignant process with a prominent inflammatory component—and what was the lineage of the infected or malignant cell? Hypotheses and bits of supporting evidence suggested almost every known immune cell type: reticulum cell, dendritic cell, histiocyte/macrophage, B cell, and T cell. The major problem for many years was the relative infrequency of the abnormal cells compared with reactive cells, making it difficult to apply immunophenotyping and genetic techniques to the question.
In the 1970s and 1980s, a number of cell lines were developed from patients with advanced-stage Hodgkin disease, and cytogenetic analysis of both these cells and fresh tumor specimens demonstrated abnormal karyotypes; together with the clinical aggressiveness of the disease, these observations confirmed that the disease was indeed a malignancy.96 In the early 1980s, Stein and colleagues at Kiel immunized mice with Hodgkin cell lines established by Diehl and associates, and developed the Ki-1 antibody, recognizing the CD30 antigen, which was found to be expressed by all Hodgkin and Reed-Sternberg (HRS) cells and by rare lymphoid blasts in normal lymphoid tissues.97 In vitro studies revealed that CD30 expression could be induced in B and T cells by mitogens and by EBV infection, suggesting that CD30+ HRS cells might be related to lymphoid cells.5,98 In the 1980s, the development of antibodies that detected B cell– and T cell–specific antigens in paraffin sections, providing sufficient morphologic detail to recognize HRS cells, showed expression of the B-cell antigen CD20 on some of the HRS cells in a proportion of patients with classical Hodgkin lymphoma (CHL).99,100 The detection of EBV genomes in HRS cells provided additional support for a lymphoid and possibly B-cell origin.101,102 Further evidence pointing toward a B-cell derivation came from the observation of composite lymphomas and metachronous CHL and NHLs, in which the NHL component was nearly always of B-cell origin, most commonly FL.103 Finally, in the 1990s, the PCR technique and primers specific for target sequences of the IGH@ and T-cell receptor (TCR) loci became available, and a method of isolating single HRS cells from frozen sections by microdissection was developed.80 The application of these techniques revealed that HRS cells were clonal B cells in 98% of the patients studied, thus confirming that they were neoplastic and of B-cell origin.41,82 This latter finding led to the change of the designation of Hodgkin disease into Hodgkin lymphoma in the WHO classification of lymphoid neoplasms.
With the recognition that nearly all instances of CHL show evidence of B-cell lineage, the following question arose: why do HRS cells express so few B-cell antigens, lack expression of immunoglobulin, and display markers not normally ex-pressed by B cells, such as CD15, TARC, or T cell–associated antigens?97,104-107 A number of explanations have been suggested, including the presence of crippling mutations in the immunoglobulin variable region genes,108 methylation of the immunoglobulin promotors,109 defects in B cell–associated transcription factors,110 and up-regulation of genes that suppress the B-cell gene expression program.111,112 The extinction of the B-cell gene expression program in HRS cells is a complex process, and its full elucidation will likely contribute to our understanding of the pathogenesis of CHL.
The REAL and WHO classifications
In 1991, an international group of pathologists (International Lymphoma Study Group [ILSG]) was formed by Peter Isaacson and Harald Stein to promote better understanding between European and American hematopathologists. At the first meeting held in London, the participants discussed a variety of topics, and found common ground on most issues. Shortly thereafter the group published a consensus report on the definition of MCL, and proposed that the term MCL be used to the exclusion of centrocytic, intermediate, or diffuse small cleaved cell lymphoma, which were overlapping but not precisely defined categories in the Kiel, modified Rappaport, and WF classifications, respectively.40 The ILSG defined MCL by a combination of morphology, immunophenotype, and genetic anomalies, and noted that it had a characteristic clinical profile. A similar report followed at the next meeting in 1992, defining nodular lymphocyte-predominant Hodgkin lymphoma (NLPHL) and elucidating criteria to distinguish it from CHL.51
At this meeting, the group felt it should try to define as many of the currently recognized entities as possible. At the third meeting, in Berlin in 1993, the group was able to reach consensus on a long list of lymphoid neoplasms, which formed the basis of a new classification of lymphoid neoplasms called the Revised European-American Classification of Lymphoid Neoplasms (REAL classification). The REAL classification, published in Blood in 1994,42 was among the 5 most highly cited papers in clinical medicine for the decade. The REAL classification, and its successor the WHO classification,45 represented a new paradigm in the classification of lymphoid neoplasms. The focus was on the identification of “real” diseases, rather than a global theoretical framework, such as survival (WF) or cellular differentiation (Kiel and Lukes-Collins classifications). The REAL classification was based on the building of consensus, and recognized that a comprehensive classification system was beyond the experience of any one individual. The 19 members of the ILSG contributed their diverse perspectives to achieve a unified point of view. In addition, the ILSG made the decision to base the classification exclusively on published data; in order for an entity to be included in the REAL classification, it had to be validated in more than one publication. A number of entities were listed as provisional, based on more limited published data. Recognizing that Hodgkin lymphoma and plasma cell myeloma are both lymphoid in origin, and that many lymphoid neoplasms can have both solid and circulating phases, the classification included all lymphoid neoplasms: Hodgkin lymphoma, so-called NHLs, lymphoid leukemias, and plasma cell disorders. The neoplasms were stratified according to lineage (B-cell and T/NK-cell), and further into precursor (lymphoblastic) versus mature/peripheral T- and B-cell neoplasms, and Hodgkin lymphoma.
The REAL classification defined distinct entities using a constellation of features: morphology, immunophenotype, genetic features, and clinical presentation and course. The REAL classification appreciated the importance of genetic abnormalities in defining disease entities. With advances in monoclonal antibody technology, some genetic abnormalities could be recognized by immunohistochemistry, such as cyclin D1 expression in the diagnosis of MCL, and ALK expression in ALCL. However, for many lymphoma subtypes, particularly the mature T-cell malignancies, the molecular pathogenesis was not yet known. The inclusion of clinical criteria, which played a major role in the classification of T-cell lymphomas, was one of the most novel aspects of the ILSG approach.113 The REAL classification recognized that the site of presentation is often a signpost for underlying biological distinctions, as in extranodal lymphomas of MALT,114 or primary mediastinal large B-cell lymphoma. The ILSG appreciated that accurate diagnosis cannot take place in a vacuum and requires knowledge of the clinical history since biologically distinct entities may appear cytologically similar.
The REAL classification recognized that because of limitations in current knowledge, some broad categories of disease could not be resolved with existing data, such as diffuse large B-cell lymphomas (DLBCLs) and peripheral T-cell lymphomas (PTCLs), unspecified or not otherwise specified (NOS). Although a number of morphologic variants had been described in both groups, evidence that these delineated distinct biological or clinical entities was lacking. The ILSG identified these categories as ripe for further studies. Indeed, as expected, new technologies have helped delineate separate biological entities within DLBCL and to a lesser extent PTCL-NOS. Gene expression profiling dissected 2 major categories from DLBCL, the germinal center B-cell (GCB) and activated B-cell type (ABC) types of DLBCL, with different patterns of transformation and deregulation.44 The relevance of the microenvironment was appreciated, and the various gene signatures could be correlated with clinical outcome and response to therapy.115,116 Gene expression profiling also validated the distinction of primary mediastinal large B-cell lymphoma from other DLBCL, which was a feature of the REAL classification.117,118
The REAL classification did not attempt to stratify lymphomas according to a concept of “grade,” either histologic or clinical, as had been done in the Kiel classification and the WF. We now recognize that lymphomas are a heterogeneous group of distinct diseases, most unrelated to one another, not a single disease with a spectrum of histologic grade and clinical behavior. In addition, many lymphomas have within them a spectrum of clinical behavior, which sometimes can be predicted by pathologic features (cell size, proliferation) or clinical features (age, stage, the International Prognostic Index [IPI]). Thus, the ILSG felt that it was neither practical nor helpful to attempt to sort these diverse diseases according to either histologic features or clinical aggressiveness. Both clinicians and pathologists need to learn the histologic and clinical spectrum of each distinct disease. In the REAL classification, grading was used within a disease entity, such as FL, but not across a range of different diseases. Moreover, low cytological grade does not necessarily translate into indolent clinical behavior. Both MCL and angioimmunoblastic T-cell lymphoma had been designated as cytologically low grade, but both diseases are associated with an aggressive clinical course. Conversely, ALCL, which cytologically is high grade, has a better prognosis than most other nodal T-cell lymphomas, with an excellent response to chemotherapy and prolonged disease-free survival.43
Following the publication of the REAL classification, an international study directed by James Armitage sought to determine whether the REAL classification could be readily applied by a group of independent expert pathologists and had clinical relevance.43 Other goals of the International Lymphoma Classification Project were (1) to determine the role of immunophenotyping and clinical data in the diagnosis of disease entities; (2) to determine both intraobserver and interobserver reproducibility in the diagnosis of the various entities; (3) to further investigate the clinical features and/or epidemiology of the various entities; and (4) to determine whether clinical groupings would be practical or useful for clinical trial or practice. The conclusions of that study affirmed the principles of the REAL classification.43 Virtually all cases could be classified in the published scheme. Intraobserver and interobserver rates of reproducibility were excellent. The use of precise disease definitions, as provided by the REAL scheme, enhanced diagnostic accuracy and reduced subjectivity on the part of pathologists. Immunophenotyping was found to be essential for many diagnostic categories, such as most peripheral T-cell lymphomas. Importantly, the significance of identifying individual disease entities was confirmed by survival data. The International Classification Lymphoma Classification project also elucidated the importance of clinical factors such as the IPI in determining clinical outcome and response to therapy within disease entities, confirming the concept that stratification of a diverse group of diseases by either cytologic or clinical “grade” was unrealistic.119
Shortly after publication of the REAL classification, the WHO decided to update the classification of hematopoietic and lymphoid neoplasms for its “Blue Book” series of Classifications of Tumors. The task for developing the classification was undertaken as a joint project by the Society for Hematopathology (SH) and the European Association of Hematopathology (EAHP), with a goal to achieve consensus and avoid the political divisions of the past. A steering committee was appointed by the 2 societies, which in turn established 10 individual committees to deal with different disease groups within hematopoietic and lymphoid malignancies.120 The WHO classification was developed over a period of 7 years, during which time the proposal was extensively discussed and vetted at a number of international meetings and symposia to ensure worldwide acceptance. Approximately 100 pathologists and clinicians gathered at a clinical advisory meeting in 1997 at Airlie House, where an agreement had so spectacularly failed in 1975, to discuss a number of questions of clinical relevance. A consensus was achieved on most of the questions raised.121 Importantly, the group concluded that clinical groupings for either protocol treatment or routine clinical practice were generally not feasible. In considering new therapies, each disease must be evaluated individually. Indeed, treatment approaches for one type of lymphoid malignancy are not necessarily applicable to other diseases, even of the same cell lineage. This point is exemplified by the broad spectrum of lymphoid malignancies composed of small B lymphocytes (ie, chronic lymphocytic leukemia (CLL)/small lymphocytic leukemia (SLL), hairy cell leukemia, MALT lymphoma, FL, and MCL). Each of these tumors exhibits deregulation of distinct signaling or transformation pathways, and thus there should be no expectation that the optimal therapy for all small B-cell neoplasms should be the same.
While work on the WHO classification was in progress, Paul Kleihues became Director of the International Agency for Research on Cancer (IARC), an agency of the WHO. Recognizing the growing role of genetics in the definition of cancers and the need for international consensus-based classifications, he initiated a new series of monographs focusing on the pathology and genetics of cancer, published by IARC Press.122 The approach to disease definition and consensus development that was introduced in the REAL classification and adopted in the WHO classification of hematologic and lymphoid neoplasms was a paradigm for this approach. The publication of the WHO classification in 2001 marked the beginning of a new era in which all scientists and clinicians as well as pathologists involved in lymphoma research, diagnosis, and patient care would finally speak the same language.
Discovering diseases: MALT lymphoma as a paradigm
Each lymphoma included in the WHO classification is a distinct disease entity. Defining a disease is a multistep process, but typically begins not in the basic science laboratory, but at the bedside or at the microscope. This process of disease discovery is exemplified by MALT lymphoma, but the same tale could be told for any number of diseases, such as adult T-cell leukemia/lymphoma,91,123 MCL,3,6,56,124, or ALCL.5,125,126
In 1963, Frand and Ramot drew attention to the high frequency of a unique variety of intestinal lymphoma in non-Ashkenazi Jews and Arabs in Israel.127 The histology of this condition, subsequently called Mediterranean lymphoma, was characterized as ranging from intense lymphoplasmacytic infiltration of the intestinal mucosa to frank large-cell lymphoma. Seligmann et al observed that patients with Mediterranean lymphoma had circulating alpha heavy chain with absent light chain and introduced the term “alpha chain disease (ACD).128 There were doubts whether ACD represented true lymphoma, particularly since some patients could be cured with antibiotics and, accordingly at a WHO conference in 1976, ACD was renamed yet again as an immunoproliferative small intestinal disease (IPSID). In the late 1970s and early 1980s, based on careful morphologic analysis and demonstration that ACD was monoclonal, Isaacson et al showed that IPSID was indeed a low-grade lymphoma.129
In the period between 1960 and 1980 the term “pseudolymphoma” came increasingly to be used for low-grade lymphoproliferative lesions arising at a variety of extranodal sites, including the stomach, lung, thyroid, and ocular adnexa. In 1983, Isaacson and Wright showed that gastric pseudolymphoma was a monotypic disorder (ie, a lymphoma) remarkably similar to IPSID.130 The properties of both lymphomas simulated those of MALT, giving rise to the term MALT lymphoma. It soon became clear that a number of other extranodal indolent B-cell lymphomas, many of which had previously been called pseudolymphomas, were examples of MALT lymphoma.131,132 Subsequent studies showed that the morphology and immunophenotype of MALT lymphoma recapitulated those of the Peyer patch, more specifically the Peyer patch marginal zone cells.133
MALT lymphoma usually presents as localized disease (stage 1E) but characteristically disseminates, either within the same organ or to other extranodal sites where MALT lymphomas are known to arise.134,135 MALT lymphomas typically arise from sites such as the stomach, where there is no organized lymphoid tissue. In seeking an explanation for this paradox, Isaacson hypothesized that Helicobacter pylori infection may result in accumulation of MALT from which gastric MALT lymphoma arises.136 Serial studies showed that there is indeed a close association of infection with H pylori and gastric MALT lymphoma, and that the growth of gastric MALT lymphoma cells can be stimulated by H pylori strain–specific T cells.137 Moreover, in 75% of patients, antibiotic eradication of H pylori leads to regression and effective cure of gastric MALT lymphoma.138 There is an interesting parallel with earlier observations of complete response of IPSID to antibiotics, where there is some evidence that Campylobacter jejuni may be the organism involved,139 and other bacterial and viral agents have been implicated in the pathogenesis of other forms of marginal zone lymphoma.140,141
Numeric chromosomal alterations, especially trisomies 3, 12, and 18, are common in MALT lymphomas. Chromosomal translocations associated with MALT lymphomas include t(11:18)(q21:q21), resulting in the production of a chimeric protein (API2-MALT1);142 and t(1;14)(p22;q32), t(14;18)(q32;q21), and t(3;14)(p14.1;q32), resulting respectively in transcriptional deregulation of BCL10, MALT1, and FOXP1.143-145 The frequencies at which the translocations occur vary markedly with the primary site of disease.146 This is unlike most other low-grade lymphomas, where a single translocation is characteristic. There is mounting evidence, however, that these different translocations are linked by the roles of BCL10 and MALT1 in the NFκB molecular pathway in lymphocytes. Thus, perhaps all of the genetic alternations appear to lead to deregulation of a common pathway.
Lymphoma classification in the third millennium
The WHO classification has been updated in the past 2 years, again as a joint effort of the hematopathology societies, with 2 clinical advisory committees and more than 130 authors from 22 countries (Table 3). Published in September 2008, it builds upon the advances of the past and makes some inroads into better defining heterogeneous or ambiguous categories of disease.1 Some changes include the introduction of provisional borderline categories, the recognition of small clonal lymphoid populations, and the identification of diseases characterized by involvement of specific anatomic sites or by other clinical features such as age. Unresolved issues include defining pathologic predictors of prognosis in common diseases such as FL, DLBCL, and peripheral T-cell lymphomas.
In the past 20 years there has been a greater appreciation of morphologic and immunophenotypic overlap between CHL and some large B-cell lymphomas—usually primary mediastinal large B-cell lymphoma (PMBL) and mediastinal nodular sclerosis subtype of classical Hodgkin lymphoma (NSCHL).103,146 In most cases, one or the other diagnosis can be made, but there may be a true biological gray zone between these entities, both of which occur in young adults and involve the mediastinum and have similarities in gene expression profiles.117,118 The 2008 WHO classification recognizes a provisional category of B-cell neoplasms with features intermediate between DLBCL and CHL.147,148 These tumors occur predominantly in young men and appear to be more aggressive than either PMBL or NSCHL; in some patients, PMBL may be followed by CHL or vice versa.
A second borderline category relates to the distinction of classical Burkitt lymphoma from diffuse large B-cell lymphomas that also carry a MYC translocation. Many of these occur in adults and morphologically resemble Burkitt lymphoma.149 The 2008 WHO classification includes a provisional category of B-cell lymphoma, unclassifiable, with features intermediate between DLBCL and Burkitt lymphoma. Many lymphomas in this grouping have a translocations of both MYC and BCL2 (“double hit”), and have a very aggressive clinical course.150 While gene expression profiling may show similarities with classical Burkitt lymphoma, other data support segregation of these tumors from Burkitt lymphoma.85,151
The multistep pathway of tumorigenesis has parallels in most organ systems, best documented in the evolution of colonic adenocarcinoma.152 Histologic progression is a well-recognized feature of many lymphoid neoplasms, but the earliest events in lymphoid neoplasia are difficult to recognize. In fact, the lymphoid system has no recognized “benign neoplasms,” a fact that may be related to the propensity of lymphoid cells or to circulate or home, and not remained confined to a single anatomic site.153 The 2008 WHO classification addresses the problem of clonal expansions of B cells, or less often T cells, that appear to have limited potential for histologic or clinical progression. For example, although up to 70% of healthy adults have circulating clonal memory B cells with the t(14;18)(q32;q21), these cells presumably lack other genetic alterations necessary for development of malignant behavior.154,155 A total of 3% to 5% of healthy adults and more than 10% of those referred for evaluation of lymphocytosis have circulating monoclonal B cells with the immunophenotype of CLL (monoclonal B lymphocytosis); many of these clones also have genetic abnormalities associated with good-prognosis CLL, yet they rarely progress to overt, progressive leukemia.156,157
Among lymphomas, in situ or early lesions have been recognized for both FL and MCL.158,159 The risk for progression to clinically significant lymphoma is not yet fully known for these focal lesions, which are often incidental findings in an otherwise reactive-appearing lymph node. A related condition is localized FL presenting as small polyps in the duodenum; these duodenal FLs rarely if ever progress to nodal or systemic disease.160,161 Duodenal FL cells express intestinal homing receptors that may retain the clonal B cells within the intestinal mucosa.162 Early gastric MALT lymphomas that are dependent on the presence of H pylori–activated T cells for survival and lack genetic alternations might also be considered benign or “in situ” lymphomas.163 Cases of reactive follicular hyperplasia in children have been reported that contain clonal populations of CD10+ germinal center B cells, and yet do not progress to overt lymphoma.164 Likewise, nodal marginal zone lymphomas in children appear to have a low risk of progression.165 In the T-cell system, primary cutaneous CD30+ T-cell lymphoproliferative disorder, lymphomatoid papulosis, is a clonal T-cell proliferation that also has limited malignant potential.166,167
Through studying these early events in lymphomagenesis, we are learning more about the circulation and homing of normal and malignant B cells and gaining insight into normal B-cell physiology. One of the great attributes of pathology as a discipline is that disease is a model that provides insight into the functioning of the healthy human organism. As we better understand the abnormal or diseased tissues, we better understand normal human physiology.
The 2008 WHO classification also emphasizes the importance of anatomic site in classification. In addition to MALT lymphomas and primary mediastinal large B-cell lymphoma, both B-cell and T-cell lineages involving cutaneous or other extranodal sites such as the central nervous system are now recognized as distinctive.168 Age may also be a factor in disease definition. Pediatric marginal zone lymphomas and pediatric FLs have been described, which tend to be localized and have an excellent prognosis.165,169,170 They differ in pathogenesis from morphologically similar lymphomas in adults, as pediatric FL typically lacks BCL2 expression and the t(14;18)(q32;q21). In contrast, some diseases appear to occur most often at advanced age, such as EBV+ DLBCL in elderly persons, which likely arise because of decreased immune surveillance.171
In 2 of the most common lymphomas—FL and DLBCL—there is a need for pathologic predictors of outcome and response to treatment. FL has traditionally been graded according to the proportion of centroblasts—a continuous variable that is associated with decreasing survival duration, but that is poorly reproducible among pathologists. It has become increasingly apparent that cases graded as Grade 1 or Grade 2 have similar outcomes that are not affected by aggressive therapy, and that they do not need to be distinguished from one another. Thus, the 2008 WHO lumps cases with few centroblasts as “FL Grade 1-2 (low grade).” Stratifying FL Grade 3 according to the presence or absence of residual centrocytes (3A vs 3B) was optional in the 2001 WHO classification, but is now mandatory. Some studies have identified biological differences between these 2 subtypes, with most instances of FL Grade 3B more closely related to DLBCL at the molecular level.172,173 However, the segregation is imperfect based on current genetic and clinical studies; this stratification should provide the opportunity to collect more information. Finally, it is emphasized that areas of DLBCL in any FL should receive a separate diagnosis of DLBCL and such patients should be treated as DLBCL (ie, there is no such thing as “FL Grade 3[A or B] with diffuse areas”). After separation of specific new subtypes of DLBCL, we are still left with a large group of DLBCL for which pathologic features are lacking to further stratify them for predicting prognosis or response to therapy. Stratification according to gene expression profiles as GCB versus ABC types has prognostic value, but as yet does not direct therapy. This stratification is imperfectly replicated by morphology, immunophenotyping, or cytogenetic analysis, and thus is not officially incorporated into the classification for practical use. Development of targeted therapies and recognition of additional markers of clinical behavior will likely result in additional modifications to this category in the future.
Finally, an intriguing new development is the recent recognition of lineage plasticity in hematopoietic cells and their neoplasms. In normal B cells, down-regulation of the B-cell regulatory factor PAX-5 can result in reprogramming of both immature and mature B cells to monocytes and even T cells. Cases of lymphoblastic neoplasms of both T- and B-cell type have been reported in which clonally related histiocytic neoplasms have developed, and recently a similar phenomenon has been reported in FL.174,175 This phenomenon may complicate interpretation of the significance of antigen-receptor gene rearrangements in assigning lineage to a neoplasm.
Acknowledgments
The authors dedicate this review to David Y. Mason, Oxford University, who died on February 2, 2008. David Mason was a pivotal figure in the development of immunohistochemistry, and pioneered the development of monoclonal antibodies reactive against epitopes preserved in formalin-fixed paraffin-embedded tissues. As a leader in the establishment of the Human Leucocyte Differentiation Antigen workshops, he helped bring order to a complex and chaotic field. Through his scientific work and reagents that he generously made available on a worldwide basis he helped shape the modern classification of lymphoid malignancies and was one of the most highly cited physicians in the field of clinical oncology. His wit and satire brightened many medical symposia. Indeed he was a scriptwriter for some of the early pre-Monty Python satirical shows, especially “That Was The Week That Was,” and had a long-standing interest in the arts. His enthusiasm for international collaboration led many to visit his laboratory, and he fostered the development of new generations of translational scientists. He will be greatly missed by his students of all ages.
Authorship
Contribution: E.J., N.L.H., H.S., and P.I. all contributed to this historical review by participating in writing the manuscript and in providing figures and graphics material.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Elaine S. Jaffe, Laboratory of Pathology, National Cancer Institute, Building 10, Room 2B 42, 10 Center Drive, MSC 1500, Bethesda, MD 20892; e-mail: elainejaffe@nih.gov.