Abstract
The development and the propagation of chronic lymphocytic leukemia (CLL) has been linked to signaling via the B-cell receptor (BCR). Protein kinase C β (PKCβ) is an essential signaling element of the BCR and was recently shown to be overexpressed in human CLL. We used the TCL1 transgenic mouse model to directly target PKCβ in the development of murine CLL. TCL1 overexpression did restore the CD5+ B-cell population that is absent in PKCβ-deficient mice. However, PKCβ-deleted TCL1 transgenic mice did not develop a CLL disease, suggesting a role of PKCβ in the establishment of the malignant clone. Moreover, targeting of PKCβ with the specific inhibitor enzastaurin led to killing of human CLL samples in vitro. We thus propose that PKCβ may be a relevant target for the treatment of CLL.
Introduction
The B-cell receptor (BCR) is proposed to generate vital signals in the pathogenesis of chronic lymphocytic leukemia (CLL). Specifically in cases with unmutated BCR sequences, crosslinking of the BCR seems to contribute to the survival and proliferation of the CLL cells.1 The observed bias in V-gene usage and the nonrandom nature of rearranged CDR3 sequences in CLL also suggest that BCR signaling is involved in the initial selection and development of the malignant clone.2
Reports have linked the activity of members of the protein kinase C family with the pathogenesis of CLL.3-7 Protein kinase C (PKC) consists of at least 10 isoenzymes with different activation requirements and substrate specificities. Several of these have been associated with diverse cancer settings.8 PKCα and PKCδ have been indirectly associated with CLL.5,7 PKCβ is involved in the transduction and fine-tuning of BCR signals in normal B cells,9 and it has recently been implicated in CLL pathogenesis. Studies have shown an overexpression of PKCβ in human CLL and link the signaling downstream of PKCβ with other relevant signaling events, such as calcium flux, or PKB/AKT phosphorylation.3,4 However, to define the role of PKCβ, these studies used inhibitors that are at best only relatively specific for the enzyme, thus warranting genetic evidence for its contribution to CLL pathogenesis. Although PKCβ is shown to be part of a poor-prognosis gene cluster in CLL linked to the transmission of BCR signals,10 its role in regulating cell survival is more complex. Depending on overall PKCβ expression, either enhanced or decreased survival was observed,3 suggesting that PKCβ signal strength may determine the outcome. Interestingly, targeted deletion of PKCβ in a murine model led to a preferential loss of CD5+ B cells,9 suggesting that in these cells PKCβ provides an essential developmental signal.
We used the TCL1 transgenic mouse model for human unmutated CLL to determine the role of PKCβ in a clean genetic targeting experiment.11,12 CLL cells in these mice display unmutated BCR sequences with a bias regarding the V-gene usage, suggesting a role of antigen-dependent selection also in the mouse model. Importantly, the premalignant stage of CD5+ B-cell hyperplasia lends itself to the exploration of initial stages of the disease.11 We crossed TCL1 transgenic mice with PKCβ knockout mice to assess the effect of PKCβ deletion on the development of both the premalignant phenotype and CLL onset. In addition, we used a novel PKCβ inhibitor, enzastaurin, currently in clinical development, to show the potential of translating our murine findings into the human system (for a review on the substance see Ma and Rosen13 ).
Methods
Mice
Eμ-TCL1 transgenic mice11 and PKCβ knockout mice9 were provided by C. Croce (Columbus, Ohio) and M. Leitges (Oslo, Norway), respectively. Both strains have been backcrossed for 9 generations to C57BL/6 mice. Genotyping of mice was performed on tail DNA by polymerase chain reaction (PCR) as previously described.9,11 Experiments were performed under approval from the Austrian Animal Ethics Committee. Mice in the tumor cohort were followed for signs of illness and killed when moribund. Samples for histology and flow cytometric analysis of tumor tissue were collected. Mice in the pretumor cohort were killed at stated ages.
Human CLL samples
Peripheral blood samples were collected after informed consent was obtained in accordance with the Declaration of Helsinki and under the ethical approval of the Ethics Commission of the State of Salzburg. Peripheral blood mononuclear cells (PBMCs) were isolated by Ficoll density centrifugation as previously described.14
Cell culture and viability analysis
Enzastaurin (LY317615) was diluted in dimethyl sulfoxide (DMSO) and added to cells in culture at the indicated concentrations (for culture conditions see Document S1, available on the Blood website; see the Supplemental Materials link at the top of the online article). Cell viability was assessed as previously described.15
Flow cytometry
CD19 and CD5 antibodies were from BD Bioscience (Franklin Lakes, NJ). Cells were analyzed using a FC500 Beckman Coulter (Fullerton, CA) flow cytometer.
BCR crosslinking experiments
Murine splenocytes were grown for 24 hours in wells of a 96-well plate that were either uncoated or coated with F(ab′)2 goat anti–mouse IgM (Jackson ImmunoResearch Laboratories, West Grove, PA; Dianova, Hamburg, Germany). Apoptosis was assessed by flow cytometry with the use of CD19 for B-cell identification and annexin V and 7-aminoactinomycin D (7AAD) for apoptosis measurements.
Results and discussion
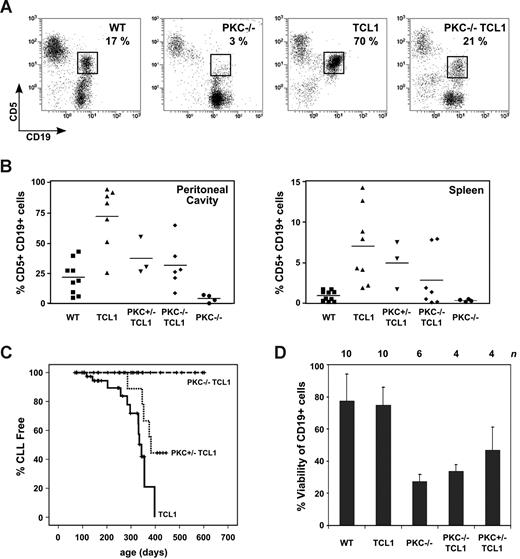
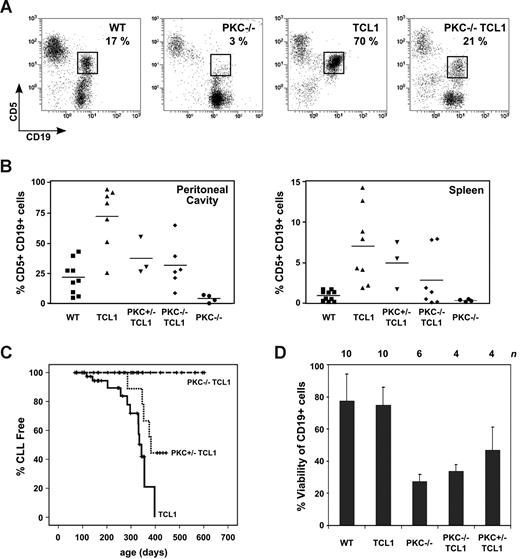
To investigate the role of PKCβ in CLL, we crossed PKCβ knockout mice with the TCL1 transgenic murine CLL model. Our mouse cohort was put onto an inbred C57BL/6 background to escape biases resulting from genetic differences. We first investigated whether abrogation of PKCβ signaling would abolish the pretumor hyperplasia generally observed in TCL1 transgenic mice. Although CD5+ B cells are mostly absent from the parental PKCβ−/− mice, overexpression of TCL1 in the B-cell compartment restored their presence in the peritoneal cavity. However, the CD5+ B-cell hyperplasia characteristically observed in spleens of TCL1 transgenic mice was significantly reduced by loss of PKCβ (Figure 1A,B). This suggests that TCL1 overexpression can compensate for the loss of an otherwise crucial PKCβ signal in this population. It has been suggested that part of the PKCβ survival signal is mediated by AKT.4 Measurement of AKT phosphorylation in native human CLL suggests that PKCβ can activate AKT independent of PI3-kinase (Figure S1). Our data from the mouse model suggest that the proposed amplification of AKT signaling by TCL1 overexpression may substitute for the loss of PKCβ signaling in CD5+ B-cell development by providing the missing AKT signal,11,16 although it cannot be ruled out that TCL1 may have AKT-independent functions. Importantly, the preleukemic accumulation of CD5+ B cells in the TCL1 transgenic mice,11 which is hypothesized to depend on BCR signals,12 depends partially on PKCβ.
TCL1 reconstitutes the absent CD5+ B-cell population in PKCβ-deficient mice, but loss of PKCβ in TCL1 mice abrogates the CLL phenotype. (A) Flow cytometric analysis of the pretumor hyperplasia phenotype as present in the peritoneal cavity in indicated genotypes. Six-month-old mice were killed, and peritoneal cavity washes were analyzed for the content of CD5+CD19+ B cells (percentage of total cells in a lymphocyte gate are given in the graphs). Results from 6-month-old mice are shown as representative examples. Genotypes are abbreviated as follows: wild-type mice, WT; PKCβ-deficient mice, PKC−/−; TCL1 transgenic mice, TCL1; and the TCL1 transgenic mice with deleted PKCβ alleles, PKC−/− TCL1. (B) Graphs showing the percentage of CD5/CD19 double-positive cells (analyzed as shown in panel A) as individually represented values per mouse analyzed (means are represented by the horizontal lines), according to genotype (PKC+/− TCL1 denotes TCL1 transgenic mice with loss of a single PKCβ allele). Data from the peritoneal cavity (PC) and spleen are shown. Statistical comparisons were performed using unpaired t test (P values shown in Table S2). (C) Mice of indicated genotypes were followed until the development of signs of illness (TCL1, n = 45; PKC+/− TCL1, n = 20; PKC−/− TCL1, n = 21). Analysis of the organs was performed, and development of CLL was scored as an event. Kaplan-Meier plots of CLL-free survival are shown. Difference between groups proved statistically significant by log-rank test (TCL1 vs PKC+/− TCL1, P = .034; TCL1 vs PKC−/− TCL1, P < 0.001; PKC+/− TCL1 vs PKC−/− TCL1, P = .009). WT controls and PKC−/− mice did not develop CLL until more than 500 days. (D) Cells (2 × 105/well) were cultured in uncoated wells or wells coated with 5 μg/mL anti-IgM F(ab′)2 fragments for 24 hours. Cell viability of anti-IgM–treated B cells compared with untreated controls is shown for the indicated genotypes. Error bars represent SEM. Groups were compared by unpaired t test: WT versus PKC−/−, P = .036; TCL1 versus PKC−/− TCL1. P = .042.
TCL1 reconstitutes the absent CD5+ B-cell population in PKCβ-deficient mice, but loss of PKCβ in TCL1 mice abrogates the CLL phenotype. (A) Flow cytometric analysis of the pretumor hyperplasia phenotype as present in the peritoneal cavity in indicated genotypes. Six-month-old mice were killed, and peritoneal cavity washes were analyzed for the content of CD5+CD19+ B cells (percentage of total cells in a lymphocyte gate are given in the graphs). Results from 6-month-old mice are shown as representative examples. Genotypes are abbreviated as follows: wild-type mice, WT; PKCβ-deficient mice, PKC−/−; TCL1 transgenic mice, TCL1; and the TCL1 transgenic mice with deleted PKCβ alleles, PKC−/− TCL1. (B) Graphs showing the percentage of CD5/CD19 double-positive cells (analyzed as shown in panel A) as individually represented values per mouse analyzed (means are represented by the horizontal lines), according to genotype (PKC+/− TCL1 denotes TCL1 transgenic mice with loss of a single PKCβ allele). Data from the peritoneal cavity (PC) and spleen are shown. Statistical comparisons were performed using unpaired t test (P values shown in Table S2). (C) Mice of indicated genotypes were followed until the development of signs of illness (TCL1, n = 45; PKC+/− TCL1, n = 20; PKC−/− TCL1, n = 21). Analysis of the organs was performed, and development of CLL was scored as an event. Kaplan-Meier plots of CLL-free survival are shown. Difference between groups proved statistically significant by log-rank test (TCL1 vs PKC+/− TCL1, P = .034; TCL1 vs PKC−/− TCL1, P < 0.001; PKC+/− TCL1 vs PKC−/− TCL1, P = .009). WT controls and PKC−/− mice did not develop CLL until more than 500 days. (D) Cells (2 × 105/well) were cultured in uncoated wells or wells coated with 5 μg/mL anti-IgM F(ab′)2 fragments for 24 hours. Cell viability of anti-IgM–treated B cells compared with untreated controls is shown for the indicated genotypes. Error bars represent SEM. Groups were compared by unpaired t test: WT versus PKC−/−, P = .036; TCL1 versus PKC−/− TCL1. P = .042.
Consequently, loss of even one allele of PKCβ delayed the onset of CLL, and loss of both completely abrogated CLL development (Figure 1C), suggesting that, although the PKCβ signal is not essential for the development of CD5+ nonmalignant B cells in TCL1 transgenic mice, the contribution of PKCβ to CLL transformation is indispensible. Abrams et al3 suggested that a PKCβ-dependent feedback mechanism on the BCR may be necessary to keep the BCR signal below a proapoptotic threshold. Thus, under conditions of loss of PKCβ, such an antigen-driven signal may be strong enough to delete potential autoantigen-driven CLL precursor cells before their transformation. In fact, when challenged by BCR crosslinking, B cells from PKC-deficient mice were significantly more sensitive to BCR-induced apoptosis, regardless of their TCL1 expression status (Figure 1D). In this light, the significant reduction of hyperplasia observed in pretumor TCL1 mice with loss of PKCβ signal may indicate that the accumulation of CD5+ B cells is driven by an autoantigenic interaction. However, tumors that did arise in TCL1 transgenic mice heterozygous for PKCβ were not dramatically different from their PKCβ wild-type counterparts (see Figure S2), suggesting that a transforming event may overcome this difference. The observation of a gene dosage effect (Figure 1C) is an encouraging aspect of our findings, because this suggests that a therapeutic benefit may be achieved by only partial inhibition of PKCβ, which is probably the case with pharmacologic inhibition.
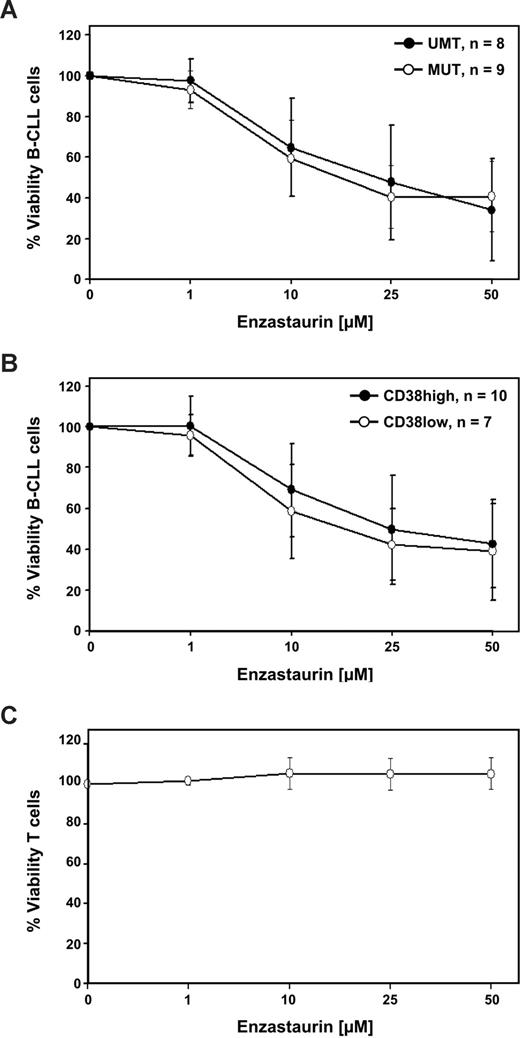
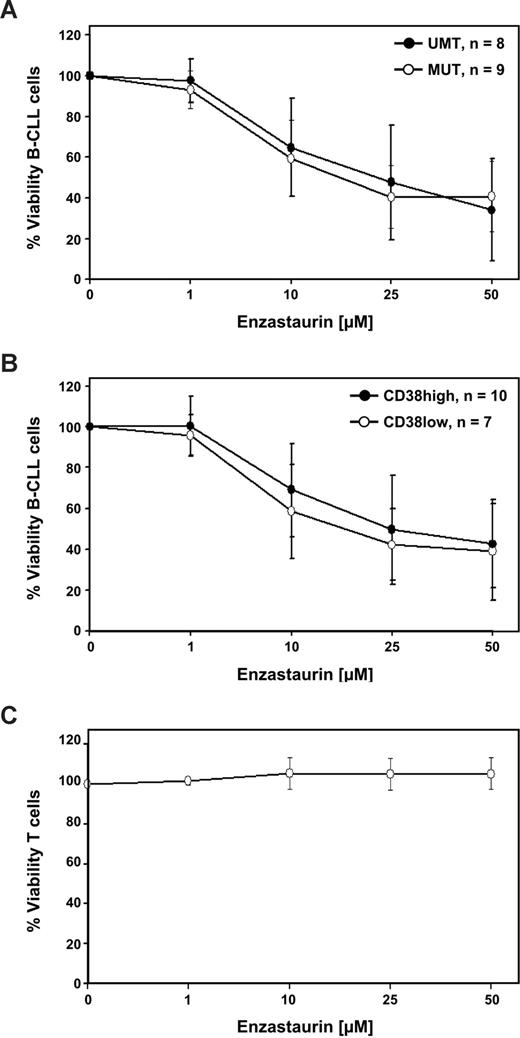
To take our observations to the human CLL disease level, we chose enzastaurin as an inhibitor of both PKCβ and AKT to synergistically target both these signaling arms downstream of the BCR. In 19 CLL samples tested (Table S1), we observed apoptosis induction on treatment with enzastaurin in vitro (Figure 2). This killing was also observed independent of risk factors analyzed (unmutated VH gene or high CD38 expression) or high-risk cytogenetics, such as del17p or del11q (data not shown). Although Abrams et al3 reported only marginal apoptosis induced by the PKCβ-specific inhibitor LY379196, targeting of both PKCβ and AKT as achieved by enzastaurin seemed efficient in CLL in this respect.17 In vivo, additional inhibitory effects of enzastaurin on VEGF signaling may further enhance its utility as a therapeutic agent.13 Phase 1 trials of enzastaurin in CLL have already been instituted.
The PKCβ inhibitor enzastaurin efficiently kills human CLL cells in vitro independent of risk factor mutation status or CD38. Human CLL cells were cultured in vitro, as described in Document S1. Indicated concentrations of enzastaurin were added, and the viable cell fraction was determined as the annexin V–negative population by flow cytometry, compared with controls. Results after 24 hours of treatment are shown. Table S1 shows the patient characteristics. (A) Data for 9 mutated (MUT) and 8 unmutated (UMT) CLL samples are shown as mean plus or minus SE. (B) Data for 10 CD38 high-risk and 7 CD38 low-risk patients are shown. (C) Survival of T cells from the same samples is shown as mean plus or minus SEM.
The PKCβ inhibitor enzastaurin efficiently kills human CLL cells in vitro independent of risk factor mutation status or CD38. Human CLL cells were cultured in vitro, as described in Document S1. Indicated concentrations of enzastaurin were added, and the viable cell fraction was determined as the annexin V–negative population by flow cytometry, compared with controls. Results after 24 hours of treatment are shown. Table S1 shows the patient characteristics. (A) Data for 9 mutated (MUT) and 8 unmutated (UMT) CLL samples are shown as mean plus or minus SE. (B) Data for 10 CD38 high-risk and 7 CD38 low-risk patients are shown. (C) Survival of T cells from the same samples is shown as mean plus or minus SEM.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported by the Austrian Science Fund (grants P19481 and L488) (A.E.), the Austrian National Bank (grant 10990) (A.E.), the state of Salzburg and the Spezialforschungsbereich 021 (R.G.), and by a research grant from Eli Lilly and Company (A.E.).
Authorship
Contribution: A.E. and R.G. designed the research; C. Holler, U.D., J.D.P., S.H., and C. Heyder performed the experimental work; A.E., C. Holler, and J.P. performed analysis; and A.E. and C. Holler wrote the paper. All authors were involved in critical discussion of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Alexander Egle, Laboratory for Immunological and Molecular Cancer Research, 3rd Medical Department for Hematology, Oncology, Hemostasiology, Infectious Diseases and Rheumatology, University Hospital Salzburg, Muellnerhauptstrasse 48, 5020 Salzburg, Austria; e-mail: a.egle@salk.at.