Abstract
As multiple myeloma tumors universally dysregulate cyclin D genes we conducted high-throughput chemical library screens for compounds that induce suppression of cyclin D2 promoter transcription. The top-ranked compound was a natural triterpenoid, pristimerin. Strikingly, the early transcriptional response of cells treated with pristimerin closely resembles cellular responses elicited by proteosome inhibitors, with rapid induction of heat shock proteins, activating transcription factor 3 (ATF3), and CHOP. Enzymatic assays and immunoblotting confirm that pristimerin rapidly (< 90 minutes) and specifically inhibits chymotrypsin-like proteosome activity at low concentrations (< 100 nM) and causes accumulation of cellular ubiquitinated proteins. Notably, cytotoxic triterpenoids including pristimerin inhibit NF-κB activation via inhibition of IKKα or IKKβ, whereas proteosome inhibitors instead suppress NF-κB function by impairing degradation of ubiquitinated IκB. By inhibiting both IKK and the proteosome, pristimerin causes overt suppression of constitutive NF-κB activity in myeloma cells that may mediate its suppression of cyclin D. Multiple myeloma is exquisitely sensitive to proteosome or NF-κB pathway inhibition. Consistent with this, pristimerin is potently and selectively lethal to primary myeloma cells (IC50 < 100 nM), inhibits xenografted plasmacytoma tumors in mice, and is synergistically cytotoxic with bortezomib—providing the rationale for pharmaceutical development of triterpenoid dual-function proteosome/NF-κB inhibitors as therapeutics for human multiple myeloma and related malignancies.
Introduction
Despite the genetic heterogeneity of cancer, tumors from unrelated individuals with seemingly unrelated mutations are often mechanistically unified by their ultimate dysregulation of similar core cellular checkpoints, such as the cyclin D-Cdk-pRb proliferation-commitment switch or p53 surveillance. In human multiple myeloma, ectopic expression of a single or 2 cyclin D gene(s), commonly CCND1 or CCND2, is a ubiquitous molecular finding that unifies at least 7 distinct primary genetic events that variously function to cis- or trans-activate cyclin D genomic loci.1 Thus, nearly half of all myeloma tumors possess 1 of 5 recurrent 14q32 (immunoglobulin enhancer) translocations—11q13 (CCND1), 6p21 (CCND3), 4p16 (FGFR3/MMSET), 16q23 (MAF), or 20q12 (MAFB)—that directly dysregulate CCND1 or CCND3, or that dysregulate either FGFR3/MMSET or maf transcription factors, which ultimately transactivate CCND.2 Other myeloma tumors are hyperdiploid with multiple trisomies, and, although these tumors generally lack recurrent 14q32 translocations, they too show overexpression of a cyclin D with biallelic transactivation of CCND1 or CCND2.1
To identify lead compounds for development as therapeutics that circumvent the heterogeneity of primary transforming mutations, we recently conducted high-throughput screening of chemical libraries for molecules that switch off cyclin D2 promoter activity in 3T3 cells.3,4 This approach has previously resulted in the identification of kinetin riboside, which induces rapid suppression of the cyclin D1 and D2 promoters via the recruitment of transcriptional repressors.4 Here, we describe the characterization of pristimerin, a naturally occurring triterpenoid and the top-ranked suppressor of cyclin D2 promoter transactivation identified from Spectrum (Microsource Discovery Systems, Gaylordsville, CT) library screening.
Triterpenoids are structurally diverse organic chemicals consisting of 6 isoprene units that are assembled in plants by cyclization of squalene, a structural precursor of steroids. The basic triterpenoid backbone can be modified in numerous ways and more than 20 000 varieties exist naturally. Several triterpenoids, including ursolic and oleanolic acid, betulinic acid, celastrol, lupeol, and the triterpenoids of ginsenosides, possess modest antitumorigenic or anti-inflammatory properties (reviewed in Salminen et al5 ). In addition, several synthetic triterpenoid derivatives have been developed to enhance antitumor potency, including 2-cyano-3,12-dioxooleana-1,9 (11)-dien-28-oic acid (CDDO), its methyl ester (CDDO-Me), and imidazolide (CDDO-Im), methyl (CDDO-MA), ethyl amides (CDDO-EA), and dintirile (Di-CDDO) derivatives. Of these CDDO, CDDO-Me (RTA 402), betulinic acid, and the ginsenosides have shown promising anticancer activities and are presently being evaluated in phase 1 clinical trials for leukemia, lymphoma, and solid tumors (for clinical trial details, see http://clinicaltrials.gov).
Triterpenoids such as CDDO are highly multifunctional although their effective concentrations for various cellular effects may be widely separated. Depending upon the dose administered, triterpenoids can induce anti-inflammatory, cytoprotective, tumor-differentiating, proliferation-arresting, and apoptotic effects.6-9 The anticancer activities of cytotoxic triterpenoids appear to be mediated, at least in part, by their common ability to block TNFα-induced NF-κB activation via inhibition of IKKα (CHUK) and/or IKKβ (IKBKβ).10-16 For example, the molecular targets of the synthetic oleanane triterpenoids include IKK and also pathways involving signal transducer and activator of transcription (STAT), IL-6, transforming growth factor beta (TGFβ), and KEAP1 (the inhibitor of the transcription factor, NRF2). Inhibition of multiple targets by triterpenoids is believed to be mediated by promiscuous reversible Michael addition of these compounds to exposed nucleophilic groups (such as accessible cysteine sulfides) of various susceptible signaling proteins.17 The effects of triterpenoids on multiple signaling pathways, and their clinical properties, including particularly those of CDDO and its derivatives have recently been the subject of review.18
Here we describe the potent anticancer activity of the natural triterpenoid, pristimerin, isolated from Celastrus and Maytenus spp. We find that pristimerin functions both to inhibit IKK phosphorylation of IκB, and as a potent novel proteosome inhibitor, causing an unfolded protein response in tumor cells and markedly suppressing NF-κB activity and cyclin D expression. As a consequence, pristimerin induces selective myeloma cell apoptosis in vitro and in vivo with greater potency than that described for other antineoplastic triterpenoids such as celastrol or CDDO, which are currently in clinical trials.
Methods
Cell culture and reagents
Human myeloma cell lines were grown in RPMI. Primary multiple myeloma and bone marrow cells were grown in IMDM. NIH3T3 cells were cultured in DMEM. Cultures were supplemented with 10% fetal bovine serum and 1 mM glutamate. Where indicated, cell lines were supplemented with IL-6, IGF-1, and BAFF (R&D Systems, Minneapolis, MN).
High-throughput screen for inhibitors of CCND2 transactivation
NIH3T3 CCND2-luc reporter cells were produced and screened as previously described for Prestwick (Prestwick Chemical, Illkirch, France) and Lopac (Sigma-Aldrich, St Louis, MO) libraries.3 Briefly, cells were dispensed into 96-well plates (13 000/well) with a Biomek FX liquid handler and following adherence were treated with compounds from the Spectrum (Microsource Discovery Systems) library at final concentration of approximately 5 μM with DMSO less than 0.1% at 37°C for 16 hours. After incubation, CCND2 activation was assessed by luciferase assay and viability was assessed by MTS assay.
Luciferase assay
Luciferase activity was assessed according to the substrate manufacturer's instructions (Promega, Madison, WI). Briefly, culture media were removed with an EMBLA plate washer (Molecular Devices, Sunnyvale, CA) and Glo Lysis buffer (Promega) was added by robot. After 10 minutes, an equal volume of Bright-Glo Luciferase substrate (Promega) was added and luminescence was detected with a Luminoskan plate reader (Thermo Scientific, Waltham, MA) using 5-second integration.
MTS and MTT viability assays
For screening, cell viability was assessed by 3-(4,5-dimethyl-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium (MTS) assay (Promega). MTS reagent 20 μL/well was added at 37°C for 4 hours and absorbance at 490 nm was determined. For follow-up studies, viability of human myeloma cell lines was determined by MTT assay (Sigma-Aldrich) following the manufacturer's instructions.
Pristimerin
Pristimerin (CAS no. 1258-84-0, ID no. 01504181), was purchased from MicroSource Discovery Systems, with verified minimum purity more than 95%. For in vitro assays, pristimerin was solubilized in DMSO at 20 mg/mL, aliquoted, and stored at −20°C. For early in vivo experiments, pristimerin was solubilized in a vehicle consisting of DMSO, ethanol, corn oil, and Tween and delivered by subcutaneous injection; for subsequent in vivo studies, pristimerin was delivered systemically in a liposomal format. To incorporate pristimerin into liposomes, the drug was first solubilized in t-butanol at 2 mg/mL at 37°C; in parallel, phospholipid reagent distearoyl phosphatidyl choline (DSPC) was solubilized in t-butanol at 10 mg/mL at 55°C. Pristimerin and DSPC solutions were then combined at a drug-lipid ratio (wt/wt) of 1:20 (1:4 vol/vol) and the resulting mix was immediately snap frozen in an ethanol–dry ice bath and freeze-dried overnight on a lyophilizer (vacuum, −40°C). The drug-DSPC was reconstituted as liposomes in normal saline at 55°C, washed, and recovered by centrifugation at 20 000g for 1 hour. Liposomes were resuspended at room temperature in saline (0.9% NaCl, 2 mM KCl) at a final concentration of pristimerin of 0.5 to 1 mg/mL. Specific incorporation of pristimerin into liposomes was determined by spectrophotometric assay (at peak absorbance, 415 nM) and was approximately 98.7%. A drug-free vehicle control liposome formulation was prepared in parallel using drug-free t-butanol in place of butanol-solubilized pristimerin. All liposome solutions were produced under sterile conditions and stored at 4°C; solutions were vortexed and filtered with 20-μm nylon mesh to remove multilamellar vesicles or aggregates prior to storage and again prior to use.
Immunoblotting
Cell-lysate preparation, gel electrophoresis, and immunoblotting were performed using standard techniques. PVDF membranes were probed with antibodies against cyclin D1 (DCS-6; BioSource, Camarillo, CA), cyclin D2 (no. 2924), cyclin D3 (DCS-22; BioSource), ubiquitin (no. 3936), phosphorylated IKKα(Ser180)/IKKβ(Ser181) (no. 2681S), IκB (no. 4814), or β-actin (no. 4967; all from Cell Signaling Technology, Beverly MA, except as specified). Proteins were visualized by chemiluminescence (Pierce, Rockford, IL).
Gene expression profiling for early pristimerin-responsive genes
H929 and U266 human myeloma cell lines were treated with pristimerin 500 nM (∼ 2 × IC50) or DMSO vehicle and harvested at 4 hours, prior to the appearance of any macroscopic evidence of perturbed viability. RNA was isolated using Trizol, column purified (QIAGEN, Valencia, CA), and hybridized to Hg_U133_plus_2 microarrays (Affymetrix, Santa Clara, CA) according to the manufacturer's instructions. The microarray data are available in the Gene Expression Omnibus (GEO) under accession number GSE14011.19 Probe set signal intensities were PLIER16-normalized using Affymetrix Expression Console software and flagged using Affymetrix Microarray Suite 5 (MAS5) Present/Absent/Marginal detection calls. Expression data were analyzed with GeneSpring 7 (Agilent Technologies, Santa Clara, CA) software, with drug-treated samples normalized per cell line to DMSO-treated controls. Gene lists were filtered to exclude nonexpressed probe sets with MAS5 “Absent” detection calls across all samples tested (treated and untreated). Probe sets up-regulated or suppressed by pristimerin in each cell line were delineated by volcano plot filter (> 1.5-fold change, FDR < 0.25) and the Venn intersection of probe sets modulated by drug in both cell lines was used in deriving a pristimerin signature.
Analysis for correlates of pristimerin gene expression signature in myeloma
To generate hypotheses surrounding the mode of activity of pristimerin in myeloma, a subset of 38 U133A legacy probe sets representing a pristimerin-response signature was derived from U133_plus_2 data. The signature included the 33 top-ranked pristimerin-induced probe sets with 1.75- to 100-fold increased signal in H929 and U266 cells and 5 down-regulated probe sets with 1.5- to 2-fold suppression in these cells. The signature was used to identify functional connections between pristimerin and previously characterized drugs by Connectivity Map (Cmap, Build 2; Broad Institute, http://www.broad.mit.edu/cmap) pattern-matching algorithms, referencing more than 6000 unique expression profiles representing 1309 compounds.
Chymotrypsin-like 20S proteosome assay
Purified human erythrocyte 20S proteosome (Biomol, Plymouth, PA) (∼ 0.1 μg/well) was combined with Suc-LLVY-AMC (Biomol; 75 μM), a fluorogenic substrate for chymotrypsin-like peptidase activity, and specified inhibitors, in 50 μL (final volume) buffer (50 mM Tris/HCl, pH 7.5, 25 mM KCl, 10 mM NaCl, 1 mM MgCl2) in an opaque white microtiter plate, as recommended by the manufacturer, and substrate degradation was monitored at 2-minute intervals using a fluorescence plate reader (excitation: 355 nm; emission: 460 nm). The rate of substrate cleavage, representing proteosomal chymotrypsin-like activity, was determined from the gradient of fluorescence versus time.
Primary bone marrow samples from myeloma patients
Bone marrow from multiple myeloma patients was obtained with Mayo Clinic institutional review board approval and in accordance with the Declaration of Helsinki. Samples were treated by ACK lysis to remove red cells and then treated as described in Figure 5.
Additional methods are described in Document S1 (available on the Blood website; see the Supplemental Materials link at the top of the online article).
Results
A high-throughput chemical library screen identifies a triterpenoid, pristimerin, as a potent upstream inhibitor of CCND2 transactivation
As poor prognosis myeloma variants commonly transactivate CCND2, we sought to discover novel pharmaceutical inhibitors of cellular pathways driving cyclin D2 promoter transactivation. To identify inhibitors that act upstream of CCND2, we used a high-throughput chemical genetics screen using NIH3T3 reporter cells stably overexpressing the CCND2 promoter driving firefly luciferase (luc) expression.4 In the 3T3 reporter system, basal cyclin D2 promoter activity was readily detectable and was further up-regulated by ectopic coexpression of c-maf.4 Maf is a CCND2 transactivating factor implicated in myelomagenesis.20
Using an automated assay, the CCND2 promoter reporter cells were aliquoted in 96-well plates and treated for 16 hours at 37°C with compounds at final concentration of approximately 5 μM and DMSO less than 0.1%. In control wells, cells were treated with buffer alone. To eliminate discovery of nonspecific broadly cytotoxic agents, which might suppress luciferase activity by killing 3T3 cells, an MTT viability assay was performed on compound-exposed cells in parallel with CCND2 reporter testing. More than 4000 compounds from Lopac, Prestwick, and Spectrum chemical libraries were screened.
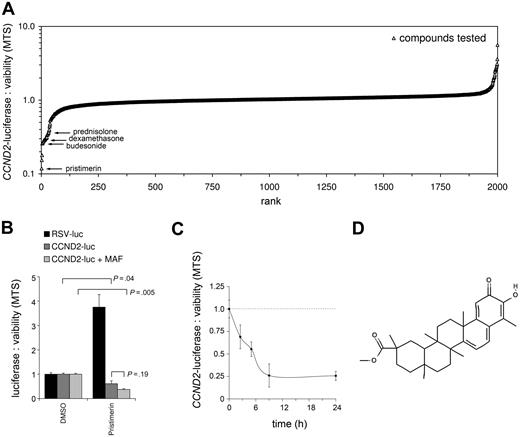
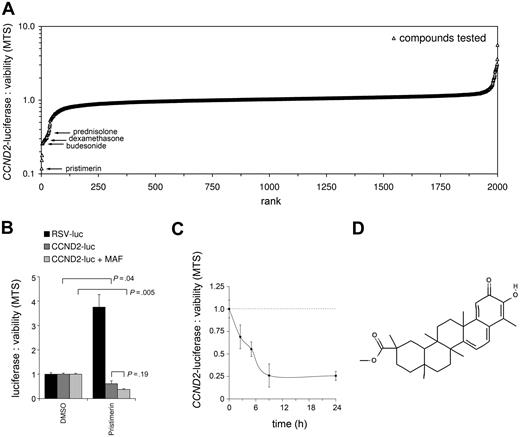
The majority of CCND2-supressing hits from the Lopac and Prestwick libraries were glucocorticoid family members.3 The mechanisms by which corticosteroids decrease cyclin D gene expression are described elsewhere.3 However, from screening the Spectrum library of drugs and natural compounds, the most potent inhibitor of CCND2 promoter activity identified was a natural triterpenoid, pristimerin. Strikingly, this triterpenoid induced a near 10-fold reduction in CCND2 promoter–driven luciferase activity, without inducing significant 3T3 cytotoxicity, outstripping the 3-fold suppression induced by conventional glucocorticoids in the same assay (Figure 1A). Although triterpenoids are related to glucocorticosteroids by their assembly in plants from a common precursor, squalene, these compounds differ substantively in final structure as triterpenoids are pentacyclic, whereas glucocorticoids are tetracyclic.
Identification of the triterpenoid, pristimerin, as an inhibitor of CCND2 transactivation. (A) Rank-ordered dot plot of the Spectrum library of 2000 drugs and natural compounds (x-axis) showing their specific effects on CCND2 promoter transactivation relative to NIH3T3 viability (as ratio of luciferase and MTT assays on vertical axis, normalized to vehicle controls with no effect). The activity of pristimerin, the top-ranked hit, and of glucocorticoids is indicated. Lopac and Prestwick drug libraries were previously screened3 but are not shown. (B) Histogram showing the effects of pristimerin on luciferase expression when transcribed from the CCND2 promoter or from a control RSV promoter. The activities of the various reporter cell lines are normalized to vehicle-treated controls. Pristimerin suppresses CCND2 transactivation both in the presence (P = .005) and absence (P = .04) of the MAF transactivator but does not suppress luciferase when expressed from a control RSV promoter. Error bars represent the sum of relative error in separate viability and luciferase measurements, determined from the standard deviation of triplicate assays. (C) Time course of pristimerin-induced suppression of CCND2 promoter expressed luciferase in NIH3T3; the luciferase protein has an estimated half-life of 3 hours. (D) Chemical structure of pristimerin.
Identification of the triterpenoid, pristimerin, as an inhibitor of CCND2 transactivation. (A) Rank-ordered dot plot of the Spectrum library of 2000 drugs and natural compounds (x-axis) showing their specific effects on CCND2 promoter transactivation relative to NIH3T3 viability (as ratio of luciferase and MTT assays on vertical axis, normalized to vehicle controls with no effect). The activity of pristimerin, the top-ranked hit, and of glucocorticoids is indicated. Lopac and Prestwick drug libraries were previously screened3 but are not shown. (B) Histogram showing the effects of pristimerin on luciferase expression when transcribed from the CCND2 promoter or from a control RSV promoter. The activities of the various reporter cell lines are normalized to vehicle-treated controls. Pristimerin suppresses CCND2 transactivation both in the presence (P = .005) and absence (P = .04) of the MAF transactivator but does not suppress luciferase when expressed from a control RSV promoter. Error bars represent the sum of relative error in separate viability and luciferase measurements, determined from the standard deviation of triplicate assays. (C) Time course of pristimerin-induced suppression of CCND2 promoter expressed luciferase in NIH3T3; the luciferase protein has an estimated half-life of 3 hours. (D) Chemical structure of pristimerin.
To assess whether pristimerin's activity was specific for the CCND2 promoter, or whether this reflected a more general effecton cellular transcription, or perhaps an off-target effect on luciferase enzyme activity, pristimerin was tested against 3T3 cells expressing luciferase from a control RSV promoter (Figure 1B). Pristimerin failed to suppress luciferase activity when this was expressed from an RSV promoter, and in fact caused a significant increase in RSV-expressed luciferase. Therefore suppression of CCND2-luciferase by pristimerin involves specific suppression of the CCND2 promoter.
We next sought to determine whether pristimerin suppresses CCND2 transactivation via a maf-dependent or maf-independent mechanism, by testing pristimerin against CCND2-luc reporter 3T3 cells both in the presence and absence of ectopic retrovirally expressed maf (Figure 1B). Untransformed 3T3 cells do not have detectable maf by immunoblotting (not shown). Pristimerin suppressed CCND2 promoter–expressed luciferase both in the absence or presence of maf, suggesting that pristimerin functions independently of the maf transcription factor to cause inhibition of CCND2 transactivation.
Suppression of cyclin D2 promoter transcription by pristimerin likely occurs with a short lag phase of less than 3 hours as, despite an estimated luciferase half-life of 3 hours, pristimerin caused a 75% reduction in CCND2 promoter–expressed luciferase within 9 hours (Figure 1C). The chemical structure of pristimerin is shown in Figure 1D.
Pristimerin is potently cytotoxic to human myeloma cell lines and induces suppression of cyclins D1, D2, and D3
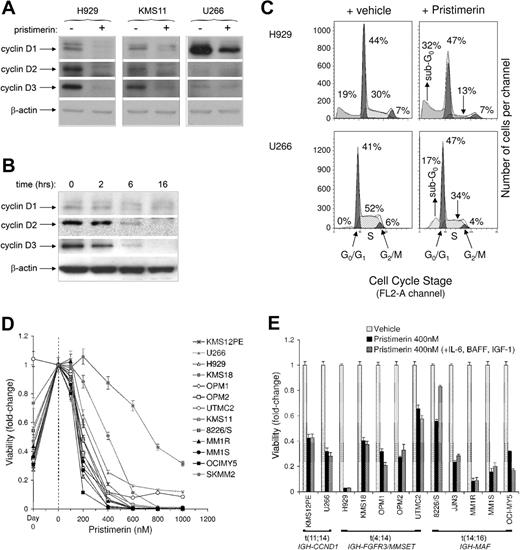
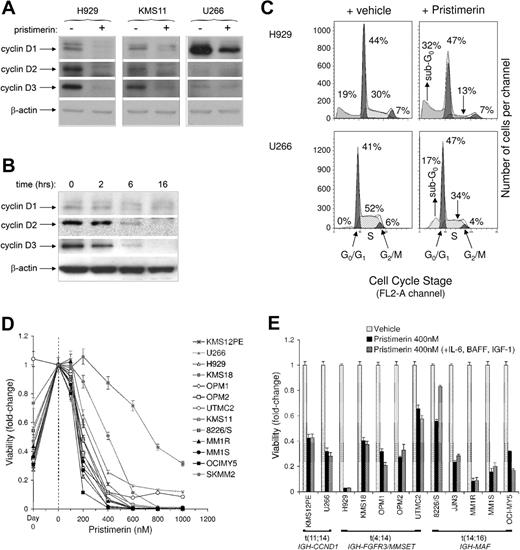
The effects of pristimerin on cyclin D protein expression were next assessed in malignant human cells. Three multiple myeloma cell lines that overexpresses cyclin D1 and/or D2, as a result of primary t(4;14), t(14;16), or t(11;14) translocations, were treated with pristimerin 500 nM and cyclin D levels were assessed by immunoblotting. As shown in Figure 2A, pristimerin caused substantial suppression of all 3 human cyclin Ds (D1, D2, and D3) in each of the myeloma lines at 14 hours.
Effects of pristimerin on cyclin D1, D2, and D3 protein expression, cell-cycle progression, and viability of human myeloma cell lines. (A) Immunoblot showing suppression of cyclins D1, D2, and D3 by pristimerin (500 nM) at 14 hours in H929, KMS11, and U266 human myeloma cells. Pristimerin effects are compared with DMSO vehicle. (B) Temporal course of cyclin D1, D2, and D3 suppression in H929 following pristimerin (500 nM) exposure, showing significant suppression by 6 hours, increasing to 16 hours. (C) Cell-cycle profiles of H929 and U266 cells grown in standard media and treated with vehicle or pristimerin (500 nM) at 16 hours. Major left and right peaks represent G0/G1 and G2/M phases, respectively. Pristimerin causes expansion of a sub-G0 fraction, corresponding to apoptotic cells. Similar results were obtained with duplicate experiments. (D) Inhibition of heterogeneous myeloma cell lines by titrated pristimerin, assessed by MTT assay at 72 hours. Results at each concentration represent the mean of triplicate wells ± SEM. At the left of the dashed line, the background proliferative activity of each cell line is presented, with MTT results shown for cells at day 0 and for untreated cells at assay completion (0 nM). The median IC50 of pristimerin against myeloma cell lines is approximately 200 nM. (E) Myeloma growth cytokines IL-6 (10 ng/mL), IGF-1 (100 ng/mL), and Baff (25 ng/mL) fail to rescue cells from pristimerin. Viability was assessed by MTT assay at 72 hours. Error bars represent the standard deviation of triplicate assay results.
Effects of pristimerin on cyclin D1, D2, and D3 protein expression, cell-cycle progression, and viability of human myeloma cell lines. (A) Immunoblot showing suppression of cyclins D1, D2, and D3 by pristimerin (500 nM) at 14 hours in H929, KMS11, and U266 human myeloma cells. Pristimerin effects are compared with DMSO vehicle. (B) Temporal course of cyclin D1, D2, and D3 suppression in H929 following pristimerin (500 nM) exposure, showing significant suppression by 6 hours, increasing to 16 hours. (C) Cell-cycle profiles of H929 and U266 cells grown in standard media and treated with vehicle or pristimerin (500 nM) at 16 hours. Major left and right peaks represent G0/G1 and G2/M phases, respectively. Pristimerin causes expansion of a sub-G0 fraction, corresponding to apoptotic cells. Similar results were obtained with duplicate experiments. (D) Inhibition of heterogeneous myeloma cell lines by titrated pristimerin, assessed by MTT assay at 72 hours. Results at each concentration represent the mean of triplicate wells ± SEM. At the left of the dashed line, the background proliferative activity of each cell line is presented, with MTT results shown for cells at day 0 and for untreated cells at assay completion (0 nM). The median IC50 of pristimerin against myeloma cell lines is approximately 200 nM. (E) Myeloma growth cytokines IL-6 (10 ng/mL), IGF-1 (100 ng/mL), and Baff (25 ng/mL) fail to rescue cells from pristimerin. Viability was assessed by MTT assay at 72 hours. Error bars represent the standard deviation of triplicate assay results.
The temporal course of cyclin D suppression was determined in H929 myeloma cells (Figure 2B). Although pristimerin caused suppression of all cyclin D proteins within 6 hours, no overt suppression of cyclins D1, D2, or D3 was evident at 2 hours. As the half-life of cyclin D proteins is short (approximately30-50 minutes, according to cell-cycle stage21 ), cyclin D suppression by pristimerin in myeloma cells likely starts more than 2 hours, and possibly as many as 4 to 5 hours, after exposure, suggesting that rather than acting directly on cyclin D genes, pristimerin's immediate molecular target(s) may be upstream of the D cyclins.
In H929 cells, pristimerin caused marked suppression of all 3 D cyclins (Figure 2A) that was associated with a marked reduction in cells entering S-phase and an early increase in sub-G0/G1 apoptotic cells (Figure 2C); by contrast, in U266 cells, which substantially overexpress cyclin D1, pristimerin caused only partial suppression of cyclin D1 (Figure 2A), associated with only a modest decline in cell-cycle progression (Figure 2C). However, like H929 cells, pristimerin-treated U266 cells showed an early increase in sub-G0/G1 apoptotic cells. Thus induction of apoptosis by pristimerin is unlikely to be caused directly by cyclin D suppression, and pristimerin's definitive molecular target again appears to be upstream of the D cyclin genes
Significantly, pristimerin is potently cytotoxic to myeloma tumor lines with median IC50 of approximately 200 nM (Figure 2D). Although other triterpenoids, such as CDDO or betulinic acid, also induce tumor cell apoptosis, and parallel cyclin D suppression, their potency compares poorly with that of pristimerin (for example, the EC50 of CDDO22 or betulinic acid23 for breast cancer cells is approximately 3-5 μM). Although cytokines such as IL-6, IGF-1, and tumor necrosis factor ligand superfamily member 13b (BAFF) can induce myeloma proliferation and protect myeloma cells from some chemotherapies,24,25 a concentrated cocktail of these cytokines fails to rescue myeloma cells from pristimerin-induced apoptosis (Figure 2E).
Pristimerin directly inhibits proteosome chymotrypsin-like activity
As pristimerin is rapidly and potently cytotoxic to myeloma cells, and as there is a 2- to 5-hour delay between pristimerin exposure and cyclin D2 promoter suppression (Figures 2B, 1C), we speculated that pristimerin targets a cellular pathway upstream of CCND2 to secondarily affect cyclin D expression and that altered expression of other cellular genes may occur before or in parallel with cyclin D suppression. We therefore performed array-based gene expression profiling studies to identify coregulated pristimerin-response genes and to deduce the compound's direct molecular target(s). Human myeloma H929 and U266 cells were exposed to pristimerin 500 nM (∼ 2-3 × IC50) or vehicle for 4 hours, and pristimerin-specific changes in gene expression were identified.
Surprisingly, from genome-wide gene expression studies, only 47 genes showed early responsiveness to pristimerin, in both H929 and U266 cells (Table 1), even when array profiles were interrogated for relatively modest (> 1.5-fold) changes in gene expression. However, pristimerin-responsive genes were remarkably enriched for endoplasmic reticulum (ER) stress and heat-shock proteins (which were strongly induced), as well as for ubiquitin life cycle enzymes, specific transcription factors, and regulators of apoptosis (Table 1 and “Discussion”).
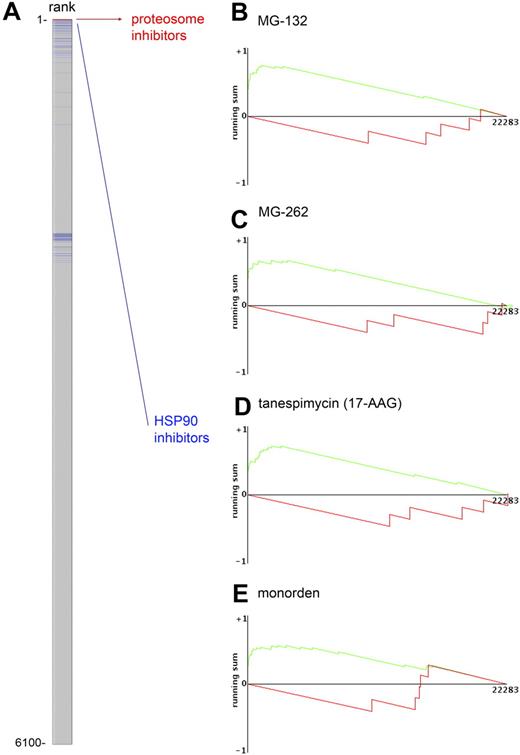
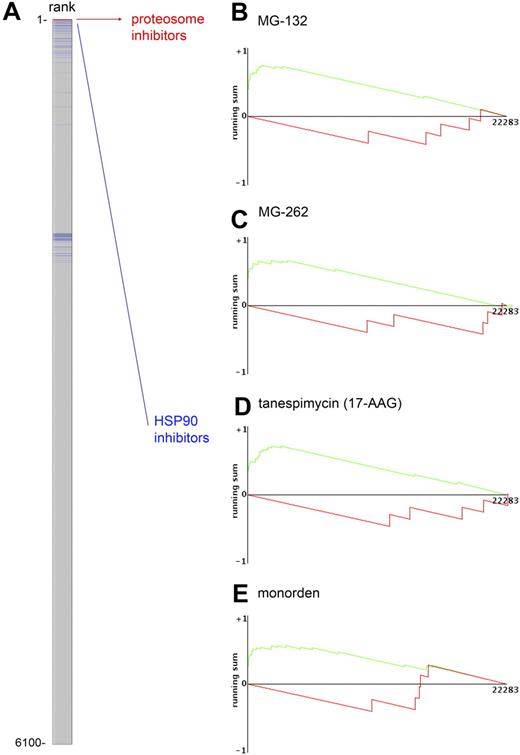
To generate hypotheses surrounding the direct mode of activity of pristimerin, a pristimerin-response signature (“Analysis for correlates of pristimerin gene expression signature in myeloma” in “Methods”), including the 33 top-ranked pristimerin-induced probe sets and the 5 maximally down-regulated probe sets, was next used to identify similarities between cellular responses to pristimerin and to other previously characterized drugs, using pattern-matching algorithms available at the Connectivity Map (Cmap, Build 2; http://www.broad.mit.edu/cmap), referencing more than 6000 unique expression profiles from 1309 compounds (Figure 3A). Significantly, 4 of the top 8 expression profiles most closely matching that of pristimerin versus myeloma cells belonged to proteosome inhibitors MG-132 (Figure 3B) and MG-262 (Figure 3C). These 4 expression profiles each ranked above the 99.8 percentile for pristimerin-signature resemblance and represent all instances of MG-132 and MG-262 in the database, demonstrating a highly significant nonrandom ranking of these profiles for similarity with the pristimerin profile. Notably, heat shock protein 90 (HSP90) inhibitors tanespimycin (17-AAG; Figure 3D), monorden (Figure 3E), and geldanamycin also ranked highly for similarity to pristimerin, but only with some database instances, as these drugs were also represented by multiple database entries in which genes suppressed by pristimerin showed no enrichment in their signature, perhaps due to the dose, timing, or cell line from which some HSP90 expression profile instances were generated.
The early cellular genetic response to pristimerin closely resembles genomic responses to proteosome and HSP90 inhibitors. (A) Genome-wide expression data from cell lines treated with vehicle or pristimerin 500 nM for 4 hours were used to generate a pristimerin early response gene signature that was then analyzed using Cmap (Build 2) to identify similarities between the pristimerin-induced biologic response and that of other drugs. More than 6000 unique expression profiles from 1309 compounds (some with multiple instances representing distinct cell lines or time points) were compared and rank-ordered for similarity to pristimerin's signature. The gray column represents the dataset of 6000 expression profiles. Four of the top-ranked profiles (red bars at the top of column), resembling the pristimerin signature, were from proteosome inhibitors, MG-132 (1/1 instance) and MG-262 (all 3/3 instances in dataset). Some gene response profiles from HSP90 inhibitors (blue bars: one per database instance) also closely resembled that of pristimerin, although other HSP90 profile instances were less closely matched, possibly reflecting the duration of drug exposure or cell line tested. (B-E) To the right are graphic representations of the connectivity scores for the gene expression signature of pristimerin and proteosome inhibitors (B) MG-132 or (C) MG-262, or Hsp90 inhibitors (D) tanespimycin (17-AAG) and (E) monorden, showing marked enrichment of the pristimerin signature in expression responses for these drugs. Interpretation of the plots and connectivity score is described at http://www.broad.mit.edu/cmap.
The early cellular genetic response to pristimerin closely resembles genomic responses to proteosome and HSP90 inhibitors. (A) Genome-wide expression data from cell lines treated with vehicle or pristimerin 500 nM for 4 hours were used to generate a pristimerin early response gene signature that was then analyzed using Cmap (Build 2) to identify similarities between the pristimerin-induced biologic response and that of other drugs. More than 6000 unique expression profiles from 1309 compounds (some with multiple instances representing distinct cell lines or time points) were compared and rank-ordered for similarity to pristimerin's signature. The gray column represents the dataset of 6000 expression profiles. Four of the top-ranked profiles (red bars at the top of column), resembling the pristimerin signature, were from proteosome inhibitors, MG-132 (1/1 instance) and MG-262 (all 3/3 instances in dataset). Some gene response profiles from HSP90 inhibitors (blue bars: one per database instance) also closely resembled that of pristimerin, although other HSP90 profile instances were less closely matched, possibly reflecting the duration of drug exposure or cell line tested. (B-E) To the right are graphic representations of the connectivity scores for the gene expression signature of pristimerin and proteosome inhibitors (B) MG-132 or (C) MG-262, or Hsp90 inhibitors (D) tanespimycin (17-AAG) and (E) monorden, showing marked enrichment of the pristimerin signature in expression responses for these drugs. Interpretation of the plots and connectivity score is described at http://www.broad.mit.edu/cmap.
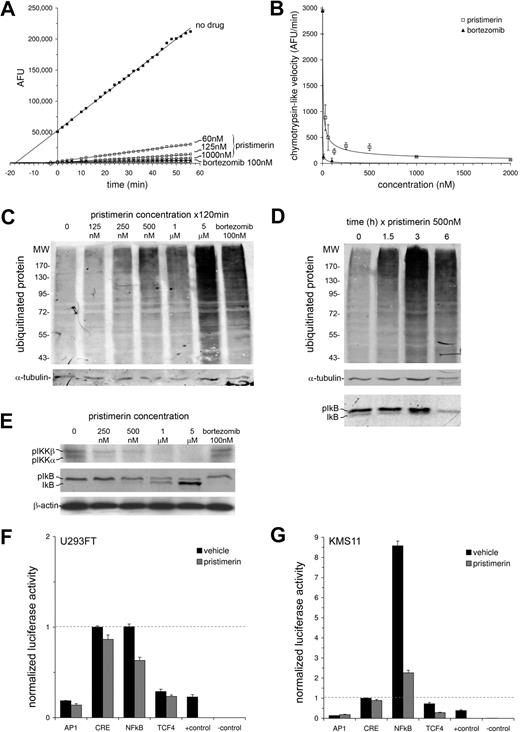
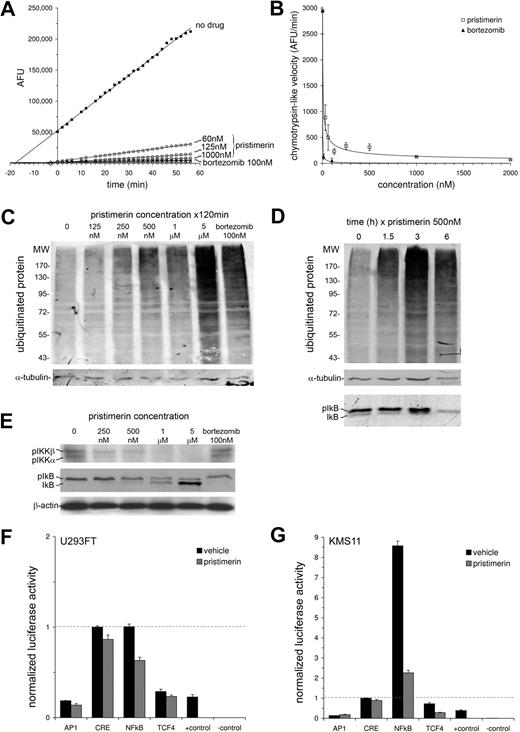
The close similarity in cellular responses to pristimerin and to proteosome inhibitors MG-132 and MG-262 suggested the hypothesis that pristimerin might function to inhibit proteosome activity. Therefore, we comprehensively tested this possibility by assaying the direct effect of pristimerin on the enzymatic function of cell-free purified human 20S proteosome (Figure 4A,B) and the effect of pristimerin on cell-based proteosome function—for the later studies, we examined pristimerin-treated cells for both proteosome enzymatic activity (Figure S1) and for accumulation of ubiquitinated cellular protein (Figure 4C,D; Figure S2). Significantly, pristimerin induced potent and rapid (Figure 4A,B; Figure S1) inhibition of proteosome chymotrypsin-like activity, by enzymatic assay, and this was paralleled in cell-based assays by rapid accumulation of high-molecular-weight ubiquitinated proteins at low drug concentrations (Figure 4C,D; Figure S2). Although chymotrypsin-like activity was potently inhibited, testing of proteosome caspase-like and trypsin-like activities suggested these were only weakly inhibited (EC50 > 5 μM, Figure S1). Therefore pristimerin functions, at least in part, as a novel selective inhibitor of proteosome chymotrypsin-like activity, with EC50 less than 125 nM, latency less than 90 minutes, and sustained effect lasting beyond 3 to 6 hours.
Pristimerin inhibits the proteosome and NF-κB activity. (A,B) The direct effect of pristimerin on the chymotrypsin-like peptidase activity of purified human 20S proteosome enzyme was assayed using a fluorogenic peptide substrate, suc-LLVY-AMC, and compared with proteosome chymotrypsin-like activity in the absence of drug or in the presence of bortezomib. (A) Time course of 20S proteosome cleavage of Suc-LLVY-AMC, in the presence (□) or absence (■) of drug, at specified concentrations, monitored by release of free AMC fluorophore (measured in arbitrary fluorescence units, AFU) at 2-minute intervals. Each square represents the mean result from duplicate wells. Linear accumulation of AMC was observed during the first hour. (B) Purified 20S proteosome chymotrypsin-like activity, calculated as the velocity of AMC release (in units of AFU/min), and dose-response curve for pristimerin (□) demonstrating an IC50 for inhibition of chymotrypsin-like activity below 30 to 60 nM. Data represent the mean velocity ± SEM per concentration. (C,D) To assess the effect of pristimerin on intracellular proteosome and NF-κB function, H929 myeloma cells were treated with pristimerin for 2 hours at various concentrations (C), or with pristimerin 500 nM for various durations (D). Lysates (10 μg per lane) were immunoblotted for ubiquitinated protein (top panel), α-tubulin (loading control: middle panel) or for IκB (D bottom panel); pristimerin causes accumulation of ubiquitinated high-molecular-weight protein, consistent with proteosome inhibition, and parallel suppression of phosphorylated IκB, consistent with inhibition of IKK. (E) To confirm parallel inhibition of IKK by pristimerin, H929 myeloma cells were treated as specified for 3 hours and assessed by immunoblot for inhibition of phosphoactivation of IKKα and IKKβ (using a S180/S181 phosphorylation-specific antibody) and for downstream phosphorylation of IκB. (F,G) Trans-activating activities of NF-κB, AP-1, TCF4, or CRE transcription factors in (F) U293FT kidney cells and (G) KMS11 myeloma cells, after exposure to pristimerin 500 nM or DMSO vehicle for 6 hours. Cells were transfected with transcription factor–specific luciferase reporter plasmids 30 hours prior to drug treatment. Relative to the other transcription factors, NF-κB trans-activating activity was greater in KMS11 myeloma cells than in 293 cells, consistent with biallelic loss of the NF-κB–negative regulator TRAF3 in KMS11.26 Allowing for a luciferase half-life of approximately 3 hours, NF-κB activity was profoundly suppressed in KMS11 by pristimerin (4-fold suppression of luciferase is observed in 2 half-lives). Positive and negative controls for luciferase detection were 2 irrelevant lysates containing, or lacking, luciferase. Data are represented as the mean of duplicate samples ± range.
Pristimerin inhibits the proteosome and NF-κB activity. (A,B) The direct effect of pristimerin on the chymotrypsin-like peptidase activity of purified human 20S proteosome enzyme was assayed using a fluorogenic peptide substrate, suc-LLVY-AMC, and compared with proteosome chymotrypsin-like activity in the absence of drug or in the presence of bortezomib. (A) Time course of 20S proteosome cleavage of Suc-LLVY-AMC, in the presence (□) or absence (■) of drug, at specified concentrations, monitored by release of free AMC fluorophore (measured in arbitrary fluorescence units, AFU) at 2-minute intervals. Each square represents the mean result from duplicate wells. Linear accumulation of AMC was observed during the first hour. (B) Purified 20S proteosome chymotrypsin-like activity, calculated as the velocity of AMC release (in units of AFU/min), and dose-response curve for pristimerin (□) demonstrating an IC50 for inhibition of chymotrypsin-like activity below 30 to 60 nM. Data represent the mean velocity ± SEM per concentration. (C,D) To assess the effect of pristimerin on intracellular proteosome and NF-κB function, H929 myeloma cells were treated with pristimerin for 2 hours at various concentrations (C), or with pristimerin 500 nM for various durations (D). Lysates (10 μg per lane) were immunoblotted for ubiquitinated protein (top panel), α-tubulin (loading control: middle panel) or for IκB (D bottom panel); pristimerin causes accumulation of ubiquitinated high-molecular-weight protein, consistent with proteosome inhibition, and parallel suppression of phosphorylated IκB, consistent with inhibition of IKK. (E) To confirm parallel inhibition of IKK by pristimerin, H929 myeloma cells were treated as specified for 3 hours and assessed by immunoblot for inhibition of phosphoactivation of IKKα and IKKβ (using a S180/S181 phosphorylation-specific antibody) and for downstream phosphorylation of IκB. (F,G) Trans-activating activities of NF-κB, AP-1, TCF4, or CRE transcription factors in (F) U293FT kidney cells and (G) KMS11 myeloma cells, after exposure to pristimerin 500 nM or DMSO vehicle for 6 hours. Cells were transfected with transcription factor–specific luciferase reporter plasmids 30 hours prior to drug treatment. Relative to the other transcription factors, NF-κB trans-activating activity was greater in KMS11 myeloma cells than in 293 cells, consistent with biallelic loss of the NF-κB–negative regulator TRAF3 in KMS11.26 Allowing for a luciferase half-life of approximately 3 hours, NF-κB activity was profoundly suppressed in KMS11 by pristimerin (4-fold suppression of luciferase is observed in 2 half-lives). Positive and negative controls for luciferase detection were 2 irrelevant lysates containing, or lacking, luciferase. Data are represented as the mean of duplicate samples ± range.
Pristimerin suppresses NF-κB transcription factor activity via proteosome-dependent and -independent mechanisms
Other triterpenoids, including CDDO-Me/Im, betulinic acid, and celastrol and ursolic acid, have been reported to possess anticancer activity and notably these triterpenoids all function, at least in part, by blocking TNFα-induced relocation of NF-κB1 p65 to the nucleus via inhibition of IKKβ and or IKKα.11,12,27-30 Inhibition of IKK activity by triterpenoids such as CDDO suppresses IKK phosphorylation of IκB, causing sustained complexing of IκB with NF-κB1 and blocking NF-κB1 nuclear activity. In contrast, proteosome inhibitors such as bortezomib or MG-132 also suppress NF-κB activity, however unlike triterpenoids, proteosome inhibitors oppress NF-κB by instead impairing the degradation of ubiquitinated IκB, which is normally rapidly inactivated (reviewed in Nakanishi and Toi31 ).
We speculated therefore that pristimerin, as both a triterpenoid and a proteosome inhibitor, might potently inhibit NF-κB signaling via one or both mechanisms, contributing to its cytotoxicity and suppression of cyclin D genes in myeloma. Importantly, NF-κB pathway up-regulation is highly prevalent in multiple myeloma, and myeloma tumors that activate NF-κB appear addicted to it for sustained tumor cell viability.26,32-34 We next assessed whether pristimerin, like other triterpenoids, influences IKK activity to suppress phosphorylation of IκB. As shown in Figure 4D and E and Figure S2A, pristimerin (but not bortezomib) suppresses phosphoactivation of IKKα and IKKβ, and inhibits downstream phosphorylation of IκB, in myeloma cells, mirroring similar results described for other triterpenoids.11,12,27-30 Inhibition of IKKα phosphorylation by pristimerin likely causes suppression of both canonical and noncanonical NF-κB pathways, in which IKKα is involved.
As pristimerin suppresses both proteosome function and IKK activity, and as both are positive regulators of NF-κB transcriptional activity, we next assessed the net effects of pristimerin on NF-κB–induced gene expression, the ultimate arbiter of NF-κB pathway influence. NF-κB transactivating activity was monitored using a luciferase reporter with luciferase expression driven by an artificial promoter containing 5× repeats of consensus NF-κB transcription factor binding site (TFBS) motifs (Figure 4F,G). Relative to the baseline activities of comparable control CRE-, AP1-, or TCF4-specific transcriptional reporters, constitutive NF-κB transcriptional activity is nearly 10-fold higher in myeloma KMS11 cells (Figure 4G) than in human kidney 293 cells (Figure 4F). Notably, KMS11 cells possesses a biallelic deletion of TRAF3, causing constitutive activation of NF-κB, as also occurs in myeloma patients.26,33 Whereas luciferase expressed by low-level NF-κB activity in 293 cells was partially suppressed (∼ 35%) by pristimerin (and was specifically suppressed compared with control CRE, AP1, or TCF4 promoters), luciferase expressed by constitutively active NF-κB in KMS11 cells was substantially suppressed (∼ 4-fold) by pristimerin exposure. Allowing for the luciferase half-life (t1/2) of 3 hours, and an assay duration of 6 hours (2 × t1/2), pristimerin must rapidly induce near 100% suppression of NF-κB promoter activity in KMS11 cells and cause an early 50% decline in basal NF-κB transcriptional activity in 293 cells. In contrast, CRE- and AP-1–specific promoters showed minimal loss of transactivation, verifying that pristimerin induces specific inhibition of NF-κB signaling.
Pristimerin induces selective apoptosis of primary multiple myeloma cells in mixed-lineage bone marrow culture
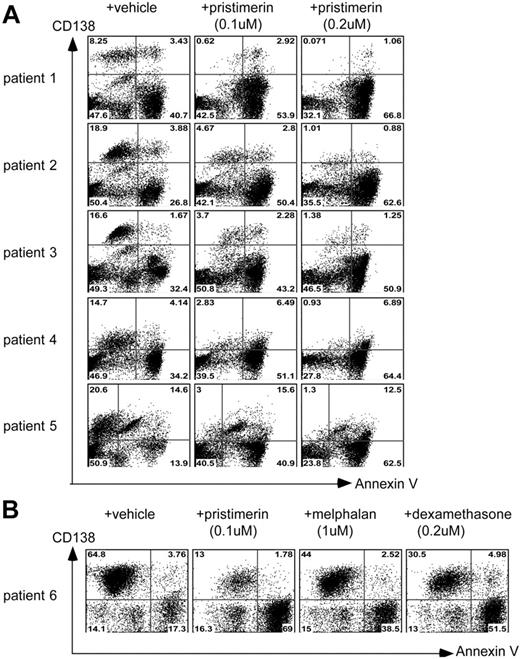
Clinical myeloma is uniquely sensitive to proteosome inhibition, as evidenced by the success of bortezomib; and myeloma cells appear equally sensitive to drugs that directly inhibit NF-κB.33 Therefore we further evaluated the antimyeloma activity of pristimerin, a combined proteosome/NF-κB inhibitor, by assessing its effects on primary bone marrow samples obtained from myeloma patients. Bone marrow samples were first processed to remove nonnucleated red cells and were then treated with pristimerin 100 nM or 200 nM for 72 hours. Importantly, pristimerin preferentially killed primary CD138+ myeloma tumor cells and was substantially less cytotoxic to nonmalignant bone marrow progenitor cells (Figure 5A; Figure S3). Conspicuously, the IC50 of pristimerin for primary myeloma cells (< 100 nM) was even lower than its IC50 for immortalized myeloma cell lines.
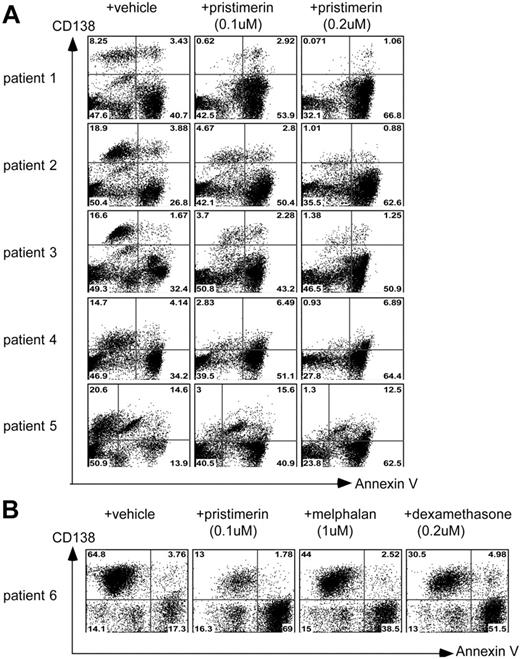
Pristimerin is selectively cytotoxic to primary myeloma cells in mixed-lineage bone marrow cultures from myeloma patients. Flow cytometric analyses of primary bone marrow samples, obtained from multiple myeloma patients, for viability or apoptosis (annexin V binding, horizontal axis) of CD138+ (myeloma) and CD138− (hematopoietic progenitor) fractions (vertical axis), after in vitro drug exposure and culture. (A) Examples of 5 myeloma patient bone marrow samples, each treated separately with either vehicle (left column), pristimerin 100 nM (middle), or pristimerin 200 nM (right column) for 72 hours, showing preferential killing of CD138+ tumor cells by pristimerin. Pristimerin induces preferential loss of viable primary tumor cells (top left quadrants, CD138+, annexin V−) and accumulation of CD138− annexin V+ cells (bottom right quadrants). Following induction of apoptosis, myeloma cells shed surface CD138 to become annexin V+, CD138−,35 and are detected in the right bottom quadrant. (B) Response of primary bone marrow cells from a patient with advanced myeloma to pristimerin 100 nM, dexamethasone 200 nM, or melphalan 1 μM, demonstrating potent selective antimyeloma in vitro efficacy of pristimerin compared with standard antimyeloma agents.
Pristimerin is selectively cytotoxic to primary myeloma cells in mixed-lineage bone marrow cultures from myeloma patients. Flow cytometric analyses of primary bone marrow samples, obtained from multiple myeloma patients, for viability or apoptosis (annexin V binding, horizontal axis) of CD138+ (myeloma) and CD138− (hematopoietic progenitor) fractions (vertical axis), after in vitro drug exposure and culture. (A) Examples of 5 myeloma patient bone marrow samples, each treated separately with either vehicle (left column), pristimerin 100 nM (middle), or pristimerin 200 nM (right column) for 72 hours, showing preferential killing of CD138+ tumor cells by pristimerin. Pristimerin induces preferential loss of viable primary tumor cells (top left quadrants, CD138+, annexin V−) and accumulation of CD138− annexin V+ cells (bottom right quadrants). Following induction of apoptosis, myeloma cells shed surface CD138 to become annexin V+, CD138−,35 and are detected in the right bottom quadrant. (B) Response of primary bone marrow cells from a patient with advanced myeloma to pristimerin 100 nM, dexamethasone 200 nM, or melphalan 1 μM, demonstrating potent selective antimyeloma in vitro efficacy of pristimerin compared with standard antimyeloma agents.
Myeloma cells exposed to pristimerin undergo apoptosis rather than other forms of cell death, as cell lines (not shown) and primary human myeloma cells rapidly acquire annexin V binding potential, shed surface CD138 (Figure 5A), and lose DNA content (Figure 2C) following triterpenoid exposure. Shedding of surface CD138 during plasma cell apoptosis is well established35 and occurs in parallel with membrane changes that promote annexin V binding.4
Evocatively, primary bone marrow myeloma cells from a patient with advanced myeloma, known to be clinically resistant to melphalan, bortezomib, thalidomide, and dexamethasone, showed a marked cytotoxic response to pristimerin (100 nM; Figure 5B) but were less responsive to dexamethasone (200 nM) or melphalan (1 μM), suggesting that simultaneous targeting of both proteosome and NF-κB vulnerabilities of myeloma cells may enable this multifunctional triterpenoid to overcome resistance to conventional antimyeloma therapeutics.
Pristimerin inhibits growth of human myeloma xenograft tumors in nude mice
Pristimerin was next evaluated for antitumor activity in vivo using plasmacytoma grown from xenografted human myeloma cells in immune-deficient mice. In an initial experiment, drug or vehicle was delivered subcutaneously in a depot lipid-detergent formulation and doses of up to 2.5 mg/kg per day were tolerated in the short term. However, despite promising evidence of antitumor effect (Figure 6A,B), mice treated with subcutaneous depot pristimerin developed delayed injection site necrosis that required cessation of therapy and euthanasia.
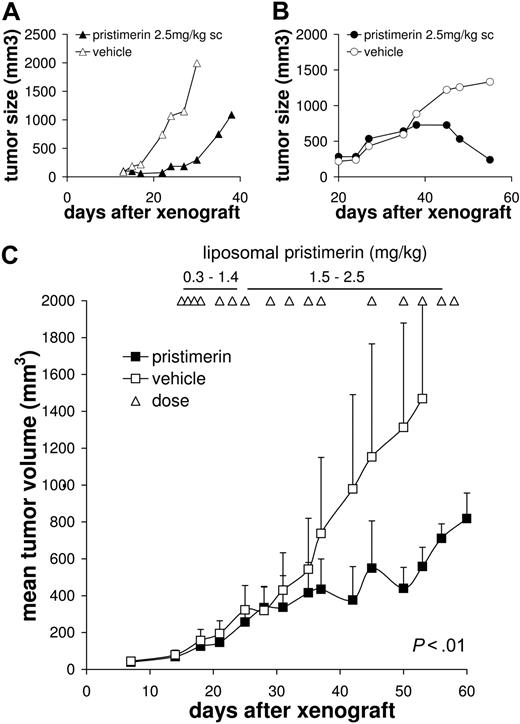
Tumoricidal activity of pristimerin versus human myeloma xenografts in mice. Human myeloma cells from RPMI-8226 or OCI-MY5 cultures were implanted subcutaneously in the right flank of beige nude (BNX) mice in 50% (vol/vol) Matrigel matrix and tumors were allowed to establish over approximately 2 weeks. In initial testing, single paired mice with (A) 8226 or (B) MY5 xenografts were treated with daily subcutaneous pristimerin 2.5 mg/kg per day in a depot formulation, or with vehicle, and tumor size was monitored. Although an antitumor effect appeared likely, mice treated with subcutaneous pristimerin developed delayed injection site necrosis, requiring cessation of therapy and euthanasia. (C) Repeat efficacy studies, using xenografted BNX mice (n = 4/group) treated with systemic liposomal pristimerin or vehicle, delivered via tail vein injection, at doses escalating from 0.25 mg/kg per dose to 2.5 mg/kg per dose, administered 2 to 3 times weekly, commenced after mean tumor volumes exceeded 70 mm.3 P value was calculated by paired t test. No cutaneous side effects were observed with systemic liposomal pristimerin.
Tumoricidal activity of pristimerin versus human myeloma xenografts in mice. Human myeloma cells from RPMI-8226 or OCI-MY5 cultures were implanted subcutaneously in the right flank of beige nude (BNX) mice in 50% (vol/vol) Matrigel matrix and tumors were allowed to establish over approximately 2 weeks. In initial testing, single paired mice with (A) 8226 or (B) MY5 xenografts were treated with daily subcutaneous pristimerin 2.5 mg/kg per day in a depot formulation, or with vehicle, and tumor size was monitored. Although an antitumor effect appeared likely, mice treated with subcutaneous pristimerin developed delayed injection site necrosis, requiring cessation of therapy and euthanasia. (C) Repeat efficacy studies, using xenografted BNX mice (n = 4/group) treated with systemic liposomal pristimerin or vehicle, delivered via tail vein injection, at doses escalating from 0.25 mg/kg per dose to 2.5 mg/kg per dose, administered 2 to 3 times weekly, commenced after mean tumor volumes exceeded 70 mm.3 P value was calculated by paired t test. No cutaneous side effects were observed with systemic liposomal pristimerin.
As pristimerin toxicity in this first experiment likely reflected high local drug concentrations associated with the mode of delivery, a systemic dosing strategy was instituted in a second experiment. A liposomal formulation of the triterpenoid was developed, successfully incorporating 98.7% of the drug; and, when given by intravenous tail vein injection proved better tolerated than deposition pristimerin. Studies of CDDO have similarly used a liposomal formulation to diminish toxicity.22,36 In the second experiment, pristimerin xenograft studies were conducted using 8226 tumors and escalating doses of liposomal pristimerin at 0.25 to 2.5 mg/kg per dose, 2 to 3 times weekly, commenced once tumors had exceeded a mean volume of 70 mm3 (Figure 6C). Statistically significant tumor growth inhibition occurred at pristimerin doses of 2 to 3 mg/kg intravenously twice weekly, compared with vehicle-treated mice (P < .01), despite considerable preceding tumor growth. Although the initial mice treated with subcutaneous depot pristimerin showed evidence of weight loss concurrent with development of cutaneous lesions, mice treated with liposomal pristimerin gained an average of 1.5 g during treatment, though this represented a mild reduction in growth compared with that observed in littermates.
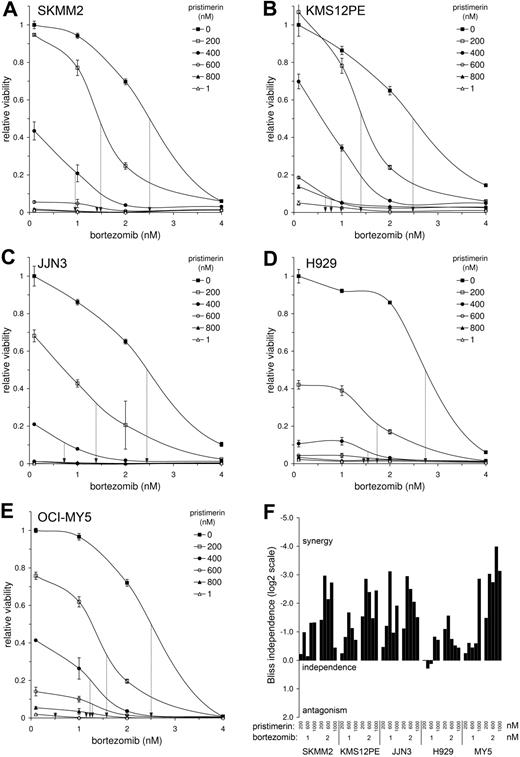
Pristimerin and bortezomib are synergistically cytotoxic to myeloma cells
Significantly, pristimerin synergistically chemosensitizes myeloma cells to bortezomib cytotoxicity (Figure 7). Bortezomib is perhaps the most efficacious agent used in the treatment of multiple myeloma today. Combining pristimerin and bortezomib together results in simultaneous reduction in the effective IC50 of both drugs, over a broad concentration range and against a spectrum of genetically heterogeneous myeloma cell lines—inducing significantly greater myeloma cell death than that anticipated from the individual effects of either drug alone. Synergistic cytotoxicity for myeloma could conceivably result from pristimerin's ability to inhibit noncanonical (as well as canonical) NF-κB signaling via its suppression of phospho-IKKα (Figure 4E), complementing bortezomib's effect on canonical NF-κB activity that results from proteosome inhibition. Alternatively the 2 compounds may cooperate to inhibit a more lethal spectrum of proteosome activities than occurs with either agent alone, as has been suggested to occur between NPI-0052 and bortezomib.38
Pristimerin and bortezomib are synergistically cytotoxic to myeloma cells across a broad range of concentrations. Human myeloma cell lines (A-E) were cotreated treated with pristimerin (IC0-IC100) and/or bortezomib (IC0-IC100) and viability (normalized to untreated cells) was determined by MTT assay at 72 hours. The bortezomib dose-response curve for each myeloma line is shown, with left-shifted bortezomib IC50 at each concentration of pristimerin illustrated as a vertical dashed arrow. Pristimerin and bortezomib uniformly chemosensitized myeloma cells to each other, reducing the effective concentrations required to induce 50% lethality (IC50) and causing synergistic cell death across a wide concentration spectrum. Similar results were obtained for t(11;14)–positive SKMM2 (A) or KMS12PE (B) cells; for t(4;14)–positive JJN3 (C) or H929 (D) cells; and for t(14;16)–positive OCI-MY5 (E); thus bortezomib-pristimerin synergy is not limited to a single molecular subgroup of tumor. (F) The synergistic, independent or antagonistic cytotoxic effects of combining pristimerin at 200, 400, 600, 800, or 1000 nM, with bortezomib at 1 nM or 2 nM, against 5 myeloma tumor lines, were evaluated using a score of Bliss independence37 (BI) and are plotted as a histogram. Negative values (plotted upward) suggest synergistic cytotoxicity from the combination of pristimerin and bortezomib that is more than that predicted by the product of effects of the agents acting independently (“more than additive” cytotoxicity). BI values are log2 based; therefore, the fold difference between the observed and expected viability resulting from combining both drugs is 2BI. Pristimerin and bortezomib commonly combine at active concentrations to produce synergistic myeloma cell cytotoxicity more than 2- to 3-fold greater than that expected from the product of effects of both drugs used independently of one another.
Pristimerin and bortezomib are synergistically cytotoxic to myeloma cells across a broad range of concentrations. Human myeloma cell lines (A-E) were cotreated treated with pristimerin (IC0-IC100) and/or bortezomib (IC0-IC100) and viability (normalized to untreated cells) was determined by MTT assay at 72 hours. The bortezomib dose-response curve for each myeloma line is shown, with left-shifted bortezomib IC50 at each concentration of pristimerin illustrated as a vertical dashed arrow. Pristimerin and bortezomib uniformly chemosensitized myeloma cells to each other, reducing the effective concentrations required to induce 50% lethality (IC50) and causing synergistic cell death across a wide concentration spectrum. Similar results were obtained for t(11;14)–positive SKMM2 (A) or KMS12PE (B) cells; for t(4;14)–positive JJN3 (C) or H929 (D) cells; and for t(14;16)–positive OCI-MY5 (E); thus bortezomib-pristimerin synergy is not limited to a single molecular subgroup of tumor. (F) The synergistic, independent or antagonistic cytotoxic effects of combining pristimerin at 200, 400, 600, 800, or 1000 nM, with bortezomib at 1 nM or 2 nM, against 5 myeloma tumor lines, were evaluated using a score of Bliss independence37 (BI) and are plotted as a histogram. Negative values (plotted upward) suggest synergistic cytotoxicity from the combination of pristimerin and bortezomib that is more than that predicted by the product of effects of the agents acting independently (“more than additive” cytotoxicity). BI values are log2 based; therefore, the fold difference between the observed and expected viability resulting from combining both drugs is 2BI. Pristimerin and bortezomib commonly combine at active concentrations to produce synergistic myeloma cell cytotoxicity more than 2- to 3-fold greater than that expected from the product of effects of both drugs used independently of one another.
Discussion
Triterpenoids such as CDDO, CDDO-Me (RTA 402), betulinic acid, and the ginsenosides possess anticancer activities in vitro and in vivo that appear to be mediated, at least in part, by their common ability to block TNFα-induced NF-κB activation via inhibition of IKKα, IKKβ, or IκBα10-16 ; and each of these unique triterpenoid compounds is currently being evaluated in United States–based clinical trials for the treatment of solid malignancies, lymphoma, or advanced dysplastic Nevus syndrome (http://clinicaltrials.gov). Here we demonstrate that the related triterpenoid, pristimerin, possesses substantial antimyeloma cytotoxic activity (IC50 < 100 nM) with a potency more than 10-fold that of CDDO or betulinic acid for solid organ malignancies, and more than 2- to 3-fold that of CDDO for multiple myeloma,39 and that pristimerin is synergistically cytotoxic with bortezomib, perhaps the most active antimyeloma agent in the clinic today. The potency of unmodified pristimerin for myeloma cells appears similar or better than that of the enhanced CDDO derivative, CDDO-Im.39,40
Uniquely, we find that pristimerin induces significant proteosome inhibition, which likely contributes to both its inhibition of NF-κBpathway signaling and specific cytotoxicity in myeloma. To our knowledge, no other triterpenoid has been demonstrated to inhibit proteosome function, although such activity could perhaps account for some of the activities of cytotoxic triterpenoids. Using in vitro and in vivo studies, we demonstrate that pristimerin causes selective antimyeloma cytotoxicity, within a therapeutic window, identifying it as a lead compound for the development of enhanced triterpenoid-derived anticancer pharmaceuticals. Provocatively, simultaneous targeting of both proteosome and NF-κB vulnerabilities of myeloma cells may enable pristimerin and its derivatives to overcome common resistance mechanisms to conventional therapeutics and may contribute to its synergistic enhancement of bortezomib.
The early genomic response to pristimerin closely resembles that of proteosome inhibitors MG-132 and MG-262, and more loosely that of HSP90 inhibitors. As might be expected, the expression signatures of proteosome inhibitors and HSP90 inhibitors are similar as both classes of drug cause a brisk unfolded protein response, either by inhibiting the clearance of proteins tagged for destruction or via inhibition of chaperone-assisted protein folding. Both MG-132 and MG-262, like bortezomib, are inhibitors of chymotrypsin-like and caspaselike 20s proteosome activity. Moreover MG-132, like bortezomib, also causes inhibition of NF-κB activity (reviewed in Nakanishi and Toi31 ).
Although an expression signature for bortezomib was not assessed for Cmap ranking against that of pristimerin, it is well established that bortezomib rapidly induces components of the proapoptotic terminal unfolded protein response, including PERK (an ER stress-specific eukaryotic initiation factor 2 [eIF2] kinase), activating transcription factor 4 (ATF4; an ER stress-induced transcription factor), and its proapoptotic targets, CHOP (DDIT3)41 and REDD1 (DDIT4). In a subtle contrast, pristimerin induces expression of ATF3 in myeloma cell lines (Table 1). Like ATF4, ATF3 is integral to the eIF2 kinase stress response42 and its expression is induced in response to endoplasmic reticulum (ER) stress by PERK. Increased expression of ATF3 requires ATF4 and can similarly lead to induction of CHOP42 ; furthermore, induction of both CHOP (DDIT3) and REDD1 (DDIT4) is in fact observed in both U266 and H929 myeloma cells within 4 hours of pristimerin exposure (Table 1), paralleling similar expression changes that occur with bortezomib.41
We first identified pristimerin initially because of its potent ability to induce suppression of the cyclin D2 promoter. Subsequently, pristimerin was found to inhibit expression of all 3 cyclin D proteins in human myeloma cells. Suppression of cyclin D by pristimerin occurs later than inhibition of NF-κB signaling, which occurs rapidly (Figures 1C, 2B, and 4G). Notably, evolutionarily conserved (mouse to human) NF-κB multitranscription factor binding sites are present in cyclin D promoters, 600- to 800-bp upstream of the transcription origin, and direct suppression of cyclin D expression has been observed following NF-κB inhibition induced by other compounds28-30 and following genetic NF-κB pathway manipulation.43 Mechanistically, therefore, pristimerin likely functions to first induce proteosome and NF-κB pathway inhibition, which then secondarily perturbs cell-cycle and apoptosis pathways, including cyclin D regulation. Cyclin D expression may be influenced by this agent at the level of transcription (due to NF-κB inhibition) and/or translation (due to ER stress44 ). Multifunctional targeting of both proteosome and NF-κB pathways by pristimerin contributes to the potent activity of this triterpenoid toward myeloma cells. These studies provide the rationale for exploration and use of pristimerin-derived proteosome inhibitors as novel multifunctional therapeutic agents for human malignancy and support early drug combination studies with bortezomib.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
R.E.T. was supported by Fellowship Awards from the Multiple Myeloma Research Foundation (MMRF; Norwalk, CT) and the Hematology Society of Australia and New Zealand (HSANZ; Sydney, Australia); and A.K.S. was supported by Senior Awards from the Leukemia & Lymphoma Society (LLS; White Plains, NY) and MMRF.
Authorship
Contribution: R.E.T. designed and performed research, analyzed the data, and wrote the paper; J.J.K. contributed analytical tools; J.S., C.-X.S., Y.X.Z., S.E.P., and X.M. performed research; A.D.S. designed research; and A.K.S. designed research and analyzed the data.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Rodger Tiedeman, Mayo Clinic, Collaborative Research Building 3-001, 13400 E Shea Blvd, Scottsdale, AZ 85259; e-mail: tiedemann.rodger@mayo.edu.