To the editor:
Marneros and colleagues have described multiple skin erosions in a patient receiving pralatrexate, a novel inhibitor of dihydrofolate reductase, for the treatment of adult T-cell lymphoma/leukemia (ATLL).1 These skin erosions were not due to the toxicity of the drug on keratinocytes but rather to the apoptosis of intra-epidermal atypical T cells as evidenced by the selective erosions on pre-existing tumoral skin lesions and by the positive labeling of the atypical T cells for activated caspase 3. The skin erosions healed a few days later and did not recur with subsequent cycles of pralatrexate therapy.
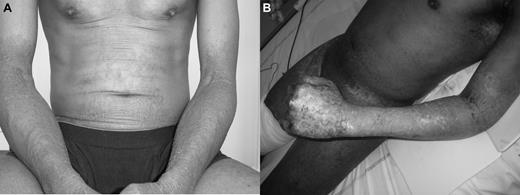
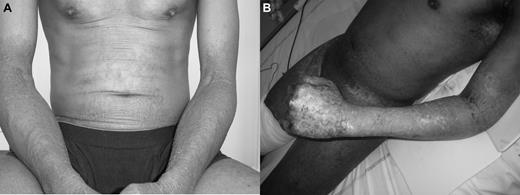
We report the case of a patient with ATLL who had multiple skin erosions limited to areas previously affected by the tumoral infiltration and that recurred after 2 chemotherapies that did not include pralatrexate. The patient was a 50-year-old male from Guadeloupe in the French West Indies who was diagnosed 1 year earlier with smoldering human T-lymphotropic virus type 1 (HTLV-1)–induced T-cell lymphoma (erythematous patches with epidermotropic infiltrate of atypical T cells, HTLV-1 antibody titer positive and clonal integration of HTLV-1 genes in the skin) according to international criteria.2 Interferon-α2b treatment was given but in addition to the cutaneous lesions (Figure 1A), the patient developed generalized fatigue, leukocytosis (217 000 white blood cell count with 95% atypical lymphocytes positive for CD4 and CD25 by immunophenotyping), and hypercalcemia consistent with leukemic conversion of his ATLL. The patient received 2 cycles of cyclophosphamide associated with VP16, allowing partial decrease of the leukocytosis (81 000 white blood cell count). An additional chemotherapy with hyper-CAVD (cyclophosphamide, adriamycine, vincristine, dexamethasone) was administered, and 4 days later the patient developed multiple skin erosions on the previously infiltrated areas. The skin lesions spontaneously healed and 19 days later, the patient received high-dose methotrexate. Five days later, he developed multiple skin erosions on the same areas (Figure 1B). Skin erosions were negative for herpes simplex virus. Histologic examination of the skin erosions showed extensive epidermal ulceration with large atypical CD3+CD4+CD25+ T lymphocytes in the dermis. In nonulcerated areas, many epidermotropic atypical lymphocytes were present. The epidermis was atrophic without pathologic evidence for toxic epidermal necrolysis or pemphigus. The skin lesions spontaneously healed with topical application of antiseptic solutions and Vaseline, but the patient died 2 weeks later because of a septic shock.
Photographs show patient at leukemic conversion phase of ATLL (A) and 5 days after methotrexate injection (B).
Photographs show patient at leukemic conversion phase of ATLL (A) and 5 days after methotrexate injection (B).
Our case report is consistent with the fact that intra-epidermal atypical T lymphocytes in patients with ATLL may undergo apoptosis after numerous chemotherapies and not only after pralatrexate. The mechanism of these lesions may be linked to what happens during tumor lysis syndrome in patients having chemotherapy for cancer.3 Therefore, we propose the denomination “cutaneous tumor lysis syndrome” should be used to describe skin erosions not otherwise explained in patients receiving chemotherapy for ATLL.
Authorship
Contribution: All authors analyzed the data and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Dr Jean-David Bouaziz, Hôpital Saint Louis, Université Paris 7, Paris, France; e-mail: bouaziz.jd@wanadoo.fr.