Abstract
Abstract 4932
Plasma cell leukemia (PCL) is a rare, poorly understood and clinically aggressive plasma cell dyscrasia that can originate from multiple myeloma (sPCL) or de novo as primary PCL (pPCL). Historically, median survival of patients with PCL has been reported to be 1 and 11 months for patients with secondary and primary PCL, respectively (Tiedemann, Leukemia 2008). The impact of novel agents and transplantation strategies on outcomes of patients with PCL remains unclear. In addition, few have reported extensively on the cytogenetics abnormalities seen in patients with PCL especially with respect to outcomes with novel therapies (proteasome inhibitor or immunomodulator). Accordingly, we thought to evaluate the clinical, cytogenetic features and outcomes of patients with PCL treated at H. Lee Moffitt Cancer Center in the era of novel agents and transplant strategies.
Retrospective review of records of patients with PCL diagnosed after 2003. The diagnosis of PCL was according to the IMWG criteria (specifically peripheral blood plasma cells ≥ 20% or 2 ×109/L). Clinical data reviewed included basic demographic, laboratory, pathologic, treatment and outcomes variables. Cytogenetics was reviewed by metaphases and FISH. Overall survival was defined as the time from diagnosis of PCL to death or last follow-up. Response criteria was according to the IMWG. Treatment was at the discretion of the treating physician.
Twenty four patients with PCL were identified: 15 patients had pPCL and 9 had sPCL. The median age of all patients was 58 years (range 37-77years). The median peripheral WBC was 15×109/L (range 3-102 ×109/L) and the median percent of peripheral plasma cells was 40% (15-93%). The median β2 microglobulin was 3 mg/L (range 1.4-23). Nine patients (38%) had renal failure (creatinine>2.0mg/L) at diagnosis of PCL and 11/19 (58%) had a serum LDH greater than the institution's upper limit of normal. Two patients had CNS disease and 6 patients had extramedullary disease.
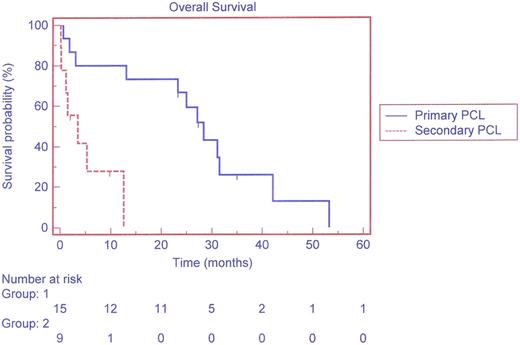
Regarding metaphase cytogenetics: One patient had a novel translocation involving 3 separate breakpoints, which included: ins(6;14)(p22;q32q32)t(6;11)(p22;q13), der (14) ins (11)(q32;q13q13)?? t(6;14)(p22;q32), 3 patients (2 with pPCL) had a translocation between chromosomes 1 and 16 including t(1;16)(q21;q24), t(1;16)(q21;22) and t(1;16)(break points not reported). 14/23 patients with PCL (61%) had deletion of chromosome 13 by either FISH or cytogenetics; while 80% of patients with pPCL (12/15) had 13q deletion. Only one patient had deletion 17p. 11 patients received bortezomib based therapy and 19 patients received a novel agent, 5 had an allogeneic transplant, 19 had high dose therapy and autologous transplantation). Best response to therapy was as follows: 9 CR, 4 VGPR, 4PR, 1MR, 2 Non evaluable (PR and better: 77%). After a median follow up of 13 months, 5 remain alive (all had autologous transplant and 3 had an allogeneic transplant) (median follow up 2 years; range 2-34 months). The median overall survival for pPCL compared to sPCL via Kaplan-Meier was 28.4 vs. 3.5 months, respectively (p=0.0018). See Figure 1.
We herein report novel cytogenetic abnormalities in patients with PCL (1 unique translocation involving chromosomes 6, 11 and 14 as well as 3 patients with t(1; 16) which has rarely been reported). Despite generally poor outcomes with traditional therapies, patients treated with novel agents and allogeneic transplant may enjoy a longer survival than previously reported.
Off Label Use: Lenalidomide in newly diagnosed myeloma. Baz:celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.