Abstract
Most patients diagnosed with primary chronic cold agglutinin disease (CAD) have a clonal lymphoproliferative bone marrow disorder. Treatment with rituximab is the only well-documented effective therapy, leading to 45%-60% partial responses (PR). Complete responses (CR) are rare, and median response duration is only 11 months. In a prospective multicenter trial, 29 patients received rituximab 375 mg/m2 on days 1, 29, 57 and 85; and fludarabine orally, 40 mg/m2 on days 1-5, 29-34, 57-61 and 85-89. Twenty-two patients (76%) responded, 6 (21%) achieving CR and 16 (55%) PR. Among 10 patients nonresponsive to rituximab monotherapy, 1 achieved CR and 6 PR. Median increase in hemoglobin level was 3.1 g/dL among the responders and 4.0 g/dL in those who achieved CR. Lower quartile of response duration was not reached after 33 months. Estimated median response duration was more than 66 months. Grade 3-4 hematologic toxicity occurred in 12 patients (41%). In conclusion, fludarabine and rituximab combination therapy is very efficient in patients with CAD. Toxicity may be a concern, and benefits should be carefully weighed against risks in very old and comorbid patients. It remains to be established whether the combination should be first-line or an efficient second-line therapy in CAD patients requiring treatment. This study is registered at http://www.clinicaltrials.gov as NCT00373594.
Introduction
The epidemiology, pathogenetic mechanisms and clinical features of chronic cold agglutinin disease (CAD) have been quite extensively elucidated in the literature,1-5 but therapy remains suboptimal.6-10 Although most authors emphasize the importance of avoiding cold exposure, a population based study showed that drug therapy had been attempted in more than 70% of the patients,9 indicating that counseling is insufficient as sole therapeutic measure in a majority. The requirement for effective pharmacologic treatment is also highlighted by hemoglobin (Hgb) levels less than 8.0 g/dL in one-third and cold-induced circulatory symptoms in more than 90% of unselected patients with CAD, whereas 50% of such patients were found to have received blood transfusions during the course of the disease.9 Corticosteroids, conventional immunosuppressive drugs and alkylating agents are generally ineffective.6,9 Treatment with the monoclonal anti-CD20 antibody rituximab is the only well-documented effective therapy, leading to partial responses (PRs) in 45%-60% of the patients, but complete responses (CRs) are rare.9,11,12 A median response duration of 11 months (range, 2-42 months) has been reported.11
Although rituximab therapy is effective in polyclonal autoimmune diseases,13,14 part of the rationale for rituximab in CAD was the demonstration of a monoclonal, B-cell lymphoproliferative bone marrow disorder in more than 90% of patients traditionally classified as having primary CAD.4,9,11 Histologic signs of nonHodgkin B-cell lymphoma were present in bone marrow biopsy specimens from 75% of unselected patients with CAD in a population based study.9 The most frequent type was lymphoplasmacytic lymphoma (LPL), which was found in 50% of the patients.
We wanted to improve on the results achieved by rituximab single-agent therapy in patients with primary CAD. The purine analogues, eg fludarabine and cladribine, are powerful therapeutic agents in a variety of lymphoproliferative diseases. Although therapy with fludarabine for CAD has not been studied systematically, successful treatment was reported in one patient.15 Histologic remission of the bone marrow lymphoproliferative disorder was observed after cladribine therapy in a series of 5 patients, but clinical remission was not achieved.8 Fludarabine therapy, alone or in combination with rituximab, has yielded high response rates in Waldenström macroglobulinemia (WM), which is considered a closely related entity.16-18 Furthermore, treatment with the fludarabine and rituximab combination has been found feasible and efficient in follicular lymphoma.19 In the present study we have investigated the potential of fludarabine and rituximab in combination in patients with CAD requiring treatment.
Methods
Study design
We conducted a prospective, uncontrolled multicenter trial of combination therapy with fludarabine and rituximab in patients with CAD requiring treatment. The Regional Medical Research Ethics Committee of Southeast Norway and the Norwegian Medicines Agency approved the protocol, which was posted at www.clinicaltrials.gov as NCT00373594. Eleven Norwegian hospitals participated, and patients were enrolled between February 1, 2005, and October 31, 2009. We have also included in this report 3 pilot patients treated in 2004 according to the same protocol
All patients underwent clinical examination, chest radiography and abdominal ultrasonography before inclusion. We recorded hematologic, biochemical, and immunologic blood and serum parameters. Flow cytometric immunophenotyping of bone marrow aspirates was performed as described previously.4,5 A centralized examination of trephine biopsies was done by experienced lymphoma pathologists (U.R. and K.B.), and lymphoproliferative disorders were classified according to the 2001 version of the World Health Organization (WHO) classification.20
Inclusion and exclusion criteria
To be eligible for the trial, each patient had to be diagnosed with CAD and require therapy because of anemia, substantial cold-induced circulatory symptoms, or both. We defined CAD as the combination of chronic hemolysis, a cold agglutinin (CA) titer at 4°C of 64 or higher and a typical pattern for the direct antiglobulin test (DAT). The typical DAT pattern was defined as a positive polyspecific DAT combined with a positive monospecific DAT for complement protein C3d and a negative (or only weakly positive) test for immunoglobulin G (IgG).9 Serum and bone marrow examinations had to confirm the presence of a clonal B-cell lymphoproliferation, as described by the combination of a monoclonal Ig band and a clonal expansion in bone marrow of lymphocytes of the corresponding phenotype, demonstrated by immune histochemistry, flow cytometry, or both.4,9,21 Informed consent was obtained from each patient in accordance with the Declaration of Helsinki.
Patients who had a typical secondary CAD (eg, CAD associated with an apparent or aggressive lymphoma) were excluded. Patients were also ineligible if they had blood lymphocyte counts of more than 50 × 109/L, nonlymphatic malignant disease other than basal cell carcinoma of the skin, severe organ dysfunction unrelated to CAD, contraindications to therapy with rituximab or purine analogs, estimated glomerular filtration rate less than 30 mL/min, or inability to cooperate.
Therapy
Eligible patients received rituximab (MabThera) intravenously at a dose of 375 mg/m2 on days 1, 29, 57, and 85 (4 infusions altogether), administered according to the manufacturer's recommendations. They also received fludarabine (Fludara) orally, 40 mg/m2 on days 1-5, 29-34, 57-61, and 85-89. The dose of fludarabine was reduced according to the protocol in case of toxicity or pre-existing renal failure. Use of growth factors, cotrimoxazole or antiviral prophylaxis was not required according to the protocol.
Patients were assessed before each cycle of therapy and monthly thereafter for 6 months. Blood samples were collected at each visit, and cold-induced circulatory symptoms were recorded using a 0-2 scale (0 indicates no improvement; 2 indicates complete resolution). Adverse events related to rituximab or fludarabine were recorded. Bone marrow histology and flow cytometry were assessed at 3 months after completion of therapy. After the initial follow-up, clinical and hematologic data were recorded at approximately 3-month intervals for the remaining time of the trial.
Response and relapse definitions
We used the same response criteria as previously published.1,11 CR was defined as absence of anemia and hemolysis, complete resolution of clinical symptoms, undetectable monoclonal IgM by serum electrophoresis and immunofixation; and no signs of clonal lymphoproliferation as assessed by flow cytometry, bone marrow histology and immunohistochemistry. The criteria for PR were a stable increase in Hgb level by at least 2.0 g/dL or to the normal range, a decrease in serum IgM concentration by at least 50% or to the normal range, improvement of clinical symptoms and transfusion independency. No response (NR) was defined as failure to achieve CR or PR.
Time to response was the time from start of the first therapy cycle to the achievement of any degree of response. Response duration was the time from achievement of response to relapse or death. The criteria for relapse were a decrease in Hgb level to below 10.0 g/dL or by at least 2.0 g/dL from the highest level achieved, and/or recurrence of clinical symptoms.
Statistics
The primary objective was to assess the efficacy of fludarabine plus rituximab in CAD. The secondary objectives were safety in the whole cohort and efficacy in patients who previously had received rituximab monotherapy. Median values were determined in order to express the central tendency of variables. We used the Wilcoxon test to calculate the statistical significance of differences between paired continuous data. Fisher exact test was used to assess the significance of differences between frequencies in cross tables of nominal variables, and Spearman ρ was calculated to examine correlations between numeric variables when at least one variable was ordinal. We did a Kaplan-Meier analysis of response duration.
Results
Baseline characteristics
Twenty-nine patients were included: 12 men and 17 women, with a median age of 73 years (range, 39-87) and median disease duration of 5 years (0-28). Twenty-five patients (86%) had cold-induced circulatory symptoms, whereas exacerbation of anemia during febrile disease had been recorded in 19 (66%). Median Hgb level was 8.7 g/dL (range, 5.4-15.6 g/dL; 2 nonanemic patients were included because of disabling circulatory symptoms). Additional baseline laboratory data are provided in Table 1. The clonal serum Ig class was IgMκ in 27 patients (93%), both IgAλ and IgMλ in 1 patient, and IgGκ in 1 patient. In 4 patients (14%), the monoclonal band was not observed by electrophoresis without immunofixation but detected after additional immunofixation. Histologic signs of a clonal lymphoproliferative bone marrow disorder were found in 21 (75%) of 28 evaluable biopsy specimens; LPL in 12 patients (43%), marginal zone lymphoma in 6 (21%) and unclassified clonal B-cell proliferation in 3 (11%). Since all patients with LPL had monoclonal IgM in serum, 12 patients (43%) were classified as also having WM.18 Fifteen patients (52%) had previously received rituximab monotherapy one or more times, resulting in 1 CR, 4 PR and 10 NR following the last series of infusions.
Response data
Table 2 shows the essential response data. Twenty-two patients (76%) responded to therapy. Six patients (21%) achieved CR and 16 (55%) PR, while 7 (24%) were nonresponders. Median time to response was 4.0 months (range, 0.3-6.0 months). Median increase in Hgb level was 3.1 g/dL (range, 0-6.9 g/dL) in the responders (4.0 g/dL and 3.1 g/dL in those who achieved CR and PR, respectively) and 2.5 g/dL (−1.2-6.9 g/dL) in the total cohort. Nonresponders had no significant change in their Hgb levels. In the 10 patients who had previously received rituximab monotherapy without achieving response, we observed 1 CR and 5 PR after combination therapy, while 4 were still nonresponders.
Follow-up trephine biopsies showed a partial or complete histologic remission of the lymphoproliferative bone marrow disorder in 9 (56%) of those who achieved PR. In the remaining partial responders, rebiopsy was either not relevant (3 patients who had no histologic signs of bone marrow lymphoma at baseline) or not done for other reasons (4 patients). Patients achieving CR had a complete histologic resolution of the lymphoproliferative bone marrow disorder by definition. Five patients achieving CR had no detectable CA in serum after CR was observed, whereas the CA titer decreased to 64 in the sixth complete responder. In the partial responders, CA titer declined by a median of 62.5% (range, 50%-87.5%).
Considering all patients, we found a weak negative correlation (Spearman ρ, −0.40) of borderline significance (P = .05) between cellular κ/λ ratio in bone marrow aspirate at baseline and response level; and a still weaker negative correlation was found between age and response level (Spearman ρ, −0.37; P = .049). We found no correlation between response level and baseline levels of Hgb, IgM, C4, or CA titer.
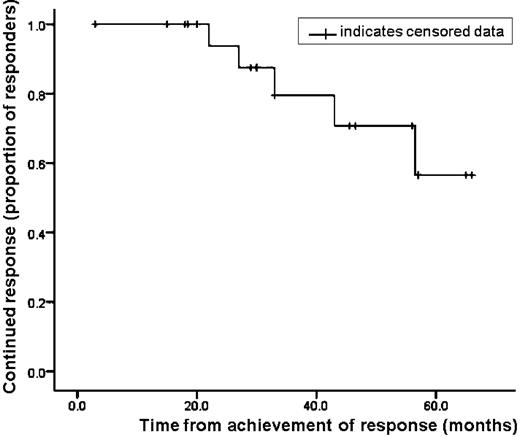
In the responders, the median time of observation from achievement of response to censoring of data was 33 months (range, 3-66 months). At this time, 5 patients (23% of all responders and 31% of the partial responders) have relapsed while 17 patients (77%) experience sustained remission. Correspondingly, the median or lower quartile observed response duration has not yet been reached. The range of observed response duration (from achievement of response to relapse or censoring of data) was 3-66 months. All relapses occurred among the partial responders. Using Kaplan-Meier analysis, the estimated lower quartile of response duration was 43 months, whereas the estimated median response duration was more than 66 months (Figure 1).
Response duration. Kaplan-Meier graph relating response status to duration (time from achievement of response to relapse or censoring of data) in the 22 complete or partial responders.
Response duration. Kaplan-Meier graph relating response status to duration (time from achievement of response to relapse or censoring of data) in the 22 complete or partial responders.
Tolerance
Two male nonresponders, 76 and 77 years old, died 7 and 9 months after start of therapy from cerebral stroke and pneumonia, respectively. They had no neutropenia or thrombocytopenia during the terminal illness.
Adverse events including cytopenias grade 1-2 without clinical manifestations were recorded in 22 patients (76%). Hematologic toxicity grade 3-4 occurred in 12 patients (41%), including grade 4 toxicity in 4 (14%). Neutropenia with neutrophil counts below 0.5 × 109/L was responsible for all cases of grade 4 toxicity. There was no significant association between hematologic toxicity grade 3-4 and age (below 73 years vs 73 years and older; Fisher exact test). Seventeen patients (59%) experienced infection grade 1-3, which was successfully treated in all, except for the patient who died of pneumonia after 9 months. Two nonresponders, however, were reported by the local investigators to have a reduced quality of life for months after completing therapy because of recurrent respiratory tract infections. Infection grade 4 or Pneumocystis jirovecii pneumonia was not observed. Three patients (10%) had herpes zoster reactivation.
Temporary exacerbation of hemolysis was observed during treatment in 3 patients (10%). All 3 hemolytic events occurred during febrile infection with high C reactive protein (CRP) levels,22,23 resolved readily upon antimicrobial therapy, and monospecific DAT remained negative for IgG.
Both medications were administered according to the normal dose schedule prescribed by the protocol in 16 patients (55%). In this subgroup, 2 patients achieved CR, 10 had PR and 4 NR. Among those who experienced toxicity, dose reduction or discontinuation of fludarabine according to the protocol occurred in 13 patients (45% of total). The median cumulative dose reduction in this subgroup was 20% (range, 12.5%-75%). We observed 4 CR, 6 PR, and 3 NR among these patients, including 3 PR in patients who had fludarabine discontinued after 1-3 cycles. Calculated from these figures, there was no significant association between response level and adherence to treatment schedule (Fisher exact test).
Discussion
With a response rate of 76%, the fludarabine and rituximab combination is a very efficient treatment for primary CAD. Randomized trials are unlikely to be undertaken in this uncommon disease,9 and comparison of nonrandomized trials should be interpreted with caution. Nevertheless, the inclusion and response criteria used in both the Norwegian and the Danish studies of rituximab monotherapy were very similar to the definitions used in this trial, and the baseline data reported in the Norwegian study matched very well with those found in the present study.11,12 Furthermore, the baseline characteristics were perfectly comparable with those of an unselected CAD population.9 In our opinion, the 76% response rate achieved by fludarabine and rituximab in combination compares favorably with the 50%-55% response rate observed after rituximab monotherapy.
CR was achieved in 6 patients (21%). A significant number of CR has never been reported with any therapy for CAD. The substantial increase in Hgb levels and improvement of cold-induced circulatory symptoms also indicate a major improvement of quality of life in most complete and partial responders. Although the trial was one-armed, 10 patients acted as their own controls by having previously received rituximab without achieving remission. With the findings of 1 CR and 6 PR in this subgroup, the combination has been shown to be effective even in patients nonresponsive to rituximab monotherapy. The response duration reported (observed lower quartile not reached after 33 months; estimated median more than 66 months) is also very favorable compared with the median response duration of 11 months reported after rituximab monotherapy.11
The exact mechanism of action of effective treatment for CAD has not yet been established. Considering the lack of effect of corticosteroids and conventional immunosuppressive agents,1,6,9 it may be hypothesized that mechanisms related to unspecific immune suppression are not essential. Previous studies of rituximab therapy were based on the presence of a clonal lymphoproliferative B-cell disorder in the bone marrow of most if not all patients with primary CAD,2,4,9,24 testing the hypothesis that targeting the pathogenic cell clone would provide an efficient therapy.11,12 We previously found, however, that PR was often achieved even though the median IgM level reduction was modest (only 54%).11 Furthermore, monotherapy with rituximab and, to some extent, purine analogs has been found beneficial in polyclonal autoimmune diseases as well.13,14,25 For autoimmune disorders in general, several alternative mechanisms of action of anti-CD20 directed therapy have been proposed, such as modulation of more global B-cell functions, receptor blocking or interfering with antigen-presenting cells.26,27 In this study, clinical and hematologic remissions were invariably linked to resolution of the lymphoproliferative bone marrow disorder. Compared with studies of rituximab monotherapy,11 the higher response rate observed in this study was also accompanied by a more profound decline in IgM levels. Furthermore, no relapses have been observed during the study period among those who achieved CR, which by definition included complete histologic resolution and disappearance of monoclonal IgM. These findings provide support for the hypothesis that targeting the pathogenic B cell clone efficiently is important for the clinical effect.
Most drug-related grade 1-3 cytopenias observed in this trial were nonsymptomatic, indicating that a majority of the patients tolerated the treatment quite well. The frequencies of grade 3-4 and grade 4 hematologic toxicity (41% and 14%, respectively) were, however, substantial. The occurrence of 2 deaths during several years' observation was not unexpected in this elderly patient cohort, although connection with therapy could not be ruled out in the patient who died of pneumonia after 9 months. Even though all other clinical infections were successfully treated, 2 patients were reported to have problems with recurrent respiratory tract infections for months. Antiviral prophylaxis was not mandatory according to protocol, and 3 patients experienced herpes zoster reactivation. Overall, more significant toxicity was observed in this trial compared with rituximab monotherapy.11,12
In the 3 cases of temporary exacerbation of hemolysis, the hemolytic episode occurred during febrile infection with high CRP level. This association has previously been well documented and explained as being caused by increased complement production in patients with constantly low levels of C3 and particularly C4.5,22,23 The rapid improvement upon antimicrobial therapy and lack of IgG expression on the erythrocyte surface during these episodes also clearly indicate that exacerbation of hemolysis was induced by acute phase reaction, not by fludarabine.
It may be argued that a chronic disease often perceived by physicians as mild should not be treated with toxic drugs. In a population based study of 86 unselected patients with CAD, however, Hgb levels were 8.9 g/dL or below in one-half of the patients and 8.0 g/dL or below in one-third; cold-induced circulatory symptoms, history of pharmacologic therapy, and perceived transfusion requirements were reported at high frequencies.9 In many patients, therefore, CAD is not an indolent disease in terms of clinical symptoms and quality of life. Taking into consideration the very favorable response rate and response duration achieved in this study, we conclude that despite the existing risk of adverse effects, fludarabine and rituximab combination therapy is often justified in patients with CAD requiring treatment.
The present study was not designed to address the risk of late-occurring secondary hematologic malignancies. Although not specific to nucleoside analogues, such late events have been reported after fludarabine-based therapy for WM.28 Such concerns should not be prohibitive to the use of combination therapy but result in an individualized, balanced consideration of risk versus benefit, particularly in the youngest patients. Regarding the older patients, we found no association between toxicity and age itself. Nevertheless, many patients with CAD are old and frail,9 and rituximab monotherapy may represent a safer option in very old and comorbid individuals.
Although nearly half of the patients had their doses of fludarabine reduced, we found no association between response level and adherence to the scheduled dose. Furthermore, based on a small retrospective series mainly of polyclonal disorders, it has been suggested that the dose of rituximab in autoimmune cytopenias may be reduced without losing the therapeutic effect.29 Thus, a potential may exist for optimizing the doses of rituximab and fludarabine.
In conclusion, fludarabine and rituximab combination therapy is very efficient in patients with CAD, resulting in a high response rate and durable remissions. For the first time, we report on a considerable number of CR after therapy for CAD, and remissions have been achieved in patients nonresponsive to rituximab monotherapy. Toxicity, particularly hematologic toxicity, is more frequent than after rituximab monotherapy, and some caution should be exerted in the oldest and most frail patients. It remains to be established whether the fludarabine-rituximab combination should be considered first-line or an efficient second-line therapy in patients with CAD requiring treatment.
An Inside Blood analysis of this article appears at the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Jann Bergheim, Jenny Foss Abrahamsen, Jörg Axel Bohl, Jack Johansen, Per Arne Standal, Vigdis Stenberg, Terje Andersson, Eystein Brandt, Håvar Knutsen, Robert Brudevold, and Petter Quist-Paulsen for participating in examination and treatment of patients. We are most grateful to Elling Ulvestad for productive collaboration during many years and for his scientific contributions to the understanding of primary CAD.
This work was supported by grants from the public hospital trusts Helse Vest RHF and Helse Fonna HF and from Larvik Society Against Cancer.
Authorship
Contribution: S.B. and G.E.T. designed the study; S.B., G.E.T., A.M.V., H.H.-H., A.V., E.-M.J., J.D. and A.S.T. did clinical research and collected data; U.R. and K.B. examined the bone marrow biopsy samples; S.B. analyzed the data and wrote the paper in cooperation with G.E.T.; and all authors discussed the findings, reviewed the manuscript critically and approved the submitted version.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Sigbjørn Berentsen, Department of Medicine, Haugesund Hospital, PO Box 2170, N-5504 Haugesund, Norway; e-mail: sigbjorn.berentsen@haugnett.no.