Abstract
Hematopoietic stem cell transplantation (HSCT) is limited by patient susceptibility to opportunistic infections. One of the most devastating infections after HSCT is invasive aspergillosis (IA), a life-threatening disease caused by Aspergillus fumigatus. Transplantation of hematopoietic stem cells (HSCs) and myeloid progenitor cells (MPCs) has been shown to mediate protection against IA, but little is known about the factors that regulate HSC and MPC cell expansion after transplantation. Herein, we investigated the role of CCR7 in a murine model of IA after combined HSC and MPC transplantation into lethally irradiated wild-type (WT) mice. Nonirradiated CCR7−/− mice had expanded populations of HSCs in the bone marrow and spleen, compared with WT mice. Irradiated WT mice reconstituted with CCR7−/− HSCs and MPCs had increased survival, decreased fungal burden, and enhanced myeloid leukocyte numbers during IA, compared with WT controls. In addition, WT mice reconstituted with WT HSCs and MPCs and treated with anti-CCR7 exhibited accelerated myeloid cell expansion similar to that observed in CCR7−/−→WT chimeras. Thus, removal of the inhibitory effects of CCR7 through genetic alteration or ligand immunoneutralization enhanced myeloid reconstitution, thereby accelerating fungal clearance in a murine model of IA.
Introduction
Hematopoietic stem cell transplantation (HSCT) has shown significant promise to treat and cure a variety of hematologic and nonhematologic diseases. One of the major drawbacks of this therapy is the period of profound leukopenia after therapy, a result of the myeloablation conditioning before transplantation, which increases susceptibility to a variety of opportunistic infections. There are several prominent viral infections and a wide array of Gram-positive and -negative bacteria that pose a significant risk for HSCT patients.1-3 In addition, fungal infections, particularly those from the Aspergillus species, are associated with a high incidence of morbidity and mortality after transplantation.4,5
Invasive aspergillosis (IA) is an acute, life-threatening disease in which inhaled conidia from Aspergillus fumigatus are not adequately cleared from the lung. Consequently, conidia germinate into hyphae and invade the lung parenchyma and vasculature, leading to severe pneumonia, massive inflammation, and fungal dissemination.6 IA primarily affects immunocompromised individuals and has been identified in as many as 10% of patients who have had an allogeneic HSCT, with mortality rates as high as 80%-90%.7 Neutropenia was originally recognized as a major risk factor in the development of IA, but recent work has demonstrated that several effector cell populations, including natural killer cells, T cells, macrophages, and myeloid dendritic cells (DCs), function in conjunction with neutrophils to mediate proper clearance of this pathogen.8-12
For HSCT to be a viable treatment option for a broad range of diseases, investigators have examined methods of enhancing myeloid cell presence and function to prevent opportunistic infections after transplantation, with encouraging results.13-16 Common myeloid progenitors (CMPs) reconstitute the entire myeloid compartment, while granulocyte-monocyte progenitors (GMPs) differentiate into granulocytes and monocytes.17 It was recently demonstrated that an infusion of myeloid progenitor cells (MPCs; CMPs and GMPs) during HSCT provided protection from IA in a murine model, compared with HSCs alone.15,16 Protection was mediated by enhanced immune reconstitution, which included a significant increase in the number of neutrophils present after HSCT. Thus, accelerated myeloid reconstitution through the use of MPCs during HSCT may be an attractive therapeutic option.
Recent work has focused on targeting chemokine/chemokine receptor interactions to enhance the engraftment and repopulation of the bone marrow (BM) compartment.18 Disruption of the interaction between CXCR4 and stromal cell–derived factor-1 (SDF-1), which functions to tether hematopoietic stem cells (HSCs) within the BM compartment, mobilizes HSCs out of the BM and into the peripheral blood, resulting in HSCs with superior repopulating potential, compared with that of BM-derived HSCs.19,20 Similar results have been achieved through the administration of CXCL2, which upon binding to its receptor, CXCR2, induces a neutrophil-mediated release of stem cells into the peripheral blood.21 In addition to stem cell mobilization, several chemokines have also been shown to impair the proliferation of hematopoietic progenitor cells in vitro and in vivo, including CCL19, and CCL21, the ligands for CCR7.22,23
In the present study, we used a murine model to examine the role of CCR7 on HSCs and MPCs during IA after HSCT. Analysis of HSCs from the BM and spleen of naïve CCR7−/− mice showed a significant increase in the number of HSCs, compared with the BM and spleen of wild-type (WT) mice. In addition, we observed that WT mice receiving CCR7-deficient HSCs and MPCs (CCR7−/−→WT chimeras) were markedly less susceptible to IA 14 days after HSCT than WT mice receiving WT HSCs and MPCs (WT→WT chimeras). This protective effect was a result of accelerated myeloid hematopoiesis in mice receiving CCR7-deficient HSCs and MPCs. The BM compartment, spleen, and lungs of mice receiving CCR7-deficient cells all showed increased myeloid cell numbers. Immunoneutralization of CCR7 using monoclonal antibody approaches during and after HSCT of WT HSCs and MCPs into WT recipients revealed that anti-CCR7 antibody treatment significantly increased the numbers of pulmonary effector cells during IA, compared with immunoglobulin G (IgG)–treated mice. Together, these findings demonstrate that CCR7 regulates myeloid cell reconstitution, resulting in delayed hematopoiesis after HSCT and, consequently, increased susceptibility to IA.
Methods
Mice
WT C57BL/6 and WT GFP+ mice were purchased from Jackson Laboratories. WT B6-LY5.2/Cr (CD45.1) mice were obtained from the NCI. CCR7−/− mice were generated and back-crossed on a C57BL/6 background by Dr Martin Lipp's group (Max-Delbrück-Center for Molecular Medicine, Germany) as previously described.24 For all experiments, mice were age- and sex-matched. Mice were used in accordance with regulations mandated by the University Committee on the Use and Care of Animals at the University of Michigan, which approved all animal studies included here.
Isolation of HSCs, CMPs, and GMPs
Hematopoietic cell isolation was performed as previously described, with a few modifications.25 Briefly, BM cells from WT or CCR7−/− mice were flushed from the femur and tibiae with sterile staining media (phosphate-buffered saline [PBS] with 5% fetal calf serum [FCS]). BM cells were filtered to yield a single-cell suspension. Using biotinylated antibodies, BM cells were labeled with the lineage markers, Ter119, Gr-1, B220, Mac-1, CD127, and CD3 (BD Biosciences) and were depleted using antibiotin beads (Miltenyi Biotech). The remaining cells were stained with fluorescein isothiocyanate (FITC) CD34 (eBioscience), phycoerythrin (PE) CD16/32, PE-CY7 Sca-1, allophycocyanin (APC) c-kit, and APC-CY7 streptavidin or PerCP-Cy5.5 CD150, FITC CD48, PE-CY7 Sca-1, APC c-Kit, and APC-CY7 streptavidin (BD Bioscience). Cells were sorted using a BD FACS Aria. HSCs were identified as lineage−, c-Kit+, Sca-1+, and either CD34− or CD150+ and CD48−. Collectively, CMPs and GMPs were defined as lineage negative, c-kit+, sca-1−, and CD34+. CMPs were CD16/32lo, while GMPs were CD16/32hi.
Reconstitution assays
CD45.1 mice were lethally irradiated with 103 cGy using a cesium source. To compare WT and CCR7−/− HSC reconstitution rates after HSCT, WT CD45.1–recipient mice were reconstituted with 3.0 × 102 CD45.2 WT or 3.0 × 102 CCR7−/− HSCs, in combination with 3.0 × 102 CD45.1 WT HSCs, 104 WT CD45.1 CMPs, and 104 WT CD45.1 GMPs. The spleen and lung were analyzed 14 days after transplantation.
IA after HSCT
WT mice were irradiated with 103 cGy using a cesium source. Each recipient mouse received 6.0 × 102 HSCs with 104 CMPs and 104 GMPs within 6 hours of irradiation via tail vein injection. Fourteen days after HSCT, mice were anesthetized and given an intratracheal injection of 2.0 × 106A fumigatus conidia suspended in 0.1% Tween 80 in PBS. A fumigatus strain 13 073 (ATCC) was used to elicit a reproducible form of invasive aspergillosis after HSCT. In some experiments, mice were given an intraperitoneal injection of 100 μg of anti–Gr-1, depleting neutrophils 24 hours before fungal infection as previously described.26
Lung histology
Lungs were collected 2 days after intratracheal conidia challenge in WT or CCR7−/−→WT chimeras. Lungs were perfused with 10% formalin, and routine histologic techniques were used to paraffin-embed the tissue. Lung sections were stained with hematoxylin and eosin (H&E) or with Gomori methanamine silver (GMS) stain to visualize A fumigatus conidia and hyphal elements (stained black). An Olympus BX40F microscope was used to capture digital images. Digital photographs were obtained and acquired with a Sony 3 charge-coupled device color video camera (DXC-960MD) and IP Lab Spectrum 3.6.4 software (MacOS 9.2.2; Scanalytics), respectively.
RNA and protein analysis of lung cytokines
RNA was isolated from homogenized lungs with Trizol reagent (Invitrogen). Approximately 5 μg of RNA was reverse transcribed to yield cDNA. Gene expression was analyzed by real-time polymerase chain reaction (RT-PCR) using an ABI Prism 7500 Sequence Detection System (Applied Biosystems). Glyceraldehyde 3-phosphate dehydrogenase (GAPDH) was analyzed as an internal control, and gene expression was normalized to GAPDH. Fold changes in gene-expression levels were calculated by comparison of the gene expression in unchallenged samples or mice, which were assigned an arbitrary value of 1. Whole-lung cytokine levels were measured using a Bioplex assay purchased from BioRad and analyzed on the BioRad Bioplex 200 system according to the manufacturer's protocol.
Flow cytometry
Whole-lung samples were minced and incubated in RPMI 1640 supplemented with 5% FCS, type IV collagenase (Sigma-Aldrich), and DNAse for 45 minutes. Cells were flushed through a nylon mesh filter and washed with fluorescence-activated cell sorting (FACS) buffer consisting of Ca2+ and Mg2+ free PBS with 0.1% azide, 1% bovine serum albumin (BSA), and 5mM EDTA (ethylenediaminetetraacetic acid) as previously described.27 Nonspecific antibody binding was blocked by incubating cells with purified rat anti–mouse CD16/CD32 monoclonal antibody (eBiosciences). Flow cytometric analysis was performed with a BD LSR II and analyzed using FlowJo software 8.8.3 (MacOS 10.5).
Statistical analysis
All results were expressed as the mean ± standard error of the mean and are representative of 2 or more experiments; the number of mice is indicated in the figure legend, where appropriate. A Student t test or analysis of variance was used to determine statistical significance between WT and CCR7−/− mice. Survival rates were expressed as percentages, and a log-rank test (χ2 test) was used to detect differences in mouse survival. P values of < .05 were considered statistically significant.
Results
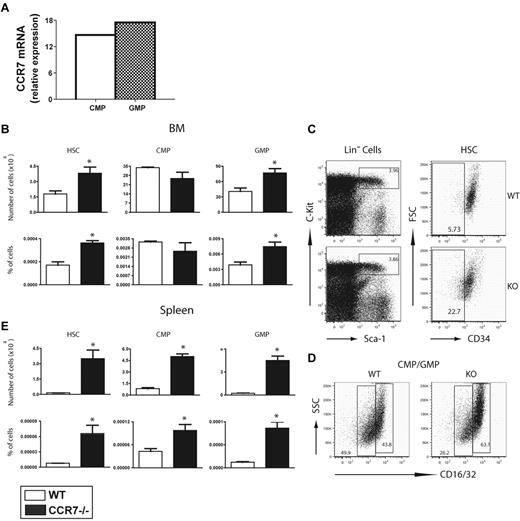
CCR7−/− mice show increased numbers of HSCs and GMPs in BM and spleen
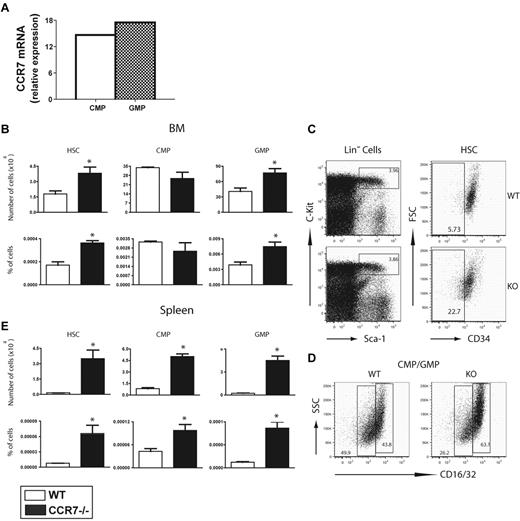
Previous studies have shown that CCL19 and CCL21 inhibit the proliferation of MPCs in vitro.22,28 In addition, our laboratory and others have detected CCR7 gene transcripts in HSCs, CMPs, and GMPs (Figure 1A).29 To examine the effect of CCR7 deficiency in the BM compartment, whole BM from CCR7−/− mice was analyzed to determine HSC, CMP, and GMP cell populations in these animals. HSCs were defined using 2 distinct sets of surface markers: Lin−, c-Kit+, Sca-1+, and CD34− (Figure 1B-C) and Lin−, c-Kit+, Sca-1+, CD150+, and CD48− (supplemental Figure 1, available on the Blood Web site; see the Supplemental Materials link at the top of the online article). Both of these cell populations have been shown to be highly enriched for HSCs.30,31 There was an approximate 2-fold increase in the number of BM HSCs in CCR7−/− mice, compared with WT mice (Figure 1B-C). The markers, Lin−, c-Kit+, Sca-1−, CD34+, and CD16/32lo (CMP) or CD16/32hi (GMP), defined MPCs. Significantly higher numbers of GMPs were detected in the BM of CCR7−/− mice, indicating that, along with HSCs, GMPs were either retained in the BM compartment, had enhanced self-renewal, or, in the case of GMPs, had an accelerated development from CMPs in CCR7−/− animals (Figure 1B,D). When the spleens of WT and CCR7−/− mice were analyzed for the presence of HSCs and MPCs, CCR7−/− mice had significantly higher numbers and percentages of HSCs, CMPs, and GMPs, compared with WT mice (Figure 1E). Together, these results demonstrate that CCR7−/− mice have increased numbers of BM and peripheral HSCs and GMPs, compared with WT mice.
CCR7−/− mice have increased numbers of HSCs and GMPs compared with WT controls. (A) CCR7 gene expression from FACS-sorted WT CMPs and GMPs were analyzed by real-time PCR (values represent CCR7 amplification cycle, compared with GAPDH). (B-E) Markers for HSCs were lineage−, c-Kit+, Sca-1+, and CD34−. CMPs were lineage−, c-Kit+, Sca-1−, CD34+, and CD16/32 low. GMPs were identical to CMPs, but were CD16/32 high. (B) HSC, CMP, and GMP numbers and percentages from BM of naïve WT and CCR7−/− mice. (C) Flow cytometric plots of lineage− BM from naïve WT and CCR7−/− mice. C-Kit+, Sca-1+, and lineage− cells (left graphs) were analyzed for the expression of CD34 (right graphs). (D) Flow cytometric plots of total MPCs show similar percentages between WT and CCR7−/− mice, but differences in the percentages of CMPs and GMPs. (E) HSC, CMP, and GMP numbers and percentages from the spleens of naïve WT and CCR7−/− mice (n = 3-5 mice per group, representative of more than 5 experiments). *P < .05, when comparing WT and CCR7−/− HSCs and MCPs.
CCR7−/− mice have increased numbers of HSCs and GMPs compared with WT controls. (A) CCR7 gene expression from FACS-sorted WT CMPs and GMPs were analyzed by real-time PCR (values represent CCR7 amplification cycle, compared with GAPDH). (B-E) Markers for HSCs were lineage−, c-Kit+, Sca-1+, and CD34−. CMPs were lineage−, c-Kit+, Sca-1−, CD34+, and CD16/32 low. GMPs were identical to CMPs, but were CD16/32 high. (B) HSC, CMP, and GMP numbers and percentages from BM of naïve WT and CCR7−/− mice. (C) Flow cytometric plots of lineage− BM from naïve WT and CCR7−/− mice. C-Kit+, Sca-1+, and lineage− cells (left graphs) were analyzed for the expression of CD34 (right graphs). (D) Flow cytometric plots of total MPCs show similar percentages between WT and CCR7−/− mice, but differences in the percentages of CMPs and GMPs. (E) HSC, CMP, and GMP numbers and percentages from the spleens of naïve WT and CCR7−/− mice (n = 3-5 mice per group, representative of more than 5 experiments). *P < .05, when comparing WT and CCR7−/− HSCs and MCPs.
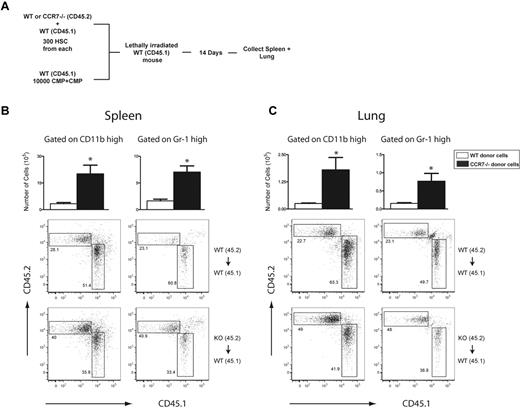
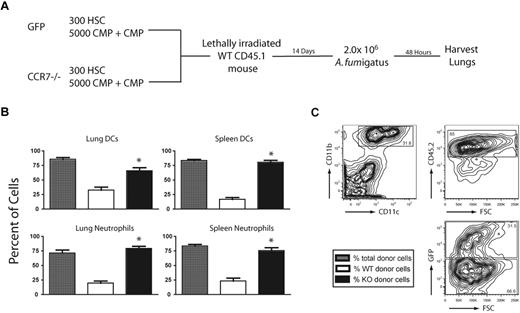
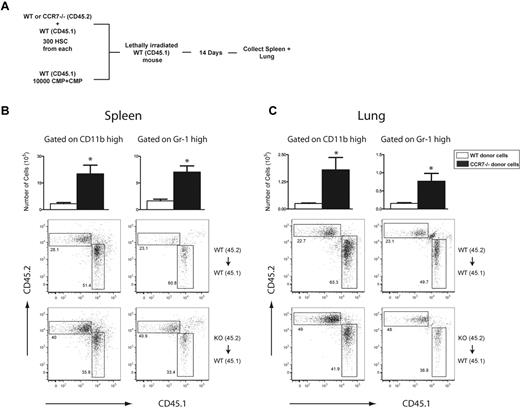
CCR7−/− HSCs repopulate the myeloid compartment more rapidly than WT cells at 14 days after HSCT: MPC inclusion is required for this rapid repopulation
The next series of experiments were directed at determining the engraftment efficiency of HSCs and MPCs from WT or CCR7−/− mice at 2 weeks after HSCT. Our motivation to examine this stemmed from studies by Brown and colleagues,15,16 in which these investigators clearly demonstrated that the inclusion of MPCs (both CMPs and GMPs) with HSCs during HSCT promoted the rapid appearance of myeloid cells necessary to protect these mice from microbial or fungal infection, while the transplant of HSCs alone required a considerably longer time to repopulate the myeloid populations necessary for the same degree of protection from infection. However, these previous studies did not address whether the included MPCs directly contributed to the increased myeloid cell populations observed after HSCT. Consequently, we next examined the engraftment efficiencies of WT and CCR7−/− HSCs and MPCs at 2 weeks after HSCT in mixed chimeras using a competitive reconstitution assay. The effects of CCR7 deficiency on HSC reconstitution of myeloid cells was examined using lethally irradiated WT CD45.1 mice, which were reconstituted with 3.0 × 102 HSCs from WT CD45.2 or CCR7−/− CD45.2 mice and cotransplanted with 3.0 × 102 HSCs and 1.0 × 104 CMP/GMPs from WT CD45.1 mice (Figure 2A). Overall, these experiments showed that CCR7−/− HSCs were able to reconstitute myeloid effector cells more effectively then WT HSCs after HSCT. Accordingly, the total number of cells in the spleen and lungs originating from CCR7−/− HSCs was significantly greater than the number of cells originating from WT HSCs (Figure 2B-C). Similar to these data, the percentage of myeloid cells in the spleen and lungs originating from CCR7−/− HSCs were significantly greater than the percentage of cells derived from WT HSCs. We next examined the impact of MPC reconstitution on the percentage of myeloid cells in lethally irradiated WT CD45.1 mice, which were intravenously injected with 6.0 × 102 HSCs from WT CD45.1 donors and 103 CMP/GMPs from either WT CD45.2 or CCR7−/− CD45.2 mice (supplemental Figure 2). A comparison of WT and CCR7−/− MPC reconstitution revealed that cells originating from CCR7−/− MPCs were no longer present in the lung or spleen 14 days after HSCT, while cells originating from WT MPCs were present, albeit at very low frequency (supplemental Figure 2). Interestingly, there was no significant difference in the numbers of CD11bhi or Gr-1hi cells in the lungs or spleens of mice receiving WT or CCR7−/− MPCs. Together, these data demonstrate that CCR7−/− HSCs more rapidly repopulate the myeloid compartment, compared with WT HSCs, after transplantation. In addition, the inclusion of either WT or CCR7−/− MPCs clearly enhanced myeloid reconstitution after HSCT, but these cells appeared to be a minor direct source of myeloid cells at day 14 after HSCT.
CCR7−/− HSCs demonstrate enhanced myeloid reconstitution after HSCT. (A) Experimental scheme of a competitive reconstitution assay in which WT CD45.1 mice were lethally irradiated and reconstituted with 3.0 × 102 HSCs from WT CD45.1 and 3.0 × 102 HSCs from either WT (CD45.2) or CCR7−/− (CD45.2) mice, and 1.0 × 104 CMPs and GMPs from CD45.1 WT mice. Fourteen days after HSCT, flow cytometric analysis revealed a significant increase in the percentage and total number of spleen and lung cells derived from CCR7−/− HSCs, compared with WT HSCs. (B) Total number of cells and flow cytometric analysis of CD11bhi and Gr-1hi cells in the spleen 14 days after competitive transplantation. (C) Total number of cells and flow cytometric analysis of CD11bhi and Gr-1hi cells in the lung 14 days after competitive transplantation (n = 5 mice per group). *P < .05, when comparing cells originating from either WT or CCR7−/− HSCs.
CCR7−/− HSCs demonstrate enhanced myeloid reconstitution after HSCT. (A) Experimental scheme of a competitive reconstitution assay in which WT CD45.1 mice were lethally irradiated and reconstituted with 3.0 × 102 HSCs from WT CD45.1 and 3.0 × 102 HSCs from either WT (CD45.2) or CCR7−/− (CD45.2) mice, and 1.0 × 104 CMPs and GMPs from CD45.1 WT mice. Fourteen days after HSCT, flow cytometric analysis revealed a significant increase in the percentage and total number of spleen and lung cells derived from CCR7−/− HSCs, compared with WT HSCs. (B) Total number of cells and flow cytometric analysis of CD11bhi and Gr-1hi cells in the spleen 14 days after competitive transplantation. (C) Total number of cells and flow cytometric analysis of CD11bhi and Gr-1hi cells in the lung 14 days after competitive transplantation (n = 5 mice per group). *P < .05, when comparing cells originating from either WT or CCR7−/− HSCs.
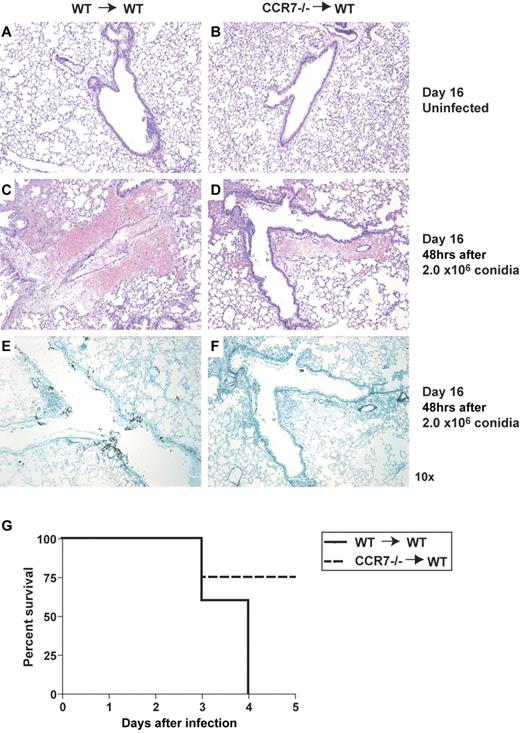
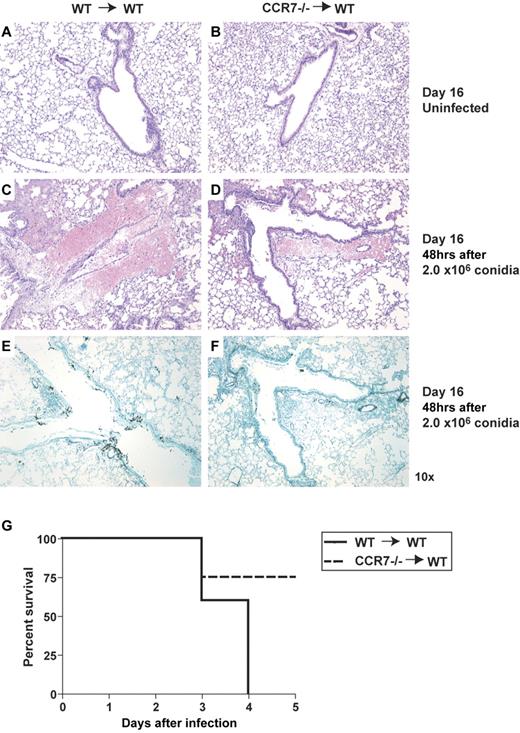
CCR7 deficiency on hematopoietic cells is protective during IA after HSCT
In mice, the most prominent period of susceptibility to IA occurs during the first few weeks after HSCT, and this is the result of severe leukopenia during this time. Chemical- or antibody-induced immunosuppression is necessary after leukocyte numbers have been restored in HSCT-transplanted mice to render WT mice susceptible to IA.15,32 In the present study, our interest was directed toward the identification of BM transplant approach that decreased the duration of leukopenia, thereby enhancing resistance to infection by Aspergillus. Our model involved the lethal irradiation of WT recipient mice before their reconstitution with HSCs, CMPs, and GMPs from WT or CCR7−/− mice. Fourteen days after transplant, mice were given an intratracheal injection of A fumigatus. To confirm that a combined HSC and MPC transplant was necessary to enhance myeloid reconstitution and protection from aspergillosis at day 14 after transplant, we examined whether a HSC transplant alone led to increased leukocyte numbers in the lung and protection from IA. At day 2 after IA, total cell numbers in irradiated WT mice that received 6 × 102 WT HSCs alone were significantly decreased by 19%, compared with the lung cell numbers detected after a combined transplant of WT HSCs and MPCs (data not shown; subsequently referred to as: WT→WT). In addition, total cell numbers in irradiated WT mice that received 6 × 102 CCR7−/− HSCs alone were significantly decreased by 51%, compared with the lung cell numbers detected after a combined transplant of CCR7−/− HSCs and MPCs (data not shown; subsequently referred to as: CCR7−/−→WT). Importantly, in both HSC-alone transplant groups, all populations of myeloid effector cells, including neutrophils and DCs, were decreased in the lung and spleen, and these mice were significantly more susceptible to IA, compared with the combined HSC and MPC transplant groups (not shown). Consequently, all remaining studies addressed the importance of CCR7 expression on the combination of HSCs and MPCs during experimental HSCT and subsequent Aspergillus challenge. Mice were either followed for survival or were euthanized 48 hours after fungal challenge for histologic analysis. Notably absent from the lungs of uninfected CCR7−/−→WT chimeric mice were lymphoid aggregates typically observed in histologic sections from naïve CCR7−/− mice33 (Figure 3A-B). H&E staining of histologic sections from both groups of infected mice revealed significant cellular infiltration into the lungs, but the inflammatory response appeared to be more prominent in WT→WT chimeras (Figure 3C-D). Lastly, using GMS staining, WT→WT chimeras were found to exhibit extensive fungal growth, which was mostly absent from the lungs of CCR7−/−→WT chimeras (Figure 3E-F). Consistent with these histologic data, WT mice reconstituted with CCR7−/− HSCs and MPCs had a dramatically higher survival rate than did WT mice reconstituted with WT HSCs and MPCs (Figure 3G). Previous reports have suggested that the protective effect provided by MPC inclusion during HSCT was due to a decreased period of neutropenia and overall neutrophil expansion.15 Neutrophil depletion in both WT or CCR7−/−→WT chimeras after HSCT revealed that CCR7−/−→WT chimeras were more efficient at clearing A fumigatus, compared with WT→WT chimeras, indicating that the increased fungal clearance in CCR7−/−→WT chimeras was not solely dependent on neutrophil numbers or recruitment (supplemental Figure 3A-D). Thus, these results indicate that CCR7 expression on hematopoietic cells appears to impair antifungal immunity due to its restraint on myeloid cell expansion after HSCT.
WT mice receiving CCR7−/− combined HSC and MPC HSCT (CCR7−/−→WT) have decreased fungal burden and increased survival, compared with WT mice receiving a WT-combined HSC and MPC HSCT (WT→WT). Lethally irradiated WT mice were reconstituted with 6.0 × 102 HSCs, 1.0 × 104 CMPs, and 1.0 × 104 GMPs from either WT or CCR7−/− mice 14 days before an intratracheal challenge with 2.0 × 106 conidia. Mice were followed for survival or harvested at 48 hours after fungal challenge. (A-F) Histologic analysis of lung tissue 2 days after conidia challenge. H&E staining of uninfected lungs (A-B) or 48 hours after conidia challenge (C-D). (E-F) Representative GMS-stained sections from WT (E) or CCR7−/− (F) mice after conidial challenge; fungal elements are stained in black. Original magnification was 10× for all sections. (G) Survival of WT mice receiving WT or CCR7−/− HSCs and MPCs (n = 4-5 mice per group, representative of 2 experiments).
WT mice receiving CCR7−/− combined HSC and MPC HSCT (CCR7−/−→WT) have decreased fungal burden and increased survival, compared with WT mice receiving a WT-combined HSC and MPC HSCT (WT→WT). Lethally irradiated WT mice were reconstituted with 6.0 × 102 HSCs, 1.0 × 104 CMPs, and 1.0 × 104 GMPs from either WT or CCR7−/− mice 14 days before an intratracheal challenge with 2.0 × 106 conidia. Mice were followed for survival or harvested at 48 hours after fungal challenge. (A-F) Histologic analysis of lung tissue 2 days after conidia challenge. H&E staining of uninfected lungs (A-B) or 48 hours after conidia challenge (C-D). (E-F) Representative GMS-stained sections from WT (E) or CCR7−/− (F) mice after conidial challenge; fungal elements are stained in black. Original magnification was 10× for all sections. (G) Survival of WT mice receiving WT or CCR7−/− HSCs and MPCs (n = 4-5 mice per group, representative of 2 experiments).
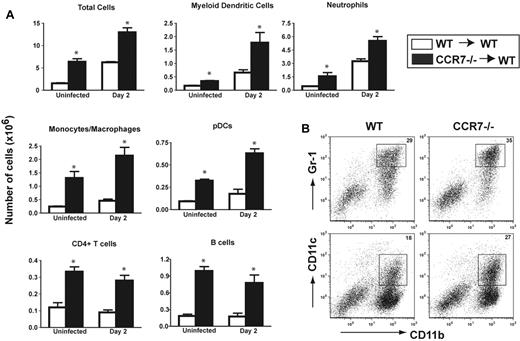
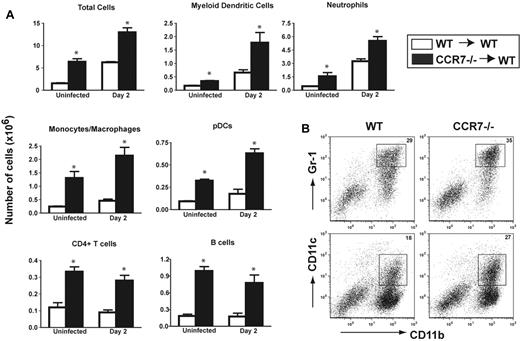
Lung leukocyte recruitment is enhanced in CCR7−/−→WT chimeras during IA
Neutropenia and other immune cell deficiencies have been linked to the development of IA after HSCT. Complete engraftment and rapid proliferation of donor cells after HSCT is necessary to reduce this period of immunodeficiency and provide protection against opportunistic infections. To determine which cell types might be providing a protective effect in the lungs of CCR7−/−→WT chimeras, we used flow cytometry to analyze immune cell subsets in chimeric mice both before and after challenge with A fumigatus. Uninfected CCR7−/−→WT chimeras had significantly higher myeloid cell numbers in the lung, and this result was recapitulated in every cell population examined (Figure 4A). In addition, 48 hours after A fumigatus infection, effector cell numbers were elevated in both WT and CCR7−/−→WT chimeras, but again, cell numbers were statistically higher in the lungs of CCR7−/−→WT chimeras, compared with WT→WT chimeras (Figure 4A). Of importance to the host immune response during IA, the numbers and percentages of neutrophils, monocytes/macrophages, and DCs were all significantly higher in the CCR7−/−→WT chimeras, compared with uninfected and infected WT→WT chimeras (Figure 4A-B). When the cellular composition of the lungs of neutrophil-depleted WT and CCR7−/− chimeric mice was examined during IA, we found that the total number of cells remained greater in the CCR7−/−→WT chimeras, compared with the WT group (supplemental Figure 3E). In addition, significantly increased numbers of DCs and monocytes/macrophages were present in lung samples from the CCR7−/−→WT chimeras, compared with the WT group. These data indicate that the enhanced antifungal protection observed in CCR7−/−→WT chimeras is a consequence of an overall increase in myeloid effector cell recruitment into the lung before and after fungal infection. Neutrophils were more abundant in the CCR7−/−→WT chimeras, but the presence of other myeloid effector cells appeared to compensate for their absence after depletion. Together, these data suggested that the enhanced immune response elicited in CCR7−/−→WT was due to the enhanced recruitment of effector myeloid cells, which appeared to rapidly clear Aspergillus from the lungs of these transplanted mice.
Lethally irradiated WT mice reconstituted with CCR7−/− HSCs and MPCs (CCR7−/−→WT) show increased leukocyte influx into the lungs before and after A fumigatus challenge, compared with WT→WT chimeras. Fourteen days after HSCT, mice were left unchallenged or were injected with 2.0 × 106 conidia. Cellular infiltration into the lung was analyzed 48 hours after challenge. (A) Myeloid DCs were CD11c high, CD11b high, and MHC II+ cells. Neutrophils were CD11b high, Gr-1 high, and CD11c−. Monocytes/macrophages were CD11b+, F4/80+, and CD11c−. Plasmacytoid DCs were B220+ and CD11c+, CD4+ T cells were CD3+ and CD4+, and B cells were B220+ and CD11c−. (B) Dot plots of DCs and neutrophils demonstrate increased percentages of myeloid effector cells during IA (n = 4-5 mice per group. Data are representative of 3 separate experiments). *P < .05, when comparing WT or CCR7−/−→WT chimeric mice.
Lethally irradiated WT mice reconstituted with CCR7−/− HSCs and MPCs (CCR7−/−→WT) show increased leukocyte influx into the lungs before and after A fumigatus challenge, compared with WT→WT chimeras. Fourteen days after HSCT, mice were left unchallenged or were injected with 2.0 × 106 conidia. Cellular infiltration into the lung was analyzed 48 hours after challenge. (A) Myeloid DCs were CD11c high, CD11b high, and MHC II+ cells. Neutrophils were CD11b high, Gr-1 high, and CD11c−. Monocytes/macrophages were CD11b+, F4/80+, and CD11c−. Plasmacytoid DCs were B220+ and CD11c+, CD4+ T cells were CD3+ and CD4+, and B cells were B220+ and CD11c−. (B) Dot plots of DCs and neutrophils demonstrate increased percentages of myeloid effector cells during IA (n = 4-5 mice per group. Data are representative of 3 separate experiments). *P < .05, when comparing WT or CCR7−/−→WT chimeric mice.
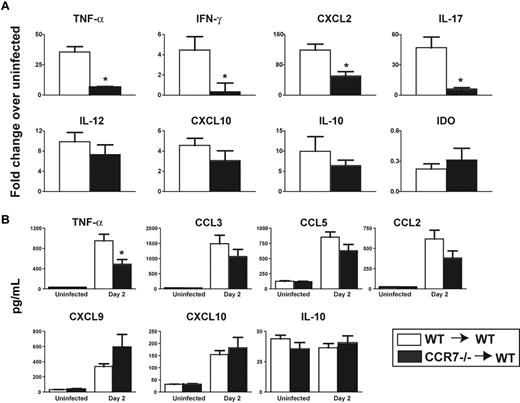
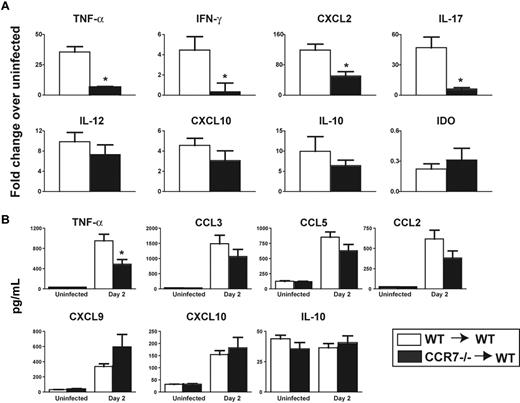
CCR7−/−→WT chimeras exhibit a modulated inflammatory response after A fumigatus challenge
Proinflammatory cytokines and chemokines are required for an appropriate antifungal immune response in the lung. However, it has recently been reported that uncontrolled inflammation inhibits fungal clearance and enhances morbidity and mortality during experimental IA.34,35 RNA analysis showed that WT→WT chimeras had significantly higher expression of tumor necrosis factor-α (TNF-α), interferon-γ, and CXCL2 and higher levels of CXCL10 and IL-12, compared with CCR7−/−→WT chimeras (Figure 5A). Levels of the anti-inflammatory mediators, indoleamine 2,3 dioxygenase (IDO) and IL-10, were similar between WT and CCR7−/−→WT chimeras. Analysis of whole-lung protein samples from WT and CCR7−/− chimeric mice demonstrated that CCR7−/−→WT chimeras had lower levels of the proinflammatory cytokines, TNF-α, CCL2, CCL5, and CCL3, but higher levels of CXCL10 and CXCL9 (Figure 5B). Both groups of chimeras had similar levels of the anti-inflammatory cytokine, IL-10. These results suggest that CCR7−/−→WT chimeric mice are able to modulate the inflammatory response to favor the efficient clearance of A fumigatus from the lung.
CCR7−/−→WT chimeras have decreased proinflammatory cytokine levels 48 hours after conidial challenge compared with WT→WT chimeras. Lethally irradiated WT mice reconstituted with WT or CCR7−/− HSCs and MPCs were infected with 2.0 × 106 conidia 14 days after HSCT and analyzed 48 hours later. (A) RNA levels were determined by real-time PCR. Values represent the fold change of infected mice, compared with uninfected mice 16 days after HSCT. (B) Cytokine and chemokine levels were determined using a Bioplex multiplex assay; all values are represented as picograms per milliliter (n = 4 mice per uninfected group; 8 mice per conidia-challenged group). *P < .05, when comparing WT and CCR7−/−→WT chimeras after conidia challenge.
CCR7−/−→WT chimeras have decreased proinflammatory cytokine levels 48 hours after conidial challenge compared with WT→WT chimeras. Lethally irradiated WT mice reconstituted with WT or CCR7−/− HSCs and MPCs were infected with 2.0 × 106 conidia 14 days after HSCT and analyzed 48 hours later. (A) RNA levels were determined by real-time PCR. Values represent the fold change of infected mice, compared with uninfected mice 16 days after HSCT. (B) Cytokine and chemokine levels were determined using a Bioplex multiplex assay; all values are represented as picograms per milliliter (n = 4 mice per uninfected group; 8 mice per conidia-challenged group). *P < .05, when comparing WT and CCR7−/−→WT chimeras after conidia challenge.
After HSCT, CCR7−/− HSCs and MPCs demonstrate enhanced hematopoiesis and chimerism during IA
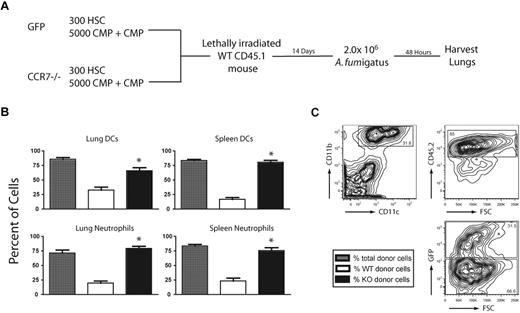
To further evaluate the differences in myeloid reconstitution between WT and CCR7−/− HSCs and MPCs during IA, mixed chimeras were generated by combining 3.0 × 102 HSCs, 5.0 × 103 CMPs, and 5.0 × 103 GMPs from green fluorescent protein (GFP)–expressing WT mice, with an equal number of the same cells from CCR7−/− mice. Recipient mice, expressing CD45.1, were congenic to the donor mice, which expressed CD45.2. This cell transfer approach allowed for the examination of donor cells and distinguished between WT and CCR7−/− cells during IA (Figure 6A). Lungs and spleens of infected mice were analyzed, and it was observed that donor chimerism was greater than 75% in both organs (Figure 6B). Interestingly, the percentage of donor neutrophils and DCs originating from CCR7−/− mice was significantly greater in these organs than the percentage of cells from WT GFP mice. In the lung, 75% of DCs were of donor origin, and of these cells, CCR7−/− DCs were 2-fold more prevalent than WT GFP-expressing DCs (Figure 6C). These data demonstrate that the transplantation of CCR7−/− HSCs and MPCs accelerated myeloid reconstitution, and this contributed to superior chimerism and a significantly enhanced number of effector cells, compared with a WT HSC and MPC transplant.
CCR7−/− HSCs and MPCs exhibit enhanced myeloid reconstitution, compared with WT cells during IA after a competitive reconstitution transplantation. (A) Experimental scheme in which WT CD45.1 mice were lethally irradiated and reconstituted with 3.0 × 102 HSCs, 5.0 × 103 CMPs, and 5.0 × 103 GMPs from CD45.2 WT GFP+ and CCR7−/− mice. Fourteen days after HSCT, mice were challenged with 2.0 × 106 conidia and cells were analyzed by flow cytometry 48 hours later. (B) Percent of total, (WT and CCR7−/−) donor neutrophils or DCs in the lungs of chimeric mice after conidial challenge (gray bars) and the percentage of donor cells derived from WT or CCR7−/− mice (white and black bars, respectively). (C) Contour plots showing donor-derived DCs from WT GFP+ or CCR7−/− mice (n = 5 mice, representative of 2 experiments). *P < .05, when comparing GFP+ and CCR7−/− donor cells after HSCT.
CCR7−/− HSCs and MPCs exhibit enhanced myeloid reconstitution, compared with WT cells during IA after a competitive reconstitution transplantation. (A) Experimental scheme in which WT CD45.1 mice were lethally irradiated and reconstituted with 3.0 × 102 HSCs, 5.0 × 103 CMPs, and 5.0 × 103 GMPs from CD45.2 WT GFP+ and CCR7−/− mice. Fourteen days after HSCT, mice were challenged with 2.0 × 106 conidia and cells were analyzed by flow cytometry 48 hours later. (B) Percent of total, (WT and CCR7−/−) donor neutrophils or DCs in the lungs of chimeric mice after conidial challenge (gray bars) and the percentage of donor cells derived from WT or CCR7−/− mice (white and black bars, respectively). (C) Contour plots showing donor-derived DCs from WT GFP+ or CCR7−/− mice (n = 5 mice, representative of 2 experiments). *P < .05, when comparing GFP+ and CCR7−/− donor cells after HSCT.
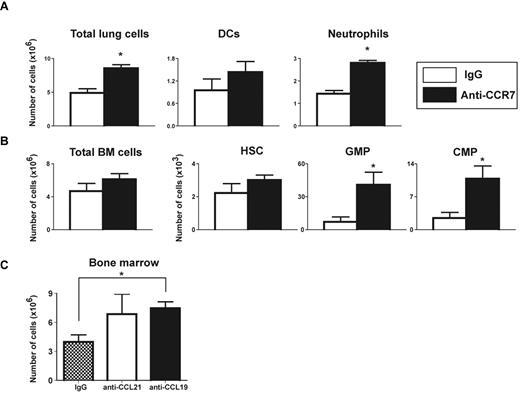
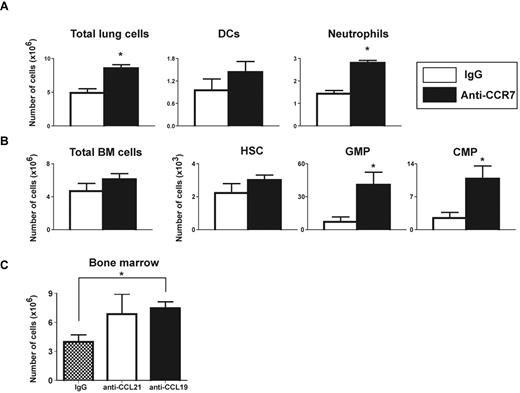
Antibody-mediated neutralization of CCR7 enhances immune reconstitution and protects mice from IA
Naive CCR7−/− mice develop immune abnormalities with age, most notably the development of autoimmunity, which is partially a result of improper regulatory T-cell function and trafficking.36,37 To address whether our prior results were a consequence of this abnormal immune response in CCR7-deficient mice, WT chimeric mice were treated with either anti-CCR7 antibody or control IgG every other day for 14 days after HSCT. Upon challenge with A fumigatus, mice treated with anti-CCR7 antibody demonstrated increased numbers of effector cells in the lung, similar to that observed in CCR7−/−→WT chimeras (Figure 7A). In addition, CMP and GMP numbers were significantly increased in mice receiving anti-CCR7 antibody therapy, although HSC numbers were comparable to control mice (Figure 7B). To examine whether the hematopoietic expansion after the blockade of CCR7 was related to one of its ligands, WT mice received WT HSCs and MPCs and were treated with IgG or anti-CCL19 or anti-CCL21 antibodies every other day for 14 days. Mice treated with anti-CCL19 antibody exhibited a significantly greater hematopoietic cell expansion in the BM compartment, compared with IgG-treated mice (Figure 7C). Together, these results demonstrate that blocking CCR7 or its ligands recapitulates the results observed using CCR7−/− HSCs and MPCs for HSCT and, again, confirms a previously unknown regulatory role for CCR7 in HSCT.
Anti-CCR7 and -CCL19 monoclonal antibodies enhance HSC and MPC proliferation after HSCT and Aspergillus challenge. Lethally irradiated WT mice reconstituted with 6.0 × 102 HSCs, 1.0 × 104 CMPs, and 1.0 × 104 GMPs from WT mice were given an intraperitoneal injection of 25 μg of anti-CCR7 (A-B), anti-CCL19 (C), or IgG (A-C) every other day for 14 days after HSCT. (A-B) Fourteen days after HSCT and anti-CCR7 treatment, mice were challenged with 2.0 × 106 conidia. Lungs (A) and BM (B) were analyzed 48 hours after infection. (C) The number of cells present in the BM of uninfected HSCT mice treated with anti-CCL19 or -CCL21 (n = 4-5 mice per group, representative of 2 experiments). *P < .05, when comparing anti-CCR7 or -CCL19 and IgG-treated chimeras.
Anti-CCR7 and -CCL19 monoclonal antibodies enhance HSC and MPC proliferation after HSCT and Aspergillus challenge. Lethally irradiated WT mice reconstituted with 6.0 × 102 HSCs, 1.0 × 104 CMPs, and 1.0 × 104 GMPs from WT mice were given an intraperitoneal injection of 25 μg of anti-CCR7 (A-B), anti-CCL19 (C), or IgG (A-C) every other day for 14 days after HSCT. (A-B) Fourteen days after HSCT and anti-CCR7 treatment, mice were challenged with 2.0 × 106 conidia. Lungs (A) and BM (B) were analyzed 48 hours after infection. (C) The number of cells present in the BM of uninfected HSCT mice treated with anti-CCL19 or -CCL21 (n = 4-5 mice per group, representative of 2 experiments). *P < .05, when comparing anti-CCR7 or -CCL19 and IgG-treated chimeras.
Discussion
The present study demonstrated a unique role for CCR7 after HSCT and during IA in a murine model. HSCT patients and other immunocompromised individuals are highly susceptible to opportunistic infections, especially A fumigatus, which can cause a serious, acute disease known as IA. A fumigatus is normally cleared from the body by effector cells of the innate immune system, including neutrophils, macrophages, monocytes, and DCs. However, elimination of these cell types during the pretransplantation myeloablative conditioning stage of HSCT renders the host highly susceptible to infection. Thus, one goal of HSCT clinical research has been to enhance the engraftment and immune reconstitution of hematopoietic cells to restore a functional immune system within the patient.38,39
Examination of the BM and spleen of CCR7−/− mice revealed a significant increase in the numbers and percentages of HSCs and GMPs in these mice, compared with WT mice. In addition, when equivalent numbers of WT and CCR7−/− HSCs and MPCs were used to reconstitute lethally irradiated WT mice, the number of myeloid cells originating from CCR7-deficient HSCs was significantly greater than the number of myeloid cells derived from WT HSCs. An in-depth analysis of the spleen and lung revealed that MPCs were not the primary source of myeloid cells 14 days after HSCT. Two weeks after HSCT, only a small percentage of neutrophils and DCs were detected that were of WT MPC origin, with still fewer cells originating from CCR7−/− MPCs (supplemental Figure 3). The lack of cells originating from CCR7−/− MPCs suggests that these cells might have rapidly differentiated into myeloid cells after transplant and were subsequently removed through homeostatic processes. Although myeloid cells originating from CCR7−/− MPCs were largely absent 2 weeks after transplant, additional studies indicated that these cells had a critical role in enhancing CCR7−/− HSC myeloid reconstitution after HSCT and were needed for the enhanced antifungal effect observed in WT mice that received a CCR7−/− HSC and MPC transplant.
In addition to enhancing HSC myeloid reconstitution, CCR7 deficiency provided protection during a murine model of IA after HSCT. When CCR7−/−→WT chimeric mice were challenged with A fumigatus, they showed a significantly reduced fungal burden 48 hours after infection. Lung histology revealed little fungal growth, as determined by GMS staining, in CCR7−/−→WT chimeras, whereas significant hyphal growth and invasion into lung airways was observed in WT→WT chimeras 2 days after fungal challenge. Flow cytometric data showed that there were significantly more cells present in the lungs of CCR7−/−→WT chimeras, compared with WT chimeras. The resultant increase in total lung cells in both uninfected and infected chimeric mice indicates that HSCs and MPCs from CCR7−/− mice demonstrate enhanced myeloid reconstitution, compared with WT cells. Indeed, CCR7−/−→WT chimeras exhibited a greater number of effector cells, including DCs, neutrophils, and macrophages, in the lung before and during fungal challenge. The present study is consistent with our previous studies in which CCR7 deficiency enhanced DC retention in the lung during IA, providing a protective antifungal effect.32
The production of proinflammatory cytokines and chemokines required for antifungal immune responses has been well documented. One study found that neutralizing TNF-α led to rapid mortality in a murine model of IA.40 However, recent reports suggest that a hyperinflammatory state results in decreased fungal clearance and enhanced mortality during IA.34,35 These contrasting findings suggest that while inflammation is required for the clearance of A fumigatus, an effective antifungal response also requires the appropriate regulation of cytokine production. Our results showed that while there was a significant increase in proinflammatory cytokine production during Aspergillus challenge in both groups of chimeras, cytokine levels were significantly higher in the WT, compared with the CCR7−/−, chimeras. The anti-inflammatory mediators, IDO and IL-10, were at similar levels in both groups of mice. Although it is not immediately clear why CXCL10 and CXCL9 were increased in the CCR7−/− chimeric mice, it has been reported that high levels of CXCL10 correlate with decreased susceptibility to IA.41 Thus, the balance of pro- and anti-inflammatory mediators produced in the CCR7−/−→WT chimeras after infection appears to enhance fungal clearance.
When using CCR7−/− mice for this model system, it was important to consider that previous studies have demonstrated the development of systemic autoimmunity with time in CCR7−/− mice.36 To address the concern that the protective phenotype provided by CCR7−/− HSCs and MPCs might be a consequence of autoimmune processes, WT→WT chimeras were treated with an anti-CCR7 monoclonal antibody for 14 days after HSCT. These antibody-treated mice exhibited a similar enhanced immune response during IA, whereas control IgG-treated mice were susceptible to IA. In this experiment, it was also evident that although HSC numbers were not altered between the 2 groups, there was a significant increase in the number of MPCs in the anti-CCR7–treated group. Together, these results indicate that inhibiting CCR7 via antibody blockade enhances engraftment and leads to increased effector cell numbers, resulting in enhanced immunity to A fumigatus.
Our current working model for the role of CCR7 during IA in mice after HSCT suggests that this chemokine receptor negatively regulates the HSC reconstitution of myeloid cells, resulting in a prolonged period of immunosuppression that leads to increased susceptibility to IA. Previous studies have shown that CCL19 and CCL21 inhibit the proliferation of human MPCs and chronic myelogenous leukemia progenitors in vitro.22,28 To test whether the addition of recombinant murine CCL19 or CCL21 had a similar effect on murine HSCs and MCPs, we cultured HSCs, CMPs, and GMPs for 7-14 days in the presence or absence of CCL19, CCL21, or both cytokines. There was no observable difference in colony formation when 20-50 ng/mL of the exogenous chemokine was added (data not shown). This result suggests that the antiproliferative effects of CCL19 and CCL21 might be occurring within the BM compartment, but not directly on the HSCs or MCPs in vitro. Although it is unclear how CCL19 and CCL21 are acting to suppress myeloid proliferation and expansion, our findings suggest that removal or inhibition of CCR7 on HSCs and MPCs increases the rate of hematopoiesis after HSCT.
IA is a serious, highly lethal disease affecting immunocompromised patients, particularly HSCT recipients. IA is very difficult to diagnose, and antifungal treatments remain highly cytotoxic. In this study, a novel, inhibitory role for the chemokine receptor CCR7 was identified. During IA, CCR7 additionally impacted myeloid reconstitution by HSCs with support by MPCs, which ultimately led to an inadequate immune response during IA. Thus, CCR7 represents a potential new target for the treatment of IA after HSCT.
An Inside Blood analysis of this article appears at the front of this issue.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: A.J.H. and L.E.K. performed all experiments and analyzed the results; C.M.H and A.J.H. wrote the manuscript; and A.J.H created the associated figures.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Cory M. Hogaboam PhD Professor, Department of Pathology, University of Michigan Medical School, Rm 4057, BSRB, 109 Zina Pitcher Pl, Ann Arbor, MI 48109-2200; hogaboam@med.umich.edu.