Abstract
We performed nonmyeloablative HSCT in 6 patients with a newly described genetic immunodeficiency syndrome caused by mutations in GATA2—a disease characterized by nontuberculous mycobacterial infection, monocytopenia, B- and NK-cell deficiency, and the propensity to transform to myelodysplastic syndrome/acute myelogenous leukemia. Two patients received peripheral blood stem cells (PBSCs) from matched-related donors, 2 received PBSCs from matched-unrelated donors, and 2 received stem cells from umbilical cord blood (UCB) donors. Recipients of matched-related and -unrelated donors received fludarabine and 200 cGy of total body irradiation (TBI); UCB recipients received cyclophosphamide in addition to fludarabine and TBI as conditioning. All patients received tacrolimus and sirolimus posttransplantation. Five patients were alive at a median follow-up of 17.4 months (range, 10-25). All patients achieved high levels of donor engraftment in the hematopoietic compartments that were deficient pretransplantation. Adverse events consisted of delayed engraftment in the recipient of a single UCB, GVHD in 4 patients, and immune-mediated pancytopenia and nephrotic syndrome in the recipient of a double UCB transplantation. Nonmyeloablative HSCT in GATA2 deficiency results in reconstitution of the severely deficient monocyte, B-cell, and NK-cell populations and reversal of the clinical phenotype. Registered at www.clinicaltrials.gov as NCT00923364.
Introduction
Recently, we and others have described a novel genetic immunodeficiency disease characterized by: (1) onset in late adolescence or early adulthood of disseminated nontuberculous mycobacterial infections (NTMs) and other opportunistic infections including disseminated human papillomavirus (HPV) and fungal infections; (2) peripheral blood flow cytometry with normal or slightly decreased T lymphocytes, but a severe deficiency of monocytes, B lymphocytes, and NK cells; (3) pulmonary alveolar proteinosis and pulmonary hypertension in approximately one-third of the patients; (4) propensity of the disease to progress to myelodysplastic syndrome (MDS)/acute myelogenous leukemia (AML); and (5) autosomal dominant inheritance in approximately one-half of patients.1,2 We have referred to this syndrome of monocytopenia and mycobacterial infections, typically Mycobacterium avium complex (MAC), as “MonoMAC.”3 We have recently shown that MonoMAC is because of mutations in GATA2, explaining the confluence of infection susceptibility and MDS/AML.4 Mutations in GATA2 were also reported as a cause of familial MDS/AML.5
Many primary immunodeficiency diseases are caused by intrinsic genetic defects of hematopoietic lineage-derived cells for which allogeneic HSCT represents an effective therapeutic approach.6 Because of the lethal nature of GATA2 deficiency,1 we sought to reconstitute the deficient hematopoietic compartments using allogeneic HSCT. We selected a nonmyeloablative-conditioning regimen because most GATA2-deficient patients had major underlying organ dysfunction and active infections at the time of transplantation, and because we anticipated that the immune deficiency in GATA2 deficiency would limit graft rejection. Here, we describe the outcomes of the first 6 patients who received allogeneic HSCT for this newly described genetic syndrome.
Methods
Study design and procedures
We conducted a phase 1-2 pilot study to determine the efficacy and safety of nonmyeloablative allogeneic HSCT for patients with GATA2 deficiency. The study was approved by the institutional review board of the National Cancer Institute, and was independently monitored for safety and data accuracy. Written informed consent and assent was obtained for all patients and donors in accordance with the Declaration of Helsinki.
Patients between 12 and 60 years of age were eligible if they met the following criteria: at least 2 episodes of life-threatening opportunistic infections (at least 1 infection should be a NTM infection); flow cytometry profile on peripheral blood demonstrating monocytopenia, CD19+ B-cell and CD3−CD56+ NK-cell lymphopenia; MDS (the percentage of blasts in the BM aspirate could be > 5%, but < 10%); a 10 of 10 matched related donor (MRD), an 8 of 8 matched unrelated donor (MUD), or a 4 of 6 or greater matched unrelated umbilical cord donor (UCB). MRDs were required to have no history of mycobacterial infections or any other opportunistic infections, and normal blood monocyte, NK-cell, and B-cell counts. We conducted this study before the gene defect was identified, therefore a MRD was only used when a MUD could not be identified, and the life expectancy of the patient was < 3 months.
Matched related and unrelated donors received 5 days of G-CSF (10 μg/kg/d), followed by apheresis on day 5 with the goal of collecting at least 5 × 106 CD34+ cells/kg of the recipient's body weight. The conditioning regimen for patients with a matched related or unrelated donor consisted of fludarabine 30 mg/m2/d on day −4, −3, and −2, and 200-cGy total body irradiation (TBI) on day −1. Matched related and unrelated donor peripheral blood stem cells (PBSCs) were infused fresh on day 0. The conditioning regimen for UCB recipients consisted of cyclophosphamide 50 mg/kg IV on day −6, fludarabine 30 mg/m2 on days −6 to −2, and 200 cGy TBI on day −1. UCB units were thawed and infused on day 0.
GVHD prophylaxis consisted of tacrolimus and sirolimus with initiation of the drugs on days −3 and −2, respectively. Both drugs were targeted at a level of 5-10 ng/mL. Immunosuppression was tapered at 6 months posttransplantation if there was no evidence of GVHD.
Supportive care
We followed standard guidelines for supportive care established at the National Institutes of Health Clinical Research Center for patients undergoing allogeneic HSCT.
T, B, and NK cells
CD14+ monocytes, CD3−/CD56+ NK cells, CD19+ B lymphocytes, and CD3+ T lymphocytes were quantified by flow cytometry pretransplantation and at designated intervals posttransplantation.
Cytogenetics
Cytogenetics were performed pretransplantation and at 28 days and 12 months after transplantation. When cytogenetic abnormalities were present, FISH was used to identify the presence of specific chromosomal abnormalities.
Analysis of chimerism
Engraftment of donor cells was assessed using polymorphisms in regions known to contain short tandem repeats. Peripheral blood CD14+, CD3−/CD56+, CD19+ and CD3+ cells were selected using flow cytometry at the designated time points, and chimerism was assessed on these subpopulations. In addition, CD14+/CD15+ myeloid cells and CD3+ T lymphocytes were selected using immunobeads, and chimerism was assessed on the selected cells. The lower limit of sensitivity for this method is 1%-3% of donor-type polymorphic markers in the mixture; these sensitivities are on the basis of studies using mixtures of known proportions of allogeneic DNA samples.
Statistical analysis
Descriptive statistics were used for chimerism, monocyte, NK, and lymphocyte counts.
Results
Characteristics of patients
Between April 2009 and September 2010, we performed allogeneic HSCT on 6 patients with GATA2 deficiency. The clinical characteristics of the 6 patients are summarized (Table 1). Median age of recipients was 33 years (range, 15-46), and the median duration of illness before the transplantation was 8 years (range 1-10). All patients had a history of disseminated NTM infection, and the majority had recurrent, severe cutaneous or genital HPV. Other opportunistic infections included invasive aspergillosis, disseminated nocardiosis, Clostridium difficile colitis requiring colectomy, and streptococcal osteomyelitis. Two patients (patients 1 and 2) had severe pulmonary hypertension and pulmonary alveolar proteinosis requiring whole lung lavage and supplemental oxygen at rest.
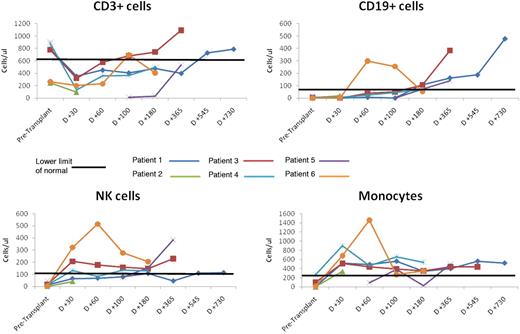
All 6 patients had characteristic hematologic abnormalities consisting of severely reduced CD14+ monocytes, CD19+ B lymphocytes, and CD3−/CD56+ NK cells, along with normal to slightly reduced CD3+ T lymphocytes in the peripheral blood (Table 1, Figure 1). In addition, all patients had MDS, and 3 had cytogenetic abnormalities associated with MDS: monosomy 7 in 1 patient, monosomy 6 in 1 patient, and trisomy 8 in 1 patient (Table 2). One patient (patient 5) had progression of MDS to refractory anemia with excess blasts (RAEB-2).
Absolute number of CD3+, CD19+, NK cells, and monocytes before and after HSCT.
The mutations in GATA2 in these patients are shown in Table 1. Four patients had missense mutations (patients 2-5), and 2 had deletions or insertions leading to frameshifts and predicted premature stop codons (patients 1 and 6).4
Three of the 6 patients had a first-degree relative with a myeloid malignancy: the sister of patient 2 ultimately died from complications of GVHD after MRD BM transplantation for chronic myelomonocytic leukemia; the mother of patient 3 died at age 32 of refractory AML; the son of patient 5 died from refractory AML at age 19 (Table 1).
Transplantation outcomes
Two patients received MRD transplantations, 2 received MUD transplantations, and 2 received UCB transplantations (Table 3). The transplant procedure itself was well tolerated. The CD34+ and CD3+ cell doses reflected the type of donor used, with MRD and MUD recipients receiving an ∼ 10-fold larger CD34+ and CD3+ cell doses than recipients of UCB.
Neutrophil engraftment (defined as a neutrophil count of > 0.5 × 109 cells/L for 3 consecutive days) was rapid in all patients except the patient who received a single UCB unit. The median duration of neutropenia was 11.5 days (range, 0-80). The median time to platelet engraftment (defined as a platelet count of > 20 × 109 cells/L for 7 consecutive days without requiring platelet transfusion) was 24.5 days (range 14-243). There were no instances of graft rejection. All patients except one were alive at a median follow-up of 17.4 months (range, 10-25).
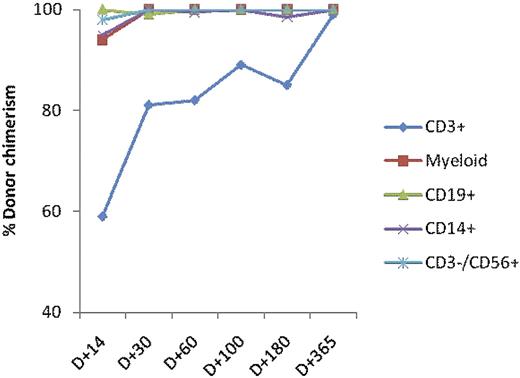
Reconstitution of the cellular compartments that were severely deficient before transplantation represented a primary objective of this study. The median percentages of donor CD3+, CD14+, CD19+, and CD3−/CD56+ cells at 1 year after transplantation, or at last follow-up for the 2 patients < 1 year from transplantation, are shown in Table 3 and Figures 1 and 2. All patients achieved 100% donor myeloid cells, as well as 99% to 100% CD14+ monocytes and CD19+ B cells. Only patient 6 had < 99% CD3−/CD56+ NK cells at last follow-up (Table 3). The kinetics of donor chimerism of CD19+, CD14/CD15+, CD56+, and CD3+ cells at different time points after the transplantation are shown (Figure 2). All patients achieved normal levels of CD19+ B cells, CD3−CD56+ NK cells, and monocytes by 1 year after HSCT (Figure 1).
Median percentage of donor chimerism. Donor chimerism of CD19+, CD14+, CD3−/CD56+, and CD3+ cells at designated time points after transplantation.
Median percentage of donor chimerism. Donor chimerism of CD19+, CD14+, CD3−/CD56+, and CD3+ cells at designated time points after transplantation.
Surprisingly, none of the patients had reactivation of either their NTM infections, or worsening of other preexisting infections after transplantation. Only patients 2 and 5 were at risk for CMV infection because of donor CMV seropositivity and recipient CMV seronegativity; both experienced CMV reactivation without disease that resolved on antiviral therapy. Patients 1, 3, and 4 had uneventful hospitalizations and were discharged by days 21, 14, and 17, respectively. Patient 1, who had been oxygen dependent before transplantation because of severe pulmonary hypertension and alveolar proteinosis, had marked improvement of his lung disease both functionally and on chest CT, and was free of supplemental oxygen and off all medications for pulmonary hypertension by 6 months after transplantation. At 2 years after the transplantation he is still off supplemental oxygen, and has stable pulmonary function tests. Even patient 2, despite receiving a transplant while on mechanical ventilation, had remarkable improvement of the pulmonary hypertension and hypoxia, before succumbing to GVHD and secondary infection. Patient 5 received a single UCB transplantation and required 76 days for engraftment.
All patients had MDS, and one-half had unfavorable chromosomal abnormalities in the BM. The cytogenetic abnormalities resolved by 6 months after transplantation.
All 5 surviving patients are outpatients and return for their follow-up visits at 6-month intervals. The 3 patients who are more than 1 year after transplantation are off all immunosuppressive medications, and off all antimycobacterial medications.
Adverse events
We anticipated major infectious complications posttransplantation in this group of immunocompromised patients. At the time of transplantation, the most severely ill patient, (patient 2), had been intubated for 30 days after whole-lung lavage for severe pulmonary alveolar proteinosis. She received conditioning and MRD transplantation while on mechanical ventilation and hemodialysis. Despite engraftment within 11 days of transplantation, she subsequently developed acute, steroid refractory GVHD after tacrolimus was discontinued because of posterior reversible encephalopathy syndrome. She died 3 months after transplantation because of complications of GVHD. Patient 4 developed an immune reconstitution inflammatory syndrome–like picture after MUD HSCT.7,8 She had mediastinal Myobacterium abscessus infection before the transplantation; 3 months after transplantation she developed new onset shortness of breath, with increased necrotic mediastinal lymph nodes, but negative stains and cultures. Treatment with prednisone resulted in resolution of all symptoms and decreased lymphadenopathy.
Patient 5 received a single UCB unit and had delayed engraftment. She developed a probable invasive fungal infection (new nodular lung lesion during prolonged neutropenia with high serum β-D-glucan). The lung nodule resolved with liposomal amphotericin B, voriconazole, and recovery of neutrophils.
Patient 6 received a double UCB transplantation. He developed autoimmune nephrotic syndrome and pancytopenia on day 90 correlating with complete switching of the dominant umbilical cord from UCB 1 to UCB 2 between days 60 and 100. His nephrosis and pancytopenia responded to rituximab and tacrolimus. During hospitalization, he developed an embolic right middle cerebral artery occlusion and was found to have culture negative endocarditis. He was treated empirically with broad-spectrum antimicrobial and antifungals with vegetation resolution over 2 months.
GVHD developed in 4 patients. Patients 1, 4, and 6 had late acute grade I-II GVHD at 9, 10, and 6 months after transplantation, respectively. As noted, patient 2 developed acute, steroid-refractory acute GVHD of the gut, skin and liver, and died from complications of GVHD and immunosuppression. There were no instances of chronic GVHD as assessed by the National Institutes of Health consensus criteria.9,10
Discussion
Here, we report that allogeneic HSCT results in reversal of the hematologic, immunologic, and clinical phenotype of a newly described, lethal, genetic immunodeficiency disease caused by mutations in GATA2. For matched related and unrelated donors, we used a nonmyeloablative-conditioning regimen.11 Patients receiving UCB transplantations were also conditioned with a modification of a nonmyeloablative regimen previously described in patients with hematologic malignancies receiving UCB donations.12,13
The underlying immunodeficiency in GATA2 deficiency—lack of monocytes, NK cells, B lymphocytes, and dendritic cells—may have facilitated engraftment and eradication of the malignant clone in this cohort of patients. Only 1 patient (patient 5) had delayed engraftment, and this patient received a single UCB unit. Engraftment occurred first in the myeloid compartment with all but 1 patient achieving 100% donor myeloid cells by 100 days posttransplantation. Donor CD3+ lymphoid chimerism lagged behind myeloid chimerism. The majority of patients with GATA2 deficiency harbored unfavorable cytogenetics with their MDS. Surprisingly, the malignant clone was essentially eradicated, irrespective of the donor source, in all patients harboring a cytogenetically abnormal clone pretransplantation. Only the patient with RAEB-2 received any prior chemotherapy before conditioning for transplantation.
We acknowledge that the role of nonmyeloablative conditioning in MDS is controversial because of the considerably higher rate of relapse compared with that seen with ablative regimens. However, the rapid engraftment and conversion to 100% donor myeloid chimerism in this cohort of patients may be attributable to the use of PBSCs, and to the lack of serotherapy in recipients of UCB.
Despite significant underlying organ system toxicity in the majority of patients with GATA2 deficiency, the regimen-related mortality was similar to that seen in other patients transplanted within the preceding decade.14 The success of allogeneic transplantation in this cohort of patients correlated with the clinical status of the patient at the time of transplantation. The 1 patient who died had had significant multiorgan dysfunction, and was intubated and on hemodialysis at the time of transplantation.
Alloreactive donor T cells are thought to mediate acute GVHD via interaction with host or donor APCs, in particular dendritic cells, in secondary lymphoid tissue.15,16 Because patients with MonoMAC lack dendritic cells,2 we speculated that they might develop less GVHD. In our cohort 4 of 6 patients developed acute GVHD, however, only 1 developed severe, early onset acute GVHD, and that occurred in the setting of stopping immunosuppression. In the other 3 patients the severity of GVHD was low grade.
These transplantations were performed before GATA2 was identified as the gene responsible for this disease. Because of the adult onset of disease, there was hesitancy to use related donors unless the patient's survival was < 3 months, and no unrelated donor was available. The clinical decision was made that the patient would not survive the potential prolonged neutropenia with UCB transplantation. In addition, based on the donor age, the donors were considered to be at very low risk of carrying the GATA2 mutation. We have subsequently demonstrated that the 2 related donors have normal wild-type GATA2 alleles (S.M.H., unpublished data, June 2011). Other patients with GATA2 deficiency likely have been transplanted without knowledge of the genetic defect. Bigley et al transplanted 2 patients with an autosomal dominant monocytopenia syndrome that is most probably GATA2 deficiency.2
GATA2 is crucial for the manteinance of HSCs,17 but it also plays a critical role in the transcriptional regulation of endothelial nitric oxide synthetase (eNOS).18,19 Some of the pulmonary changes seen in GATA2 deficiency likely result from pulmonary alveolar macrophage dysfunction and defective eNOS expression in the pulmonary epithelium. Important for our understanding of pulmonary physiology, BM transplantation markedly improved lung function in the 2 patients who had severe pulmonary hypertension and alveolar proteinosis. The critical link between hematopoiesis, nitric oxide synthase activity, and pulmonary arterial function suggests a novel role for BM transplantation.
In summary, we report that nonmyeloablative HSCT results in reversal of the hematologic, immunologic, and clinical manifestations in a newly described, genetic immunodeficiency with predisposition to MDS/AML because of GATA2 deficiency.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work has been supported with federal funds from the National Cancer Institute, National Institutes of Health, in part by the Division of Intramural Research, and in part under contract no. HHSN261200800001E.
The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the US government.
National Institutes of Health
Authorship
Contribution: J.C.-R., J.G.-B., S.M.H., and D.D.H. designed the research, supervised the study, and drafted the manuscript; A.F.F., A.P.H., C.S.Z., K.R.C., J.W., R.K., and K.N.O. provided critical revision of the manuscript for important intellectual content; K.R.C. reviewed the histopathology; and R.K. performed and analyzed the chimerism studies.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Dr Dennis D. Hickstein, 9000 Rockville Pike, Bldg 10/CRC, 3-3142, Bethesda, MD 20892; e-mail: hicksted@mail.nih.gov.