Abstract
Abstract 4521
About 1/3 of advanced Hodgkins lymphoma (HL) patients fail first line therapy and are candidates for autologous stem cell transplantation (ASCT). Studies describing the outcomes of relapsed/refractory HL in adults have shown that the long-term survival is about 40–60%, following treatment with high dose chemotherapy and ASCT. Surveillance, Epidemiology and End Results (SEER) data indicates that children/adolescents with HL have different disease characteristics from adults (Bazzeh et al, Leukemia and Lymphoma 2010), which we hypothesized could lead to different ASCT outcomes. The aim of this study was to describe the demographic distribution of relapsed/refractory HL patients requiring ASCT at a major transplant center and to study the overall survival (OS) post ASCT with age as a covariate.
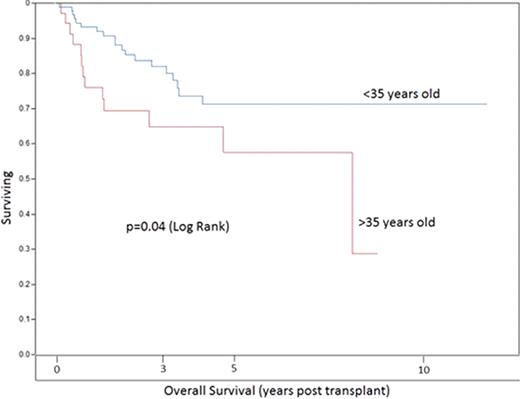
We performed an IRB approved, retrospective analysis of a combined cohort of adult and pediatric HL patients undergoing ASCT at Winship Cancer Institute at Emory University and Children’s Healthcare of Atlanta from 1995 to 2011. A total of 131 patients were included in the study (adult=112, pediatric=19). Demographics of patients include: 54% male, 65% Caucasians, 26% African American. The mean age of diagnosis was 30 ± 12 years and the mean age at transplant was 33 ± 13 years. Patients were divided into two categories, younger (≤35 years, n=96) and older (>35 years old, n=35), based on the bimodal distribution of the incidence of HL observed in the SEER database (first peak in the age group 15–35 years and the second one around 55 years). Overall survival was compared using Kaplan Meier estimates for the time-to-event analysis and log rank test for comparing the two groups. Predicted survival for individuals of different ages (in the absence of cancer) was derived from Social Security Administration life tables.
As expected from the incidence data in the SEER database, there was a bimodal distribution of age at diagnosis among HL patients undergoing ASCT for relapsed/refractory disease, with a first peak at 25 years and the second peak at 46 years [Figure 1]. 75% patients had nodular sclerosing histology, 8% had mixed-cellularity and 6% had the lymphocyte predominant histological subtype. The distribution of histological subtypes did not differ by age. A univariate analysis revealed that patients with age > 35 years had significantly higher post-transplant mortality (p=0.037) than those ≤35 years [Figure 2]. A multivariable model that included age ≤35, histology, disease status at transplant and chemo-sensitivity indicated that only one of these variables (age) was explanatory in the model.
As expected by the increased suitability of ASCT for younger patients, the number of patients ≤35 years undergoing ASCT for refractory/relapsed HL was much higher than the number of older patients. Overall survival of older HL patients who underwent ASCT was worse than that for younger HL patients, likely due to differences in supportive care, toxicity from treatments, and comorbid diseases. The age related differences in post-transplant survival were not explained by the decreased actuarial life expectancy of older subjects based upon life-table projections of survival for the general population. The bimodal distribution in the incidence of HL, and the inferior survival of older HL patients undergoing ASCT suggests that there may be differences in the biology of the disease based upon the age at which HL is diagnosed. Alternative strategies for autologous transplantation of older patients with relapsed/refractory HL are needed.
Flowers:Genentech/Roche (unpaid): Consultancy; Celgene: Consultancy, Research Funding; Millennium/Takeda: Consultancy, Research Funding; Spectrum: Consultancy, Research Funding; Novartis: Research Funding; Seattle Genetics: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.